ABSTRACT
There is a lack of instruments assessing child–caregiver attachment relationships in early childhood to be used in attachment‐based practice, in particular from a caregiver's perception, which is an important factor of clinical importance to take into account in parenting interventions targeting young children. Therefore, the 48‐item Attachment Relationship Inventory—Caregiver Perception 2–5 years (ARI‐CP 2–5) was developed. Survey data of 446 caregivers of 2‐ to 5‐year‐old children were collected, and a subsample of 83 caregivers participated in an observation study. Confirmatory factor analysis confirmed a four‐factor structure of secure, avoidant, ambivalent, and disorganized attachment relationship. Indications of configural, metric, and scalar invariance were found for caregivers’ and children's sex, children's age, and population (clinical vs. general population). The four scales showed sufficient internal consistency and significant associations with children's psychopathology, caregivers’ general attachment representations, caregivers’ mind‐mindedness, and population type. Moreover, preliminary evidence for convergent validity with observational attachment measures was found. It is concluded that the ARI‐CP 2–5 is a valid instrument that can be used as part of the screening and assessment of insecure attachment relationships.
Keywords: attachment relationships, caregivers’ perception, questionnaire, validation, relaciones de afectividad, percepción de los cuidadores, cuestionario, validación, relations d'attachement, perception des aidants naturels, questionnaire, validation, Bindungsbeziehungen, Perspektive der Bezugspersonen, Fragebogen, Validierung, 愛着関係, 養育者の認識, 調査票, 検証, 依恋关系, 看护者感知, 问卷, 验证, علاقات التعلق، منظور مقدمي الرعاية، استبيان، التحقق من الصحة
RESUMEN
Hacen falta instrumentos que evalúen las relaciones de afectividad niño‐cuidador en la temprana niñez para ser usados en la práctica que se basa en la afectividad, en particular desde la perspectiva del cuidador, lo cual es un factor clave de importancia clínica para tomar en cuenta en las intervenciones de crianza que se enfocan en niños pequeños. Por tanto, se desarrolló el Inventario de la Relación Afectiva – Percepción del Cuidador 2–5 años, que consta de 48 aspectos (ARI‐CP 2–5). Se recogió información de encuesta de 446 cuidadores de niños de 2 a 5 años de edad, y un subgrupo muestra de 83 cuidadores participó en un estudio de observación. Los análisis de factores confirmatorios corroboraron una estructura de cuatro factores de la relación de afectividad que es segura, la que evita, la ambivalente y la desorganizada. Se encontraron indicaciones de invariabilidad en el aspecto configuracional, métrico y de escala en cuanto al género sexual de los cuidadores y del niño, la edad del niño, y la población (clínica y general).
Las cuatro escalas mostraron una suficiente consistencia interna y asociaciones significativas con la sicopatología de los niños, las representaciones generales de afectividad del cuidador, la conciencia mental de los cuidadores, así como el tipo de población. Es más, se encontró una evidencia preliminar para la validez convergente con las medidas de afectividad de observación. Se concluye con que el ARI‐CP 2–5 es un instrumento válido que puede usarse como parte de la detección y evaluación de las relaciones de afectividad inseguras.
RÉSUMÉ
Il y a un manque d'instruments évaluant les relations d'attachement enfant‐aidant naturel dans la petite enfance pouvant être utilisés dans une pratique basée sur l'attachement, en particulier sur la perception de l'aidant naturel, qui est un facteur important de l'importance clinique à prendre en compte dans les interventions de parentages ciblant les jeunes enfants. Par conséquent l'Inventaire de 48 articles de la Relation d'Attachement – Perception de l'Aidant Naturel 2–5 ans (abrégé en anglais ARI‐CP 2–5) a été développé. Les données de sondage de 446 aidants naturels d'enfants de 2 à 5 ans ont été recueillies et un sous‐échantillon de 83 aidants naturels ont participé à une étude d'observation. Une analyse factorielle confirmatoire a confirmé une structure à quatre facteurs de la relation d'attachement sécure, évitant, ambivalent et désorganisé. Des indications d'invariance configurale, métrique et scalaire ont été trouvées pour le sexe des aidants naturels et des enfants, l’âge des enfants, et la population (clinique par rapport à population générale). Les quatre échelles ont démontré une cohérence interne suffisante et des associations importantes avec la psychopathologie des enfants, les représentations de l'attachement générale des aidants naturels, l'esprit‐qualité mentale et le type de population. De plus une preuve préliminaire de validité convergente ave les mesures observationnelles d'attachement a été trouvée. Nous concluons que l'ARI‐CP 205 est un instrument valide qui peut être utilisé pour le dépistage et l’évaluation de relations d'attachement insécures.
ZUSAMMENFASSUNG
Entwicklung und Validierung des Inventars für Bindungsbeziehung – Eltern‐ bzw. Betreuer_innenperspektive 2–5 Jahre (ARI‐CP 2–5): Psychometrische Struktur, externe Validität und Normen
Es fehlen Instrumente zur Beurteilung der Bindungsbeziehungen zwischen Kleinkind und Bezugsperson, die in der bindungsbasierten Praxis verwendet werden können. Insbesondere fehlen hierbei Instrumente, die die Wahrnehmung der Bezugspersonen einschließen ‐ ein Faktor von großer klinischer Bedeutung, der bei Elterninterventionen für Kleinkinder berücksichtigt werden sollte. Aus diesem Grund wurde das 48‐Punkte‐Inventar für Bindungsbeziehung – Eltern‐ bzw. Betreuer_innenperspektive 2–5 Jahre (ARI‐CP 2–5) entwickelt. Von 446 Bezugspersonen 2‐5‐jähriger Kinder wurden Umfragedaten gesammelt und eine Teilstichprobe von 83 Bezugspersonen nahm an einer Beobachtungsstudie teil. Eine konfirmatorische Faktoranalyse ergab eine Vier‐Faktoren‐Struktur aus sicheren, vermeidenden, ambivalenten und unorganisierten Bindungsbeziehungen. Hinweise auf konfigurale, metrische und skalare Messinvarianz wurden für Geschlecht und Alter der Bezugspersonen und Kinder sowie für die Stichprobe (klinisch vs. allgemein) gefunden. Die vier Skalen wiesen ausreichende interne Konsistenz und signifikante Assoziationen mit der kindlichen Psychopathologie, den allgemeinen Bindungsrepräsentationen, dem Mind‐Mindedness der Bezugspersonen und der Art der Stichprobe auf. Darüber hinaus wurden vorläufige Belege für konvergente Validität mit beobachtenden Bindungsmaßen gefunden. Es wird der Schluss gezogen, dass der ARI‐CP 2–5 ein valides Instrument ist, das im Rahmen von Screenings und Beurteilungen unsicherer Bindungsbeziehungen verwendet werden kann.
抄録
愛着関係調査票–2歳から5歳の養育者の認識 (ARI‐CP 2–5)の開発と検証:心理検 査構造、外部の妥当性と規範 幼児期に幼児―養育者の愛着関係を評価する方策が不足しており、幼児を対象と した子育て介入において臨床的に考慮すべき重要な要素である愛着、特に愛着に 対する養育者の認識に基づいた実践に活用できない。そこで、48項目の愛着関係 調査票‐2歳から5歳の養育者の認識 (ARI‐CP 2–5)が開発された。446人の2歳から 5歳の子どもの養育者の調査データが収集され、二次標本として83人の養育者が 観察研究に参加した。確認的因子分析で安全型、回避型、抵抗/両価型、混乱型 の愛着という4因子の構造を確認した。養育者と子どもの性別、子どもの年齢、 集団 (臨床と一般) のために構成の指標と測定基準、およびスカラー不変性が発 見された。4つのスケールは十分な内的整合性を示し、子どもの精神病理、養育 者の一般的な愛着表現、養育者のマインドマインドネス、母集団のタイプとの間 に有意な関連を示した。さらに観察に基づいた愛着の評価とともに収束性妥当性 のための予備的証拠が見つかった。ARI‐CP 2–5は、不安定型愛着関係のスクリー ニングと評価の一部として使用できる有効な手段であると結論付けられる。
摘要
摘 要:目前缺乏可用于依恋实践的评估儿童早期看护者依恋关系的工具, 特别是从看护者的感知角度, 这是针对幼儿的养育干预措施中需要考虑的一个重要临床因素。因此, 编制了含括48题的依恋关系 – 2–5岁儿童看护者感知量表 (ARI‐CP 2–5)。收集了446名2–5岁儿童看护者的调查数据, 并以83名看护者子样本为被试进行观察研究。验证性因素分析证实了安全、回避、矛盾和无序依恋关系的四因素结构。在看护者和儿童性别、儿童年龄以及人群 (临床和一般人群) 中发现了构型、度量和标量不变性的迹象。四个量表显示出足够的内在一致性, 并与儿童的精神病理学、看护者的一般依恋表征、看护者的心智和人群类型显著相关。此外, 还发现了通过观察依恋措施聚合效度的初步证据。结论:ARI‐CP 2–5是一种有效的工具, 可用于不安全型依恋关系的部分筛选和评估。
ملخص
تطوير وتحقيق مقياس التعلق المرتبط بالعلاقات ‐ تصورات مقدم الرعاية 2–5 سنوات
دراسة البنية السيكوميترية والصلاحية الخارجية والمعايير
هناك نقص في الأدوات التي تقيِّم العلاقات بين الأطفال ومقدمي الرعاية في مرحلة الطفولة المبكرة لاستخدامها في الممارسة القائمة على التعلق، ولا سيما من منظور مقدم الرعاية، والذي يعتبر عامل مهم من العوامل ذات الأهمية الاكلينيكية التي ينبغي مراعاتها في التدخلات الوالدية التي تستهدف الأطفال الصغار. ولذلك تم تطوير قائمة فحص التعلق من 48 عنصر ‐ منظور مقدم الرعاية 2–5 سنوات (5‐CP 2‐ARI) وتم جمع بيانات استقصائية عن 446 من مقدمي الرعاية للأطفال الذين تبلغ أعمارهم سنتين إلى خمس سنوات، وشارك في دراسة الملاحظة عينة فرعية من 83 من مقدمي الرعاية. أكد تحليل العامل وجود أربعة عوامل تمثل بنية التعلق الآمن، والمتجنب، والمتناقض، والغير منظم. وأشارت النتائج إلى وجود مؤشرات لثوابت شكلية، وقياسية من حيث جنس مقدمي الرعاية والأطفال، وأعمار الأطفال، والتركيبة السكانية (العينة الإكلينيكية مقابل عامة السكان).وأظهرت المقاييس الأربعة اتساقًا داخليًا كافيًا وارتباطا إحصائياً مع الصحة النفسية للأطفال، والتصورات العامة للتعلق عندمقدمي الرعاية، والتصورات الذهنية لمقدمي الرعاية، ونوع السكان. وعلاوة على ذلك، وُجد دليل أولي على الصلاحية المتقاربة لمقاييس التعلق القائمة على الملاحظة. وتخلص الدراسةإلى أن مقياس (5‐CP 2‐ARI) يعتبر أداة صالحة يمكن استخدامها كجزء من فحص وتقييم علاقات التعلق غير الآمنة .
1. INTRODUCTION
The child–parent attachment relationship constitutes the basis of children's social and emotional development (Bowlby, 1969). Children in secure attachment relationship rely on their caregivers as a secure haven when in need of comfort and protection, use them as a secure base to explore the world, and the caregiver is able to provide in this need (Powell, Cooper, Hoffman, & Marvin, 2013). However, in insecure attachment relationships, caregivers do not provide the secure haven and base for children, and therefore, these children cannot find the balance between proximity and distance to an attachment figure, or sometimes have no strategy at all to keep such a balance (Ainsworth, Blehar, Waters, & Wall, 1978; Main & Hesse, 1990; Powell et al., 2013).
Children showing insecure attachment relationships with their caregivers have a higher risk for psychopathology, such as internalizing problems (Colonnesi et al., 2011; Groh, Fearon, van IJzendoorn, Bakermans‐Kranenburg, & Roisman, 2017; Spruit et al., 2020) and externalizing problems (Hoeve et al., 2012; Madigan, Brumariu, Villani, Atkinson, & Lyons‐Ruth, 2016). Therefore, it is of great importance that in clinical practice attention is directed toward the quality of parent–child attachment relationships. The current study reports on the development and reliability, validity, and norms of the Attachment Relationship Inventory—Caregiver Perceptions 2–5 years (ARI‐CP 2–5; Reference blinded for peer review), a caregiver‐report questionnaire aimed at measuring the caregiver's perception of the attachment relationship with their child aged between 2 and 5 years.
1.1. Attachment relationships
The quality of the attachment relationship between children and their caregivers is perceived as a complex, multidimensional construct (Bosmans & Kerns, 2015; Bretherton, 1985, Solomon & George, 2008; Waters & Cummings, 2000; Zeanah & Boris, 2012). The attachment relationship is dyadic in nature (Bretherton, 1985; Sroufe & Fleeson, 1988; Zeanah & Boris, 2012). It consists of proximal processes between children and caregivers: behaviors of the caregiver influence behaviors of their children, which in turn affect the caregiver's reactions (George & Solomon, 2008; Powell et al., 2013). The quality of the attachment relationship is, therefore, expressed by attachment‐related behavioral interactions, and also includes mental components, such as attachment representations (i.e., the way relationships are perceived, mentally represented, remembered, and described) that drive behaviors of both children and their caregivers within that relationship (Bretherton, 1985; Solomon & George, 2008; Zeanah & Benoit, 1995). Thus, attachment relationships are characterized by dyadic processes at both behavioral and representational levels.
Four types of attachment relationships have been described in literature (Ainsworth et al., 1978; Main & Hesse, 1990; Powell et al., 2013). Secure attachment relationships (Type B) are characterized by healthy child–caregiver interactions in which children use their consistently sensitive caregivers both as a secure haven and secure base. Children of caregivers who are consistently insensitive and possibly rejecting are assumed to minimize their attachment behaviors to keep proximity to the caregiver, which is typical of an insecure–avoidant attachment relationship (Type A). When the caregiver is inconsistently sensitive, children maximize their attachment behaviors to keep proximity to the caregiver, which is typical of an insecure–ambivalent attachment relationship (Type C; Ainsworth et al., 1978; Cassidy & Berlin, 1994). Finally, the disorganized attachment relationship was identified, in which children perceive their caregivers as a source of both comfort and fear, which is an unsolvable paradox (Main & Hesse, 1990). This “fear with no solution” prohibits the development of an organized strategy for the use of the attachment figure in case of distress, and results in a mixture of different types of insecure and secure behaviors, combined with frightening reactions to harsh parenting or disrupted, frightening behaviors of caregivers (ibid., 1990).
1.2. Measuring the quality of attachment relationships
Instruments that assess (aspects of) child–caregiver attachment relationships can be categorized in several ways. First, the most basic distinction is that between behavioral and representational measures (O'Connor & Byrne, 2007). Historically, there has been a dominance of focusing on the behavioral aspect of the attachment relationship in infancy and early childhood, for example, by using the Strange Situation Procedure (SSP; Ainsworth et al., 1978). Later, the value of the underlying mental processes of attachment‐related behaviors (i.e., internal working models) in both children and their caregivers was emphasized (O'Connor & Byrne, 2007; Solomon & George, 2008). Second, attachment instruments focus on the child, the caregiver, or both. For example, the SSP assesses the observable behavior of the child, whereas the Atypical Maternal Behavior Instrument for Assessment and Classification (AMBIANCE; Bronfman, Parsons, & Lyons‐Ruth, 1999) codes the caregivers’ behaviors (Tryphonopoulos, Letourneau, & Ditommaso, 2014). The Emotional Availability Scales (Biringen, 2008) rate both behaviors of the child and the caregiver (Biringen, Derscheid, Vliegen, Closson, & Easterbrooks, 2014).
In clinical practice, it is important to know the caregiver's contribution to the attachment relationship with his or her child, because in attachment‐based interventions the caregiver is the target to obtain secure attachment relationships (Benoit, Madigan, Lecce, Shea, & Goldberg, 2001; Juffer, Bakermans‐Kranenburg, & Van IJzendoorn, 2014; Zeegers, Colonnesi, Noom, Polderman, & Stams, 2020). More specifically, there is a clinical need to be aware of the caregiver's perception of the attachment relationships with the child (Bailey, Redden, Pederson, & Moran, 2016).
Assessing the caregivers’ perception might contribute to successful attachment‐based treatment, because caregivers experience their child over longer periods of time in a multitude of attachment‐related situations, and are therefore able to provide valuable information on the child–caregiver attachment relationship. Further, the caregiver's perception of the relationship with the child influences his or her emotional response to the child, and ultimately also the attachment behavior of the child toward the caregiver (Benoit, Zeanah, Parker, Nicholson, & Coolbear, 1997; Bugental & Johnston, 2000; Vreeswijk, Maas, & van Bakel, 2012). Moreover, it is important to be aware of possibly distorted perceptions of caregivers, because (lack of) relational insights of caregivers have shown to correlate with the quality of attachment (Bailey et al., 2016; Koren‐Karie, Oppenheim, Dolev, Sher, & Etzion‐Carasso, 2002). If, for example, caregivers deny problems within the attachment relationship when multiple indications of attachment‐related problems exist, therapists first need to direct attention to distorted perceptions before they can start behavioral‐focused attachment‐based interventions (Molinari & Freeborn, 2006). Alternatively, these distorted perceptions may be a target of attachment‐based treatment itself (Bailey et al., 2016). Passing by the caregivers’ perceptions could lead to resistance, and might stand in the way of effective parenting interventions (Girvin, 2004; Hawley & Weisz, 2003). Attachment‐oriented measures focusing on the caregivers’ perceptions are thus valuable.
No available attachment instrument is able to capture the full width of the dyadic, multi‐facetted attachment construct. It is therefore important to be specific about which component of the attachment relationship is measured and what the specific measure reflects (Bosmans & Kerns, 2015; Spruit et al., 2018). In the assessment of the quality of attachment relationships, it is therefore recommended to combine information from multiple instruments, each focusing on a different aspect of the attachment relationship in order to obtain a total picture of the quality of the child–caregiver attachment relationship (Bosmans & Kerns, 2015).
Questionnaires have the advantage to be rather straightforward, practical, and economical instruments to assess an aspect of the quality of attachment relationships between children and their caregivers. Other types of instruments, such as observational measures and interviews, are rather time consuming or require extensive training (Dwyer, 2005). In clinical practice, the lack of straightforward instruments could lead to the (wrong) decision to not assess the quality of attachment relationships at all (Spruit et al., 2018). All in all, there is a clear desire for a straightforward, practical attachment relationship instrument, and a questionnaire might be able to fulfill this need.
1.3. The current study
With the need for practical instruments focusing on the attachment relationship between young children and their caregivers, and the importance of understanding the caregiver's perception of this relationship in mind, the Attachment Relationship Inventory—Caregiver Perception 2–5 years (Reference blinded for peer review) was developed. The ARI‐CP 2–5 is a caregiver‐report questionnaire aimed at measuring the caregiver's perception of the attachment relationship with the child of 2–5 years old. The development of the ARI‐CP 2–5 is more extensively described in Section 2. The current study presents the internal structure, external validity, and norms of the final ARI‐CP 2–5 years. The ARI‐CP 2–5 consists of 48 items covering four subscales: secure, insecure–avoidant, insecure–ambivalent, and insecure–disorganized attachment.
The ARI‐CP 2–5 is developed to be used in clinical practice as part of the assessment of the quality of attachment relationships and the screening of insecure attachment relationships. Also, the ARI‐CP 2–5 is meant to be used in research as a straightforward, practical, and economical instrument to assess the caregiver's perception of the attachment relationship with the child. The ARI‐CP aims to provide an indication, based on population‐based norms, of the extent to which caregivers recognize secure and insecure attachment patterns in the relationship with their child. It gives insights into how caregivers perceive the attachment relationship.
The current study is aimed at testing the validity and reliability of the ARI‐CP 2–5. First, the internal structure of the ARI‐CP 2–5 was determined. Next, measurement invariance of the instrument was examined across mothers and fathers, boys and girls, 2‐ to 3‐year olds, and 4‐ and 5‐year olds, as well as across children from a general population sample and a clinical sample. Moreover, reliability information on the four subscales and the concordance between two caregivers of the same child were examined. We further aimed to present population‐based norms. Additionally, convergent validity was examined with the use of the Attachment Q‐Sort (AQS; Waters & Deane, 1985) and the Emotional Availability Scales fourth edition (EAS; Biringen, 2008).
Concurrent validity of the ARI‐CP was examined by assessing the correlations of the ARI‐CP and instruments that measure related constructs. First, the associations between the ARI‐CP and children's psychopathology were studied, because there is empirical evidence showing that the quality of the attachment relationship is associated with psychopathology (Colonnesi et al., 2011; Madigan et al., 2016; Spruit et al., 2020). Second, we assessed the association between the ARI‐CP 2–5 and the general attachment representation of the caregivers, because previous research showed intergenerational transmission of attachment patterns (Verhage et al., 2016). Third, we examined the association between the ARI‐CP 2–5 and caregivers’ mind‐mindedness, that is, the caregivers’ capacity to represent and treat the child taking into consideration his or her thoughts and emotions (Meins, 2013). Secure attachment and mind‐mindedness have been shown to be positively correlated, meaning that parents’ representations of the child enhance a secure attachment relationship (Zeegers, Colonnesi, Stams, & Meins, 2017). Moreover, we tested differences in the ARI‐CP 2–5 between a clinical and general population, because we would expect higher insecure and lower secure attachment scores in the clinical population (Van IJzendoorn, Scheungel, & Bakermans‐Kranenborg, 1999; Wissink et al., 2016). Finally, the predictive validity of the ARI‐CP 2–5 was calculated based upon observed measures of the quality of the attachment relationship (with the AQS and EAS) to test the ability of the ARI‐CP 2–5 to correctly differentiate between those dyads that have been identified by the AQS and the EAS as secure and insecure attachment relationships.
2. METHODS
2.1. Participants
In total, 509 Dutch caregivers participated in the survey study. This sample consisted of 63 caregiver pairs who filled in the survey about the same child. To avoid dependent data structures, one caregiver in each pair was randomly excluded. The final sample consisted of 446 caregivers, including 211 fathers (47.3%) and 235 (52.7%) mothers. The sample consisted of caregivers from a general population (n = 378; 84.8%) and a clinical population (n = 68; 15.2%). The mean age of the caregivers was 35.8 (SD = 5.9) years old. The majority of the sample consisted of biological parents (93.5%), and the rest of the sample consisted of adoptive, foster‐, or step‐parents (6.5%). On average, the children had been placed under the caregiver's care for 2.24 years, with a minimum of 2 months and a maximum of 5 years and 9 months. The children of whom the caregivers filled in the questionnaires consisted of 225 (50.4%) boys and 221 (49.6%) girls. The age ranged from 2 to 5 and the mean age of the children was 3.7 (SD = 1.10) years.
A subsample of 83 caregivers from the survey study also participated in the observation study. The main aim of the observation study was to examine the convergent validity of the ARI‐CP 2–5 years. This subsample consisted of 15 caregivers (17.9%) who belonged to the clinical population and 68 caregivers (81.9%) to the general population. The observation sample contained 39 fathers (46.4%) and 44 (53.6%) mothers. The mean age of the caregivers was 36.3 (SD = 7.10) years old. The majority of the observation study sample consisted of biological parents (94.0%), and the rest of the sample consisted of adoptive, foster‐, or step‐parents (6.5%). The children in the observation study were 42 (51.2%) boys and 41 (48.8%) girls. The mean age of the children was 3.6 (SD = 1.1) years old. The two subsamples (those parents who only participated in the survey study vs. those who participated in the survey study and the observation study) did not significantly differ on population type (clinical vs. general population) (x 2 = .546), caregiver's sex (x 2 = .032), caregiver's relationship to the child (x 2 = .598), child's sex (x 2 = .023), age of the caregiver (t = –0.868), or age of the child (t = 0.998).
Finally, we performed analyses on the dependent data sample of 63 caregiver pairs, which consisted of 64 mothers and 62 fathers, with a mean age of 36.1 (SD = 5.0) years old. In total, 47 (74.6%) pairs belonged to the general population and 16 (25.4%) pairs belonged to the clinical population. The caregivers reported on 35 (55.6%) boys and 28 (44.4%) girls.
2.2. Procedure
The clinical sample was recruited through organizations for youth (mental health) care. The staff members of these facilities reached out to the caregivers of the 2 to 5 year olds who were referred to their facility, and asked if they were willing to participate in the current study. Caregivers in the general population sample were recruited through social media, child care centers, kindergarten, and schools. After being informed about the study and giving consent to use their anonymous data for the current study, the caregivers filled out the questionnaires, which took them approximately 30 min. At the end of the survey, caregivers could leave their email address to receive a 10‐euro gift card. Additionally, they were asked if they were willing to participate in the observation study.
The observation study consisted of 1.5‐hr home visits by research assistants. Once the caregivers had filled out the questionnaires and expressed their interest in the home visit, the home visits were planned as soon as possible. There was an average of 42 (SD = 23.5) days between filling in the questionnaires and the home visits. The home visits were recorded on video and consisted of naturalistic observations, a minimum of 20‐min free play between the caregiver and the child, and a 2‐min separation–reunion procedure. The caregivers were informed about the study while planning the home visit over the phone. At the start of the home visit, the research assistants explained the purpose and procedures, and informed consent of the caregivers was obtained. At the end of the home visits, the caregivers received a gift card of 40 euros. The current study was approved by the ethical committee of the Faculty of Social and Behavioral Sciences at the University (Blinded for review) (2017‐CDE‐7943).
2.3. Measures
2.3.1. The ARI‐CP 2–5
The process that led to the development of the ARI‐CP consisted of two paths: gathering examples of frequently occurring manifestations of secure and insecure attachment relationships and examining experiences with an existing caregiver report, the Attachment Insecurities Screening Inventory 2–5 years (AISI 2–5; Wissink et al., 2016), to create an improved instrument. The AISI 2–5 is a 20‐item parent report, aimed to measure attachment insecurity in 2–5 year olds, with the use of three insecure attachment subscales (avoidant, ambivalent, and disorganized attachment) and a total insecurity scale.
To gather manifestations of secure and insecure attachment relationships and learn from clinical experiences with the AISI 2–5, four focus groups with 24 professionals working in clinical practice with families were held. Further, 26 professionals who frequently used the AISI 2–5 filled in a survey about their experiences with the AISI 2–5. Moreover, interviews with five clinical attachment experts and 32 parents were conducted. These studies led to the understanding that the AISI 2–5 is providing in a clinical need for practical attachment instruments, but that there is also room for improvement. Furthermore, the construct needed to be more carefully formulated. It was recommended to clearly specify that a caregiver report measures the perception of the caregiver with regard to attachment problems. Further, it was advised to shift from a focus on child attachment behaviors to a more dyadic focus, in which the caregivers’ attachment‐related cognitions and experiences about the relationship with the child also have a place. Finally, the addition of a secure scale was recommended. These recommendations formed the basis for the development of the ARI‐CP 2–5.
The first step was the creation of an item pool of the ARI‐CP 2–5 using the manifestations of secure and insecure attachment relationships between caregivers and their young child that were collected in the focus groups with professionals and interviews with clinical attachment experts and caregivers. Subsequently a few items were added based on recent literature on attachment relationships. This process resulted in a list of 160 potential items for the ARI‐CP 2–5.
The second step was the selection of the best 86 items out of the 160 potential items, based on clinical and theoretical insights, and considerations derived from research on the construction of questionnaires. This 86‐item pilot version of the ARI‐CP 2–5 was then distributed among 112 Dutch caregivers from a general and clinical population, and subsequently analyzed for the purpose of item reduction. Several indicators played a role in selecting the items, such as the opinion of the caregivers about items, measures of dispersion, skewness, and internal consistency, Principal Component Analyses, Confirmative Factor Analyses, and the authors impressions of face and construct validity. In total, 30 items were removed from the 86‐item version, two items were altered in formulation, and 10 new items were added, which resulted in a second pilot version of the ARI‐CP 2–5 of 66 items.
In the third step, the data of the current study were used for purposes of item reduction. We used measures of dispersion, skewness, and internal consistency, Principal Component Analyses, Confirmative Factor Analyses, requested modification indices in R using the lavaan‐package to examine the possibility of cross‐loading items, and impressions of face and construct validity to remove an additional 18 items, resulting in the final 48‐item ARI‐CP 2–5.
The final ARI‐CP 2–5 contains 48 5‐point Likert‐type items (does not apply at all to fully applies) assessing the perceptions of caregivers about the attachment relationship with their child. The ARI‐CP 2–5 contains items on the thoughts, feelings, and behaviors of caregivers and their children. The items belong to either the Secure (13 items), Avoidant (11 items), Ambivalent (11 items), or Disorganized (13 items) attachment scale (see the Appendix [Supporting Information]). Scale scores represent the sum scores of all items of the scale.
The ARI‐CP 2–5 was developed in Dutch. Appendix A (Supporting Information) shows the English translation of the ARI‐CP 2–5. Two bilingual researchers (not involved in the development of the ARI‐CP 2–5) independently translated the ARI‐CP 2–5 from Dutch to English. Together with the first author, they discussed and resolved discrepancies. Next, two other bilingual researchers independently translated the English translation back into Dutch. Discrepancies were discussed and resolved. Finally, the first and last author compared the resulting Dutch version to the original Dutch version, and discussed and resolved discrepancies.
2.3.2. Strengths and Difficulties Questionnaire
The parent‐report Strengths and Difficulties Questionnaire (SDQ; Goodman, 2001; Van Widenfelt, Goedhart, Treffers, & Goodman, 2003) is a brief behavioral screening questionnaire for parents of preschoolers to adolescents up to 16 years old. The SDQ contains 25 items with positive and negative attributes. The caregivers used 3‐point Likert‐type scales to indicate to what extent each attribute applied to their preschool‐aged child. With the SDQ, four domains of psychopathological symptoms were assessed: emotional symptoms, conduct problems, hyperactivity/inattention, and peer problems. Additionally, there is a fifth domain on prosocial behavior. The four domains of psychopathological symptoms can also be summed to generate a total score for psychopathology. The validity and reliability of the SDQ were established to be satisfactory (Goodman, 2001; Muris, Meesters, & van den Berg, 2003; Stone, Otten, Engels, Vermulst, & Janssens, 2010). The Cronbach's alphas in the current study were .67 for Emotional problems, .68 for Conduct problems, .77 for Hyperactivity/inattention, .59 for Peer problems, .68 for Prosocial behavior, and .82 for Total problems.
2.3.3. Relationship Questionnaire
The attachment representation of the caregivers was assessed using the Relationship Questionnaire (RQ; Bartholomew & Horowitz, 1991; Spruit & Meesters, 2018). The RQ consists of four vignettes, each describing an attitude toward relationships in general: security, preoccupation, dismissing‐avoidance, and fearful‐avoidance. Participants rated the level in which each description applies to them on a 7‐point scale (does not apply at all to fully applies). The Relationship Questionnaire as a measure of adult attachment has been widely used and has shown sufficient concurrent validity as assessed with measures of interpersonal functioning (Bartholomew & Horowitz, 1991) and behavioral and personality characteristics (Klohnen & Bera, 1998).
2.3.4. Mind‐Mindedness Interview
Caregivers’ mind‐mindedness was assessed with the Mind‐Mindedness Interview (Meins, Fernyhough, Russell, & Clark‐Carter, 1998). Caregivers completed the describe‐your‐child measure. The interviews were coded following the manual of Meins and Fernyhough (2015). Caregivers’ descriptions of their child were divided into discrete sentences and each sentence was categorized as follows: mind‐related descriptions (i.e., mental descriptions, interests, preferences, needs, desires, and emotions), behavior descriptions (i.e., behavioral, physical, or general descriptions), or general comments (i.e., about other or related topics in which no description of the child was provided). The emotional valence of each mind‐related description was classified as either positive, negative, or neutral, based on the comments itself (Demers, Bernier, Tarabulsy, & Provost, 2010). Parents’ positive mind‐mindedness reflects their representation of the child's mental states as proper for a healthy and adaptive development (i.e., “he likes the company of other children,” “she is curious,” “he is often very happy”). Conversely, parents’ negative mind‐mindedness is a manifestation of their representation of the child's mind in terms of worries, frustration, and consciousness of the child's difficulties (i.e., “he is often worried,” “she can be egoistic,” “he doesn't like others’ attention”). Parents’ mind‐related description with no specific positive or negative valence was classified as neutral (i.e., “he has a strong will,” “she doesn't like to be the first one,” “he is a perfectionist”). Parents’ positive and neutral mind‐related comments were combined, whereas negative mind‐related descriptions were analyzed separately. A total score of mind‐mindedness (including positive/neutral and negative description) was also included as general capacity of mentalization. Mind‐mindedness scores were the numbers of mental descriptors expressed as a proportion of the total number of descriptors used in order to control for differences in caregivers’ verbosity.
Scores for the total mind‐mindedness and for the two valences were computed as proportions of the total amount of comments parents made (Meins & Fernyhough, 2015). Trained coders (n = 5) independently rated the interviews and 15% (n = 67) was randomly selected to calculate the interrater agreement among the coders. Interrater agreement on the proportion of mind‐related comments per transcript was good (ICC = .96) and for the coding of the valance of positive/neutral, and negative comments interrater agreement was also substantial (ICCs = .95 and .91, respectively).
2.3.5. Attachment Q‐Sort
The Attachment Q‐Sort (AQS; Waters & Deane, 1985) assesses attachment security of children between 1 and 5 years old (secure‐base behavior) and contains 90 items. The 90 items are sorted in nine clusters of items containing 10 items each. Attachment scores are calculated by computing the correlation between the observer sort and a criterion sort of the prototypically secure child (the cutoff scores of Park and Waters [1989], Waters & Deane [1985]). A score below the cutoff indicates a lack of attachment security. For the current study were used: for boys a score below .25 and for girls a score below .36 is perceived as a lack of attachment security. Research into the validity of the attachment Q‐sort showed satisfactory convergent, discriminant, and predictive validity (Van Ijzendoorn, Vereijken, Bakermans‐Kranenburg, & Riksen‐Walraven, 2004). The AQS was sorted by trained researchers, and 11% of the cases (n = 9) were double‐coded. The ICC of the continuous AQS rating between the researchers in the current study was .76, which is indicative of good interrater agreement (Koo & Li, 2016).
2.3.6. Emotional Availability Scales
The EAS fourth edition (Biringen, 2008) assesses the affective quality of the caregiver–child relationship. In the current study, the caregiver component “Adult sensitivity” and the child component “Child responsiveness to the adult” were used. The EAS Adult sensitivity measures an attachment‐based quality and refers to the emotional and behavioral sensitivity and responsiveness to the child's needs. The EAS Child responsiveness to the adult measures the child's emotional and social responsiveness toward the caregiver and reflects attachment security. Both scales can be rated from one to seven (with the highest score indicative of optimal sensitivity/responsiveness). Scores equal or below 5.0 were indicative of insecure attachment relationships. The EAS proved to have sufficient reliability and validity (Biringen et al., 2014). All coders (first, second, and fifth author) completed the mandatory online training by Zeynep Biringen and showed satisfactory interrater agreement with Zeynep Biringen. In total, 11% of the cases (n = 9) were double‐coded. The ICC between the coders in the current study was .77 for Adult sensitivity and .87 for Child responsiveness to the adult.
2.4. Analyses
First, the internal structure of the four‐factor ARI‐CP 2–5 was determined by means of a confirmatory factor analysis (CFA) in R version 3.6.1, using the lavaan‐package (Rosseel, 2012). Fit indices were used to test model fit in the CFA‐model. The following cutoff values are indicative of acceptable model fit: RMSEA < .06, CFI > .90, TLI > .95, and GFI > .90 (Hu & Bentler, 1999). Moreover, we have tested three alternative models that have some theoretical basis. The first model was a one‐factor overall attachment model, with all the items of the ARI‐CP 2–5 loading on one factor. The second alternative model was a two‐factor secure/insecure model, with the Secure scale as one factor and the Avoidant, Ambivalent, and Disorganized scales combined in another factor. The third alternative model was a two‐factor organized/disorganized model, with the Secure, Avoidant, and Ambivalent scale combined in one factor and the Disorganized scale as the other factor. The last alternative model was a three‐factor secure/organized‐insecure/disorganized model, with the Secure scale as one factor, the Avoidant and Ambivalent scale combined in the organized‐insecure factor, and the Disorganized scale as one factor.
Next, with multigroup CFA, measurement invariance of the instrument was examined across mothers and fathers, boys and girls, 2‐ to 3‐year olds, and 4‐ and 5‐year olds, as well as across families from a general population sample and a clinical sample in R version 3.6.1, using the semTools‐package and measEq.syntax (Jorgensen, Pornprasertmanit, Schoemann, & Rosseel, 2018). It was first tested whether the common factors of the ARI‐CP 2–5 were associated with the same items across groups (configural invariance; Gregorich, 2006). The fit of the configural model was tested using the Hu and Bentler (1999) cutoff scores. Second, because the ARI‐CP 2–5 produces ordinal data, the thresholds structure was modeled following instructions of Wu and Estabrook (2016). Third, it was examined whether the common factors have the same meaning across groups, by testing whether the factor loadings were equal across groups (metric invariance; Gregorich, 2006). Finally, it was examined whether comparisons of group means across groups are meaningful, by testing whether factor intercepts were equal across groups (scalar invariance; Gregorich, 2006). Any significant decrease of model fit (based on a drop in CFI greater than .005) indicates that the more stringent condition of measurement invariance for that model has not been met.
Next, reliability information of the four subscales was examined, by calculating ordinal Cronbach's alphas for each ARI‐CP 2–5 scale in R using the userfriendlyscience package (Peters, 2018). Moreover, we examined the concordance on the ARI‐CP 2–5 between two caregivers of the same child by calculating Pearson correlation coefficients. We did not expect high correlations between two caregivers of the same child, because they both reported on a different relationship. We further created population‐based norms, based on T‐score distribution in the general population in the current study. T‐scores < 30 were defined as low, between 30 and 40 as below average, between 40 and 60 as average, between 60 and 70 as above average, and scores >70 as high scores. For the insecure scales of the ARI‐CP 2–5 years, above average and high scores were labeled as indicative of perceived attachment relationship insecurity. For the secure scale, below average and low scores were labeled as indicative of perceived attachment relationship insecurity.
Concurrent validity was studied by computing correlations between the latent factors of the ARI‐CP 2–5 (extracted from the CFA) and the SDQ, RQ, and the MMI. Finally, in studying the concurrent validity, we tested differences on the ARI‐CP 2–5 scales between the clinical and general population using ANCOVA. Additionally, convergent validity was examined by computing the correlations between the ARI‐CP 2–5 scales and the AQS and EAS in SPSS version 25. In the analyses to test concurrent and convergent validity, one‐sided p‐values were used. The predictive validity of the ARI‐CP 2–5 was then examined by calculating the sensitivity, specificity, false‐positives, false‐negatives, and total correct predictions based upon the cutoff scores of the AQS and EAS to test the ability of the ARI‐CP 2–5 to correctly identify those dyads with and without problems within the attachment relationship.
3. RESULTS
3.1. Internal structure
The assumed four‐factor model of the ARI‐CP 2–5 was tested in the survey dataset (N = 446), by means of a CFA (see Figure 1). All fit indices of the tested model—χ 2 (df) = 2,622.07 (1,074), RMSEA = 0.057, CFI = 0.960, TLI = 0.958, and GFI = 0.962—indicate sufficient model fit according to the guidelines of Hu and Bentler (1999). We did not allow for any error terms to covary. Some items have factor loading of <.30. Removal of these items resulted in a worse model fit, therefore, these items were kept.
FIGURE 1.
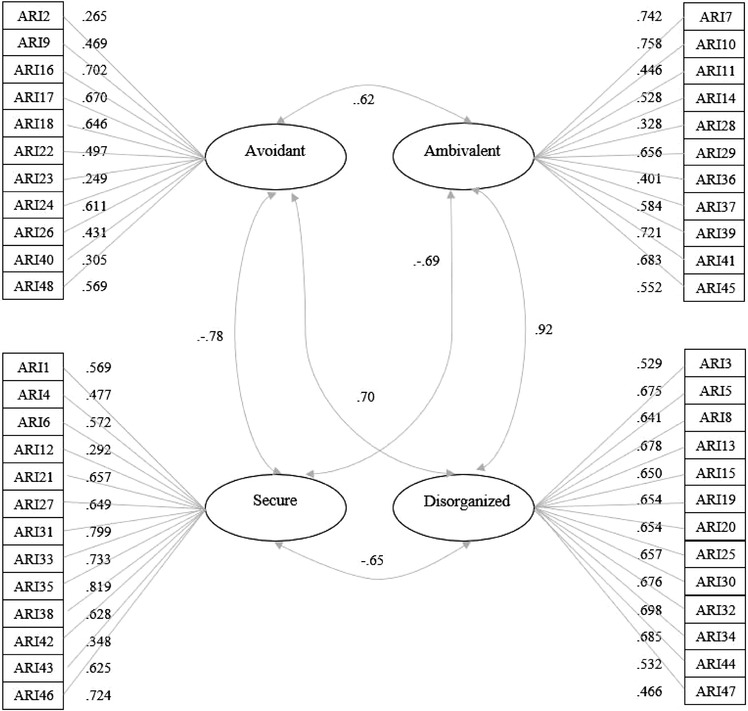
Internal structure of ARI‐CP 2–5
Moreover, we tested three alternative model structures. The first alternative model was a one‐factor structure, with all items included in one overall attachment factor. The one‐factor model resulted in a worse model fit than the assumed four‐factor model, χ 2 (1,080) = 2,921.82, RMSEA = 0.074, CFI = 0.933, TLI = 0.930, and GFI = 0.946. The second alternative model was the two‐factor secure/insecure model, which produced the following fit indices: χ 2 (1,079) = 2,555.75, RMSEA = 0.065, CFI = 0.948, TLI = 0.946, and GFI = 0.955. The third alternative model was the two‐factor organized/disorganized model, which produced the following fit indices: χ 2 (1,079) = 2,555.75, RMSEA = 0.071, CFI = 0.938, TLI = 0.935, and GFI = 0.950. The final alternative factor was the three‐factor secure/organized‐insecure/disorganized, with χ 2 (1,077) = 2,490.69, RMSEA = 0.063, CFI = 0.951, TLI = 0.949, and GFI = 0.957. All alternative models had a worse fit than the assumed four‐factor model. Therefore, we continued with the four‐factor model.
3.2. Measurement invariance
Next, we tested for measurement invariance between fathers (N = 211) and mothers (N = 235), boys (N = 225) and girls (N = 221), 2 to 3‐year olds (N = 259), and 4‐ to 5‐year olds (N = 186), as well as across families from a general population sample (N = 378) and a clinical sample (N = 68). We started with testing whether the configural models for each multigroup CFA would have sufficient model fit. Each step afterward (thresholds model, loadings, and intercepts model) had more stringent requirements for measurement invariance. Table 1 presents the results of the measurement invariance analyses.
TABLE 1.
Results of the measurement invariance analyses (N = 446)
| Type measurement invariance | x 2(df) | RMSEA | CFI | TLI | GFI |
|---|---|---|---|---|---|
| Sex caregivers | |||||
| Configural | 3,232.909 (2,148) | 0.057 | 0.962 | 0.960 | 0.944 |
| Thresholds | 3,296.824 (2,214) | 0.056 | 0.963 | 0.962 | 0.943 |
| Loadings | 3,303.467 (2,258) | 0.057 | 0.060 | 0.960 | 0.941 |
| Intercepts | 3,323.788 (2,302) | 0.058 | 0.958 | 0.959 | 0.939 |
| Sex child | |||||
| Configural | 3,227.469 (2,148) | 0.057 | 0.963 | 0.961 | 0.943 |
| Thresholds | 3,289.207 (2,214) | 0.056 | 0.963 | 0.963 | 0.942 |
| Loadings | 3,293.383 (2,258) | 0.057 | 0.961 | 0.961 | 0.940 |
| Intercepts | 3,308.695 (2,302) | 0.058 | 0.959 | 0.960 | 0.938 |
| Age child | |||||
| Configural | 3,161.311 (2,148) | 0.054 | 0.964 | 0.963 | 0.946 |
| Thresholds | 3,217.816 (2,206) | 0.053 | 0.965 | 0.964 | 0.945 |
| Loadings | 3,193.690 (2,250) | 0.053 | 0.965 | 0.964 | 0.944 |
| Intercepts | 3,224.771 (2,294) | 0.054 | 0.962 | 0.963 | 0.942 |
| Population | |||||
| Configural | 3,090.036 (2,148) | 0.059 | 0.958 | 0.956 | 0.946 |
| Thresholds | 3,148.757 (2,211) | 0.057 | 0.959 | 0.958 | 0.945 |
| Loadings | 3,191.088 (2,255) | 0.060 | 0.955 | 0.955 | 0.943 |
| Intercepts | 3,204.557 (2,299) | 0.060 | 0.953 | 0.954 | 0.943 |
The configural model testing measurement invariance for sex of the caregiver showed sufficient model fit, indicating that the common factors of the ARI‐CP 2–5 were associated with the same items across mothers and fathers. Each following step resulted in a drop in CFI of less than .005, indicating that the more stringent requirements have been met. This means the common factors of the ARI‐CP 2–5 have the same meaning across mothers and fathers (metric invariance), and that group means can be meaningfully compared across mothers and fathers (scalar invariance). Additionally, the results indicate configural, metric, and scalar invariance for sex of the child, age of the child, and population type.
3.3. Reliability
We have tested the ordinal alphas for the ARI‐CP 2–5 scales. Ordinal alpha was .78 for Avoidant attachment, .89 for Secure attachment, .85 for Ambivalent attachment, and .89 for Disorganized attachment. The internal consistency of the ARI‐CP 2–5 scales was therefore sufficient.
3.4. Concordance between caregivers of the same child
The concordance between caregivers of the same child was examined in a subgroup of 63 caregiver pairs that filled out the ARI‐CP 2–5 about the same child. The correlations between caregivers of the same child on the Secure, Avoidant, and Ambivalent scale were significant, r = .42, p = .001; r = .42, p = .001; and r = .39, p = .002, respectively. The correlation between the caregivers of the same child of the Disorganized scale was not significant, r = .08, p = .557.
3.5. Population‐based norms
The norms of the ARI‐CP 2–5 (see Table 2) were based on the general population sample (n = 378) in the current study. This sample consisted of 378 caregivers. The sample consisted of 196 fathers (51.9%) and 182 (48.1%) mothers. The mean age of the caregivers was 35.5 (SD = 5.5) years old. The sample consisted of biological parents in 376 cases (99.5%), and two stepparents (0.5%). The children of whom the caregivers filled in the questionnaires consisted of 183 (48.4%) boys and 195 (51.6%) girls. The age ranged from 2 to 5 and the mean age of the children was 3.64 (SD = 1.08) years old. Based on the T‐scores in the general population sample, scale scores were converted into low, above average, average, above average, or high scores. For the insecure scales of the ARI‐CP 2–5 years, above average and high scores were labeled as indicative of perceived attachment relationship insecurity. For the Secure scale, below average and low scores were labeled as indicative of perceived attachment relationship insecurity. Based on these norms of the ARI‐CP 2–5, 62.1% of the total sample in the current study (N = 446) did not show an indication of perceived attachment relationship insecurity, and 37.9% of the total sample had indications of perceived attachment relationship insecurity. For the general population sample (n = 378), this was 66.1% and 33.9%, respectively, and for the clinical population sample (n = 68) 39.7% and 60.3%, respectively.
TABLE 2.
Population‐based a norms of the ARI‐CP 2–5
| Low | Below‐average | Average | Above‐average | High | |
|---|---|---|---|---|---|
| Secure | ≤46 | 47–51 | 52–61 | 62–65 | – |
| Avoidant | ≤11 | 12–15 | 16–24 | 25–28 | ≥29 |
| Ambivalent | ≤10 | 11–14 | 15–24 | 25–29 | ≥30 |
| Disorganized | ≤12 | 13–17 | 18–30 | 31–36 | ≥37 |
Normgroup consisted of N = 378 caregivers from the general population sample.
3.6. Concurrent validity
3.6.1. ARI‐CP and SDQ
Table 3 presents the associations between the latent factors of the ARI‐CP and the SDQ. As expected, significant correlations were found between the ARI‐CP 2–5 and measures of psychopathology and prosocial behavior, ranging from r = .28 (between ARI‐CP Avoidant factor and SDQ Emotional problems scale) to r = .70 (between ARI‐CP Disorganized factor and SDQ Total problems). All correlations were significant and in the expected direction.
TABLE 3.
Correlations between the latent factors of the ARI‐CP 2–5 and the SDQ (N = 446)
| SDQ total problems | SDQ emotional problems | SDQ hyperactivity | SDQ conduct problems | SDQ peer problems | SDQ prosocial behavior | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Secure | –.569 *** | (–.515 *** ) | –.357 *** | (–.339 *** ) | –.444 *** | (–.384 *** ) | –.437 *** | (–.380 *** ) | –.359 *** | (–.356 *** ) | .428 *** | (.421 *** ) |
| Avoidant | .543 *** | (.365 *** ) | .279 *** | (.109 * ) | .441 *** | (.328 *** ) | .460 *** | (.330 *** ) | .332 *** | (.236 *** ) | –.355 *** | (–.191 *** ) |
| Ambivalent | .694 *** | (.649 *** ) | .436 *** | (.461 *** ) | .553 *** | (.499 *** ) | .590 *** | (.504 *** ) | .351 *** | (.358 *** ) | –.410 *** | (–.402 *** ) |
| Disorganized | .696 *** | (.713 *** ) | .400 *** | (.406 *** ) | .559 *** | (.560 *** ) | .632 *** | (.687 *** ) | .337 *** | (.329 *** ) | –.387 *** | (–.367 *** ) |
Note. Zero‐order correlations between the ARI‐CP 2–5 scale scores and the SDQ between the brackets.
*** p < .001; * p < .05.
3.6.2. ARI‐CP and RQ
Table 4 shows the associations between the ARI‐CP 2–5 latent factors and the RQ. As expected, significant correlations were found between the ARI‐CP 2–5 and a measure of caregivers’ attachment representations, ranging from r = –.17 (between ARI‐CP Avoidant factor and RQ Secure score) to r = .31 (between ARI‐CP Disorganized factor and RQ Preoccupied score). All correlations were significant and in the expected direction.
TABLE 4.
Correlations between latent factors of the ARI‐CP 2–5 and the RQ scores (N = 446)
| RQ secure | RQ fearful | RQ preoccupied | RQ dismissing | |||||
|---|---|---|---|---|---|---|---|---|
| Secure | .195 *** | (.196 *** ) | –.242 *** | (–.210 *** ) | –.202 *** | (–.125 ** ) | –.260 *** | (–.257 *** ) |
| Avoidant | –.166 *** | (–.092 * ) | .206 *** | (.121 ** ) | .233 *** | (.124 ** ) | .245 *** | (.240 *** ) |
| Ambivalent | –.175 *** | (–.155 *** ) | .256 *** | (.262 *** ) | .304 *** | (.277 *** ) | .134 ** | (.094 * ) |
| Disorganized | –.164 *** | ( –.152 ** ) | .227 *** | (.206 *** ) | .311 *** | (.295 *** ) | .134 ** | (.119 ** ) |
Note. Zero‐order correlations between the ARI‐CP 2–5 scale scores and the RQ between the brackets.
*** p < .001; ** p < .01; * p < .05.
3.6.3. ARI‐CP and MMI
Table 5 presents the associations between the ARI‐CP 2–5 latent factors and the MMI scores. As expected, we found significant correlations in the expected direction between the ARI‐CP latent factors and positive/neutral caregivers’ mind‐mindedness, ranging from r = –.18 for the Avoidant and r = –.26 for the Ambivalent scale. Negative mind‐mindedness significantly correlated with the ARI‐CP 2–5 latent factors, ranging from r = .10 for the Avoidant and r = –.27 for the Ambivalent scale, all in the expected direction. The total mind‐mindedness score correlated significantly and in the expected direction with the ARI‐CP latent variables, ranging from r = .09 for the Disorganized and r = –.12 for the Avoidant factor.
TABLE 5.
Associations between the latent factors of the ARI‐CP 2–5 and the MMI scores (N = 446)
| Positive/neutral mind‐mindedness | Negative mind‐mindedness | Total mind‐mindedness | ||||
|---|---|---|---|---|---|---|
| Secure | .186 *** | (.200 *** ) | –.150 *** | (–.187 *** ) | .093 * | (.059) |
| Avoidant | –.183 *** | (–.139 ** ) | .104 * | (–.056) | –.115 ** | (–.097 * ) |
| Ambivalent | –.256 *** | (–.294 *** ) | .271 *** | (.281 *** ) | –.094 * | (–.094 * ) |
| Disorganized | –.243 *** | (–.284 *** ) | .259 *** | (.282 *** ) | –.088 * | (–.063) |
Note. Zero‐order correlations between the ARI‐CP 2–5 scale scores and the MMI between the brackets.
***p < .001; ** p < .01; * p < .05.
3.6.4. ARI‐CP and population type
As a final indication of convergent validity, we tested for differences on the ARI‐CP between the general population (n = 378) and a clinical sample (n = 68). We first checked for differences between the populations on sex of the caregivers, sex of the child, and age of the child. The clinical sample consisted of significantly more female caregivers (51.5% male in general population and 27.3% in clinical population; x 2 = 14.99; p < .000) and children were significantly older (M clinical = 3.64; M general = 4.20; t = –4.14; p < .000). Therefore, in the analyses, we controlled for sex of the caregiver and child's age. Table 6 shows the results of the analyses. Caregivers from the clinical population sample scored significantly lower on the Secure scale (d = 0.60) and significantly higher on the Avoidant (d = 0.32), Ambivalent (d = 0.63), and Disorganized (d = 0.57) scale.
TABLE 6.
Differences on the ARI‐CP 2–5 scales between the clinical and general population sample (N = 446)
| M (SD) clinical sample | M (SD) general population sample | F a | d | |
|---|---|---|---|---|
| Secure | 53.59 (7.21) | 56.55 (4.96) | 22.91 *** | 0.60 |
| Avoidant | 21.25 (5.79) | 20.20 (4.28) | 6.62 ** | 0.32 |
| Ambivalent | 22.54 (6.78) | 19.23 (4.86) | 25.09 *** | 0.63 |
| Disorganized | 28.00 (9.26) | 23.99 (6.12) | 20.99 *** | 0.57 |
Controlled for sex of caregiver and age of child.
***p < .001; ** p < .01.
3.7. Convergent validity
Table 7 presents the associations between the ARI‐CP 2–5 scales and the AQS, EAS Adult Sensitivity, and EAS Child Responsiveness. We used both the continuous ARI‐CP scale scores and the dichotomous ARI‐CP scale scores based on the cutoff scores (indication of perceived attachment insecurity or not). Although the continuous scores will probably be used more often in research, the cutoff can be relevant scores for clinical.
TABLE 7.
Correlations between ARI‐CP 2–5 scales and ARI‐CP insecure attachment relationship indication and the AQS and EAS (N = 83)
| AQS | EAS child responsiveness | EAS adult sensitivity | |
|---|---|---|---|
| Secure | .286 * (–.274 ** ) | .236 * (–.163) | .220 * (–.138) |
| Avoidant | –.045 (–.173) | –.001 (–.182 * ) | –.028 (–.158) |
| Ambivalent | –.176 (–.308 ** ) | –.119 (–.302 ** ) | –.066 (–.195 * ) |
| Disorganized | –.195 * (–.303 ** ) | –.210 * (–.435 *** ) | –.142 (–.376 *** ) |
| Indication of perceived attachment relationship insecurity based on all scales | (–.295 ** ) | (–.362 *** ) | (–.333 ** ) |
Note. The correlations in the brackets represent point biserial correlations, based on the cutoff scores of the ARI‐CP scales (0 = no indication of perceived attachment relationship insecurity, 1 = indication of perceived attachment relationship insecurity).
***p < .001; ** p < .01; * p < .05.
We first calculated the Pearson correlations between the continuous ARI‐CP scale scores and the AQS and EAS. The ARI‐CP 2–5 Secure scale correlated significantly and in the expected direction with the AQS, EAS Adult Sensitivity, and EAS Child Responsiveness. In other words, caregivers reporting more secure attachment relationships also showed more sensitivity, and their children showed more secure attachment behavior and more responsiveness. The ARI‐CP 2–5 Disorganized scale correlated significantly and in the expected direction with the AQS and the EAS Child Responsiveness, but not with the EAS Adult Sensitivity. The ARI‐CP 2–5 Avoidant and Ambivalent scales did not show significant associations with the observation measures.
Next, we computed the point biserial correlations between the ARI‐CP cutoff scores for perceived attachment relationship insecurity and the three observation measures. Whether the Secure scale indicated perceived attachment relationship insecurity or not was significantly associated with the AQS and EAS Child Responsiveness. For the Avoidant scale, the perceived attachment relationship insecurity indication was significantly correlated to the EAS Child Responsiveness. The dichotomous indication of perceived attachment relationship insecurity (yes or no) for the Ambivalent, Disorganized, and all ARI‐CP scales combined showed significant correlations with all of the observation measures.
3.8. Predictive validity
The predictive validity of the ARI‐CP 2–5 was examined by comparing the ARI‐CP 2–5 Indication of perceived attachment relationship insecurity (i.e., above average and high scores on the insecure scales or below average and low scores on the Secure scale) with the indications of attachment problems based on the cutoff points of the AQS and EAS (see Table 8). The sensitivity of the ARI‐CP 2–5 ranged from 80.0% to 83.6%, depending on the specific observation measure. The specificity ranged from 53.6% to 60.7%. The number of false‐positives ranged from 10.8% to 13.3%. The number of false negatives ranged from 13.3% to 15.7%. Finally, the total number of correct prediction of the ARI‐CP, based on the AQS and EAS, ranged from 71.1% to 75.9%.
TABLE 8.
Predictive validity of the ARI‐CP 2–5
| AQS | EAS responsiveness | EAS sensitivity | |
|---|---|---|---|
| Sensitivity | 80.0% | 83.6% | 81.5% |
| Specificity | 53.6% | 60.7% | 55.2% |
| False‐positives | 13.3% | 10.8% | 12.0% |
| False‐negative | 15.7% | 13.3% | 15.7% |
| Total correct prediction | 71.1% | 75.9% | 72.3% |
4. DISCUSSION
The present study aimed to develop and subsequently test the validity and reliability of the ARI‐CP 2–5 in a sample of N = 446 caregivers from a general and clinical population sample, and to develop norms of the ARI‐CP based on the general population sample. The ARI‐CP 2–5 was developed to measure the caregiver's perception of the attachment relationship with their 2‐ to 5‐year‐old child. The theoretically based factor model of the ARI‐CP with the four types of attachment relationships (secure, insecure‐avoidant, insecure‐ambivalent, and insecure‐disorganized) was confirmed in a CFA, indicating construct validity of the ARI‐CP 2–5. Further, configural, metric, and scalar measurement invariance of the ARI‐CP were found across mothers and fathers, boys and girls, 2‐ to 3‐year olds, and 4‐ to 5‐year olds, as well as across families from a general and clinical population sample. This means that the common factors of the ARI‐CP were associated with the same items across the groups, and indicates that the common factors of the ARI‐CP 2–5 have similar meaning across the groups, and that group means can be compared in a meaningful way across the groups (Gregorich, 2006). The assumption of measurement invariance is important, because otherwise it is unclear whether differences among groups reflect actual differences or by differences between groups in how the items are interpreted. The scales of the ARI‐CP showed sufficient internal consistency, with the ordinal alphas ranging from .78 for the Avoidant scale and .89 for the Secure and Disorganized scales, suggesting that the ARI‐CP had acceptable reliability.
We then tested the concurrent validity of the ARI‐CP 2–5, by calculating the correlations between the ARI‐CP 2–5 scales and measures of child's psychopathology. All of the correlations between the ARI‐CP 2–5 scales and the SDQ as a measure of child's psychopathology were significant, ranging from small to large effect sizes. This is in line with the large amount of meta‐analytical studies that have showed clear associations between the quality of attachment relationships and child's psychopathology (Colonnesi et al., 2011; Madigan et al., 2016; Spruit et al., 2020). The associations between the ARI‐CP 2–5 and the SDQ are rather large, which can be explained by meta‐analytic evidence, showing that disorganized attachment has the largest association to psychopathology in general, compared to the other attachment relationship types (Madigan et al., 2016; Spruit et al., 2020). Moreover, in the current study, associations may be elevated by the cross‐sectional design, common methods, and shared informants approach.
The next indication of concurrent validity comes from the associations between the ARI‐CP 2–5 and a measure of caregivers’ general attachment representations, the RQ. Significant correlations were found between the ARI‐CP 2–5 and the RQ, ranging from small to moderate associations. Because previous studies showed a clear generational transmission of the quality of attachment relationships with small to moderate effect sizes (Verhage et al., 2016), the small to moderate associations between the caregivers’ perceptions of the attachment relationship with their child and the caregivers’ general attachment representations are an indication of concurrent validity.
Further, we assessed concurrent validity of the ARI‐CP 2–5 by examining the associations between the ARI‐CP 2–5 latent variables and a measure of caregivers’ mind‐mindedness. As expected, the Secure factor was positively related to positive/neutral mind‐mindedness and total mind‐mindedness, and negatively related to negative mind‐mindedness. This is in line with previous research showing that parents’ use of positive mind‐related descriptions of their child is positively associated with a more sensitive behavior and state of mind and parents’ stress and negatively related to parents’ perception of their child's negative temperament stress (Demers et al., 2010; McMahon & Meins, 2012), confirming the idea that caregivers with better mentalizing capacities are able to create more secure attachment relationships with their child. The Ambivalent, Avoidant, and Disorganized factors were positively related to negative mind‐mindedness and negatively to positive/neutral mind‐mindedness. These results show that caregivers with more negative mind‐mindedness also perceive more insecurity in the attachment relationship with their child, which is in line with expectations (e.g., see Powell et al., 2013).
The final indication for concurrent validity comes from comparing the ARI‐CP scores between caregivers from the general and clinical population sample. Caregivers from the clinical population sample perceived the attachment relationship with their child as less secure (d = 0.60) and more avoidant (d = 0.32), ambivalent (d = 0.63), and disorganized (d = 0.57). This is conform expectations, because caregiver–child dyads with developmental, mental health, or child rearing problems generally have more insecurities within the attachment relationship (Van IJzendoorn et al., 1999; Vasileva & Petermann, 2018), suggesting concurrent validity of the ARI‐CP 2–5.
To test the convergent validity of the ARI‐CP 2–5, we examined the associations between the ARI‐CP 2–5 and observational measures of attachment. The continuous ARI‐CP Secure scale showed significant small‐to‐moderate correlations with all observation measures (r ranged from .22 to .29), and for the continuous ARI‐CP 2–5 Disorganized scale, these were small‐to‐moderate correlations between the AQS (r = –.20) and EAS Child Responsiveness (r = –.21). No significant associations between the continuous Avoidant and Ambivalent scales and the observational measures were found. All dichotomous indications of perceived attachment relationship insecurity (yes or no) of the ARI‐CP correlated significantly with at least one observational measure, ranging from r = –.138 (ns.) between the Secure scale and EAS Adult Sensitivity and r = –.435 (p < .001) between the Disorganized scale and EAS Child Responsiveness. Thus, the results suggest partial evidence for the convergent validity of the continuous ARI‐CP 2–5 scales and full convergent validity of the dichotomous cutoff scores of the ARI‐CP 2–5.
We would not expect perfect correlations between the ARI‐CP 2–5 and observational measures of attachment. For example, Hendriks, Van der Giessen, Stams, and Overbeek (2018) found in a comprehensive meta‐analysis a small, yet significant correlation of r = .17 for parent‐reported and observed parenting. The authors conclude that this provides evidence that parent reports and observational measures assess the same underlying construct, indicating convergent validity. They just measure a different aspect of the underlying construct (i.e., perceptions vs. visible behaviors; Hendriks et al., 2018). We believe that there is enough shared variance between the ARI‐CP 2–5 and the AQS and EAS to conclude that this argumentation is applicable to the current study as well: the ARI‐CP 2–5 and the AQS and EAS measure overlapping, but different aspects of the same attachment relationship construct.
Notably, even the well‐validated SSP and AQS (both observational attachment measures) showed an association between them of “only” r = .31 (Van Ijzendoorn et al., 2004). Next to the perceptions versus visible behavior distinctions, unique variance between the ARI‐CP and AQS and EAS can also be explained by other factors. For instance, the AQS and EAS were sorted and coded based on one home visit and are therefore just a momentary recording, whereas the ARI‐CP 2–5 is supposed to provide a more general picture of the caregivers’ perception of the attachment relationship. Moreover, the EAS and AQS scores were based on behavior within the home environment, whereas using the ARI‐CP 2–5, the caregiver is able to provide their perceptions of the attachment relationship across multiple settings and contexts. We therefore conclude that there is enough evidence suggesting convergent validity for the continuous Secure and Disorganized scale and all of the dichotomous indications of perceived attachment relationship insecurity of the ARI‐CP scales.
Moreover, the current study suggests sufficient predictive validity of the ARI‐CP 2–5 indication of perceived attachment insecurity, expressed by the sensitivity (ranging from 80% to 84%), specificity (54% to 61%), percentage of false‐negatives (13% to 16%), percentage of false positives (11% to 13%), and the percentage of overall correct predictions (71% to 76%) based on the AQS and EAS cutoff scores. For screening purposes, high sensitivity (i.e., the chance that “insecure” attachment relationships are correctly identified as such by the ARI‐CP 2–5) is considered to be more important than high specificity (i.e., the chance that “secure” attachment relationships are correctly identified as such by the ARI‐CP 2–5). Therefore, we believe that the predictive validity of the ARI‐CP 2–5 is satisfying.
The scores of caregivers of the same child on the Secure, Avoidant, and Ambivalent scales were significantly and moderately associated, suggesting concordance of the perceptions of the attachment relationship between caregivers of the same child. This is in line with previous meta‐analytic evidence showing concordance in secure, insecure‐avoidant, and insecure‐ambivalent attachment classifications based on the SSP between fathers and mothers (Fox, Kimmerly, & Schafer, 1991). No significant correlation was found for the Disorganized scale. This might indicate that the Disorganized ARI‐CP 2–5 scale reflects the perceptions of the unique attachment relationship every caregiver has with a child, and is not very affected by shared factors between caregivers, including characteristics of the child or systemic factors, such as family stress.
We created norms based on the general population sample (n = 378). Using the T‐scores within the norm group, scale scores of the ARI‐CP 2–5 were converted into low, below average, average, above average, or high scores. Moreover, we determined that for the Secure scale, below average and low scores were indicative of perceived attachment relationship insecurity. For the insecure scales, above average and high scores were labeled as indicative of perceived attachment relationship insecurity. The prevalence of perceived attachment relationship insecurity based on the ARI‐CP 2–5 in the general population sample was 33.9% and in the clinical population sample 60.3%, which is conform expectations based on the attachment distributions reported in Van IJzendoorn et al. (1999).
The current study has some limitations that need to be mentioned. First, in examining the convergent validity of the ARI‐CP 2–5 we ideally would have used an attachment instrument that would be able to differ between the different types of attachment relationships. Currently, we have used the AQS and EAS, which consist of a scale of attachment security, but are not designed to distinguish between the three insecure attachment relationships. This might explain why we did not find significant correlations between the continuous Avoidant and Ambivalent scales and the AQS and EAS; the AQS and EAS scores simply do not reflect avoidant and ambivalent attachment relationships. Therefore, there is at this moment not enough evidence to suggest convergent validity of the continuous Avoidant and Ambivalent ARI‐CP 2–5 scales. Future studies should examine the convergent validity of the ARI‐CP using attachment measure that distinguishes between the different types of insecure attachment relationships.
A second shortcoming of the current study is the rather large amount of time between filling out the questionnaires and the home visits (M = 42, with a maximum of 100 days). Although relatively stable, new attachment experiences or changed conditions (such as life events, or improved parental functioning) can alter the quality of the attachment relationship and the internal working model of the child (Fraley, 2002; Waters, Merrick, Treboux, Crowell, & Albersheim, 2000). Some of the clinical families were enrolled in attachment‐based interventions over the course of the study. This may have resulted in suppressed correspondence between the ARI‐CP 2–5 and the observational measures. It is advised in future studies that the ARI‐CP 2–5 be filled out at the same moment as the observations take place.
A third limitation is the lack of longitudinal data. Therefore, in the current study, it was not possible to examine test–retest reliability of the ARI‐CP 2–5. Future studies should preferably examine this, in order to understand the applicability of using the ARI‐CP 2–5 in ROM or the evaluation of interventions.
A final limitation is that the sample was not large and diverse enough to test for other grouping variables (beyond sex of the caregivers, sex of the children, age of the children, and population type) that could potentially cause measurement invariance, for example, ethnic background or social–economic status. Therefore, caution is warranted for using the norms of the ARI‐CP 2–5 that have been presented in the current study in populations that deviate from the sample of the current study.
Despite the limitations, the current study offers important implications for clinical practice. First and foremost, this study showed that the ARI‐CP 2–5 is a reliable and valid instrument to assess the caregiver's perception of the attachment relationship with the child. Insecure attachment relationships have been found to co‐occur with, or may even lay at the root of, internalizing and externalizing problems in children (Colonnesi et al., 2011; Groh et al., 2017; Madigan et al., 2016; Spruit et al., 2020). The presence of attachment insecurity directs treatment, for example, from behavior management programs in case of exclusively conduct problems (Leijten et al., 2019), to attachment‐based interventions in case of conduct problems that are caused by or co‐occur with attachment insecurity (Juffer et al., 2014). Therefore, it is important to understand if insecure attachment relationships are present in families with young children. Using the ARI‐CP 2–5 to obtain a first indication of the quality of the attachment relationship based on the perceptions of the caregivers is a rather practical approach, and makes it possible to address attachment in primary mental health care or in clinical intake procedures. Elevated scores on the ARI‐CP 2–5 could be a first indication of attachment insecurity, and a reason to refer families to specialists in diagnosing attachment problems for a more comprehensive observation‐based assessment of attachment insecurity and, if necessary, to attachment‐based interventions.
Second, we emphasize that the ARI‐CP 2–5 cannot (solely) be used to classify attachment relationships as secure or insecure. The quality of attachment relationship is a complex, multilayered construct (Bosmans & Kerns, 2015; Bretherton, 1985, Solomon & George, 2008; Waters & Cummings, 2000; Zeanah & Boris, 2012), and the caregivers’ perception is just one aspect of it. Moreover, the caregivers’ perception might be disturbed in insecure attachment relationships (Bailey et al., 2016; Koren‐Karie et al., 2002). For example, we expect that caregivers in an avoidant attachment relationships with their child tend to disavow attachment problems (Bailey et al., 2016). Therefore, discrepancies between the ARI‐CP 2–5 and observations may provide valuable diagnostic information (Bailey et al., 2016). Thus, in the assessment of the quality of attachment relationships, the results of the ARI‐CP 2–5 should always be interpreted and weighted in a broader diagnostic process, which would also include file information, observations, interviews, and attachment‐focused anamneses.
In conclusion, this study found evidence for the four‐factor structure of the ARI‐CP 2–5 and indications of measurement invariance among mothers and fathers, boys and girls, 2‐ to 3‐year olds, and 4‐ and 5‐year olds, as well as across families from a general and clinical population sample. Moreover, the reliability, concurrent validity, and predictive validity of the ARI‐CP 2–5 were sufficient and population‐based norms were established. Finally, convergent validity of the continuous Secure and Disorganized ARI‐CP 2–5 scales was found, and also for all the dichotomous cutoff scores of the ARI‐CP 2–5 scales. Therefore, we advocate the use of the ARI‐CP 2–5 in order to obtain a first indication of the quality of the attachment relationship, based on the caregivers’ perception. In the end, caregivers do not rely on a single observation, but experience the attachment relationship with their child in different contexts and for an extended period of time. Further, the attachment relationship should not only be expressed in the quality of the behavioral interactions, but also in the emotional and cognitive aspects. Additionally, the caregiver's perception of the attachment relationship with the child influences parental behavior, which impacts the attachment behaviors of the child toward the caregiver. Finally, insights into caregivers’ perceptions may offer important diagnostic information and direct treatment goals. Insecure attachment relationships are predictive of a range of developmental problems in life. Therefore, a questionnaire for caregivers provides in the clinical need for straightforward instruments that can be used as part of the screening and assessment of insecure attachment relationships, and enables the inclusion of caregivers’ perceptions in attachment research.
CONFLICT OF INTEREST
The authors declare no conflict of interest.
Supporting information
SUPPORTING INFORMATION
Spruit A, Colonnesi C, Wissink I, et al. Development and validation of the Attachment Relationship Inventory—Caregiver Perception 2–5 years (ARI‐CP 2–5): Psychometric structure, external validity, and norms. Infant Ment Health J. 2021;42:188–205. 10.1002/imhj.21909
REFERENCES
- Ainsworth, M. D. S. , Blehar, M. , Waters, E. , & Wall, S. (1978). Patterns of attachment. Hillsdale, NJ: Erlbaum. [Google Scholar]
- Bailey, H. N. , Redden, E. , Pederson, D. R. , & Moran, G. (2016). Parental disavowal of relationship difficulties fosters the development of insecure attachment. Canadian Journal of Behavioural Science, 48, 49–59. [Google Scholar]
- Bartholomew, K. , & Horowitz, L. M. (1991). Attachment styles among young adults: A test of a four‐category model. Journal of Personality and Social Psychology, 61, 226–244. [DOI] [PubMed] [Google Scholar]
- Benoit, D. , Madigan, S. , Lecce, S. , Shea, B. , & Goldberg, S. (2001). Atypical maternal behavior toward feeding‐disordered infants before and after intervention. Infant Mental Health Journal, 22, 611–626. [Google Scholar]
- Benoit, D. , Zeanah, C. H. , Parker, K. C. , Nicholson, E. , & Coolbear, J. (1997). “Working model of the child interview”: Infant clinical status related to maternal perceptions. Infant Mental Health Journal, 18, 107–121. [Google Scholar]
- Biringen, Z. (2008). The Emotional Availability (EA) Scales and the Emotional Attachment & Emotional Availability (EA2) Clinical Screener: Infancy/Early Childhood Version (4th ed.). Boulder, CO: EmotionalAvailability. [Google Scholar]
- Biringen, Z. , Derscheid, D. , Vliegen, N. , Closson, L. , & Easterbrooks, M. A. (2014). Emotional availability (EA): Theoretical background, empirical research using the EA Scales, and clinical applications. Developmental Review, 34, 114–167. [Google Scholar]
- Bosmans, G. , & Kerns, K. A. (2015). Attachment in middle childhood: Progress and prospects. New Directions for Child and Adolescent Development, 2015, 1–14. [DOI] [PubMed] [Google Scholar]
- Bowlby, J. (1969). Attachment and loss: Attachment. New York, NY: Basic Books. [Google Scholar]
- Bretherton, I. (1985). Attachment theory: Retrospect and prospect. Monographs of the Society for Research in Child Development, 50, 3–35. [Google Scholar]
- Bronfman, E. , Parsons, E. , & Lyons‐Ruth, K. (1999). Atypical Maternal Behavior Instrument for Assessment and Classification (AMBIANCE): Manual for coding disrupted affective communication . Unpublished manuscript.
- Bugental, D. B. , & Johnston, C. (2000). Parental and child cognitions in the context of the family. Annual Review of Psychology, 51, 315–344. [DOI] [PubMed] [Google Scholar]
- Cassidy, J. , & Berlin, L. J. (1994). The insecure/ambivalent pattern of attachment: Theory and research. Child Development, 65, 971–991. [PubMed] [Google Scholar]
- Colonnesi, C. , Draijer, E. M. , Stams, G. J. J. M. , Van der Bruggen, C. O. , Bögels, S. M. , & Noom, M. J. (2011). The relation between insecure attachment and child anxiety: A meta‐analytic review. Journal of Clinical Child and Adolescent Psychology, 40, 630–645. [DOI] [PubMed] [Google Scholar]
- Demers, I. , Bernier, A. , Tarabulsy, G. M. , & Provost, M. A. (2010). Maternal and child characteristics as antecedents of maternal mind‐mindedness. Infant Mental Health Journal, 31, 94–112. [DOI] [PubMed] [Google Scholar]
- Dwyer, K. M. (2005). The meaning and measurement of attachment in middle and late childhood. Human Development, 48, 155–182. [Google Scholar]
- Fearon, R. P. , Bakermans‐Kranenburg, M. J. , Van IJzendoorn, M. H. , Lapsley, A. M. , & Roisman, G. I. (2010). The significance of insecure attachment and disorganization in the development of children's externalizing behavior: A meta‐analytic study. Child Development, 81, 435–456. [DOI] [PubMed] [Google Scholar]
- Fox, N. A. , Kimmerly, N. L. , & Schafer, W. D. (1991). Attachment to mother/attachment to father: A meta‐analysis. Child Development, 62(1), 210–225. [PubMed] [Google Scholar]
- Fraley, R. C. (2002). Attachment stability from infancy to adulthood: Meta‐analysis and dynamic modeling of developmental mechanisms. Personality and Social Psychology Review, 6, 123–151. [Google Scholar]
- George, C. , & Solomon, J. (2008). The caregiving system: A behavioral systems approach to parenting. In Cassidy J. & Shaver P. R. (Eds.), Handbook of attachment: Theory, research, and clinical applications (pp. 833–856). New York, NY: The Guilford Press. [Google Scholar]
- Girvin, H. (2004). Beyond ‘stages of change:’ Using readiness for change and caregiver‐reported problems to identify meaningful subgroups in a child welfare sample. Children and Youth Services Review, 26, 897–917. [Google Scholar]
- Goodman, R. (2001). Strengths and Difficulties Questionnaire (SDQ). London, UK: Youthinmind. [Google Scholar]
- Gregorich, S. E. (2006). Do self‐report instruments allow meaningful comparisons across diverse population groups? Testing measurement invariance using the confirmatory factor analysis framework. Medical Care, 44, S78–S94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Groh, A. M. , Fearon, R. P. , van IJzendoorn, M. H. , Bakermans‐Kranenburg, M. J. , & Roisman, G. I. (2017). Attachment in the early life course: Meta‐analytic evidence for its role in socioemotional development. Child Development Perspectives, 11, 70–76. [Google Scholar]
- Hawley, K. M. , & Weisz, J. R. (2003). Child, parent and therapist (dis) agreement on target problems in outpatient therapy: The therapist's dilemma and its implications. Journal of Consulting and Clinical Psychology, 71, 62–70. [DOI] [PubMed] [Google Scholar]
- Hendriks, A. M. , Van der Giessen, D. , Stams, G. J. J. M. , & Overbeek, G. (2018). The association between parent‐reported and observed parenting: A multi‐level meta‐analysis. Psychological Assessment, 30, 621–633. [DOI] [PubMed] [Google Scholar]
- Hoeve, M. , Stams, G. J. J. M. , Van der Put, C. E. , Dubas, J. S. , Van der Laan, P. H. , & Gerris, J. R. (2012). A meta‐analysis of attachment to parents and delinquency. Journal of Abnormal Child Psychology, 40, 771–785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hu, L. T. , & Bentler, P. M. (1999). Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling, 6, 1–55. [Google Scholar]
- Jorgensen, T. D. , Pornprasertmanit, S. , Schoemann, A. M. , & Rosseel, Y. (2018). semTools: Useful tools for structural equation modeling . R package version 0.5‐1. Retrieved from https://CRAN.R-project.org/package=semTools
- Juffer, F. , Bakermans‐Kranenburg, M. J. , & Van IJzendoorn, M. H. (2014). Attachment‐based interventions: Sensitive parenting is the key to positive parent‐child relationships. In Holmes P. & Farnfield S. (Eds.), The Routledge handbook of attachment: Implications and interventions (pp. 83–103). London, UK: Routledge. [Google Scholar]
- Klohnen, E. C. , & Bera, S. (1998). Behavioral and experiential patterns of avoidantly and securely attached women across adulthood: A 31‐year longitudinal perspective. Journal of Personality and Social Psychology, 74, 211–223. [DOI] [PubMed] [Google Scholar]
- Koo, T. K. , & Li, M. Y. (2016). A guideline of selecting and reporting intraclass correlation coefficients for reliability research. Journal of Chiropractic Medicine, 15, 155–163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koren‐Karie, N. , Oppenheim, D. , Dolev, S. , Sher, E. , & Etzion‐Carasso, A. (2002). Mothers’ insightfulness regarding their infants’ internal experience: Relations with maternal sensitivity and infant attachment. Developmental Psychology, 38, 534–542. [DOI] [PubMed] [Google Scholar]
- Leijten, P. , Gardner, F. , Melendez‐Torres, G. J. , Hutchings, J. , Schulz, S. , Knerr, W. , & Overbeek, G. (2019). Meta‐analyses: Key parenting program components for disruptive child behavior. Journal of the American Academy of Child and Adolescent Psychiatry, 58, 180–190. [DOI] [PubMed] [Google Scholar]
- Lyons‐Ruth, K. , & Spielman, E. (2004). Disorganized infant attachment strategies and helpless‐fearful profiles of parenting: Integrating attachment research with clinical intervention. Infant Mental Health Journal, 25, 318–335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McMahon, C. A. , & Meins, E. (2012). Mind‐mindedness, parenting stress, and emotional availability in mothers of preschoolers. Early Childhood Research Quarterly, 27, 245–252. [Google Scholar]
- Madigan, S. , Brumariu, L. E. , Villani, V. , Atkinson, L. , & Lyons‐Ruth, K. (2016). Representational and questionnaire measures of attachment: A meta‐analysis of relations to child internalizing and externalizing problems. Psychological Bulletin, 142, 367–399. [DOI] [PubMed] [Google Scholar]
- Madigan, S. , Hawkins, E. , Goldberg, S. , & Benoit, D. (2006). Reduction of disrupted caregiver behavior using modified interaction guidance. Infant Mental Health Journal, 27, 509–527. [DOI] [PubMed] [Google Scholar]
- Main, M. , & Hesse, E. (1990). Parents’ unresolved traumatic experiences are related to infant disorganized attachment status: Is frightened and/or frightening parental behavior the linking mechanism? In Greenberg M. T., Cicchetti D., & Cummings E. M. (Eds.), Attachment in the preschool years: Theory, research, and intervention (pp. 161–182). Chicago, IL: University of Chicago Press. [Google Scholar]
- Meins, E. (2013). Security of attachment and the social development of cognition. Hove, UK: Psychology Press. [Google Scholar]
- Meins, E. , & Fernyhough, C. (2015). Mind‐mindedness coding manual . Unpublished manuscript.
- Meins, E. , Fernyhough, C. , Russell, J. , & Clark‐Carter, D. (1998). Security of attachment as a predictor of symbolic and mentalising abilities: A longitudinal study. Social Development, 7, 1–24. [Google Scholar]
- Molinari, D. L. , & Freeborn, D. (2006). Social support needs of families adopting special needs children. Journal of Psychosocial Nursing and Mental Health Services, 44, 28–34. [DOI] [PubMed] [Google Scholar]
- Muris, P. , Meesters, C. , & van den Berg, F. (2003). The strengths and difficulties questionnaire (SDQ). European Child & Adolescent Psychiatry, 12, 1–8. [DOI] [PubMed] [Google Scholar]
- O'Connor, T. G. , & Gerard Byrne, J. (2007). Attachment measures for research and practice. Child and Adolescent Mental Health, 12, 187–192. [DOI] [PubMed] [Google Scholar]
- Park, K. A. , & Waters, E. (1989). Security of attachment and preschool friendships. Child Development, 60, 1076–1081. [DOI] [PubMed] [Google Scholar]
- Peters, G. (2018). Userfriendlyscience (UFS): Quantitative analysis made accessible . 10.17605/osf.io/txequ [DOI]
- Powell, B. , Cooper, G. , Hoffman, K. , & Marvin, B. (2013). The circle of security intervention: Enhancing attachment in early parent‐child relationships. New York, NY: Guilford Publications. [Google Scholar]
- Rosseel, Y. (2012). lavaan: An R package for structural equation modeling. Journal of Statistical Software, 48, 1–36. [Google Scholar]
- Solomon, J. , & George, C. (2008). The measurement of attachment security and related constructs in infancy and early childhood. In Cassidy J. & Shaver P. R. (Eds.), Handbook of attachment: Theory, research, and clinical applications (2nd ed., pp. 383–416). New York, NY: Guilford Press. [Google Scholar]
- Spruit, A. , & Meesters, C. (2018). Relationships Questionnaire – Nederlandse versie voor volwassenen. Amsterdam, The Netherlands: Universiteit van Amsterdam. [Google Scholar]
- Spruit, A. , Goos, L. , Weenink, N. , Rodenburg, R. , Niemeyer, H. , Stams, G. J. J. M. , & Colonnesi, C. (2020). The relation between attachment and depression in children and adolescents: A multilevel meta‐analysis. Clinical Child and Family Psychology Review, 23, 54–69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spruit, A. , Wissink, I. , Noom, M. J. , Colonnesi, C. , Polderman, N. , Willems, L. , … Stams, G. J. J. M. (2018). Internal structure and reliability of the Attachment Insecurity Screening Inventory (AISI) for children age 6 to 12. BMC Psychiatry, 18, 30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sroufe, L. A. , & Fleeson, J. (1988). The coherence of family relationships. In Hinde R. & Stevenson‐Hinde J. (Eds.), Relationships within families (pp. 27–47). Oxford, UK: Oxford University Press. [Google Scholar]
- Stone, L. L. , Otten, R. , Engels, R. C. , Vermulst, A. A. , & Janssens, J. M. (2010). Psychometric properties of the parent and teacher versions of the strengths and difficulties questionnaire for 4‐to 12‐year‐olds: A review. Clinical Child and Family Psychology Review, 13, 254–274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tryphonopoulos, P. D. , Letourneau, N. , & Ditommaso, E. (2014). Attachment and caregiver–infant interaction: A review of observational‐assessment tools. Infant Mental Health Journal, 35, 642–656. [DOI] [PubMed] [Google Scholar]
- Van IJzendoorn, M. H. , Scheungel, C. , & Bakermans‐Kranenborg, M. J. (1999). Disorganized attachment in early childhood: Meta‐analysis of precursors, concomitants, and sequel. Development and Psychopathy, 11, 225–259. [DOI] [PubMed] [Google Scholar]
- Van Ijzendoorn, M. H. , Vereijken, C. M. , Bakermans‐Kranenburg, M. J. , & Riksen‐Walraven, M. J. (2004). Assessing attachment security with the attachment Q sort: Meta‐analytic evidence for the validity of the observer AQS. Child Development, 75, 1188–1213. [DOI] [PubMed] [Google Scholar]
- Van Widenfelt, B. M. , Goedhart, A. W. , Treffers, P. D. , & Goodman, R. (2003). Dutch version of the Strengths and Difficulties Questionnaire (SDQ). European Child & Adolescent Psychiatry, 12, 281–289. [DOI] [PubMed] [Google Scholar]
- Vasileva, M. , & Petermann, F. (2018). Attachment, development, and mental health in abused and neglected preschool children in foster care: A meta‐analysis. Trauma, Violence, & Abuse, 19, 443–458. [DOI] [PubMed] [Google Scholar]
- Verhage, M. L. , Schuengel, C. , Madigan, S. , Fearon, R. M. , Ooster‐man, M. , Cassibba, R. , … van IJzendoorn, M. H. (2016). Narrow‐ing the transmission gap: A synthesis of three decades of research on intergenerational transmission of attachment. Psychological Bulletin, 142, 337–366. [DOI] [PubMed] [Google Scholar]
- Vreeswijk, C. M. , Maas, A. J. B. , & van Bakel, H. J. (2012). Parental representations: A systematic review of the working model of the child interview. Infant Mental Health Journal, 33, 314–328. [DOI] [PubMed] [Google Scholar]
- Waters, E. , & Cummings, E. M. (2000). A secure base from which to explore close relationships. Child Development, 71, 164–172. [DOI] [PubMed] [Google Scholar]
- Waters, E. , & Deane, K. E. (1985). Defining and assessing individual differences in attachment relationships: Q‐methodology and the organization of behavior in infancy and early childhood. Monographs of the Society for Research in Child Development, 50, 41–65. [Google Scholar]
- Waters, E. , Merrick, S. , Treboux, D. , Crowell, J. , & Albersheim, L. (2000). Attachment security in infancy and early adulthood: A twenty‐year longitudinal study. Child Development, 71, 684–689. [DOI] [PubMed] [Google Scholar]
- Wissink, I. B. , Colonnesi, C. , Stams, G. J. J. M. , Hoeve, M. , Asscher, J. J. , Noom, M. J. , … Kellaert‐Knol, M. G. (2016). Validity and reliability of the attachment insecurity screening inventory (AISI) 2–5 years. Child Indicators Research, 9, 533–550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu, H. , & Estabrook, R. (2016). Identification of confirmatory factor analysis models of different levels of invariance for ordered categorical outcomes. Psychometrika, 81, 1014–1045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zeanah, C. H. , & Benoit, D. (1995). Clinical applications of a parent perception interview in infant mental health. Child and Adolescent Psychiatric Clinics, 4, 539–554. [Google Scholar]
- Zeanah, C. H. , & Boris, N. W. (2012). Disturbances and disorders of attachment in early childhood. Handbook of Infant Mental Health, 2, 353–368. [Google Scholar]
- Zeegers, M. A. , Colonnesi, C. , Noom, M. J. , Polderman, N. , & Stams, G. J. J. M. (2020). Remediating child attachment insecurity: Evaluating the basic trust intervention in adoptive families. Research on Social Work Practice, 30, 736–749. [Google Scholar]
- Zeegers, M. A. , Colonnesi, C. , Stams, G. J. J. M. , & Meins, E. (2017). Mind matters: A meta‐analysis on parental mentalization and sensitivity as predictors of infant–parent attachment. Psychological Bulletin, 143, 1245–1272. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
SUPPORTING INFORMATION


