Abstract
With the advent of the COVID-19 pandemic in the United States, resources have been reallocated and elective cases have been deferred to minimize the spread of the disease, altering the workflow of cardiac catheterization laboratories across the country. This has in turn affected the training experience of cardiology fellows, including diminished procedure numbers and a narrow breadth of cases as they approach the end of their training before joining independent practice. It has also taken a toll on the emotional well-being of fellows as they see their colleagues, loved ones, patients or even themselves struggling with COVID-19, with some succumbing to it. The aim of this opinion piece is to focus attention on the impact of the COVID-19 pandemic on fellows and their training, challenges faced as they transition to practicing in the real world in the near future and share the lessons learned thus far. We believe that this is an important contribution and would be of interest not only to cardiology fellows-in-training and cardiologists but also trainees in other procedural specialties.
Fellows-in-training (FITs) and medical residents have served on the frontline during the U.S. coronavirus disease of 2019 (COVID-19) pandemic. In many hospitals, schedules and workflow have changed for trainees since the outbreak started. Not only has the pandemic created a novel training experience, it has resulted in a unique, once in a lifetime, educational opportunity. Although it may have temporarily taken away from their traditional core curricula, it has taught FIT real-life lessons about disaster preparedness in health care, compelled them to brush up on critical care knowledge and skills, fostered greater collaboration with between medical and surgical specialties, and made them rethink the ethics around end-of-life care and medical futility. Herein, we provide our perspective regarding the impact that COVID-19 has had on our lives, both personally and professionally, and share novel solutions that have been adopted to maximize our educational experience.
Interventional Training
In the initial days of the COVID-19 pandemic, U.S. healthcare systems began limiting elective procedures at the recommendation of the CDC.1 For interventional cardiology, this meant a temporary moratorium on ‘elective’ cardiac catheterizations, coronary angiography, and on percutaneous coronary, peripheral, and structural interventions. At some institutions, the management of acute STEMI, reverted to a time when thrombolytics were used in lieu of percutaneous coronary intervention (PCI).2 This possibility motivated FITs to re-educate themselves around specific thrombolytic agents and their respective dosing.
The cessation of elective cases corresponded with the final quarter of interventional cardiology fellowship training. This time was vital for those in advanced fellowships where trainees are honing their skill sets prior to entering the workforce as independent operators. The decrease in case volume affected the supervised hands on experience and left FITs at lower volume centers vulnerable to meeting the minimum Accreditation Council of Graduate Medical Education (ACGME) requirements.
Although this may be uncharted territory for many, it is not unprecedented. Fellows on research tracks or those who have had to take time off for personal reasons were able to graduate in time this past academic year. Since interventional cardiology requires both cognitive and procedural skills, the time away from the laboratory could be used effectively to build on the other core aspects and to attain all other major ACGME mandated milestones during this global crisis. Given the disrupted training with closed clinical settings, decreased patient and procedural volumes, what has transpired is the incorporation of the program director's assessment of individual fellow's competency to complete their truncated training and a deep dive into exploring the utility of simulated virtual cases where fellows can incorporate hands-on interactive experience during this pandemic.3
Meetings and Conferences
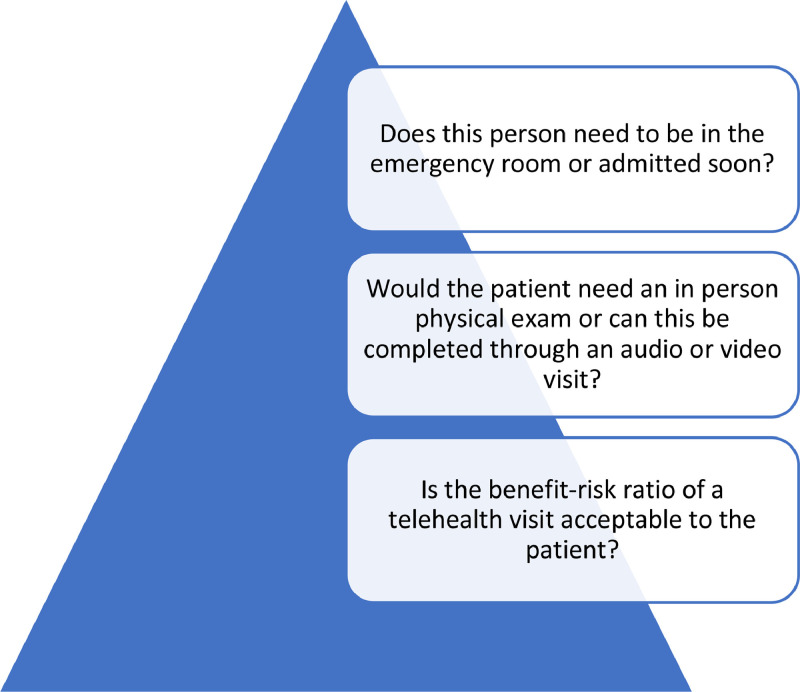
The cancellation of many academic journal clubs, grand rounds, and national professional society scientific meetings also placed a further strain on education.4 Luckily, this led to the innovation of virtual platforms and video conferencing (i.e., Zoom Video Communications Inc., 2016 or GoToMeeting, or Microsoft Teams Collaboration Software). This has since promoted the rapid use of telemedicine that has been advantageous to both patients and clinicians alike to prevent direct contact and respecting social distancing mandates (Figure 1 ). Cardiovascular medical societies have been empathic and have undertaken multiple initiatives to promote learning. This demonstrates unwavering support for FITs during this time and is much appreciated. This is further supported by the fact that the American College of Cardiology (ACC), Society for Cardiovascular Angiography and Imaging (SCAI) and Transcatheter Cardiovascular Therapeutics (TCT) have gone virtual this year for the first time. Our hope is to have these opportunities available free of charge in the future as well. We remain confident that fellow education will continue to remain a focus post the COVID-19 era.
Figure 1.
Basic checklist when triaging patients for a telemedicine visit.
Employment Opportunities
Historically fellows have traveled across the country for face to face interviews to secure employment or further training opportunities. Given required social distancing measures, many institutions have mandated that all interviews be conducted virtually. The reduction in travel may help counterbalance reduced fellow procedural volumes described above. Additionally, hiring freezes and salary cuts resulting from the economic consequences of COVID-19 have made the job market in both private and academic sectors, which were already competitive, even more so. These facts on the ground have led many FITs to re-think their future, expand skill sets by exploring further subspecialty training, and take on new roles to ensure their marketability. Such changes have caused economic, financial, and emotional strain that will have a lasting impact on FITs, extending long after the COVID-19 pandemic.
Physician Wellbeing
A final facet to consider is FIT wellbeing during the pandemic. The fear and anxiety over potentially placing immediate family members have added emotional and mental strife on fellows. Several trainees have been out of work with COVID-19 and some have unfortunately succumbed to it. Limited in-classroom schedules and day-care capacity means that parents have to juggle child-care responsibilities while managing their professional lives and taking care of patients.
Luckily, most academic institutions have provided access to mental wellness resources during this time. The goal of continuing a work-life balance for FITs while not violating duty hours, possible hazard pay, allocation of appropriate PPE, access to child care, and support from our governing bodies have been invaluable to FITs in these unique times. The COVID-19 pandemic has ushered in a ‘new call to action’; we have learned to embrace innovative solutions and broaden partnerships to accelerate the ongoing changes (Table 1 ).
Table 1.
Impact of COVID-19 on fellows’ training, well-being and transition to early career
| Impact on fellows & early career | Novel solutions | |
|---|---|---|
| Impact on Training |
|
|
| Fellow Education |
|
|
| Changes in STEMI management strategy |
|
|
| Fellow safety and wellbeing |
|
|
| Job Recruitment |
|
|
Lessons Learned
COVID-19 pandemic is a historical life changing event that will be engraved in memory forever. Planning ahead for the future can significantly reduce the real‐time burden which is particularly important as clinical demands increase with a surge.5 We have an opportunity to implement a competency-based approach for which many educators have been calling for a long time now.6 This unique experience of being a doctor in the trenches during a global pandemic has provided the opportunity for physicians to create collaborative and innovative techniques to promote education and patient care. This has inspired many trainees with the confidence to take on new leadership roles to prepare for future crises. We hope that the lessons we have learned on triaging coronary and structural interventions can provide centers with guidance now and for future preparedness. With the introduction of rapid testing at most sites, we are mitigating the risk of unnecessary exposure to COVID in the cath lab and critical care setting.
It is easy to lose sight of how much progress science has made over the past 10 months; we now have promising vaccines, better testing and treatments and greater knowledge about how to control this virus. That should give us all cause for hope and optimism.
Author Contribution
Sabeeda Kadavath MD, Dalia Hawwas, MD, Aaron Strobel, MD, Jay Mohan, DO: Conceptualization And Writing. Marie Bernardo, MD, Adnan Kassier, MD, Lina Ya'qoub, MD, Nidhi Madan, MD MPH, Said Ashraf, MD,Negar Salehi, MD, Sagger Mawri, MD MS, Karim Abdur Rehman MD, Aisha Siraj: Original draft preparation and tables/figures, Chadi Alraies, MD MPH, Marwan Saad MD PhD, Herbert Aronow Writing- Reviewing and Editing.
Disclosures
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper
References
- 1.Coronavirus disease 2019 (COVID-19) - interim guidance for businesses and employers [Internet]. Centers for Disease Control and Prevention 2020 Available from: https://www.cdc.gov/coronavirus/2019-ncov/community/guidance-business-response.html
- 2.Jing Z-C, Zhu H-D, Yan X-W, Chai W-Z, Zhang S. Recommendations from the Peking Union Medical College Hospital for the management of acute myocardial infarction during the COVID-19 outbreak. Eur Heart J. 2020;41:1791–1794. doi: 10.1093/eurheartj/ehaa258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.ACGME Guidance Statements. Available at: https://acgme.org/COVID-19/ACGME-Guidance-Statements
- 4.Roffi M., Capodanno D., Windecker S., Baumbach A., Dudek D. Impact of the COVID-19 pandemic on interventional cardiology practice: results of the EAPCI survey. EuroIntervention. 2020;16:247–250. doi: 10.4244/EIJ-D-20-00528. [DOI] [PubMed] [Google Scholar]
- 5.US Centers for Disease Control and Prevention. https://www.cdc.gov/coronavirus/2019-ncov/cases-updates/index.html
- 6.Goldhamer MEJ, Pusic MV, Co JPT, Weinstein DF. Can Covid catalyze an educational transformation? Competency-based advancement in a crisis. N Engl J Med. 2020;383:1003–1005. doi: 10.1056/NEJMp2018570. [DOI] [PubMed] [Google Scholar]