Abstract
Background
Using a controlled trial, this study aimed to evaluate the effectiveness of adhesive strapping to improve the natural healing rate of umbilical hernia.
Methods
This prospective, observational study included 128 patients from Kumamoto, Japan (97 in the adhesive strapping group, and 31 in observation group), from 2012–2015. The duration from first hospital visit to the hernia orifice closure was compared between the two groups.
Result
Kaplan‐Meier curves showed that the probability of umbilical hernia in the adhesive strapping group was lower until approximately 200 days, but it was not statistically significant in the log rank test. According to multivariate Cox proportional hazard models, the hazard risk of umbilical hernia in the adhesive strapping group was significantly higher within 0–60 days after adjusting for confounding factors such as hernial cavity and hernia orifice area (P < 0.0001).
Conclusion
Adhesive strapping of umbilical hernia was significantly associated with earlier closure of the hernia orifice from baseline until at least 60 days.
Keywords: adhesive strapping, umbilical hernia
Key Notes.
This study aimed to evaluate the effectiveness of adhesive strapping to improve the natural healing rate of umbilical hernia using a controlled trial.
Adhesive strapping of umbilical hernia was significantly associated with earlier closure of the hernia orifice from baseline until at least 60 days.
Umbilical hernias in infants are caused by incomplete fascial closure of the umbilical ring, resulting in protrusion of intra‐abdominal organs. 1 They occur in 10‒20% of infants at birth and are more common in preterm infants (75% of those weighing <1,500 g). 2 , 3 The incidence of umbilical hernia increases with a disease state such as trisomy 21. 2 , 3 The majority of umbilical hernias spontaneously close during the first 3 years of life. 4 In Japan, the frequency of spontaneous closure is reported to be 80% in children aged <1 year and 90% in children aged <2 years. 5
Adhesive strapping of the hernias has been found to be generally ineffective. However, in Japan, Oshio et al. reported that adhesive strapping was more effective than the conservative observation method. 6 Hence, many physicians in Japanese clinics started to use adhesive strapping as a treatment for infantile umbilical hernia. However, few epidemiological controlled studies on the usefulness of adhesive strapping have been conducted to date. This study, therefore, aimed to clarify, in a controlled trial, the effectiveness of adhesive strapping to improve the natural healing rate of umbilical hernias.
Methods
This multi‐institutional, prospective study enrolled patients who visited our clinics in Kumamoto, Japan because of umbilical hernia from June 2012 to June 2015. Patients aged ≤6 months during their first visit were included in the study; those with trisomy 21, hypothyroidism, muscle disease, congenital heart disease, hypospadias, spina bifida, meningocele, and mucopolysaccharidosis, were excluded. We also excluded patients with birthweight of <1,500 g. At the first visit, the following clinical information was obtained through interviews: age, sex, presence or absence of a twin, and family history. Date of birth, gestational age, birthweight, birth height, and birth method were recorded using the Maternal and Child Health Handbook, provided to every pregnant woman by the Ministry of Health and Welfare of Japan. The length, width and height of each hernia were measured using a scale. The length and width of the hernia orifice were measured by estimating its relationship to the width of the examiner's inserted index finger. The capacity of the umbilical hernia was represented as the product of the length, width and height of the hernia, and the area of hernia orifice was represented as the product of the length and width of the hernia orifice. After we explained the method and risk of adhesive strapping to the patient's family, they were asked to select the course of treatment, namely, only observation or adhesive strapping. Adhesive strapping was performed in the following manner. First, the umbilical mass was pushed into the abdominal cavity using a fingertip. Next, a ball of gauze or cotton wool matching the size of the hernia was inserted into the hernial sac. The skin over the abdominal rectus muscles was drawn over the hernia and fixed in place using an elastic adhesive plaster. Next, a transparent film dressing that had been cut slightly larger than the adhesive plaster was placed on the umbilicus to make the area waterproof. The adhesive plaster was changed every week. A hernia orifice was considered closed if there was no protrusion on removing the strap. When the hernia orifice was closed, the closure was reconfirmed within 4 weeks. When the skin was irritated by the plaster, adhesive strapping was terminated for a few days until the skin redness improved. In the observation group, the umbilical hernia was assessed during the patients' visit to our clinics for vaccination or routine health checkups. In both groups, patients with an unclosed umbilical hernia were followed up to 2 years old. At 2 years old, the presence or absence of an umbilical hernia was reconfirmed at a hospital visit or through telephone interviews with the family.
Written informed consent was obtained from the families of all the patients. The study was approved by the institutional review board of the Japan Pediatric Association.
The Fisher's exact test was used to compare categorical variables between the study groups, and the two‐tailed, unpaired t‐test, or the Wilcoxon rank‐sum test was used to compare continuous variables. The time of hernia orifice closure was determined using the Kaplan–Meier method with comparisons between curves based on log rank chi‐squared statistics. Univariate Cox proportional hazard analyses were used to examine the association of the variables with the time of hernia orifice closure. Variables with significant associations on univariate analyses were considered candidates for multivariate Cox proportional hazard analysis. All analyses were conducted using SAS statistical software, version 12 (SAS Institute Inc., Cary, NC, USA). A P‐value of <0.05 was considered statistically significant.
Result
Over a 35‐month period, (June 2012–June 2015) 133 patients were assessed for eligibility, and 130 were enrolled in the trial: 99 in the adhesive strapping group and 31 in the observation group. In the adhesive strapping group, two patients were excluded: one because of missing data and the other because he was not operated on until 2 years old. Thus, 97 patients were included in the adhesive group (Fig 1).
Fig. 1.
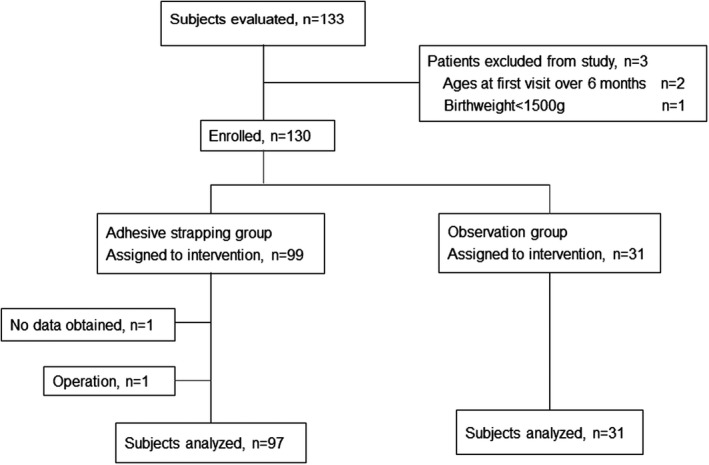
Participant flow chart.
Baseline characteristics in the adhesive strapping and observation group during the first clinic visit are shown in Table 1. The mean of area of the hernia orifice was significantly larger among patients in the observation group. No significant differences in sex, age, gestational age, birthweight, birth length, and hernia capacity were observed between the two groups.
Table 1.
Baseline characteristics of group subjects
| Variable | Adhesive strapping (n = 99) | Observation (n = 31) | P ‐value |
|---|---|---|---|
| Male, n (%) | 58 (59) | 15 (48) | 0.41 |
| Age (months) | 1.7 ± 0.7 | 1.9 ± 00.9 | 0.22 |
| Gestational age (day), | 269.9 ±10.8 | 266.0 ± 12.5 | 0.17 |
| Birthweight (g), | 2,905.1 ± 418.5 | 2,818.0 ± 560.5 | 0.35 |
| Birth length (cm), | 49.0 ± 2.1 | 48.5 ±2.5 | 0.28 |
| Capacity of hernia (cm3), ✝ | 8.5 ± 8.5 | 6.8 ±5.3 | 0.88 |
| Area of hernia orifice (cm2), ǂ | 1.2 ± 1.1 | 1.8 ± 1.0 | 0.0004 |
Values are mean ± SD, except where otherwise indicated.
Capacity of hernia indicates width (cm) × length (cm) × height (cm) of umbilical hernia.
Area of hernia orifice indicates width (cm) × length (cm) of hernia orifice.
Kaplan‐Meier curves for probability of umbilical hernia in the observation and adhesive strapping group are shown in Figure 2. Until about 200 days, the adhesive strapping group had fewer probability of umbilical hernia. Kaplan–Meier estimates for the median time from the start to middle levels of probability were 55 days in the adhesive strapping group and 107 days in the observation group. However, the probability difference of umbilical hernia between the two groups was not statistically significant using the log rank test.
Fig. 2.
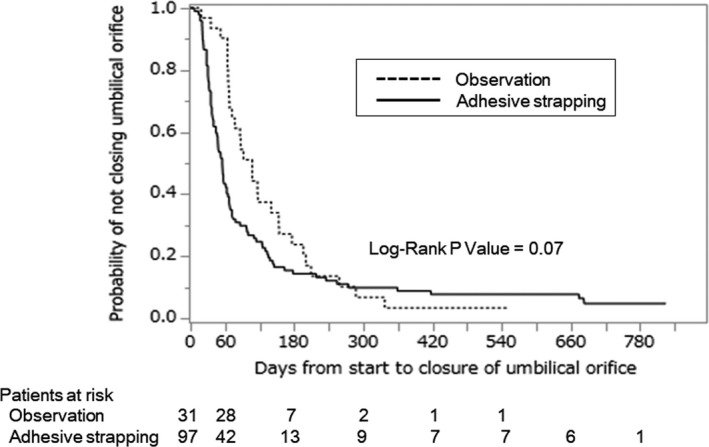
Kaplan‐Meier curve relating adhesive strapping to time to closure of hernia orifice. ‐‐‐; observation; –, adhesive trapping.
To analyze variables that may have influenced the probability of umbilical hernia, univariate Cox proportional hazard analyses were used (Table 2). The hernial capacity, the area of the hernia orifice, and the adhesive strapping group significantly influenced within 0‒60, 0‒120, and 0‒180 days. The hernial capacity and the area of the hernia orifice were negatively associated with the probability of umbilical hernia, and the hazard ratio in the area of the hernia orifice was lower than that in the hernial capacity.
Table 2.
Cox proportional hazards analyses of time to closure of hernia orifice with variables (unadjusted analyses; n = 128)
| Variable | 0 – 60 days | 0 – 120 days | 0 – 180 days | |||
|---|---|---|---|---|---|---|
| HR (95% CI) | P‐value | HR (95% CI) | P ‐value | HR (95% CI) | P ‐value | |
| Gender (male/female) | 1.07 (0.64-1.82) | 0.79 | 1.25 (0.83-1.91) | 0.28 | 1.28 (0.88-1.89) | 0.20 |
| Age(months) | 1.00 (0.19-4.47) | 1.00 | 0.92 (0.26-2.89) | 0.89 | 0.81 (0.26-2.29) | 0.70 |
| Gestational age (days) | 1.82 (0.50-7.35) | 0.37 | 1.70 (0.63-4.82) | 0.30 | 1.36 (0.56-3.51) | 0.51 |
| Birthweight (g) | 1.15 (0.32-4.30) | 0.83 | 0.76 (0.28-2.03) | 0.58 | 0.70 (0.29-1.73) | 0.44 |
| Birth length (g) | 2.18 (0.50-10.15) | 0.30 | 1.06 (0.34-3.50) | 0.92 | 0.95 (0.33-2.87) | 0.93 |
| Capacity of hernia | 0.04 (0.004-0.31) | 0.0009 | 0.09 (0.018-0.35) | 0.0002 | 0.24 (0.07-0.71) | 0.008 |
| Area of hernia orifice | 0.0009 (0.00002-0.02) | <0.0001 | 0.003 (0.0002-0.02) | <0.0001 | 0.02 (0.002-0.10) | <0.0001 |
| Adhesive strapping | 7.99 (2.95-32.81) | <0.0001 | 1.81 (1.12-3.04) | 0.014 | 1.76 (1.13-2.82) | 0.011 |
CI, confidence interval; HR, hazard ratio.
Multivariate Cox proportional hazard analyses were used to analyze whether the adhesive strapping group had a significantly higher probability of umbilical hernia. The hernial capacity and the area of the hernia orifice were used confounding factors. Results were shown in Table 3. Adjusted for the hernial capacity and the area of hernia orifice, the hazard ratio in the adhesive strapping group was significantly higher only within 0‒60 days and not within 0‒120 or 0‒180 days.
Table 3.
Cox proportional hazards analyses of time to closure of hernia orifice among patients with adhesive strapping (n = 128)
| Model | 0 – 60 days | 0 – 120 days | 0 – 180 days | |||
|---|---|---|---|---|---|---|
| HR (95% CI) | P ‐value | HR (95% CI) | P ‐value | HR (95% CI) | P ‐value | |
| Unadjusted | 7.99 (2.95-32.81) | <0.0001 | 1.81 (1.12-3.04) | 0.014 | 1.76 (1.13-2.82) | 0.011 |
| Adjusted for capacity of hernia and area of hernia orifice | 6.54 (2.33-27.34) | <0.0001 | 1.36 (0.81-2.36) | 0.25 | 1.41 (0.87-2.35) | 0.16 |
CI, confidence interval; HR, hazard ratio.
In the adhesive strapping group, skin complications, such as skin redness and exudation, occurred in 40/97 (41.2%) of patients. These complications were relatively mild and we could restart the adhesive strapping after several days of rest or by applying a steroid ointment. In both groups, no other serious complications occurred.
Discussion
To the best of our knowledge, this is the first prospective, controlled, multi‐institutional study to analyze the effectiveness of adhesive strapping to improve the natural healing rate of umbilical hernias. This study shows that closure of the hernia orifice in the adhesive strapping group was significantly earlier, up to at least 60 days, than that in the observation group.
From the 1950s to 1960s, there was controversy over whether adhesive strapping affects the natural healing rate of umbilical hernias. Haworth demonstrated that adhesive strapping hastened the time of disappearance of umbilical hernia more efficiently, especially of large hernias (hernial protrusion size >6 mm), or of the large hernia orifice (orifice size >6 mm). 7 Conversely, Karlström concluded that no difference in the healing tendency of hernias between the adhesive strapping and observation groups could be established. 8 Because of the lack of epidemiological evidence, in Europe and America adhesive strapping is considered to have no beneficial effect. 9
In Japan, Oshio et al. in their prospective study compared the healing rate of umbilical hernia at 6 months between two institutions. Patients with a hernia in one institute were only observed and those in the other were treated with adhesive strapping. At 6 months, the healing rate in the observation group was 45.8% and that in the adhesive strapping group was 100%. They concluded that this difference was statistically significant and that adhesive strapping was effective. 6 After the publication of this report, several studies published in Japan showed the effectiveness of adhesive strapping as a natural treatment method for umbilical hernias. 5 , 10
Our study added several new findings to these studies. First, as depicted in Figure 2, Kaplan–Meier curves for the probability of umbilical hernia showed early closure of hernia orifice in the adhesive strapping group until approximately 200 days, which was not statistically significant. Second, to minimize the effect of confounding factors, multivariate analysis was performed. In general, umbilical hernias spontaneously disappear in most cases. 4 The size of hernia orifice and hernia sac are reported to be correlated with the time of disappearance of the hernia. 11 In this report, the area of hernia orifice and hernial capacity were negatively associated with the probability of umbilical hernia according to the univariate Cox proportional hazard analyses. Therefore, the area of hernia orifice and hernial capacity were considered as confounding factors in evaluating the effectiveness of adhesive strapping in improving the natural healing rate using multivariate Cox proportional hazard analyses. After adjustment, adhesive strapping was still significantly associated with the closure of the hernia orifice within 0‒60 days.
This study was conducted in multi‐institutional setting, where nearly all research members were pediatricians employed in clinics. Previous studies published in Japan after 2000 were mainly conducted by pediatric surgeons in general hospitals. 5 , 6 , 10 Hence, patients with an umbilical hernia who visited the general hospital were thought to have more severe disease than those who visited the clinical office. We think that our research targeted patients with more general umbilical hernias rather than special ones.
This study has two limitations. First, the width and length of the hernia orifice were measured relative to the size of examiner's inserted index finger. Because this method tends to be arbitrary, ultrasonography may more accurately measure the size of the hernia orifice. Second, the target patients of this research were Japanese. As the incidence of umbilical hernia is influenced by race, more studies in other countries will be needed to apply our results universally.
In conclusion, adhesive strapping was significantly associated with early closure of hernia orifice during the initial visit until at least 60 days according to multivariate Cox proportional hazard analyses.
Disclosure
The authors declare no conflict of interest.
Author contributions
A.K. designed the study and wrote the manuscript. T.M., Y.M., Y.S., E.S., T.O., T.K., K.E. and Y.H. collected and analyzed data. All authors read and approved the final manuscript.
Acknowledgment
The authors thank Prof. Koichiro Usuku, MD, PhD, (Kumamoto Medical University Hospital, Kumamoto, Japan) for his critical comments and suggestions regarding statistical analysis.
References
- 1. Cresson SL, Pilling GP. Lesions about the umbilicus in infants and children. Pediatr. Clin. North Am. 1959; 6: 1085–116. [Google Scholar]
- 2. Snyder CL. Current management of umbilical abnormalities and related anomalies. Semin. Pediatr. Surg. 2007; 16: 41–9. [DOI] [PubMed] [Google Scholar]
- 3. Meier AH, Richetts RR. Surgical complications of inguinal and abdominal wall hernias. Semin. Pediatr. Surg. 2003; 12: 83–8. [DOI] [PubMed] [Google Scholar]
- 4. Cilley RE. Disorders of the umbilicus. In: Coran AG (ed). Pediatric Surgery, 7th edn. Elsevier Saunders, Philadelphia, 2012; 961–72. [Google Scholar]
- 5. Hayashida M, Shimozono T, Meiri S et al. Umbilical hernia: Influence of adhesive strapping on outcome. Pediatr. Int. 2017; 59: 1266–9. [DOI] [PubMed] [Google Scholar]
- 6. Oshio T, Hino M, Oshita M, Hinoki T, Gotoh T, Akiyama T. Comparison of outcomes between the conservative observation and the adhesive strapping for infantile umbilical hernia: A prospective study. J. Jpn. Soc. Pediatr. Surg. 2002; 38: 768–74. [Google Scholar]
- 7. Haworth JC. Adhesive strapping for umbilical hernia in infants, clinical trial. Br. Med. J. 1956; 2: 1286–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Karlströme F. Should infantile umbilical hernias be treated with navel emplastra? J. Pediatr. 1961; 59: 87–9. [DOI] [PubMed] [Google Scholar]
- 9. Carlo WA, Ambalavanan N. The umbilicus. In: Kliegman RM (ed). Nelson Textbook of Pediatrics, 20th edn. Elsevier, Philadelphia, 2016; 890–1. [Google Scholar]
- 10. Yanagisawa S, Kato M, Oshio T, Morikawa Y. Reappraisal of adhesive strapping as treatment for infantile umbilical hernia. Pediatr. Int. 2016; 58: 363–8. [DOI] [PubMed] [Google Scholar]
- 11. Heifetz CJ. Observations on the disappearance of umbilical hernias of infancy and childhood. Surg. Gynecol. Obstet. 1963; 116: 469–73. [PubMed] [Google Scholar]


