Abstract
The main aim of this project was to explore the efficacy of Acceptance and Commitment Therapy (ACT)‐based educational course in different formats (i.e., pure and guided self‐help with different durations, and guided self‐help with and without access to a discussion forum) for body shape dissatisfaction. Two randomized controlled studies (RCT) were carried out. In the first RCT, the participants were randomized to a 12‐ or 16‐week guided self‐help, a 16‐week pure self‐help, or a waitlist control condition. In the second RCT, the efficacy of 12‐week guided self‐help with or without access to a discussion forum was investigated. ACT‐based self‐help resulted in promising improvements in body shape dissatisfaction, and modest effects on general health indicators (i.e., symptom of depression, self‐esteem, satisfaction with life, and quality of life). The findings also showed no additional effects of support, access to the online discussion forum, and longer duration of self‐help, suggesting the 12‐week self‐help with or without support is a viable option for reducing body shape dissatisfaction.
Keywords: Body shape dissatisfaction, acceptance and commitment therapy, educational course, guided and pure self‐help, discussion forum, randomized controlled trial
INTRODUCTION
Body dissatisfaction, a negative evaluation of one’s own physical body (Stice & Shaw, 2002), is a prevalent problem affecting more than half of all females (Garner, 1997). It is positively associated with depression (Stice, Hayward, Cameron, Killen & Taylor, 2000), suicidal ideation (Kim, 2009), anxiety (Kostanski & Gullone, 1998), unhealthy eating behaviors (Neumark‐Sztainer, Wall, Story & Perry, 2003), and reduced self‐esteem (Tiggemann, 2005). It is also a risk factor for later development of eating disorders (e.g., Fairburn, Cooper, Doll & Welch, 1999; Stice, 2002). Hence, primary interventions for body dissatisfaction are considered critical both to improve the general psychological health of individuals with this problem and to prevent other more complex conditions such as eating disorders (Ghaderi, 2001). However, the majority of those suffering from body dissatisfaction neither seek nor receive any psychological treatment.
Interventions for body dissatisfaction, including self‐help, have been mostly based on Cognitive Behavioral Therapy (CBT; e.g., Cash, 1997), with promising evidence of efficacy (e.g., Jarry & Ip, 2005; Strachan & Cash, 2002). On the other hand, some researchers (e.g., Mancuso, 2016; Stewart, 2004) asserted that mindfulness‐based interventions enhancing the psychological flexibility – the state of being fully aware of the present moment and all inner experiences while moving toward life goals – might also have positive impacts on body image concerns by weakening rigid and inflexible aspects of them (i.e., thoughts, behaviors, emotions, and perceptions). In this sense, Acceptance and Commitment Therapy (ACT; Hayes, Luoma, Bond, Masuda & Lillis, 2006), which includes mindfulness and acceptance strategies and is one of the CBT's third‐wave approaches, has received attention in the literature (e.g., Pearson, Heffner & Follette, 2010; Sandoz, Wilson & Dufrene, 2011). Studies yielded encouraging findings regarding the efficacy of ACT‐based interventions on reducing body image concerns, including body dissatisfaction (e.g., Fogelkvist, Gustafsson, Kjellin & Parling, 2020, and see Griffiths, Williamson, Zucchelli, Paraskeva & Moss, 2018 for a review). To build on previous studies and extend their findings, we evaluated the efficacy of an educational course based on ACT. According to this approach, avoidance of negative experiences might give short‐term relief but long‐term detrimental consequences. Hence, ACT mainly encourages people to embrace their unwanted or negative experiences (i.e., emotions, thoughts, and physical sensations) that they usually avoid and not to react to these experiences with maladaptive responses such as suppression (Hayes et al., 2006).
Face‐to‐face psychological interventions for body dissatisfaction will never be available on a wide scale for such a widespread problem, not only due to its high prevalence, but also due to the low number of specialist therapists, time and costs, and stigmatization towards those receiving psychological treatment (Cuijpers, van Straten & Andersson, 2008). Pure or guided self‐help might be a viable solution to address many of these obstacles (Andersson & Titov, 2014). Also, it has been strongly suggested that low‐cost interventions such as self‐help should be applied first, and that the intense and high‐cost treatments should be reserved for people who do not benefit from low‐intensity treatments (Haaga, 2000). Consequently, self‐help appears to be a viable option for reducing body dissatisfaction (Hrabosky & Cash, 2007; Strachan & Cash, 2002).
The role of support by a facilitator on the efficacy of self‐help is unclear. Whereas some meta‐analyses supported the superiority of guided self‐help over pure self‐help (e.g., Hirai & Clum, 2006; Jarry & Ip, 2005), others established that facilitator contact yields no additional effect (e.g., Farrand & Woodford, 2013; Gloud & Clum, 1993). Despite these inconsistent findings, some researchers suggest minimal therapist contact for increasing the compliance of intervention or monitoring progress even when they have no therapeutic purpose (e.g., Cash & Hrabosky, 2003; Haug, Nordgreen, Öst & Havik, 2012). To extend the findings from previous studies (e.g., Fogelkvist et al., 2020), the efficacy of pure and guided self‐help was investigated in the current study.
The relation between dose (i.e., number of therapy session) and response (i.e., therapy outcome) has been extensively investigated in psychotherapy research (for a meta‐analysis see: Howard, Kopta, Krause & Orlinsky, 1986). Hansen, Lambert, and Forman (2002) found that an average of 12.7 sessions is adequate for a significant proportion of patients to achieve targeted improvements. However, in the following years, Harnett, O’Donovan, and Lambert (2010) suggested that more therapy sessions are required to obtain reliable therapy outcomes. Time in therapy might be an important variable per se. Thus, two different durations of self‐help (12 and 16 weeks) were investigated in the current study.
Even though a previous meta‐analysis indicated that the use of online discussion forums does not increase intervention effectiveness (Barak, Hen, Boniel‐Nissim & Shapira, 2008), qualitative studies have established that they provide a safe and flexible therapeutic environment to their users (e.g., Kendal, Kirk, Elvey, Catchpole & Pryjmachuk, 2017). Also, the use of forums was found to be positively associated with optimism, control over the future, and self‐confidence in the treatment process (Aardoom, Dingemans, Boogaard & Van Furth, 2014). Consequently, we assessed whether accessing such a forum would increase the efficacy of self‐help.
Previous systematic reviews have indicated that self‐help for body dissatisfaction lead to improvements in several indicators of general psychological health such as depression and self‐esteem (Jarry & Berardi, 2004; Jarry & Ip, 2005). These indicators were also assessed in the current studies within this project.
To summarize, we conducted two studies of ACT‐based self‐help that presented as an educational course for body dissatisfaction. In the first study, we investigated the efficacy of 12‐ or 16‐week guided self‐help, and a 16‐week pure self‐help, compared to a waitlist control condition. In the second study, we investigated the efficacy of 12‐week guided self‐help with or without access to a discussion forum.
Study 1: Method
In this trial, the participants were randomized to one of four conditions: 12‐week guided self‐help, 16‐week guided self‐help, 16‐week pure self‐help, or a waitlist control condition. The effects of the self‐help courses on body shape dissatisfaction and general psychological health indicators, namely depression, self‐esteem, satisfaction with life, and quality of life, were assessed. It was hypothesized that those in the active groups would report significantly more improvements in all outcomes compared to the waitlist control condition. However, as we adopted an exploratory approach for differences between the active conditions, no hypothesis was proposed in this regard.
Participants
Of the 236 who responded to the ads, 196 completed the screening, of which 108 were excluded based on inclusion and exclusion criteria. The remaining 88 were asked to get access to the self‐help book and to respond to the baseline questionnaires. A total of 71 females, aged 18–55 years (M = 30.5, SD = 8.1) did so and participated. Of them, 36.6% (n = 26) were students, 56.3% (n = 40) were employees, and the rest (7.0%, n = 5) reported other occupations. In terms of educational background, 70.4% (n = 50) had a university degree, 18.3% (n = 13) had completed high school, and 11.3% (n = 8) reported other education. The average body mass index (BMI) was 24.5 (SD = 3.5).
Measurements
Screening measures
In the screening process, a demographic information list, Montgomery‐Åsberg Depression Rating Scale‐Self‐rated (MADRS‐S; Svanborg & Åsberg, 1994), Eating Disorder Examination Questionnaire (EDE‐Q; Fairburn & Beglin, 1994), and Symptom Check List – 90 (SCL‐90‐R, Derogatis, 1994; Fridell, Cesarec, Johansson & Malling Thorsen, 2002) were used to select eligible subjects.
Primary outcome measure
Body Shape Questionnaire (BSQ; Cooper, Taylor, Cooper & Fairburn, 1987) was used to assess body shape dissatisfaction. It consists of 34 items measured on a six‐point Likert scale ranging from 1 (never) to 6 (always). Higher scores on the BSQ indicate stronger body shape dissatisfaction. The Swedish version of the BSQ showed good psychometrics, including high test‐retest reliability (0.90) (Ghaderi & Scott, 2004).
Secondary outcome measures
The Montgomery–Åsberg Depression Rating Scale‐Self assessment (MADRS‐S; Svanborg & Åsberg, 1994) was used to measure the severity of depression symptoms. It consists of nine statements rated on a seven‐point Likert scale ranging from zero to six and the total score ranges from 0 to 63. Higher scores indicate more severe symptoms.
The Satisfaction with Life Scale (SWLS; Diener, Emmons, Larsen & Griffin, 1985) is a self‐report inventory used to assess one’s general life satisfaction. It includes five items (e.g., the conditions of my life are excellent) rated on a seven‐point Likert scale ranging from 1 (strongly disagree) to 7 (strongly agree). Higher scores reflect higher perceived life satisfaction.
The Rosenberg Self‐Esteem Scale (RSES; Rosenberg, 1965) is a 10‐item scale used to assess one’s global self‐worth. The items (e.g., I certainly feel useless at times) are rated on a four‐point Likert scale ranging from 1 (strongly agree) to 4 (strongly disagree). Higher scores represent higher perceived self‐worth.
The Quality of Life Inventory (QOLI; Frisch, Cornell, Villanueva & Retzlaff, 1992) assesses one’s subjective well‐being and happiness. It consists of 16 life domains such as health, love, and work. Respondents evaluate each life domain based on how its importance for them (ranging from 0 = not important to 2 = very important) and how much they are satisfied with it (ranging from −3 = very dissatisfied to +3 = very satisfied). Higher scores reflect higher subjective well‐being.
Educational course
The course consisted of reading and doing exercises in the ACT‐based self‐help book for body dissatisfaction Lev med din kropp [Live with your body] (Ghaderi & Parling, 2009). The first part includes information and psychoeducation about appearance, body perception, factors contributing to the development of negative body image, self‐esteem and self‐image. The six processes in ACT are presented as skills to practice to enable the participants to live a rich life with their body. A short description of the content follows: step (1) identifying and clarifying values and set goals accordingly; step (2) increase awareness of consequences of avoidance and control behaviors and the importance of thoughts; step (3) the association between body image and self‐esteem, improving self‐esteem via behaviors connected to values; step (4) recognize common thinking errors and their consequences, conducting behavioral experiments; step (5) learning willingness and acceptance, labeling inner experiences without reacting on them; step (6) engaging in present moment awareness of the body in activities; and step (7) review, making plans for future, and relapse prevention. At each step, the readers are encouraged to engage in behaviors according to their values and practice mindfulness guided by audio files that accompany the book (http://www.nok.se/levmeddinkropp).
The pure self‐help condition: the participants read and worked through the material on their own. The researchers only sent reminders for filling out the measurements.
The guided self‐help conditions: the participants read and worked through the material and received weekly support via e‐mail that consisted of validation of difficulties and encouraged positive progress but no therapeutic interventions. The support was provided by two facilitators, who were pursuing their postgraduate education in psychology. The standardization of support was ensured with the help of predetermined start and end sections of e‐mail messages, peer‐supervision and supervision of an experienced psychotherapist. The facilitators responded to the participants within 48 hours. When a participant did not email at her specific day of communication about the program, reminders (a maximum of three reminders for the first week and only one reminder for each following week) were sent.
The waitlist control condition: the participants waited until the post‐course assessments were completed before they received guided self‐help.
Procedure
Information about the study was provided through Internet forums, flyers, magazines, and weekly newspapers. Those interested were asked to visit a secure website where they could read about the study, and complete a screening battery after online informed consent was obtained. Participants were informed about the study which was presented as an educational course for improving body image, the voluntary nature of the study, and that they could terminate their participation in the study at any time without providing a reason. They were also informed that all data would be handled securely, and only accessible by eligible research staff within the project. They were also informed that data and outcome would be presented on group level in scientific journals. Inclusion criteria were being adult, female with body image concerns. As the study was presented as an educational course for improving body image, and to ensure the safety of all the participants, the following exclusion criteria were applied: being underaged, BMI < 19, scoring over 30 on MADRS‐S that indicates severe depression, indications of suicidality (over three points on the suicide question of the MADRS‐S), indication of eating disorders (reported symptoms of eating disorders in the EDE‐Q that would be verified later in a telephone interview), any indication of addiction or psychotic symptoms (as indicated by the SCL‐90‐R), and ongoing psychological treatment. Subjects excluded from the study were informed about the reasons for their exclusion, and when deemed adequate received information as how and where to seek information and support. Participants were then asked to obtain a copy of the self‐help book and to fill out the baseline measures. They were then randomly assigned to one of two facilitators and one of four conditions via an Internet‐based randomization service (www.randomizer.org) (please see Fig. 1 for the details on the flow of subjects in the study). No difference were found across randomized groups in terms of baseline measures or demographics. The subjects in the active conditions were informed via e‐mail about how long their course would last and with whom they would be in contact throughout the course. Those in the waitlist control condition were notified that their course would start when the post‐course assessments were completed for the other groups. At the end of the course, the participants were invited via e‐mail to log in to the study website to respond to the assessment battery. After the posttest, all the identifying information that could be linked to individual participants was deleted to secure the anonymity of participants.
Fig. 1.
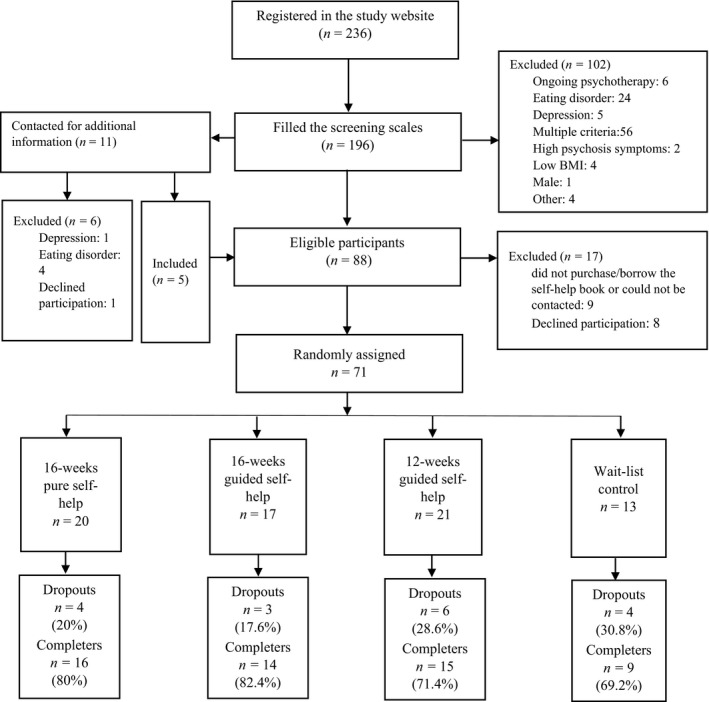
Chart showing the flow of participants through the first study.
Analytic strategy
Data were screened and tested for normality via descriptive statistics and Q‐Q plots. A binary logistic regression analysis was conducted to explore if the baseline data, age, and body mass index (BMI) predicted dropout or completer status. Fisher’s exact test was performed to see if dropouts were independent of the conditions. For hypothesis testing, we preferred generalized linear mixed models (GLMM) instead of traditional analyses as this approach offers several statistical advantages such as including participants with partial data mostly caused by dropout (for details see Heck, Thomas & Tabata, 2014). The between‐subject factor was group with four conditions whereas the within‐subject factor was time with two conditions (i.e., the pretest and the posttest). We used Fisher’s least significant difference (LSD) post hoc test for multiple comparisons and Cohen’s d for measuring effect sizes (Cohen, 1988). All the statistical analyses were conducted using SPSS version 26 (IBM Corp, 2019). Besides, clinical improvement in completers’ BSQ scores was examined using the Reliable Change Index (RCI = 22.36) and the criterion of c for clinical significance (c = 108.54), according to the guideline suggested by Jacobson and Truax (1991), using Swedish clinical and normal samples’ BSQ scores (Ghaderi & Scott, 2004). We considered participants who achieved a reliable change in the expected direction and passed the cut‐off as recovered, those who achieved a reliable change in the expected direction but could not pass the cut‐off as improved, those who achieved a reliable change in the opposite direction as deteriorated, and the rest as unchanged. Lastly, we conducted Fisher's exact test to compare the conditions in terms of the number of clinically improved participants.
Results
The overall attrition rate was 23.94%. The binary regression model testing the predictive effects of age, body mass index (BMI), and baseline scores of the outcome measures on dropout was significant, χ 2 (7) = 15.98, p = 0.025, Nagelkerke R 2 = 31. Of the predictors, lower BMI [Wald χ 2 (1) = 4.71,p = 0.030, OR = 0.72, 95% CI [0.53, 0.97]] and lower depressive symptomatology [Wald χ 2 (1) = 6.47, p = 0.011, OR = 0.79, 95% CI [0.66, 0.95]] were associated with an increased probability of dropping out of self‐help. However, age (p = 0.059), body shape dissatisfaction (p = 0.411), quality of life (p = 0.737), self‐esteem (p = 0.704), and satisfaction with life (p = 0.087) were not significant predictors for distinguishing between the dropouts and completers. In addition, dropout was independent of the condition, according to Fisher’s exact text.
We tested the efficacy of self‐help through GLMM. As descriptive statistics and Q‐Q plots had supported the normality of data, we specified the probability distribution as normal and the link function as identity in the analyses. Table 1 shows the means and standard errors of the outcome variables for each condition and time point.
Table 1.
Estimated means, standard errors, and cohen’s d within and between group effect sizes of the outcome variables
| 12‐WG (n = 21) | 16‐WG (n = 17) | 16‐WP (n = 20) | WC (n = 13) | Cohen’s d between‐group at the posttest | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
Pretest M (SE) |
Posttest M (SE) |
d within‐group |
Pretest M (SE) |
Posttest M (SE) |
d within‐group |
Pretest M (SE) |
Posttest M (SE) |
d within‐group |
Pretest M (SE) |
Posttest M (SE) |
d within‐group | 12‐WG vs. 16‐WG | 12‐WG vs. 16‐WP | 12‐WG vs. WC | 16‐WG vs. 16‐WP | 16‐WG vs. WC | 16‐WP vs. WC | |
| BSQ | 117.24 (6.06) | 90.81 (5.67) | 0.94 | 116.71 (5.07) | 91.12 (6.73) | 1.31 | 115.55 (6.33) | 91.05 (7.99) | 0.95 | 114.23 (9.13) | 111.62 (8.51) | 0.19 | 0.01 | 0.01 | 0.77 | 0.00 | 0.73 | 0.63 |
| MADRS‐S | 16.43 (1.41) | 11.95 (1.40) | 0.67 | 15.00 (1.39) | 12.00 (1.49) | 0.44 | 14.55 (6.07) | 10.80 (1.33) | 0.59 | 12.92 (1.89) | 10.92 (2.11) | 0.42 | 0.01 | 0.19 | 0.15 | 0.20 | 0.16 | 0.02 |
| RSES | 2.81 (0.31) | 3.38 (0.33) | 0.51 | 2.12 (0.38) | 3.18 (0.39) | 0.85 | 2.70 (0.33) | 3.50 (0.27) | 0.62 | 3.38 (0.43) | 3.69 (0.41) | 0.33 | 0.13 | 0.09 | 0.21 | 0.23 | 0.34 | 0.15 |
| SWLS | 18.52 (1.31) | 21.62 (1.65) | 0.53 | 19.82 (1.68) | 21.35 (1.67) | 0.40 | 20.70 (1.47) | 23.30 (1.68) | 0.48 | 21.46 (1.70) | 22.54 (1.78) | 0.48 | 0.04 | 0.23 | 0.13 | 0.28 | 0.18 | 0.11 |
| QOLI | 1.02 (0.30) | 1.52 (0.31) | 0.35 | .84 (0.33) | .95 (0.37) | 0.11 | 1.22 (0.35) | 1.71 (0.39) | 0.48 | 1.33 (0.34) | 1.69 (0.40) | 0.51 | 0.40 | 0.12 | 0.12 | 0.47 | 0.51 | 0.01 |
BSQ = Body Shape Questionnaire; MADRS‐S = The Montgomery–Åsberg Depression Rating Scale; RSES = Rosenberg Self‐Esteem Scale; SWLS = The Satisfaction with Life Scale; QOLI = The Quality of Life Inventory; 12‐WG = 12‐weeks guided self‐help; 16‐WG = 16‐weeks guided self‐help; 16‐WP = 16‐weeks pure self‐help; WC = Waitlist Control.
For our primary outcome variable, that is, body shape dissatisfaction, GLMM showed a significant time effect [F(1, 134) = 48.63, p < 0.0001] and a groupXtime interaction effect [F(3, 134) = 3.39, p = 0.02]. According to fixed coefficients, change across time in the 12‐ [t(134) = 2.87, p = 0.005] and the 16‐week [t(134) = 2.65, p = 0.009] guided, and the 16‐week pure self‐help [t(134) = 2.62, p = 0.01] conditions were significantly different from the waitlist control condition. On the other hand, the post hoc test results indicated that the participants in both the 12‐week guided condition (M = 90.81, SD = 25.96, p = 0.043) and the 16‐week pure condition (M = 91.05, SD = 35.74, p = 0.048) had significantly lower BSQ scores than those in the control condition (M = 111.62, SD = 30.70) at the posttest, with medium effect sizes (d = 0.77 and 0.63, respectively). However, the 16‐week guided condition (M = 91.12, SD = 27.75, p = 0.056) did not differ from the control condition despite the medium effect size (d = 0.73). Also, no significant difference was found between the active conditions (p > 0.97).
The secondary outcome variables were depression, satisfaction with life, self‐esteem, and quality of life. We found a significant time effects for depression [F(1, 134) = 18.85, p < 0.0001], satisfaction with life [F(1, 134) = 12.92, p < 0.0001], self‐esteem [F(1, 134) = 23.38, p < 0.0001], and quality of life [F(1, 134) = 7.23, p < 0.008], but no interaction (groupXtime) effect.
Lastly, by taking into consideration the advantages of clinical significance over statistical significance (Jacobson & Truax, 1991), we also carried out the clinical significance test for BSQ scores. According to the results, in the 12‐week guided self‐help, 40.0% of the participants (n = 6) remained unchanged, 6.7% (n = 1) improved, and 53.3% (n = 8) recovered. In the 16‐week guided self‐help, 35.7% (n = 5) remained unchanged, 21.4% (n = 3) improved, and 42.9% (n = 6) recovered. In the 16‐week pure self‐help, 37.5% (n = 6) remained unchanged, 31.3% (n = 5) improved, and 31.3% (n = 5) recovered. However, in the waitlist condition, 11.1% (n = 1) deteriorated and the rest (88.9%, n = 8) remained unchanged. [Corrections made on 20 January 2021, after first online publication: In the preceding statements, ‘self‐help, 35.7%’ has been corrected to ‘self‐help, 37.5%’ and ‘11.1% (n = 6)’ has been corrected to ‘11.1% (n = 1)’ in this version] The results of Fisher's exact test showed that clinical improvements were different across the conditions (p = 0.021). Whereas the proportions of improved and recovered participants were similar across the active conditions, they were significantly higher as compared to those in the waitlist control condition (p < 0.05).
Brief discussion
For body shape dissatisfaction, both the GLMM and the clinical significance test results mostly supported the efficacy of the educational course in the self‐help format; the active conditions reached larger reductions on BSQ scores as compared to the control condition. These findings are all consistent with a systematic review that suggested that ACT might facilitate reduction in body image dissatisfaction and weight self‐stigma in adults (Griffiths et al., 2018). Concerning the general psychological health indicators, depression scores reduced and satisfaction with life, self‐esteem, and quality of life scores increased, but the active conditions were not superior to the control condition.
We did not find any difference between the active conditions in terms of any outcome variables, which is not surprising given the small samples and dropouts. More precisely, pure and guided self‐help led to similar changes. Even though this finding conflicts with the meta‐analytic findings of Jarry and Ip (2005), it confirms the meta‐analytic findings of Farrand and Woodford (2013). Also, the dropout rates were similar between these two conditions. Thus, these findings suggest that it is possible to obtain similar improvements without support. Similarly, the 12‐ and 16 conditions were not different from each other on neither the improvements in the outcome variables nor the dropout rates. Hence, the 12‐week program might be a viable option for reducing body shape dissatisfaction.
Study 2: Method
The aim of this trial was to investigate the efficacy of 12‐week guided self‐help with or without access to a discussion forum. It was hypothesized that access to a discussion forum would increase the efficacy of self‐help.
Participants
Of 102 potentially interested participants, 79 completed the screening, of which 39 were excluded based on inclusion and exclusion criteria. Then, 12 participants in the waiting list control condition of the first RCT were added to the remaining pool of 40 to be randomized to one of the conditions. In total, 12 out of 52 did not get access to the self‐help book or fill out the baseline measures, which resulted in a total sample of 40 females, aged 18–61 years (M = 36.68, SD = 10.54). Of them, 25.0% (n = 10) were students, 55.0% (n = 22) were employees, and the rest (20.0%, n = 8) reported other occupations. In terms of educational background, 72.5% (n = 29) had a university degree, 15.0% (n = 6) had completed high school, and 12.5% (n = 5) reported other education. The average of their BMI was 27.65 (SD = 7.06).
Measurements
In this trial, our primary outcome variable was body shape dissatisfaction and secondary outcome variables were depression, self‐esteem, and satisfaction with life. Hence, except for QOLI, the scales were the same as ones used in the first trial.
Educational course
The course was the same as in the first trial, consisted of reading and doing exercises in the self‐help book.
The condition without access to the discussion forum: the participants received guided self‐help, they read and worked through the material and received weekly support via e‐mail from a facilitator (please see the first trial for the details of the support).
The condition with access to the discussion forum: in addition to the guided self‐help, the participants had access to a password‐protected online discussion forum for exchanging personal experiences about the educational course and body image issues. The forum was activated 2 weeks later after the course had started to make sure they had time to accumulate some experiences and questions. As no posts were observed in the 2‐week period following the activation, the participants received an e‐mail asking them to send and respond to at least one post for each of seven steps in the self‐help book. The forum was monitored daily to ensure that no inappropriate or offensive posts were present. No such posts were detected. After the course was completed, the discussion forum was closed.
Procedure
Participants were recruited in the same manner as in study 1. Inclusion and exclusion criteria were the same as in the first study, with the exception of BMI, for which the cut‐off for exclusion was <18.5 instead of <19. The eligible participants were randomly assigned to one of two facilitators and one of two conditions via an Internet‐based randomization service (www.randomizer.org) (please see Fig. 2 for the details on the flow of subjects in the study). No significant difference between the groups in terms of age, BMI, and baseline measures was found. After randomization, the participants were informed about the course via e‐mail and asked to purchase or borrow the self‐help book. For participants who were included from the waitlist control condition of the first trial, their posttest scores in the first study were considered as their pretest scores in this trial, whereas newly recruited participants were asked to complete the baseline measures. At the end of the course process, the participants were invited via e‐mail to log in to the study website to respond to the post‐course measures within 3 days. Those who did not do so were remined by e‐mail first and then by phone.
Fig. 2.
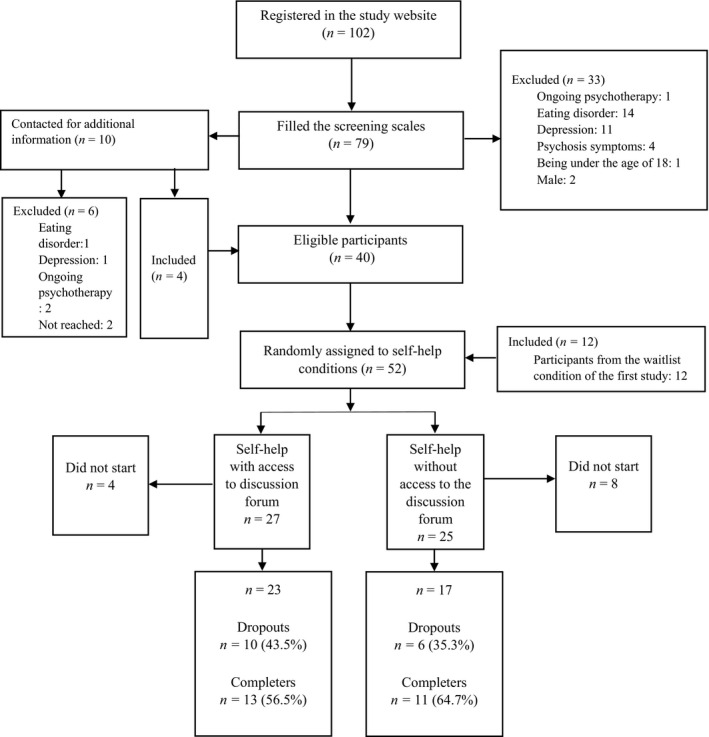
Chart showing the flow of participants through the second study.
Analytic strategy
We followed the same strategy as in the first trial. The only difference was the use of Chi‐Square instead of Fisher’s exact test to examine if dropouts were associated with the conditions. In this trial, the Reliable Change Index for BSQ scores was 23.91.
Results
The attrition rate after the start of the course was 40%. According to the results of binary regression analysis, age, BMI, and baseline measures of outcome did not predict the dropout [χ 2 (6) = 6.52, p = 0.368], indicating that the dropouts were random. Also, the results of the chi‐square test of independence showed that dropouts were not related to the conditions.
We performed GLMM to test the study hypothesis. Since the normality assumption was met for each outcome variable, we specified the probability distribution as normal and the link function as identity in the analyses. Table 2 shows the means and standard errors of the outcome variables for each condition and time point.
Table 2.
Estimated means, standard errors, and cohen´s d within and between group effect sizes of the outcome variables
|
Self‐help with access to discussion forum (n = 23) |
d within‐group |
Self‐help without access to discussion forum (n = 17) |
d within‐group | d between‐group at the posttest | |||
|---|---|---|---|---|---|---|---|
|
Pretest M (SE) |
Posttest M (SE) |
Pretest M (SE) |
Posttest M (SE) |
||||
| BSQ | 128.43 (5.52) | 104.45 (7.83) | 0.87 | 116.06 (6.43) | 93.00 (7.29) | 0.78 | 0.34 |
| MADRS‐S | 13.87 (1.51) | 11.96 (1.71) | 0.46 | 15.71 (1.46) | 13.65 (1.81) | 0.34 | 0.22 |
| RSES | 2.52 (0.34) | 3.00 (0.36) | 0.28 | 3.35 (0.38) | 3.65 (0.36) | 0.28 | 0.41 |
| SWLS | 17.74 (1.53) | 20.30 (1.76) | 0.42 | 21.24 (1.72) | 22.24 (1.82) | 0.42 | 0.25 |
BSQ = Body Shape Questionnaire; MADRS‐S = The Montgomery–Åsberg Depression Rating Scale; RSES = Rosenberg Self‐Esteem Scale; SWLS = The Satisfaction with Life Scale.
For body shape dissatisfaction, GLMM indicated a significant time effect [F(1, 76) = 26.83, p < 0.0001], but no interaction (time × condition) effect. Body shape dissatisfaction decreased over time in the both conditions, representing a large effect size (d = 0.78–0.87). This pattern was also the same for two secondary outcome variables, depression and satisfaction with life; a significant time effect [F(1, 76) = 5.92, p = 0.017; F(1, 76) = 5.08, p = 0.027, respectively], but no interaction effect. However, regarding self‐esteem, there was neither a significant time effect [F(1, 76) = 2.73, p = 0.103] nor an interaction effect. The effect sizes at the posttest scores were small for all outcome measures (d = 0.22–0.41). Thus, contrary to our expectation, these findings indicated that access to a discussion forum does not improve the efficacy of self‐help.
Furthermore, we conducted a clinical significance test to check if the change over time in BSQ scores was clinically meaningful. According to the results, in the condition with access to discussion forum, 23.1% of the participants (n = 3) remained unchanged, 38.5% (n = 5) improved and 38.5% (n = 5) recovered. On the other side, in the condition without access to discussion forum, 36.4% of those (n = 4) remained unchanged, 9.1% (n = 1) improved, and 54.5% (n = 6) recovered. The results of Fisher's exact test confirmed that both conditions led to similar clinical improvements in terms of body shape dissatisfaction.
Brief discussion
The results indicated significant pre‐to‐post changes in terms of body shape dissatisfaction, depression, and satisfaction with life, but not for self‐esteem. Body shape dissatisfaction decreased over time, with large effect sizes that were compatible with those obtained from the active conditions in the first trial (see Tables 1 and 2). The observed change in body dissatisfaction was also clinically significant. This finding is consistent with the findings of the first trial and the previous studies (e.g., Fogelkvist et al., 2020) investigating the efficacy of ACT‐based intervention on body image. For secondary outcome variables, participants reported greater satisfaction with life and less depression at the posttest as compared to the scores at the pretest. However, the effect sizes of these changes were small and not better than the effect sizes observed for the control condition in the first trial (see Tables 1 and 2), strengthening the possibility of the natural course of depression and satisfaction with life might have caused these changes. Besides, no significant improvement in self‐esteem over time was found. Even though all these findings contradict the previous findings showing the positive effects of stand‐alone interventions for body image on general psychological health indicators (see Jarry & Berardi, 2004 for a review), it should be considered that the small sample size in the current trial might have caused this inconsistency.
Access to the online discussion forum did not contribute to the efficacy of the course. This is in line with previous meta‐analytic findings showing that discussion forums used as a component of interventions do not produce an additional effect (Barak et al., 2008). Lack of effect of discussion forum might be explained by the significance of support provided by facilitators. The guidance and support might have already met the informational and emotional needs of the participants, making the discussion forum redundant and thus underused. The activity level in the discussion forum was quite low; the average number of messages was 2.09 for all participants in the condition with access to the forum, and 3.54 for the completers. Given the previous findings demonstrating the positive relationship between the frequency of using online peer interaction and getting better results (Houston, Cooper & Ford, 2002), the current low activity level might have hampered the impact of the discussion forum.
General discussion
The present project investigated the efficacy of the ACT‐based self‐help presented as an educational course on body shape dissatisfaction as well as depression, satisfaction with life, self‐esteem, and quality of life. Also, it attempted to find out which combinations in terms of the presence of facilitator support (with support vs. pure), access to a discussion forum (with access vs. without access), and the duration of the process (12 vs. 16‐week) are best for the effectiveness of the course.
The findings for the efficacy of the educational course on body shape dissatisfaction were promising. The results of GLMM and the magnitude of the pre‐to‐post changes – large effect sizes for the active conditions but very small effect size for the control condition – showed that the active conditions produced better outcomes as compared to the control condition. Consistently, the results of clinical significance tests in both trials confirmed the efficacy of self‐help on body shape dissatisfaction. In total, 65% of the participants in the active conditions but no participant in the waitlist control condition reported clinically reliable reductions on BSQ scores. These results all support the previous findings indicating that ACT might be effective for reducing body image dissatisfaction (Fogelkvist et al., 2020; see also Griffiths et al., 2018 for a review) and those suggesting self‐help is a viable option for improving body image (e.g., Jarry & Berardi, 2004). Thus, if these findings can be replicated in further studies with larger sample sizes, ACT‐based self‐help might be considered as an alternative to CBT‐based ones.
For the secondary dimensions, both trials yielded significant time effects. While depression scores decreased over time, satisfaction with life, quality of life, and self‐esteem scores increased, except for the insignificant change in self‐esteem scores in the second trial. Although these positive improvements were consistent with the prior findings pointing out the similar changes in depression and self‐esteem (e.g., Strachan & Cash, 2002; also see Jarry & Berardi, 2004 for a review), we did not find any significant group or interaction effect in the first trial. In other words, the improvements were statistically similar between the waitlist control and the active conditions. Hence, it should be noted that the natural course of general psychological indicators might have caused these improvements.
Regarding the role of facilitator support, contrary to the previous findings suggesting guided self‐help is superior to pure‐self‐help (e.g., Jarry & Ip, 2005), we found no significant difference between the 16‐week guided and pure self‐help conditions. This finding might be associated with two possibilities. First, being in the educational course process, filling measurement tools regularly, and having the researchers’ attention might have resulted in some placebo effects for the pure self‐help group. Second, the possible high quality of the educational course might have hampered the influence of the support or the possible poor quality of it might have led to similar placebo effects in both groups.
Concerning the course duration, no group difference was established between the 16 and 12‐week conditions in terms of the study outcomes. Also, it was found that the dropouts do not change significantly between these conditions. Therefore, it seems possible to achieve similar developments with both 12‐ and 16‐week self‐help. This finding also might be explained by the proximity of course durations preferred in this study; the 4‐week difference between these two conditions might not be enough to elicit a significant change. Thus, considering the findings of Harnet et al. (2010) indicating that more than 20 sessions are essential to achieve a reliable therapy outcome, further studies are suggested to include more variations in terms of the course duration.
Also, the findings showed that the online discussion forum does not increase the effectiveness of self‐help, supporting the findings of previous RCTs (see Barak et al., 2008 for a meta‐analysis). However, it should be kept in mind that the facilitator contact might have diminished functionality of the discussion forum.
Our dropout rates were 23.94% and 40% in the first and the second trials, respectively. Even though these rates were lower than the rate of 53% reported in a similar study (Strachan & Cash, 2002), the difference across the current trials was noteworthy. Two possible reasons might have caused this difference. First, since 12 subjects of the second study had come from the waitlist condition of the first trial, their motivation to receive the course might have decreased over time because of the waiting period. Second, given that relatively more subjects in the discussion forum group (n = 11) as compared to no discussion forum group (n = 6) left the study, the extra time needed for posting messages to the forum might have resulted in more dropouts.
Unlike the second study's findings indicating that the dropouts were random, the results of the first study showed that both lower BMI and depressive symptomatology were predictors of increased likelihood of dropout. This suggests that those with lower BMI and depression scores were less troubled and therefore dropped out to a higher extent. However, given the inconsistency across the findings of the current two studies, it can be suggested that this pattern should be approached with caution.
The current study had some limitations to be considered. First, the sample sizes in both trials were quite small. To reach more reliable findings regarding the efficacy of the course, further studies with larger sample sizes are recommended. Second, the present findings cannot be generalized for men, as all the participants were women. Therefore, further studies with men are needed to explore how the course works for men. Third, since no follow‐up measurement was taken, it is not known whether the improvements lasted after the course completed. Thus, further studies with follow‐ups are suggested to clarify the long‐term effect of the course on body shape dissatisfaction and general psychological health indicators.
Conclusion
Overall, the current findings revealed that the ACT‐based self‐help presented as an educational course might reduce body shape dissatisfaction. However, its effect on general health indicators was not clear. Also, facilitator support, access to an online discussion forum, and longer duration did not increase its effectiveness. Hence, 12‐week self‐help with or without support appears as a viable option for reducing body shape dissatisfaction. However, given the small sample sizes and the dropouts, much more research is essential to draw firm conclusions.
Funding
This study was not funded by any institution. The study was conducted in accordance with Declaration of Helsinki. Online informed consent was obtained from all individual participants included in the study. Ghaderi, A. & Parling, T. authored the self‐help book “Lev med din kropp” that was used in the present studies.
Selvi, K. , Parling, T. , Ljótsson, B. , Welch, E. & Ghaderi, A. (2021). Two randomized controlled trials of the efficacy of acceptance and commitment therapy‐based educational course for body shape dissatisfaction. Scandinavian Journal of Psychology, 62, 249–258.
DATA AVAILABILITY STATEMENT
Data availability: Data are available upon request from the corresponding author.
References
- Aardoom, J. J. , Dingemans, A. E. , Boogaard, L. H. & Van Furth, E. F. (2014). Internet and patient empowerment in individuals with symptoms of an eating disorders: A cross‐sectional investigation of a pro‐recovery focused e‐community. Eating Behaviors, 15, 350–356. [DOI] [PubMed] [Google Scholar]
- Andersson, G. & Titov, N. (2014). Advantages and limitations of internet‐based interventions for common mental disorders. World Psychiatry, 13, 4–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barak, A. , Hen, L. , Boniel‐Nissim, M. & Shapira, N. (2008). A comprehensive review and a meta‐analysis of the effectiveness on internet‐based psychotherapeutic interventions. Journal of Technology in Human Services, 26, 109–160. [Google Scholar]
- Cash, T. F. (1997). The body image workbook: An 8‐step program for learning to like your looks. Oakland, CA: New Harbinger Publications. [Google Scholar]
- Cash, T. F. & Hrabosky, J. I. (2003). The effects of psychoeducation and self‐monitoring in a cognitive‐behavioral program for body‐image improvement. Eating Disorders, 11, 255–270. [DOI] [PubMed] [Google Scholar]
- Cohen, J. (1988). Statistical power analysis for the behavioral sciences (2nd edn). Lawrence Erlbaum Associates. [Google Scholar]
- Cooper, P. , Taylor, M. , Cooper, Z. & Fairburn, C. G. (1987). The development and validation of the Body Shape Questionnaire. International Journal of Eating Disorders, 6, 485–494. [Google Scholar]
- Corp, I. B. M. (2019). IBM SPSS statistics for windows, version 26.0. Armonk, NY: IBM Corp. [Google Scholar]
- Cuijpers, P. , van Straten, A. & Andersson, G. (2008). Internet‐administered cognitive behavior therapy for health problems: A systematic review. Journal of Behavioral Medicine, 31, 169–177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Derogatis, L. R. (1994). Symptom Checklist‐90‐R: Administration, scoring & procedure manual for the revised version of the SCL‐90. Minneapolis, MN: National Computer Systems. [Google Scholar]
- Diener, E. , Emmons, R. A. , Larsen, R. J. & Griffin, S. (1985). The satisfaction with life scale. Journal of Personality Assessment, 49, 71–75. [DOI] [PubMed] [Google Scholar]
- Fairburn, C. G. & Beglin, S. J. (1994). Assessment of eating disorders: Interview or self‐report questionnaire? The International Journal of Eating Disorders, 16, 363–370. [PubMed] [Google Scholar]
- Fairburn, C. G. , Cooper, Z. , Doll, H. A. & Welch, S. L. (1999). Risk factors for anorexia nervosa: Three integrated case‐control comparisons. Archives of General Psychiatry, 56, 468–476. [DOI] [PubMed] [Google Scholar]
- Farrand, P. & Woodford, J. (2013). Impact of support on the effectiveness of written cognitive behavioural self‐help: A systematic review and meta‐analysis of randomised controlled trials. Clinical Psychology Review, 33, 182–195. [DOI] [PubMed] [Google Scholar]
- Fogelkvist, M. , Gustafsson, S. A. , Kjellin, L. & Parling, T. (2020). Acceptance and commitment therapy to reduce eating disorder symptoms and body image problems in patients with residual eating disorder symptoms: A randomized controlled trial. Body Image, 32, 155–166. [DOI] [PubMed] [Google Scholar]
- Fridell, M. , Cesarec, Z. , Johansson, M. & Malling Thorsen, S. (2002). SCL‐90: Svensk normering, standardisering och validering av symtomskalan. Statens institutionsstyrelse, Rapport nr 4/2002. Retrieved from https://www.stat‐inst.se/contentassets/8d7c5ef825a04cb8b5befdfbfbf6fa5a/scl90‐svensk‐normering‐standardisering‐och‐validering‐av‐symtomskalan.pdf. Last Accessed May 22, 2020.
- Frisch, M. B. , Cornell, J. , Villanueva, M. & Retzlaff, P. J. (1992). Clinical validation of the Quality of Life Inventory. A measure of life satisfaction for use in treatment planning and outcome assessment. Psychological Assessment, 4, 92–101. [Google Scholar]
- Garner, D. M. (1997). The 1997 body image survey results. Psychology Today, 30, 30–44. [Google Scholar]
- Ghaderi, A. (2001). Review of risk factors for eating disorders: Implications for primary prevention and cognitive behavioural therapy. Scandinavian Journal of Behaviour Therapy, 30, 57–74. [Google Scholar]
- Ghaderi, A. & Parling, T. (2009). Lev med din kropp: Om acceptans och självkänsla. Stockholm, Sweden: Natur & Kultur Akademisk. [Google Scholar]
- Ghaderi, A. & Scott, B. (2004). The reliability and validity of the Swedish version of the Body Shape Questionnaire. Scandinavian Journal of Psychology, 45, 319–324. [DOI] [PubMed] [Google Scholar]
- Gloud, R. A. & Clum, G. A. (1993). A meta‐analysis of self‐help treatment approaches. Clinical Psychology Review, 13, 169–186. [Google Scholar]
- Griffiths, C. , Williamson, H. , Zucchelli, F. , Paraskeva, N. & Moss, T. (2018). A systematic review of the effectiveness of acceptance and commitment therapy (ACT) for body image dissatisfaction and weight self‐stigma in adults. Journal of Contemporary Psychotherapy, 48, 189–204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haaga, D. A. F. (2000). Introduction to the special section on stepped care models in psychotherapy. Journal of Consulting and Clinical Psychology, 68, 547–548. [PubMed] [Google Scholar]
- Hansen, N. B. , Lambert, M. J. & Forman, E. M. (2002). The psychotherapy dose‐response effect and its implications for treatment delivery services. Clinical Psychology: Science and Practice, 9, 329–343. [Google Scholar]
- Harnett, P. H. , O’Donovan, A. & Lambert, M. J. (2010). The dose response relationship in psychotherapy: Implications for social policy. Clinical Psychologist, 14, 39–44. [Google Scholar]
- Haug, T. , Nordgreen, T. , Öst, L. G. & Havik, O. E. (2012). Self‐help treatment of anxiety disorder: a meta‐analysis and meta‐regression of effects and potential moderators. Clinical Psychology Review, 32, 425–445. [DOI] [PubMed] [Google Scholar]
- Hayes, S. C. , Luoma, J. B. , Bond, F. W. , Masuda, A. & Lillis, J. (2006). Acceptance and commitment therapy: Model, processes and outcomes. Behaviour Research and Therapy, 44, 1–25. [DOI] [PubMed] [Google Scholar]
- Heck, R. H. , Thomas, S. & Tabata, L. (2014). Multilevel and longitudinal modeling with IBM SPSS. New York: Routledge. [Google Scholar]
- Hirai, M. & Clum, G. A. (2006). A meta‐analytic study of self‐help interventions for anxiety problems. Behavior Therapy, 37, 99–111. [DOI] [PubMed] [Google Scholar]
- Houston, T. K. , Cooper, L. A. & Ford, D. E. (2002). Internet support groups for depression: A 1‐year prospective cohort study. The American Journal of Psychiatry, 159, 2062–2068. [DOI] [PubMed] [Google Scholar]
- Howard, K. I. , Kopta, S. M. , Krause, M. S. & Orlinsky, D. E. (1986). The dose‐effect relationship in psychotherapy. American Psychologist, 41, 159–164. [PubMed] [Google Scholar]
- Hrabosky, J. I. & Cash, T. F. (2007). Self‐help treatment for body‐image disturbances. In Latner J. D. & Wilson G. T. (Eds.), Self‐help approaches for obesity and eating disorders: Research and practice (pp. 118–138). New York: The Guilford Press. [Google Scholar]
- Jacobson, N. S. & Truax, P. (1991). Clinical significance: A statistical approach to defining meaningful change in psychotherapy research. Journal of Consulting and Clinical Psychology, 59, 12–19. [DOI] [PubMed] [Google Scholar]
- Jarry, J. L. & Berardi, K. (2004). Characteristics and effectiveness of stand‐alone body image treatments: A review of the empirical literature. Body Image, 1, 319–333. [DOI] [PubMed] [Google Scholar]
- Jarry, J. L. & Ip, K. (2005). The effectiveness of stand‐alone cognitive‐behavioral therapy for body image: A meta‐analysis. Body Image, 2, 317–331. [DOI] [PubMed] [Google Scholar]
- Kendal, S. , Kirk, S. , Elvey, R. , Catchpole, R. & Prymachuk, S. (2017). How moderated online discussion forum facilitates support for young people with eating disorders. Health Expectations, 20, 98–111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim, D. S. (2009). Body image dissatisfaction as an important contributor to suicidal ideation in Korean adolescents: Gender difference and mediation of parent and peer relationships. Journal of Psychosomatic Research, 66, 297–303. [DOI] [PubMed] [Google Scholar]
- Kostanski, M. & Gullone, E. (1998). Adolescent body image dissatisfaction: Relationships with self‐esteem, anxiety, and depression controlling for body mass. Journal of Child Psychology and Psychiatry, 39, 255–262. [PubMed] [Google Scholar]
- Mancuso, S. G. (2016). Body image inflexibility mediates the relationship between body image evaluation and maladaptive body image coping strategies. Body Image, 16, 28–31. [DOI] [PubMed] [Google Scholar]
- Neumark‐Sztainer, D. , Wall, M. M. , Story, M. & Perry, C. L. (2003). Correlates of unhealthy weight‐control behaviors among adolescents: Implications for prevention programs. Health Psychology, 22, 88–98. [DOI] [PubMed] [Google Scholar]
- Pearson, A. , Heffner, M. & Follette, V. (2010). Acceptance and commitment therapy for body image dissatisfaction: A practitioner’s guide to using mindfulness, acceptance, and values‐based behavior change strategies. Oakland, CA: New Harbinger Publications Inc. [Google Scholar]
- Rosenberg, M. (1965). Society and the adolescent self‐image. Princeton, NJ: Princeton University Press. [Google Scholar]
- Sandoz, E. K. , Wilson, K. G. & Dufrene, T. (2011). Acceptance and commitment therapy for eating disorders: A process‐focused guide to treating anorexia nervosa and bulimia. Oakland, CA: New Harbinger Publications. [Google Scholar]
- Stewart, T. M. (2004). Light on body image treatment: Acceptance through mindfulness. Behavior Modification, 28, 783–811. [DOI] [PubMed] [Google Scholar]
- Stice, E. (2002). Risk and maintenance factors for eating pathology: A meta‐analytic review. Psychological Bulletin, 128, 825–848. [DOI] [PubMed] [Google Scholar]
- Stice, E. , Hayward, C. , Cameron, R. P. , Killen, J. D. & Taylor, C. C. (2000). Body‐image and eating disturbances predict onset of depression among female adolescents: A longitudinal study. Journal of Abnormal Psychology, 190, 438–444. [PubMed] [Google Scholar]
- Stice, E. & Shaw, H. E. (2002). Role of body dissatisfaction in the onset and maintenance of eating pathology: A synthesis of research findings. Journal of Psychosomatic Research, 53, 985–993. [DOI] [PubMed] [Google Scholar]
- Strachan, M. D. & Cash, T. F. (2002). Self‐help for a negative body image: A comparison of components of a cognitive‐behavioral program. Behavior Therapy, 33, 235–251. [Google Scholar]
- Svanborg, P. & Åsberg, M. (1994). A new self‐rating scale for depression and anxiety states based on the Comprehensive Psychopathological Rating Scale. Acta Psychiatrica Scandinavica, 89, 21–28. [DOI] [PubMed] [Google Scholar]
- Tiggemann, M. (2005). Body dissatisfaction and adolescent self‐esteem: Prospective findings. Body Image, 2, 129–135. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data availability: Data are available upon request from the corresponding author.


