Abstract
Aim
To determine which factors other than child age play a role in the division and transfer of diabetes care responsibilities between parents and children with type 1 diabetes.
Design
Qualitative focus group study.
Methods
Across four sites in the Netherlands, 18 parents (13 mothers) of children (9–14 years) with type 1 diabetes participated in four focus groups in 2015–2016, as part of the research project 'Whose diabetes is it anyway?'. Qualitative content analysis and the constant comparison method were used to analyse the data.
Results
According to parents, the transfer process included both direct and indirect tasks, had different levels (remembering, deciding, performing), was at times a difficult and stressful process, and showed large variation between families. A large number of child, parent and context factors were identified that affected the division and transfer of diabetes care responsibilities according to parents. Both positive and negative consequences of the transfer process were described for parental and child health, behaviour and well‐being. Parental final evaluations of the division and transfer of diabetes care responsibilities appeared to be dependent on parenting values.
Conclusion
How families divide and transfer diabetes care tasks appeared to be affected by a complex interplay of child, parent and context characteristics, which had an impact on several parent and child domains.
Impact
Parents struggle with the right timing of transfer, which calls for more support from diabetes nurses. The identified factors can be used as input for integrating a more family‐based approach into current age‐based guidelines, to improve regular care.
Keywords: child, diabetes mellitus, nursing, parents, self care, transfer, type 1
摘要
目的
确定除儿童年龄外, 哪些因素可能对父母和患有1型糖尿病的儿童的糖尿病护理责任划分和转移产生影响。
设计
定性焦点小组研究。
方法
2015‐2016年间, 在荷兰境内四地展开研究, 研究对象为18名患有1型糖尿病的儿童 (9‐14岁) 的父母 (13名母亲) , 共分为四个重点小组, 此类研究作为‘谁患有糖尿病’研究项目的一部分。此外, 采用定性含量分析法和持续比较法对数据进行分析。
结果
父母表示, 转移过程中, 需执行不同难度的直接和间接任务 (记忆、决定、执行) , 部分情况下, 面临较大困难和压力, 并且, 不同家庭的差异较大。经确定, 大量儿童、父母和背景因素可能对糖尿病护理责任的划分和转移造成影响。现已对转移过程对父母和儿童健康、行为和幸福的积极和消极后果进行描述。父母对糖尿病护理责任划分和转移的最终评估取决于其价值观。
结论
家庭分配和转移糖尿病护理责任的方式似乎与儿童、父母及背景特征的复杂作用相关, 而此类作用对父母和儿童均有一定程度的影响。
影响
父母忙于确定准确的转移时间, 因此, 糖尿病护士需予以更多支持。可考虑此类已确定的因素, 以便将更多家庭方法整合至现有基于年龄的指南中, 从而改善常规护理。
1. INTRODUCTION
Most young people with type 1 diabetes are not yet able to successfully manage the condition on their own given the magnitude of tasks (Coffen, 2009) and the appeal on still developing abilities. These include higher‐level cognitive skills (e.g., planning, numeracy, problem solving) (Scott, 2013), fine motor skills (e.g., performing finger prick, changing pump infusion site) (Markowitz et al. 2015), and self‐control and emotion processing skills (e.g., managing disappointment or fear to prevent diabetes care avoidance) (Hughes et al. 2012). Therefore, parents play an important role in the child's diabetes care long after diagnosis. Over time, parents transfer diabetes care responsibilities to their children. However, families often struggle to determine the right timing of transfer (Akre & Suris, 2014). Transferring responsibilities while the child is not ready can result in suboptimal diabetes self‐care (Wiebe et al. 2014) and higher HbA1c (Helgeson et al. 2008). Transferring responsibilities too late can deprive the child of learning opportunities and hamper independence (Reed‐Knight et al. 2014).
2. BACKGROUND
Several guidelines describe at which age or developmental stage children can be expected to master diabetes care responsibilities including diabetes‐specific tasks, knowledge and skills (American Diabetes Association, 2018; de Boer et al. 2012; Kinder Diabetes Centrum Nijmegen, 2020; Lange et al. 2014; Markowitz et al. 2015; Scott, 2013). Most guidelines recommend that over time, parental responsibilities should shift to responsibilities that are shared between parents and children, before the child bears sole responsibility. This process can start around the age of 4–5 years with the child's involvement in daily blood glucose management (e.g., performing fingerprick, administer insulin). Although cross‐sectionally increasing age has been related to more child responsibility for diabetes care tasks in several studies (Robinson et al. 2011; Wiebe et al. 2005), variability is observed in the timing of transfer between families of children of the same age (King et al. 2014). Furthermore, in some longitudinal analyses age was not related to declines in parental involvement over time (age at enrolment 10–14 years, 2.5‐year follow‐up with half year assessment) (King et al. 2014; Wiebe et al. 2014). This suggests that, apart from age, there are other factors playing a role in this process.
Accordingly, previous questionnaire studies indicated that the division of diabetes care tasks was, for example, related to the ranking of general and diabetes‐specific parenting goals (Robinson et al. 2011), parenting behaviours (e.g., monitoring) (Berg et al. 2011; Pate et al. 2019) and age at diabetes diagnosis (Wiebe et al. 2005). However, results of existing studies often vary in terms of significance and the direction of the effect, hampering a straightforward interpretation of the quantitative literature (Helgeson et al. 2008; Robinson et al. 2011; Wiebe et al. 2005, 2014). Furthermore, quantitative studies examine associations on a group level, and as a consequence may average out factors that are relevant to certain families. Qualitative research provides a deeper understanding of complex and dynamic processes by eliciting what is important from the population of interest itself on an individual level, which may help clinicians to provide more family‐tailored support and researchers to formulate new hypotheses (Gelo et al. 2008). However, the few qualitative studies in this area (Newbould et al. 2008; Olinder et al. 2011; Schilling et al. 2006; Williams, 1999) were limited to a specific set of predefined tasks (Newbould et al. 2008; Olinder et al. 2011), only described the division of care responsibilities (Schilling et al. 2006), focused on the impact of only one factor (i.e., sex) (Williams, 1999), or combined the experiences of youth with asthma and diabetes and their parents (Newbould et al. 2008).
3. THE STUDY
3.1. Aims
Available recommendations to guide families in the transfer process are currently based on the child's age, while age differences and factors beyond the child's age have been documented in prior studies. With the ultimate goal of complementing these age‐based guidelines with family‐tailored advice, the primary aim of the present focus group study was to comprehensively examine which factors play a role in the division and transfer of diabetes care responsibilities from a parental point of view. To understand the broader context, it was also examined what parents considered as relevant diabetes care tasks; how responsibilities were divided between parents and children; and how parents experienced the current division of responsibilities and the transfer process so far.
3.2. Design
This qualitative focus group study is part of the larger multi‐method research project ‘Whose diabetes is it anyway?’ among parents and children with type 1 diabetes from three Dutch general hospitals (Catharina Hospital Eindhoven, Elisabeth‐TweeSteden Hospital Tilburg, Jeroen Bosch Hospital ‘s‐Hertogenbosch) and specialized diabetes centres (Diabeter Deventer, Rotterdam and Veldhoven).
3.3. Sample/Participants
Families were excluded in case of diabetes duration <6 months, insufficient command of the Dutch language or severe child intellectual disabilities that made future fully independent child responsibility impossible (based on the judgement of the diabetes care team), or if families already participated in research or previously indicated no interest in participating in research projects. To maximize sample diversity, only one parent per family was invited; invitations were randomly addressed to mothers or fathers. For the present analyses, focus group data of parents of a child aged 9–14 years was used. These parents were recruited from Catharina Hospital, Elisabeth‐TweeSteden Hospital, and Diabeter Rotterdam‐Veldhoven.
Focus groups were separately organized for parents with a child aged 9–11 years (primary school) or 12–14 years (secondary school). This age‐group was selected as it was expected that most care tasks were transferred in response to increased cognitive and physical maturity and the transition from primary to secondary school. Selected parents received information about the study, a written informed consent form and a pre‐stamped return envelope. Enrolled parents were contacted by phone to plan a focus group meeting when at least three parents per hospital/centre in a specific age‐group agreed to participate. When less than three participants per hospital/centre gave informed consent, families who did not reply to the invitation were contacted by telephone to verify their interest. If the randomly selected parent indicated during the phone call that he/she did not want to participate, the other parent was invited for study participation. For one focus group, parents from two different centres/hospitals were combined. Eligible families were invited to participate until data saturation was reached (i.e., no new themes were identified, based on constant comparison) (Boeije, 2002; Onwuegbuzie et al. 2009). Of the 108 contacted families, 26 parents of 25 families initially gave informed consent. In total, 18 parents of 17 families actually participated and 8 parents dropped out (no show: N = 2; not available on planned date: N = 5; not enough participants: N = 1). For one family, both parents participated.
3.4. Data collection
In total, four focus groups were organized at the participating centres from July 2015 to November 2016; duration varied between 90 and 120 min. Group size ranged from three to six parents (i.e., children were not present). Parents completed a questionnaire about sociodemographic and family characteristics, including parental age, ethnic background, educational level, employment status, and family composition. Employment status, background and education were subsequently categorized into, respectively, having versus not having a paid job, non‐Dutch/mixed versus Dutch background and high (i.e., university) versus medium‐low educational level. Child demographics and clinical data at the focus group data were extracted from medical records.
All focus group meetings were chaired by the first author (PhD student, MSc in medical psychology, relevant research training) and an observer (GN, EH or undergraduate psychology student) who did not participate in the discussion but made field notes. Both the moderator and observer were not known to participants. A script was used to guide the meeting (Table 1), including a pre‐defined set of potential diabetes care tasks composed in collaboration with health care professionals (HJA, PW) and containing tasks about glucose management, general health and social life. First, the moderator asked parents which tasks they distinguished in the diabetes care of their child. Parents were asked their opinion about unmentioned activities from the predefined list. Second, after completing VAS‐scales about who remembered doing a particular task ('thinking about'), who made the decision ('deciding'), and who actually performed the task ('doing'), parents provided an overall indication of the current division of diabetes care responsibilities between parent and child. Third, parents were asked to indicate whether they were satisfied with this division. Fourth, parents were asked to elaborate their ideas about what helped them or their child and what made it difficult to transfer diabetes responsibility. Finally, parents were asked what they would retrospectively change in their approach in transferring diabetes care responsibilities to their child, or which approach they would recommend to other families.
TABLE 1.
Overview of questions during the focus group meetings
| Question | |
|---|---|
| Opening questions |
|
| Introductory question |
Tasks were listed by the moderator. When certain tasks of the predefined list were not mentioned by parents, these tasks were discussed. For the tasks that were listed, parents mapped the current division of diabetes care tasks in their family on a VAS scale in the domains 'remembering', 'deciding' and 'performing' (range: always parent to always child) |
| Introductory question |
Parents were supported to discuss similarities and differences |
| Transition question |
|
| Key question |
|
| Transition question |
|
| Key question |
|
| Ending questions |
Relevant information that was discussed during the focus groups was summarized by the moderator
|
3.5. Ethical considerations
The Ethical Review Board of Tilburg University approved this study (EC 2015.02).
3.6. Data analysis
Data collection and analysis were performed simultaneously. Qualitative content analysis and the constant comparison method were used to analyse the data (Boeije, 2002; Cho & Lee, 2014). For each research question, a separate coding scheme was developed, resulting in four coding schemes about (a) relevant diabetes care tasks, (b) the current division of diabetes care responsibilities between parents and children, (c) parental experiences about the current division of responsibilities and the transfer process so far and (d) child, parent and context factors affecting the division and transfer of diabetes care responsibilities. Relevant responses were labelled per research question by using colour coding in MS Word. For the first transcript, open coding was used to code different responses (Barbour, 2001). Then, codes were compared and grouped into categories (axial coding). Next, categories were grouped into a hierarchical structure (selective coding) (Boeije, 2002; Onwuegbuzie et al. 2009). Based on these preliminary coding schemes, the other transcripts were coded. When codes, themes or hierarchical structures were added or revised, analyses of already coded focus groups were updated. MS Visio was used to visualize the data. To examine age‐group differences, themes emerging from focus groups of parents with children aged 9–11 years and aged 12–14 years were compared.
3.7. Validity and reliability/Rigour
Audio recordings of all focus group meetings were transcribed by research assistants and checked by JA. For the first transcript, JA and GN independently coded responses. Other coding steps by JA were checked by GN or EH. Throughout the analysis, coding disagreements were solved by discussion (Barbour, 2001; Boeije, 2002; Onwuegbuzie et al. 2009).
4. FINDINGS
Characteristics of the 18 participating parents (mothers N = 13) and their families are presented in Table 2. Diabetes duration ranged from 2 to 14 years. Over half of the children had an HbA1c above the recommended target (N = 9, HbA1c ≥ 7.5%/58 mmol/mol (8); N = 14 had an HbA1c ≥ 7.0%/53 mmol/mol (DiMeglio et al. 2018). With regard to family characteristics, most children grew up in an intact family (N = 14) and in all families both biological parents were working.
TABLE 2.
Characteristics of parents participating in the focus groups (N = 18)
| N (%) | Mean (SD) | Range | |
|---|---|---|---|
| Parent sociodemographics (N = 18) | |||
| Age, years | 45.4 (4.5) | 37–52 | |
| Sex, female | 13 (72) | ||
| Ethnic background, non‐Dutch or mixed ethnic background | 2 (11) a | ||
| Education, high educational level | 11 (61) | ||
| Employment status, paid job | 18 (100) | ||
| Child characteristics (N = 17) b | |||
| Age child, years | 12.6 (1.9) | 9.8–15.3 | |
| Sex, girl | 11 (65) | ||
| Education child, secondary school | 9 (53) | ||
| Treatment, insulin pump | 16 (94) | ||
| CGM use as reported in the child's medical record, yes c | 4 (29) | ||
| Age at diabetes onset, years | 6.9 (3.6) | 0.9–12.4 | |
| Diabetes duration, years | 5.8 (3.2) | 2.2–14.3 | |
| Most recent HbA1c value, % | 7.8 (1.0) | 6.5–10.2 | |
| Most recent HbA1c value, mmol/mol | 61.7 (10.4) | 48–88 | |
| Comorbidity d , yes | 3 (18) | ||
| Family characteristics (N = 17) b | |||
| Family composition, biological parents live together | 14 (82) | ||
| Number of siblings | 1.12 (0.6) | 0–2 | |
| Employment status parents, both parents are working | 17 (100) | ||
| Educational level parents, both parents are highly educated | 8 (47) | ||
| Ethnic background parents, both parents have a non‐Dutch or mixed ethnic background | 2 (12) | ||
Both participants reported a mixed ethnic background including Dutch
For one family both parents participated
CGM = Continuous Glucose Monitoring (e.g., sensor or scanner), N = 14 as for 3 children information about sensor use could not be obtained from the child's medical record
Comorbidities included autism, lipoatrophy, celiac disease and hypothyroidism
The most important findings per research question are presented in Figure 1 and outlined below.
FIGURE 1.
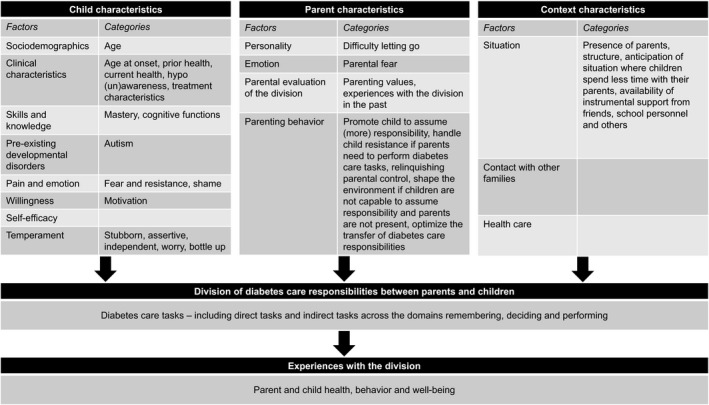
Overview of main study findings.
4.1. Diabetes care tasks
Tasks mentioned by parents could be categorized into those directly or indirectly related to glucose management. All focus group transcripts included the direct tasks of blood glucose measurement, insulin usage, determining the amount of carbohydrate intake, changing injection/infusion site and managing extreme blood glucose values. Indirect tasks included management of supplies, telling others about diabetes, monitoring health, carrying supplies when leaving the house, contacting health care team and managing emotions and support. When mentioned by the moderator, most parents did not consider the implementation of lifestyle recommendations, such as a healthy diet and regular exercise, and foot care as diabetes care tasks. These were not considered diabetes‐specific, were not an issue (e.g., pump allows easy insulin administration for any food) or would make the child feel (more) different from peers. Exercising and healthy food choices were recognized as diabetes care tasks when the child was overweight or when parents wanted to limit the amount of insulin. There were no major differences between the two age groups with regard to the number or content of diabetes care tasks, except parents of younger children listing more communication tasks.
4.2. Division of diabetes care responsibilities
Families varied largely in how tasks were divided between parents and children. In general, children performed more tasks on their own at school than at home. Remembering tasks and deciding about tasks were often parental responsibilities. Older children (12–14 years) had more responsibility in deciding about tasks compared with younger children (9–11 years). As for specific tasks, most children independently performed glucose measurements and shared tasks related to carbohydrate calculations. Parents were frequently in charge of planning and communication. However, older children were, in general, more likely to inform others about diabetes and to independently administer insulin, compared with younger children. Older children were in general primarily responsible for day‐to‐day diabetes care, yet parents reported to take over responsibilities in demanding situations (e.g., at night, while doing sports).
4.3. Experiences about division and transfer
Parents experienced the transfer of diabetes care responsibilities as a dynamic, ongoing process with many challenges and ups and downs. Although parents observed that their child became more skilled and performed more tasks independently over time, parents repeatedly had to retake previously transferred responsibilities. Furthermore, parents indicated that there is no 'one size fits all' approach about the transfer process, given the individual differences between children. Although some parents experienced it as a natural process, others expressed insecurities about when to transfer and retake responsibilities, especially when parental emotional and rational judgments about task division did not align.
Some parents found it difficult to indicate whether they were satisfied with the current division of diabetes care tasks. For them, satisfaction was not relevant, since it was part of parenting and alternatives were not possible. However, the division of tasks could have both positive and negative consequences for their own and their child's health (e.g., fatigue, glycaemic outcomes), behaviour (e.g., actual responsibility taken by the child, parental monitoring and attendance with social activities, conflicts) and well‐being (e.g., fear and worries, distress). Parents of older children reported more frequently that their child resisted assuming responsibility and was less willing to share information about diabetes care with parents.
How these positive and negative experiences were weighted to form a final evaluation of the division was dependent on parental evaluation criteria (i.e., parenting values) (Figure 1). For example, some parents were more positive about the division when their child's health was optimal while others found it more important that their child showed care commitment.
Parents expected that with increasing age, more treatment responsibilities would shift to their child, as children would be more capable and willing to assume responsibility. However, parents also expressed worries about the negative consequences of increasing child responsibility in the future (e.g., child not assuming responsibilities, suboptimal glucose values, refusal of parental involvement and advice).
4.4. Factors playing a role in the division and transfer
According to parents, several child, parent and context factors affected the division and transfer of diabetes care responsibilities. The full list of factors and categories, illustrated by quotes, can be found in Supplement A.
4.4.1. Child factors
About sociodemographics, only increasing child age was frequently used as a proxy measure for an increase in the child's ability to assume responsibility. Relevant clinical factors included age at diagnosis, the child's current and prior health, unawareness of symptoms or actions and treatment characteristics. Younger age at diagnosis could either facilitate the transfer of responsibility (e.g., already used to diabetes care, easier to pick up tasks at a younger age) or hamper it:
'You deal with it [referring to diabetes care tasks] in the same way, unless they are very young, because then you [referring to parent] have always been doing it and you just hold on to that […] Then there is no moment that you say: “Okay, when you are six years old, then you can start handling it [referring to diabetes care tasks] yourself'. (parent 4, 14‐year‐old daughter, diabetes duration of 3 years).
Parents were more involved in their child's diabetes care in case of a history of negative events, a deterioration in health, and current problematic glucose values in terms of frequency and (perceived) controllability and severity.
'I became much more afraid. With such things, I used to be more easygoing, but three years ago [child's name] had a severe hypo. She passed out, became blue, purple, stopped breathing […] After that we became more careful in saying “you can do it yourself”'. (parent 3, 11‐year‐old daughter, diabetes duration of 7 years).
'What I find really difficult with him, is that sometimes he's just not accountable for what he is doing. So he's not thinking when he has a hyper or hypo. And in that state he's making decisions, with me thinking […] “Why on earth do you think that?!”. And persistently sticking with it, because he just doesn't know it anymore. And in those moments, I find it difficult to say: “Hey, you need to assume responsibility.” That is not possible'. (parent 1, 11‐year‐old son, diabetes duration of 9 years).
Hypoglycaemia awareness determined whether the child was better in recognizing and managing signs of hypoglycaemia or whether parents needed to step in, as was unintentional insulin administration during sleep. With respect to treatment factors, the location of the cannula/injection site could necessitate parental assistance, while sensor use facilitated parents to stay up‐to‐date with glucose values. This allowed them to (a) easily take responsibility during tasks requiring special attention, such as sports, (b) retake responsibility of previously transferred tasks faster when diabetes management was suboptimal, (c) gain more trust in the child's ability to manage diabetes and (d) improve the child's self‐efficacy in the transfer process.
With respect to the skills and knowledge necessary for diabetes care tasks, relevant aspects included mastery level and cognitive functions facilitating the acquisition process. These included good arithmetic skills, affinity with technology, and the ability to learn quickly. If the child had difficulties in remembering to perform tasks (e.g., forgetting tasks while playing, easily distracted, chaotic, memory difficulties), parents stayed involved by providing reminders. Pre‐existing developmental disorders complicated the transfer process, as did the experience of pain and negative emotions such as fear of needles, general anxiety, shame.
'For us, the combination of diabetes and autism also makes it difficult. All changes go along with a lot of resistance. For me that is challenging, also the link between cause and effect is often difficult. […] You keep explaining things and it takes a long time before he remembers it'. (parent 10, 15‐year‐old son, diabetes duration of 5 years).
Another important factor was the willingness of the child to take over and assume responsibility. Some parents indicated that their child was not motivated to perform tasks and sometimes even refused responsibility. The onset of puberty was described as a particularly difficult period, as parents observed that their children became less focused on diabetes care and less willing to accept parental involvement. During hyperglycaemia, children also often refused to perform necessary tasks and rejected parental help. On the other hand, children also appeared willing to take over responsibilities, if it would provide them desired freedom, for example if the parent does not need to join school trips. The perception of the child about his/her ability to manage diabetes care tasks (diabetes self‐efficacy) determined whether children asked for parental reassurance or could handle more independence.
As for child temperament, children who were characterized as stubborn, assertive and independent frequently took initiatives to take over diabetes care responsibilities, but found it difficult to accept parental involvement. The tendency to worry a lot and bottle up negative emotions made children more prone to hide high glucose results from parents and less likely to ask for help.
4.4.2. Parental factors
Parental factors that affected the division and transfer of diabetes care responsibilities included personality characteristics (e.g., finding it difficult to 'let go' despite adequate child behaviours) and potentially problematic emotions such as parental fear of needles and complications.
'Yes, I catch myself doing that [referring to checking] as well. Since last week, she has been changing her infusion set and connects her pump, and everything, herself, but then I catch myself checking on what she has done. Then she tells me “Mom, I really know now”. So, I also need to learn that I need to keep quiet and just keep an eye on her from a distance. Every once and a while when it goes wrong, then maybe it is what it is. I need to learn to let go, because she is doing it very well'. (parent 16, 10‐year‐old daughter, diabetes duration of 8 years).
Another important factor was how parents evaluated the division, i.e., how their parenting values interacted with current/prior experiences with the division. Parental values included prioritizing normal child development, serving the child independence level, providing security for the child, supporting what is most important to the child, minimizing conflict/preserving the parent‐child relationship, supporting the child's learning process, keeping the child's health as optimal as possible, and supporting child commitment to diabetes care. Parents changed the division of diabetes care tasks if the consequences of the division were positively or not in line with their parenting value(s):
'You're constantly searching for the right balance, that's what I notice. Yes, sometimes you temporarily retake it and later on you let go again, as long as it goes well, you let go'. (parent 4, 14‐year‐old daughter, diabetes duration of 3 years).
Parents also identified parenting behaviours that affected how diabetes care responsibilities were divided between parents and children. Table 3 provides an overview of behaviours parents used during the transfer process to (a) directly promote the child to assume responsibility, (b) handle child resistance, (c) relinquish parental control, (d) shape the environment to enable the child to assume responsibility and (e) optimize the transfer process of diabetes care responsibilities. However, parenting behaviours stressing the need to take responsibility for diabetes care tasks, like becoming angry when tasks are not performed and constant reminders, did not actually promote the child to assume responsibility.
TABLE 3.
Behaviours parents use during the transfer of diabetes care responsibilities
| Goal of parenting behaviour | Categories | Examples |
|---|---|---|
| Promote child to assume (more) responsibility | Increase knowledge and promote skills |
|
| Help the child to assume responsibilities |
|
|
| Handle child resistance if parents need to perform diabetes care tasks |
|
|
| Relinquishing parental control |
|
|
| Shape the environment if children are not yet capable to assume responsibility and parents are not present | Enable the child to take responsibility themselves |
|
| Enable the child to ask parents for help and involve others |
|
|
| Optimize the transfer of diabetes care responsibilities |
|
4.4.3. Context factors
Children assumed less responsibility for diabetes care if parents were near, compared with situations without parents.
'When I'm there, it's as if he doesn't know how to do it anymore. Then I need to say “[name child] did you measure? Did you do this? Did you do that?” “Oh yeah right, oh yeah right, oh yeah right”. But on Mondays, I work all day and then there is no one around to look after him. He has chosen not to spend his lunchbreak at school anymore. So, he just manages everything. Then everything is fine, he figures it all out by himself. He knows exactly what to do'. (parent 1, 11‐year‐old son, diabetes duration of 9 years).
Furthermore, children assumed more responsibility during the week compared with less structured weekends and holidays. In preparation for situations where children spend more time without their parents, diabetes care tasks were transferred to children.
'And soon she will attend secondary school. I know that in the first year of secondary school, if she goes to that school, that they will have a school camping trip […]. Then I'm not allowed to go with her anymore. So, I said, “You are going to the final school trip of primary school this year, that will be your rehearsal. We will go with you, or mom is going with you, but you will do everything yourself”'. (parent 3, 11‐year‐old daughter, diabetes duration of 7 years).
If parents were not physically near, the availability of instrumental support from friends, school personnel and others played an important role in the child's diabetes independence level. Other factors that changed the balance of responsibility between parents and children were noticing alternative divisions of diabetes care tasks in comparable families and the level of encouragement that children received from the health care team to assume responsibility for diabetes care. In case of problems, health care providers also assisted families to restore the division balance.
5. DISCUSSION
This qualitative study among 18 parents of children with type 1 diabetes aged 9–14 years explored which factors were related to the division and transfer of diabetes care responsibilities. To provide context, we first examined what parents considered as relevant diabetes care tasks, how responsibilities were divided between parents and children, and how parents experienced the current division and transfer of responsibilities. The results of these themes will be discussed first. Subsequently, we will discuss which factors are in line with previous studies, how the current findings complement prior findings, and which identified factors are novel.
According to parents, the transfer of diabetes care responsibilities occurred in a broad context of tasks. This process was not only limited to direct tasks such as taking insulin, but also included indirect tasks like monitoring health and contacting the paediatric team. The list of relevant tasks that emerged from the focus groups largely overlapped with, yet was more extensive and up‐to‐date, than the content of the most commonly used questionnaire to measure the division of care responsibilities (Anderson et al. 1990). With regard to task division, parents were mainly responsible for remembering and deciding about tasks, while children's responsibility mainly focused on performing tasks. This stresses the importance of considering different activities in specific tasks (i.e., remembering, deciding and performing), while studying the division and transfer of diabetes care responsibilities. In line with prior results (Cameron et al. 2008; Schilling et al. 2006), younger children (9–11 years) assumed in general on average less responsibility for diabetes care tasks compared with older children (12–14 years).
However, substantial differences were observed among families of the same age group with respect to how tasks were divided, underlining that other factors beyond the child's age play a role in the timing of transfer. Parents experienced the timing of transfer as difficult and stressful, partly because of potential consequences for both parent and child health, behaviour and well‐being. This matches earlier quantitative associations between the division of treatment responsibilities and factors like family conflict (Lewandowski & Drotar, 2007) and distress (Wiebe et al. 2011). Parental diabetes responsibilities come on top of, and often conflict with, responsibilities for general child development including promoting independence (de Boer et al. 2012). However, parents of chronically ill children experience a deficiency in support from health care providers with respect to the transfer process (Akre & Suris, 2014).
Several factors identified by parents as important in the division and transfer of responsibilities were in line with previous qualitative and quantitative studies (Cameron et al. 2008; Fortenberry et al. 2014; Helgeson et al. 2008; Holmes et al. 2006; Marker et al. 2018; Mulvaney et al. 2013; Newbould et al. 2008; Olinder et al. 2011; Wiebe et al. 2005, 2014). However, our study supplemented previous results with regard to parenting goals/values. In a prior study, the ranked importance of diabetes‐specific parenting goals (e.g., maintain HbA1c below 8.0%, maintain a positive attitude toward diabetes) and general parenting goals (e.g., be able to enjoy a normal childhood, to pass school exams) differed between families and was related to how diabetes care tasks were divided (Robinson et al. 2011). The current study revealed which parenting values were especially important in parents' evaluation of and changes to the division and transfer of diabetes care responsibilities. Additionally, this study also provided a broader overview and deeper understanding of parental views on parenting behaviours during the transfer process of diabetes care responsibilities. Both learning in small steps and parental monitoring of the division have previously been considered as helpful (Berg et al. 2011; Olinder et al. 2011; Pate et al. 2019). In the present study, parents also pointed out that it was helpful to structure the environment, relinquish some parental control, and to make diabetes care tasks meaningful to the child. According to parents, it was less helpful to stress that the child needed to take more responsibility. These findings can best be seen in the light of self‐determination theory (Deci & Ryan, 2000), which specifies that behaviours will be more frequent and stable when they help to reach personal goals (e.g., be independent or healthy) and are less likely when performed to avoid punishment or guilt (e.g., parental disappointment).
Novel factors that were identified in the current study as important for the division and transfer included treatment‐related variables, willingness and motivation of the child, hypoglycaemia awareness, pre‐existing developmental disorders, parental tendency to keep checking the child despite adequate child behaviours, and parental fears. Compared with previous qualitative studies that identified factors affecting the division and transfer of diabetes care responsibilities, this was the first study that specifically focussed on factors affecting this process from a parental point view for a broad range of care tasks exclusively related to diabetes care. As a result, it is difficult to evaluate if results are specific to the included sample. However, in a study among parents of children with type 1 diabetes and autism, self‐management challenges were reported to be amplified by autism and parents described facing a high emotional burden because of constant monitoring and performing of diabetes care tasks (Oser et al. 2020). Moreover, in a study among children with type 1 diabetes, motivation was considered as an important aspect of the transition towards autonomy in self‐management (Karlsson et al. 2008). These newly identified constructs include non‐modifiable factors to take into account when determining a realistic transfer pathway, as well as factors that are modifiable and can be targeted in interventions. Future studies are needed to evaluate whether these results are transferable to other parent groups and whether changes in these constructs are followed by a change in the division of diabetes care responsibilities.
6. LIMITATIONS
This study has several limitations. Firstly, the sample mainly consisted of highly educated, working parents with an intact family and a Dutch background; selection bias with respect to other sociodemographic and clinical variables (e.g., HbA1 c) is likely to have occurred, but it is unclear to which extent, since no comparisons could be made between responders and nonresponders. Secondly, we did not ask participants whether they were the parent who was primarily responsible for their child's diabetes care. Thirdly, only views of parents of children aged 9–14 years were examined. Future studies are needed to examine whether children hold similar views to their parents, how these constructs are viewed in younger (6–8 years) and older (15–17 years) age groups, and what works best for families with specific challenges in the transfer process, for example in case of intellectual disabilities, very high HbA1 c values. Fourthly, to facilitate interpretation, factors that affected division and transfer were presented as single entities, whereas interactions between factors were also observed.
This study underlines that health care providers need to keep in mind that many factors beyond age play a role in the transfer process and that families might struggle to find the right balance of responsibility, as this might have a negative impact on the child and family. Health care providers should be aware that a 'successful transition of diabetes care tasks' is defined differently across families because of a different ranking in parenting values and that it might differ from their own definition. The listed factors can be used by diabetes care teams (with an important role for specialized nurses) as a discussion tool to identify facilitators and barriers in the transfer process in the family and determine how these factors interact with each other to come to truly family‐tailored advice. For example, the use of a sensor might help families who struggle with the division because of the child's self‐efficacy or parental trust. In case of current treatment characteristics or impaired awareness of hypoglycaemia are identified as barriers, health care providers can further assist families in resolving these issues. Furthermore, depending on specific problems, parents can be empowered by providing them with identified examples of helpful parenting behaviours. Although some families did not experience major problems during the transfer process, most parents mentioned off‐record that they found it helpful to exchange experiences with each other about this topic.
This study showed that questionnaires measuring the division need to be updated to reflect relevant diabetes care tasks and need to consider responsibilities for different activities in specific tasks (i.e., remembering, deciding and performing). Additionally, future quantitative studies can evaluate whether parenting support (groups) might be an effective intervention method for families experiencing problems with this process. Future studies are also needed to further examine how specific factors affect the division and transfer of diabetes care responsibilities (as some factors such as autism were only present in one family) and whether our results are transferable to different cultures/health care settings and parent groups with different characteristics compared with the current sample. To examine parental experiences about the transfer process in more detail, future qualitative studies might consider focusing on parent dyads as this study showed that parental characteristics play a role in how this process is perceived.
7. CONCLUSION
To conclude, several child, parent and context characteristics were identified that affected how families divide and transfer diabetes care tasks. As parents of children with diabetes find it difficult to find the right division and transfer process of diabetes care responsibilities, these characteristics can serve as input for further research integrating a more family‐tailored approach into current age‐based guidelines to improve regular care support. Additional quantitative research can also shed more light on how these factors and the responsibility division are related to health outcomes.
CONFLICT OF INTEREST
No conflict of interest has been declared by the authors.
AUTHOR CONTRIBUTIONS
J. A., E. E., F. P. and G. N. obtained funding and designed the study. J. A. coordinated the data collection. E. E., P. W., E.v. M., A. R. V., E. M. M., H. J. A. and G. N. assisted in data collection and provided administrative support. J. A., E. E. and G. N. analysed data. J. A. and G. N. drafted the manuscript. E. E., P. W., E.v. M., A. R. V., E. M. M., H. J. A. and F. P. reviewed the manuscript. All authors have read and approved the final manuscript.
Supporting information
Supplementary Material
ACKNOWLEDGEMENTS
The authors are grateful to all participating parents for sharing their personal experiences and to all participating centres for their support during the recruitment. The authors thank William Alexander Keuchler and Kevin Matlock for providing feedback on the translation of the included quotes. Finally, the authors would like to thank the student assistants who assisted in the data collection.
Aalders J, Hartman E, Pouwer F, et al. The division and transfer of care responsibilities in paediatric type 1 diabetes: A qualitative study on parental perspectives. J Adv Nurs. 2021;77:1968–1979. 10.1111/jan.14781
Funding Information
This study was supported by the Dutch Research Council (NWO) (Research Talent – 406‐14‐103). The funding source had no role in the design of the study, the collection and analysis of data, the preparation of the manuscript and the decision to submit the manuscript.
REFERENCES
- Akre, C. , & Suris, J.‐C. (2014). From controlling to letting go: What are the psychosocial needs of parents of adolescents with a chronic illness? Health Education Research, 29(5), 764–772. 10.1093/her/cyu040 [DOI] [PubMed] [Google Scholar]
- American Diabetes Association . (2018). 12. Children and adolescents: standards of medical care in diabetes—2018. Diabetes Care, 41(Suppl 1), S126–S136. [DOI] [PubMed] [Google Scholar]
- Anderson, B. J. , Auslander, W. F. , Jung, K. C. , Miller, J. P. , & Santiago, J. V. (1990). Assessing family sharing of diabetes responsibilities. Journal of Pediatric Psychology, 15(4), 477–492. 10.1093/jpepsy/15.4.477 [DOI] [PubMed] [Google Scholar]
- Barbour, R. S. (2001). Checklists for improving rigour in qualitative research: A case of the tail wagging the dog? BMJ, 322(7294), 1115–1117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berg, C. A. , King, P. S. , Butler, J. M. , Pham, P. , Palmer, D. , & Wiebe, D. J. (2011). Parental involvement and adolescents' diabetes management: The mediating role of self‐efficacy and externalizing and internalizing behaviors. Journal of Pediatric Psychology, 36(3), 329–339. 10.1093/jpepsy/jsq088 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boeije, H. (2002). A purposeful approach to the constant comparative method in the analysis of qualitative interviews. Quality & Quantity, 36(4), 391–409. [Google Scholar]
- Cameron, F. J. , Skinner, T. C. , de Beaufort, C. E. , Hoey, H. , Swift, P. G. , Aanstoot, H. , Aman, J. , Martul, P. , Chiarelli, F. , Daneman, D. , Danne, T. , Dorchy, H. , Kaprio, E. A. , Kaufman, F. , Kocova, M. , Mortensen, H. B. , Njolstad, P. R. , Phillip, M. , Robertson, K. J. , … Skovlund, S. E. (2008). Are family factors universally related to metabolic outcomes in adolescents with type 1 diabetes? Diabetic Medicine, 25(4), 463–468. [DOI] [PubMed] [Google Scholar]
- Cho, J. Y. , & Lee, E.‐H. (2014). Reducing confusion about grounded theory and qualitative content analysis: Similarities and differences. The Qualitative Report, 19(32), 1–20. [Google Scholar]
- Coffen, R. D. (2009). The 600‐step program for type 1 diabetes self‐management in youth: The magnitude of the self‐management task. Postgraduate Medicine, 121(5), 119–139. 10.3810/pgm.2009.09.2059 [DOI] [PubMed] [Google Scholar]
- de Boer, G. , van Dongen, L. , Poolman–Mazel, T. , Portegijs, C. & Wierenga, W. (2012). De inzet van de medisch psycholoog bij de behandeling van kinderen & jeugdigen met diabetes mellitus. Sectie Psychologen Algemene/Academische Ziekenhuizen (PAZ) van het Nederlands Instituut Van Psychologen (NIP) en Vereniging Van Kinder‐ en Jeugdpsychologen en Orthopedagogen in Ziekenhuizen.
- Deci, E. L. , & Ryan, R. M. (2000). The" what" and" why" of goal pursuits: Human needs and the self‐determination of behavior. Psychological Inquiry, 11(4), 227–268. 10.1207/S15327965PLI1104_01 [DOI] [Google Scholar]
- DiMeglio, L. A. , Acerini, C. L. , Codner, E. , Craig, M. E. , Hofer, S. E. , Pillay, K. , & Maahs, D. M. (2018). ISPAD clinical practice consensus guidelines 2018: Glycemic control targets and glucose monitoring for children, adolescents, and young adults with diabetes. Pediatric Diabetes, 19(S27), 105–114. 10.1111/pedi.12737 [DOI] [PubMed] [Google Scholar]
- Fortenberry, K. T. , Berg, C. A. , King, P. S. , Stump, T. , Butler, J. M. , Pham, P. K. , & Wiebe, D. J. (2014). Longitudinal trajectories of illness perceptions among adolescents with type 1 diabetes. Journal of Pediatric Psychology, 39(7), 687–696. 10.1093/jpepsy/jsu043 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gelo, O. , Braakmann, D. , & Benetka, G. (2008). Quantitative and qualitative research: Beyond the debate. Integrative Psychological and Behavioral Science, 42(3), 266–290. 10.1007/s12124-008-9078-3 [DOI] [PubMed] [Google Scholar]
- Helgeson, V. S. , Reynolds, K. A. , Siminerio, L. , Escobar, O. , & Becker, D. (2008). Parent and adolescent distribution of responsibility for diabetes self‐care: Links to health outcomes. Journal of Pediatric Psychology, 33(5), 497–508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holmes, C. S. , Chen, R. , Streisand, R. , Marschall, D. E. , Souter, S. , Swift, E. E. , & Peterson, C. C. (2006). Predictors of youth diabetes care behaviors and metabolic control: A structural equation modeling approach. Journal of Pediatric Psychology, 31(8), 770–784. 10.1093/jpepsy/jsj083 [DOI] [PubMed] [Google Scholar]
- Hughes, A. E. , Berg, C. A. , & Wiebe, D. J. (2012). Emotional processing and self‐control in adolescents with type 1 diabetes. Journal of Pediatric Psychology, 37(8), 925–934. 10.1093/jpepsy/jss062 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karlsson, A. , Arman, M. , & Wikblad, K. (2008). Teenagers with type 1 diabetes–a phenomenological study of the transition towards autonomy in self‐management. International Journal of Nursing Studies, 45(4), 562–570. 10.1016/j.ijnurstu.2006.08.022 [DOI] [PubMed] [Google Scholar]
- Kinder Diabetes Centrum Nijmegen . (2020). Diabetes groeimodel. https://www.diabetesgroeimodel.nl/
- King, P. S. , Berg, C. A. , Butner, J. , Butler, J. M. , & Wiebe, D. J. (2014). Longitudinal trajectories of parental involvement in type 1 diabetes and adolescents' adherence. Health Psychology, 33(5), 424–432. 10.1037/a0032804 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lange, K. , Swift, P. , Pańkowska, E. , & Danne, T. (2014). Diabetes education in children and adolescents. Pediatric Diabetes, 15(S20), 77–85. 10.1111/pedi.12187 [DOI] [PubMed] [Google Scholar]
- Lewandowski, A. , & Drotar, D. (2007). The relationship between parent‐reported social support and adherence to medical treatment in families of adolescents with type 1 diabetes. Journal of Pediatric Psychology, 32(4), 427–436. [DOI] [PubMed] [Google Scholar]
- Marker, A. M. , Noser, A. E. , Clements, M. A. , & Patton, S. R. (2018). Shared responsibility for type 1 diabetes care is associated with glycemic variability and risk of glycemic excursions in youth. Journal of Pediatric Psychology, 43(1), 61–71. 10.1093/jpepsy/jsx081 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Markowitz, J. T. , Garvey, K. C. , & Laffel, L. M. B. (2015). Developmental changes in the roles of patients and families in type 1 diabetes management. Current Diabetes Review, 11(4), 231–238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mulvaney, S. A. , Lilley, J. S. , Cavanaugh, K. L. , Pittel, E. J. , & Rothman, R. L. (2013). Validation of the diabetes numeracy test with adolescents with type 1 diabetes. Journal of Health Communication, 18(7), 795–804. 10.1080/10810730.2012.757394 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Newbould, J. , Smith, F. , & Francis, S. A. (2008). 'I'm fine doing it on my own': Partnerships between young people and their parents in the management of medication for asthma and diabetes. Journal of Child Health Care, 12(2), 116–128. [DOI] [PubMed] [Google Scholar]
- Olinder, A. L. , Nyhlin, K. T. , & Smide, B. (2011). Clarifying responsibility for self‐management of diabetes in adolescents using insulin pumps ‐ a qualitative study. Journal of Advanced Nursing, 67(7), 1547–1557. 10.1111/j.1365-2648.2010.05588.x [DOI] [PubMed] [Google Scholar]
- Onwuegbuzie, A. J. , Dickinson, W. B. , Leech, N. L. , & Zoran, A. G. (2009). A qualitative framework for collecting and analyzing data in focus group research. International Journal of Qualitative Methods, 8(3), 1–21. 10.1177/160940690900800301 [DOI] [Google Scholar]
- Oser, T. K. , Oser, S. M. , Parascando, J. A. , Grisolano, L. A. , Krishna, K. B. , Hale, D. E. , Litchman, M. , Majidi, S. , & Haidet, P. (2020). Challenges and successes in raising a child with type 1 diabetes and autism spectrum disorder: Mixed methods study. Journal of Medical Internet Research, 22(6), e17184.– 10.2196/17184 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pate, T. , Klemenčič, S. , Battelino, T. , & Bratina, N. (2019). Fear of hypoglycemia, anxiety, and subjective well‐being in parents of children and adolescents with type 1 diabetes. Journal of Health Psychology, 24(2), 209–218. 10.1177/1359105316650931 [DOI] [PubMed] [Google Scholar]
- Reed‐Knight, B. , Blount, R. L. , & Gilleland, J. (2014). The transition of health care responsibility from parents to youth diagnosed with chronic illness: A developmental systems perspective. Families, Systems, & Health, 32(2), 219–234. 10.1037/fsh0000039 [DOI] [PubMed] [Google Scholar]
- Robinson, E. M. , Iannotti, R. J. , Schneider, S. , Nansel, T. R. , Haynie, D. L. , & Sobel, D. O. (2011). Parenting goals: Predictors of parent involvement in disease management of children with type 1 diabetes. Journal of Child Health Care, 15(3), 199–209. 10.1177/1367493511406567 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schilling, L. S. , Knafl, K. A. , & Grey, M. (2006). Changing patterns of self‐management in youth with type I diabetes. Journal of Pediatric Nursing, 21(6), 412–424. 10.1016/j.pedn.2006.01.034 [DOI] [PubMed] [Google Scholar]
- Scott, L. K. (2013). Developmental mastery of diabetes‐related tasks in children. Nursing Clinics of North America, 48(2), 329–342. 10.1016/j.cnur.2013.01.015 [DOI] [PubMed] [Google Scholar]
- Wiebe, D. J. , Berg, C. A. , Korbel, C. , Palmer, D. L. , Beveridge, R. M. , Upchurch, R. , Lindsay, R. , Swinyard, M. T. , & Donaldson, D. L. (2005). Children's appraisals of maternal involvement in coping with diabetes: Enhancing our understanding of adherence, metabolic control, and quality of life across adolescence. Journal of Pediatric Psychology, 30(2), 167–178. 10.1093/jpepsy/jsi004 [DOI] [PubMed] [Google Scholar]
- Wiebe, D. J. , Chow, C. M. , Palmer, D. L. , Butner, J. , Butler, J. M. , Osborn, P. , & Berg, C. A. (2014). Developmental processes associated with longitudinal declines in parental responsibility and adherence to type 1 diabetes management across adolescence. Journal of Pediatric Psychology, 39(5), 532–541. 10.1093/jpepsy/jsu006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wiebe, D. J. , Gelfand, D. , Butler, J. M. , Korbel, C. , Fortenberry, K. T. , McCabe, J. E. , & Berg, C. A. (2011). Longitudinal associations of maternal depressive symptoms, maternal involvement, and diabetes management across adolescence. Journal of Pediatric Psychology, 36(7), 837–846. 10.1093/jpepsy/jsr002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams, C. (1999). Gender, adolescence and the management of diabetes. Journal of Advanced Nursing, 30(5), 1160–1166. 10.1046/j.1365-2648.1999.01168.x [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Material


