Abstract
Background
The COVID-19 pandemic has impacted healthcare in various vulnerable patient subpopulations. However, data are lacking on the impact of COVID-19 on hip fractures, seen mainly in older patients. Using national claims data, we aimed to describe the epidemiology during the first COVID-19 wave in the USA.
Methods
We compared patients admitted for hip fractures during March and April of 2020 with those admitted in 2019 in terms of patient and healthcare characteristics, COVID-19 diagnosis, and outcomes. An additional comparison was made between COVID-19-positive and -negative patients. Outcomes included length of hospital stay (LOS), admission to an ICU, ICU LOS, use of mechanical ventilation, 30-day readmission, discharge disposition, and a composite variable of postoperative complications.
Results
Overall, 16 068 hip fractures were observed in 2019 compared with 7498 in 2020. Patients with hip fractures in 2020 (compared with 2019) experienced earlier hospital discharge and were less likely to be admitted to ICU, but more likely to be admitted to home. Amongst 83 patients with hip fractures with concomitant COVID-19 diagnosis, we specifically observed more non-surgical treatments, almost doubled LOS, a more than 10-fold increased mortality rate, and higher complication rates compared with COVID-19-negative patients.
Conclusions
The COVID-19 pandemic significantly impacted not only volume of hip fractures, but also patterns in care and outcomes. These results may inform policymakers in future outbreaks and how this may affect vulnerable patient populations, such as those experiencing a hip fracture.
Keywords: COVID-19, critical care, geriatrics, hip fracture, hospitalisation, outcome, surgery
Editor's key points.
-
•
COVID-19 has had major impacts on access to elective surgery and complications in those undergoing elective and non-elective surgeries.
-
•
This study found that in the US there was a halving in the number of hip fracture surgeries in 2020 compared with in 2019.
-
•
Patients with COVID-19 having hip fracture surgery had markedly increased rates of serious complications, including mortality.
-
•
Pulmonary complications occurred in more than one in five patients diagnosed with COVID-19.
The SARS-CoV-2 (COVID-19) pandemic has caused a substantial strain on the US healthcare system, with various professional organisations, including the American Academy of Orthopaedic Surgeons, providing guidance on postponement or cancellation of elective and non-urgent surgeries to slow the transmission of the disease and to conserve healthcare resources.1 Although these recommendations did not apply to urgent/emergent trauma surgeries, the shift of resources towards treating patients diagnosed with COVID-19 during the surge had the potential to leave the trauma system under-resourced.2 , 3 Many anaesthetists and operating practitioners were pulled away to cover ICUs, resulting in reduced capacity for surgery and non-COVID-19 patient care. Despite observations that showed reduced emergency department admissions likely because of stay-at-home orders,4, 5, 6 the necessity of caring for hip fractures in older patients remained a concern.7 , 8 In addition to potential resource shortages during the pandemic, patients with hip fractures represent a very vulnerable population with multiple comorbidities9 that is susceptible to respiratory infections attributable to the inability to ambulate.10 Indeed, several studies have reported increased rate of severe complications and high mortality rate amongst patients with hip fractures with concomitant COVID-19 diagnosis.11, 12, 13, 14
Despite these observations, it remains largely unknown how the first US COVID-19 wave impacted hip fracture volume, treatment options, and outcomes.
Therefore, using a national database, this study aimed to describe the epidemiology and compare patient and healthcare-related characteristics and outcomes of patients with hip fractures admitted during the COVID-19 outbreak with patients admitted during an identical pre-COVID-19 period. Further, we sought to compare patient characteristics and outcomes between patients with hip fractures with and without COVID-19.
Methods
Study design and cohort
This study was approved by the Institutional Review Board at the Hospital for Special Surgery (IRB#2012-050). The requirement for written informed consent was waived given the de-identified nature of the data. Patient information was derived from the Premier Healthcare database (Premier Healthcare Solutions, Inc., Charlotte, NC, USA).15 Individuals who were diagnosed with hip fracture upon hospital admission during March and April of 2019 and 2020 were queried. We selected patients admitted during the initial surge of COVID-19 from March 1 to April 30, 2020, as these were the most recent data available to us at the time of analysis. To compare this cohort to controls, we selected patients admitted during the same time frame the year before. This was done, as fracture incidence and volume show seasonal variability.16, 17, 18
Hip fracture codes were identified and further classified based on the International Classification of Diseases, 10th Revision (ICD-10) diagnosis codes for the location of fracture: femoral neck (S72.0), intertrochanteric (S72.1), subtrochanteric (S72.2), or multiple locations. Hip fracture repair procedures were identified and classified into groups according to ICD-10 procedure codes: internal fixation, hemiarthroplasty, total hip arthroplasty, or non-surgical (Supplementary material). Patients were excluded if they were <18 yr old (N=382), pregnant (N=2), or missing gender information (N=5).
Study variables
Variables of interest were patient and healthcare characteristics, COVID-19 diagnosis, and outcomes. Patient characteristics included age, gender, race (black, white, or other), Charlson–Deyo comorbidity index19 (categorised as 0, 1, 2, or 3+), source of admission (clinic, transfer from other health facility, non-healthcare, or others), admission type (elective, emergent/urgent/trauma, or others), and insurance provider (commercial, Medicaid, Medicare, uninsured, or unknown). Fracture type and type of surgical procedure were classified as mentioned previously. Healthcare characteristics analysed included location (urban vs rural), size (<300, 300–500, or >500 beds), teaching status, and region (Midwest, Northeast, South, or West). Patients diagnosed with COVID-19 were identified using ICD-10 codes (U07.1 or U07.2).20 Outcomes included length of hospital stay (LOS), admission to an ICU, length of stay in the ICU, use of mechanical ventilation, 30 day readmission, in-hospital death, discharge disposition (home or facility/others), and a composite variable of postoperative complications (acute renal failure, acute myocardial infarction, other cardiovascular complications, delirium, deep vein thrombosis, sepsis/septic shock, inpatient fall, haemorrhage/haematoma, pulmonary complications, pulmonary embolism, pneumonia, wound complications, and CNS events). All complications were defined based on ICD-10 diagnosis codes (Supplementary material).
Statistical analysis
All statistical analyses were performed using SAS version 9.4 (SAS Institute, Cary, NC, USA). Descriptive analyses were stratified by year and by COVID-19 diagnosis within the 2020 cohort. Categorical variables were reported as absolute numbers and frequencies (%), and continuous variables were reported as median and inter-quartile range (IQR). Patient and healthcare characteristics were compared using standardised differences rather than P-values, as univariable group differences easily reach statistical significance in large sample sizes. A standardised difference of 0.1 (or 10%) generally indicates a meaningful difference in covariate distribution between groups.21 Odds ratios (ORs) are used to describe risk. Binary outcomes were compared using bivariate logistic regression, and continuous outcomes were compared using Wilcoxon rank-sum tests. A P-value <0.05 was used to determine significant differences between 2020 and 2019. Given the descriptive nature of this paper, P-values should be interpreted carefully.
Results
Overall, 16 068 hip fractures were observed in 2019 compared with 7498 (a 53% reduction) in 2020.
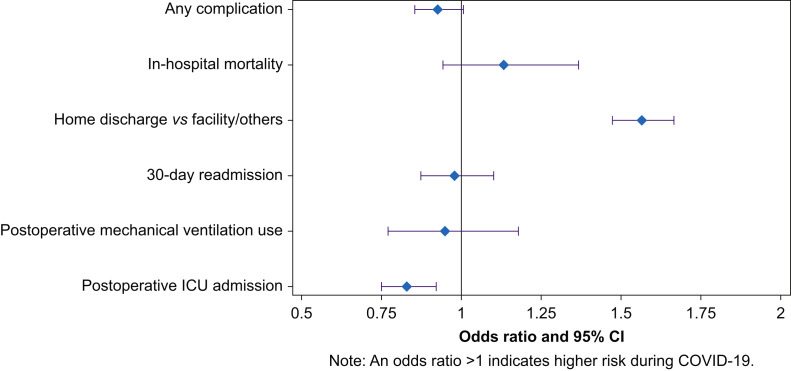
Absolute differences of patient and healthcare characteristics between 2019 and 2020 were relatively small, except for source of admission and teaching hospital, both with standardised differences of >0.1 (Table 1 ). Regarding outcomes, patients with a hip fracture during the COVID-19 surge were discharged 1 day earlier (median [IQR]: 4 [3–6] days) compared with the cohort admitted in 2019 (median [IQR]: 5 [3–7]; P<0.001). In addition, patients were less likely to be admitted to an ICU postoperatively (OR 0.85 [95% confidence interval {CI}: 0.77, 0.93]; P<0.001), and more likely to be discharged home (OR 1.57 [95% CI: 1.47, 1.67]; P<0.001). There were no differences between the two cohorts in 30 day readmission rates, use of mechanical ventilation, overall ICU days, or the incidence in composite complications (Fig 1 ).
Table 1.
Patient and healthcare characteristics pre-COVID-19 and during COVID-19
| Pre-COVID-19 | During COVID-19 | Standardised difference | |
|---|---|---|---|
| N (%) | 16 068 (68.2) | 7498 (31.8) | |
| Age, median (IQR) | 81 (71–88) | 81 (71–88) | 0.015 |
| Female, n (%) | 10 674 (66.4) | 4936 (68.5) | 0.013 |
| Race, n (%) | 0.060 | ||
| Black | 704 (4.4) | 365 (4.8) | |
| White | 14 145 (88) | 6562 (87.5) | |
| Other | 1219 (7.6) | 573 (7.6) | |
| Deyo index, n (%) | 0.050 | ||
| 0 | 6826 (42.5) | 2994 (39.9) | |
| 1 | 2071 (12.9) | 972 (13.0) | |
| 2 | 4190 (26.1) | 2093 (27.9) | |
| 3+ | 2981 (18.6) | 1439 (19.2) | |
| Source of admission, n (%) | 0.114 | ||
| Clinic | 838 (5.2) | 558 (7.4) | |
| Transfer from other health facility | 2767 (17.2) | 1340 (17.9) | |
| Non-healthcare | 12 356 (76.9) | 5562 (74.2) | |
| Others | 107 (0.7) | 38 (0.5) | |
| Admission type, n (%) | 0.036 | ||
| Elective | 1461 (9.1) | 615 (8.2) | |
| Emergent/urgent/trauma | 14 489 (90.2) | 6840 (91.2) | |
| Others | 118 (0.7) | 43 (0.6) | |
| Insurance, n (%) | 0.076 | ||
| Commercial | 1162 (7.2) | 493 (6.6) | |
| Medicaid | 552 (3.4) | 313 (4.2) | |
| Medicare | 13 681 (85.1) | 6362 (84.8) | |
| Uninsured | 240 (1.5) | 88 (1.2) | |
| Unknown | 433 (2.7) | 242 (3.2) | |
| Fracture location, n (%) | 0.043 | ||
| Multiple | 1112 (6.9) | 524 (7.0) | |
| Neck | 7839 (48.8) | 3516 (46.9) | |
| Pertrochanteric | 6468 (40.3) | 3149 (42.0) | |
| Subtrochanteric | 649 (4.0) | 309 (4.1) | |
| Procedure, n (%) | <0.001 | ||
| Non-surgical | 2827 (17.6) | 1330 (17.7) | |
| Internal fixation | 8273 (51.5) | 3848 (51.3) | |
| Total hip arthroplasty | 1093 (6.8) | 509 (6.8) | |
| Hemiarthroplasty | 3875 (24.1) | 1811 (24.2) | |
| Urban/rural hospital, n (%) | 0.038 | ||
| Urban | 13 623 (84.8) | 6252 (83.4) | |
| Rural | 2445 (15.2) | 1246 (16.6) | |
| Teaching hospital, n (%) | 7052 (43.9) | 3701 (49.4) | 0.110 |
| Bed group, n (%) | 0.063 | ||
| 0–300 beds | 6450 (40.1) | 2737 (36.5) | |
| 300–500 beds | 4601 (28.6) | 2354 (31.4) | |
| 500+ beds | 5017 (31.2) | 2407 (32.1) | |
| Hospital region, n (%) | 0.096 | ||
| Midwest | 3755 (23.4) | 1697 (22.6) | |
| Northeast | 2619 (16.3) | 1248 (16.6) | |
| South | 7687 (47.8) | 3745 (49.9) | |
| West | 2007 (12.5) | 808 (10.8) |
IQR, inter-quartile range.
Fig 1.
Unadjusted odds ratios for the associations between time (during COVID-19 vs pre-COVID-19) and patient outcomes. CI, confidence interval.
We identified 83 (1.1% of our 2020 cohort) patients with a hip fracture and concomitant COVID-19 diagnosis. Compared with patients without COVID-19, patients diagnosed with COVID-19 were more likely to be non-white, to have higher comorbidity burden, to be on emergent/urgent/trauma admission, to have Medicare/Medicaid insurance, to have pertrochanteric fracture, and to receive non-surgical treatments. Patients diagnosed with COVID-19 were more commonly admitted to urban and teaching hospitals; the majority of these patients were admitted in hospitals located in the northeast (69.9%). All standardised differences were >0.1 (Table 2 ).
Table 2.
Patient and healthcare characteristics between patients with and without COVID-19 during COVID-19 surge
| Without COVID-19 | With COVID-19 | Standardised difference | |
|---|---|---|---|
| N (%) | 7415 (98.9) | 83 (1.1) | |
| Age, median (IQR) | 81 (71–88) | 81 (72–89) | 0.074 |
| Female, n (%) | 4884 (65.9) | 52 (62.7) | 0.067 |
| Race, n (%) | 0.563 | ||
| Black | 358 (4.8) | 5 (6) | |
| White | 6506 (87.7) | 56 (67.5) | |
| Other | 551 (7.4) | 22 (26.5) | |
| Deyo Index, n (%) | 0.583 | ||
| 0 | 2979 (40.2) | 15 (18.1) | |
| 1 | 965 (13) | 7 (8.4) | |
| 2 | 2055 (27.7) | 38 (45.8) | |
| 3+ | 1416 (19.1) | 23 (27.7) | |
| Source of admission, n (%) | 0.098 | ||
| Clinic | 551 (7.4) | 7 (8.4) | |
| Transfer from other health facility | 1317 (17.8) | 23 (27.7) | |
| Non-healthcare | 5510 (74.3) | 52 (62.7) | |
| Other | 37 (0.5) | 1 (1.2) | |
| Admission type, n (%) | 0.189 | ||
| Elective | 611 (8.2) | 4 (4.8) | |
| Emergent/urgent/trauma | 6761 (91.2) | 79 (95.2) | |
| Other | 43 (0.6) | 0 (0) | |
| Insurance, n (%) | 0.227 | ||
| Commercial | 489 (6.6) | 4 (4.8) | |
| Medicaid | 309 (4.2) | 4 (4.8) | |
| Medicare | 6288 (84.8) | 74 (89.2) | |
| Uninsured | 88 (1.2) | 0 (0) | |
| Unknown | 241 (3.3) | 1 (1.2) | |
| Fracture location, n (%) | 0.104 | ||
| Multiple | 519 (7) | 5 (6) | |
| Neck | 3480 (46.9) | 36 (43.4) | |
| Pertrochanteric | 3110 (41.9) | 39 (47) | |
| Subtrochanteric | 306 (4.1) | 3 (3.6) | |
| Procedure, n (%) | 0.452 | ||
| Non-surgical | 1300 (17.5) | 30 (36.1) | |
| Internal fixation | 3810 (51.4) | 38 (45.8) | |
| Total hip arthroplasty | 506 (6.8) | 3 (3.6) | |
| Hemiarthroplasty | 1799 (24.3) | 12 (14.5) | |
| Urban/rural hospital, n (%) | 0.210 | ||
| Urban | 6177 (83.3) | 75 (90.4) | |
| Rural | 1238 (16.7) | 8 (9.6) | |
| Teaching hospital, n (%) | 3639 (49.1) | 62 (74.7) | 0.548 |
| Bed group, n (%) | 0.087 | ||
| 0–300 beds | 2709 (36.5) | 28 (33.7) | |
| 300–500 beds | 2329 (31.4) | 25 (30.1) | |
| 500+ beds | 2377 (32.1) | 30 (36.1) | |
| Hospital region, n (%) | 0.357 | ||
| Midwest | 1688 (22.8) | 9 (10.8) | |
| Northeast | 1190 (16) | 58 (69.9) | |
| South | 3729 (50.3) | 16 (19.3) | |
| West | 808 (10.9) | 0 (0) |
IQR, inter-quartile range.
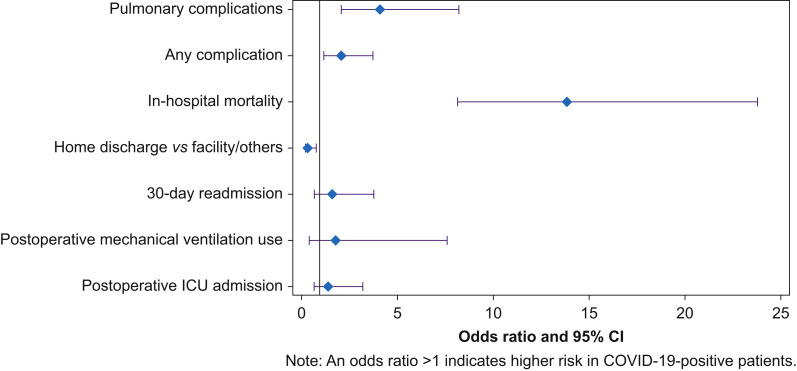
Comparing the outcomes between patients with and without COVID-19 after hip fracture, patients diagnosed with COVID-19 stayed in hospital almost twice as long as patients without COVID-19 (P<0.001) with a median length of stay of 7 days (IQR: 4–12 days) compared with 4 days (IQR: 3–6 days). The in-hospital mortality rate for patients with COVID-19 (22.9%) was 14 times higher (OR 13.9 [95% CI: 8.13, 23.8]; P<0.001) compared with the cohort without COVID-19 (2.1%). Patients with COVID-19 had higher (OR 2.1 [95% CI: 1.18, 3.77]; P<0.001) composite complication rates (41.0%) compared with patients without COVID-19 (14.5%). The most frequently identified complication amongst patients with COVID-19 was pulmonary complications (22.9%), which was significantly higher (OR 4.14 [95% CI: 2.09, 8.2]; P<0.001) than in patients without COVID-19 (4.8%) (Fig 2 ).
Fig 2.
Unadjusted odds ratios for the associations between COVID-19 status (patients with COVID-19 vs patients without COVID-19) and patient outcomes during COVID-19. CI, confidence interval.
Discussion
In this analysis of national claims data, we identified a more than 50% decrease in patients admitted for hip fracture during the COVID-19 surge compared with an identical time period in 2019. Patients with hip fractures during the pandemic were discharged earlier and were less frequently admitted to an ICU, whilst comparable rates of mortality, composite complications, and readmissions were observed between the pre- and post-pandemic eras. COVID-19-positive patients with hip fractures had increased LOS, higher rates of perioperative complications, increased mortality rates, and more frequently received non-surgical treatment.
We identified a significant reduction in the admission volume of patients with hip fractures during the COVID-19 surge compared with the year before. This finding may possibly in part be attributed to the lack of activity during the periods of the stay-at-home orders across the USA. However, numerous studies reported that osteoporotic hip fractures remained unchanged during the COVID-19 pandemic.7 8 These studies represent large single institutional experiences, which are possibly biased by the fact that many trauma patients were redirected to major centres, thus maintaining a relatively high volume at these locations. Consistent with this theory, our data show that during the COVID-19 surge, patients with hip fractures were more likely to be admitted to large teaching hospitals.
Interestingly, the outcomes associated with hip fracture care were not compromised despite the challenges hospitals faced during the COVID-19 surge.23 We found that in-hospital mortality rate, 30 day readmission rate, use of mechanical ventilation, and complication rate were not different between during COVID-19 and pre-COVID-19 cohorts. Patients were discharged 1 day earlier and had a lower chance of being admitted to ICU during COVID-19. Whilst speculative, this may suggest an increased focus to expedite care and remove patients from potential at-risk environments, such as hospitals. In addition, this finding may suggest that previous approaches to patient care in this cohort might be too conservative in the timing of discharge from the hospital. Future studies are needed that may provide further insights into alternative approaches to discharge decisions after surgical repair of hip fractures. Similar reports regarding outcomes of earlier discharge, readmission rate, and complication rates of patients with hip fractures during COVID-19 were published from a high-volume individual institution.22 However, other institutions reported worse outcomes for patients with hip fractures during the COVID-19 pandemic. Increased time from admission to surgical intervention (attributable to extensive COVID-19 testing protocols), lower availability of blood products, and limited operating theatre and staff capacity were commonly noticed in their practice.23, 24, 25, 26
Even though the overall outcome of patients with hip fractures during the pandemic remained similar compared with the pre-COVID-19 era, COVID-19-positive patients experienced significantly increased LOS, higher risk of perioperative complications, and increased mortality rates compared with COVID-19-negative patients. Other authors have also reported significantly worse outcomes amongst COVID-19-positive patients with hip fractures.10 , 12, 13, 14 A meta-analysis showed that COVID-19 was associated with a seven-fold increase in risk of mortality in patients with hip fractures.27 This can be explained by several possible factors that show an overlap in COVID-19 pathophysiology and a common risk profile of patients with hip fractures. Patients diagnosed with COVID-19 are more likely to develop severe pulmonary complications, including pneumonia, acute respiratory distress syndrome (ARDS), and respiratory failure.28 Further, patients with hip fractures are susceptible to thromboembolic complications because of reduced mobility. Coagulopathy in COVID-19 increases the risk of venous thromboembolism and disseminated intravascular coagulation, which further increased the risk for thromboembolic complications.13 , 14 Subsequent inflammation after injuries and surgical procedures, combined with COVID-19-induced cytokine storm, can lead to serious complications, including ARDS and multiple organ dysfunction.27 Last, but not least, older age and high comorbidity burden, which are common characteristics amongst patients with hip fractures, are also associated with increased mortality of COVID-19.
There was no change in non-surgical approach and type of surgical repair observed in 2019 and 2020. Non-operative treatment of hip fractures requires longer recovery time, which increases the risk of pulmonary infection, pressure ulcers, urinary tract infection, lower limb venous thrombosis, and mortality.28 , 29 Mi and colleagues30 found that even though many hip fracture surgeries were delayed during COVID-19, patients with hip fractures were more likely to benefit from delayed surgery rather than non-operative therapy with decreased pain level, better function, and a lower likelihood of developing major complications. However, we found that COVID-19-positive patients with hip fractures were more likely to be treated non-surgically. This is consistent with our finding that COVID-19-positive patients experienced prolonged hospital stay. This finding may have numerous reasons, including lack of necessary resources, the avoidance of airway instrumentation, and a risk–benefit analysis in an already at-high-risk population. Dupley and colleagues31 also reported that patients with COVID-19 were more likely to be deemed non-surgical and treated conservatively for hip fracture. Surgery can trigger excessive inflammation in patients with COVID-19 and decrease patients' immunity, increasing postoperative pulmonary complications. Therefore, considering the high mortality rate, some institutions recommended to carefully plan surgeries for COVID-19-positive patients with hip fractures.30
Our study has limitations. First, whilst Premier, Inc.15 consists of data from approximately 20–25% of all hospital discharges in the USA, there are some patient populations that are not captured within the database (e.g. patients treated at Veterans Affairs hospitals). Second, the geographic-level identifier in Premier is limited to region level, so we were not able to identify the ‘hotspots’ during COVID-19 and control for its effect on patient outcome. Third, the relative difficulty of obtaining COVID-19 testing in March and April 2020 may have resulted in some non-COVID-19 cases actually being unrecognised COVID-19-positive cases. Also, given the relatively small number of COVID-19-positive patients, it is difficult to know how generalisable the present information is. Fourth, the existing database does not contain long-term follow-up information of the COVID-19 cohort yet, so there may be long-term differences that were not yet captured by this study. Lastly, hip fracture repair procedures were identified according to ICD-10 procedure codes. The number of non-operative repair may be overestimated.
Conclusions
The number of hip fracture cases during the COVID-19 surge decreased by 50% compared with the same time period in the previous year. Patients with hip fracture during the pandemic were discharged earlier and were less frequently to be admitted to ICU. In-hospital mortality rate, 30 day readmission rate, use of mechanical ventilation, and complication rate were not different between the COVID-19 pandemic period and the pre-COVID-19 era. COVID-19-positive patients with hip fractures had increased LOS, higher rates of perioperative complications, increased mortality rates, and more frequently received non-surgical treatment. As our society returns to more normal levels of activity, hip fracture volumes are likely to increase to pre-surge levels. Healthcare institutions need to be prepared to manage these patients timely and safely, with special plans for caring for COVID-19-positive patients that experience hip fractures and protecting patients without COVID-19 from in-hospital exposure. Furthermore, incidental findings of shorter hospital length of stay, less ICU utilisation, and more home discharge without compromising outcome deserve further study, with the question of whether pre-pandemic strategies in care for patients with hip fractures should be adjusted.
Authors' contributions
Study design/planning: all authors
Data analysis: HZ, LAW
Interpretation of results: all authors
Preparation of paper: HZ, LAW, JP, SGM
Review of paper: all authors
Revision of paper: HZ.
Declarations of interest
SGM is a director on the boards of the American Society of Regional Anesthesia and Pain Medicine and the Society of Anesthesia and Sleep Medicine. He is a one-time consultant for Sandoz, Inc. and Teikoku, and is currently on the medical advisory board of HATH. He has a pending US patent application for a multicatheter infusion system (US-2017-0361063). He is the owner of SGM Consulting, LLC and co-owner of FC Monmouth, LLC. None of the aforementioned relations influenced the conduct of the present study. All other authors declare that they have no conflicts of interest.
Handling editor: Paul Myles
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.bja.2021.04.003.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
Supplementary material is available at British Journal of Anaesthesia online.
References
- 1.American Academy of Orthopaedic Surgeons . 2020. AAOS guidelines for elective surgery during the COVID-19 pandemic 2020.https://www.aaos.org/globalassets/about/covid-19/georgia-surgery--invasive-elective-procedure-guidelines.pdf [Google Scholar]
- 2.Haut E.R., Leeds I., Livingston D.H. The effect on trauma care secondary to the COVID-19 pandemic: collateral damage from diversion of resources. Ann Surg. 2020;272:e204–e207. doi: 10.1097/SLA.0000000000004105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Randau T.M., Jaenisch M., Haffer H. Collateral effect of COVID-19 on orthopedic and trauma surgery. PLoS One. 2020;15 doi: 10.1371/journal.pone.0238759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hernigou J., Morel X., Callewier A., Bath O., Hernigou P. Staying home during “COVID-19” decreased fractures, but trauma did not quarantine in one hundred and twelve adults and twenty eight children and the “tsunami of recommendations” could not lockdown twelve elective operations. Int Orthop. 2020;44:1473–1480. doi: 10.1007/s00264-020-04619-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sherman W.F., Khadra H.S., Kale N.N., Wu V.J., Gladden P.B., Lee O.C. How did the number and type of injuries in patients presenting to a regional level I trauma center change during the COVID-19 pandemic with a stay-at-home order? Clin Orthop Relat Res. 2021;479:266–275. doi: 10.1097/CORR.0000000000001484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lubbe R.J., Miller J., Roehr C.A. Effect of statewide social distancing and stay-at-home directives on orthopaedic trauma at a southwestern level 1 trauma center during the COVID-19 pandemic. J Orthop Trauma. 2020;34:e343–e348. doi: 10.1097/BOT.0000000000001890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hadfield J.N., Gray A.C. The evolving COVID-19 effect on hip fracture patients. Injury. 2020;51:1411–1412. doi: 10.1016/j.injury.2020.06.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Nuñez J.H., Sallent A., Lakhani K. Impact of the COVID-19 pandemic on an emergency traumatology service: experience at a tertiary trauma centre in Spain. Injury. 2020;51:1414–1418. doi: 10.1016/j.injury.2020.05.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sheikh H.Q., Hossain F.S., Aqil A., Akinbamijo B., Mushtaq V., Kapoor H. A comprehensive analysis of the causes and predictors of 30-day mortality following hip fracture surgery. Clin Orthop Surg. 2017;9:10–18. doi: 10.4055/cios.2017.9.1.10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mi B., Chen L., Xiong Y., Xue H., Zhou W., Liu G. Characteristics and early prognosis of COVID-19 infection in fracture patients. J Bone Jt Surg Am. 2020;102:750–758. doi: 10.2106/JBJS.20.00390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.LeBrun D.G., Konnaris M.A., Ghahramani G.C. Hip fracture outcomes during the COVID-19 pandemic: early results from New York. J Orthop Trauma. 2020;34:403–410. doi: 10.1097/BOT.0000000000001849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Egol K.A., Konda S.R., Bird M.L. Increased mortality and major complications in hip fracture care during the COVID-19 pandemic: a New York City perspective. J Orthop Trauma. 2020;34:395–402. doi: 10.1097/BOT.0000000000001845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kayani B., Onochie E., Patil V. The effects of COVID-19 on perioperative morbidity and mortality in patients with hip fractures. Bone Jt J. 2020;102-B:1136. doi: 10.1302/0301-620X.102B9.BJJ-2020-1127.R1. 45. [DOI] [PubMed] [Google Scholar]
- 14.Muñoz Vives J.M., Jornet-Gibert M., Cámara-Cabrera J. Mortality rates of patients with proximal femoral fracture in a worldwide pandemic: preliminary results of the Spanish HIP-COVID observational study. J Bone Jt Surg Am. 2020;102:e69. doi: 10.2106/JBJS.20.00686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Premier, Inc . 2020. Premier healthcare database white paper: data that informs and performs.https://learn.premierinc.com/white-papers/premier-healthcare-database-whitepaper [Google Scholar]
- 16.Hayashi S., Noda T., Kubo S. Variation in fracture risk by season and weather: a comprehensive analysis across age and fracture site using a national database of health insurance claims in Japan. Bone. 2019;120:512–518. doi: 10.1016/j.bone.2018.12.014. [DOI] [PubMed] [Google Scholar]
- 17.Mazzucchelli R., Crespí-Villarías N., Pérez-Fernández E. Weather conditions and their effect on seasonality of incident osteoporotic hip fracture. Arch Osteoporos. 2018;13:1–8. doi: 10.1007/s11657-018-0438-4. [DOI] [PubMed] [Google Scholar]
- 18.Zamora-Navas P., Esteban-Peña M. Seasonality in incidence and mortality of hip fracture. Rev Esp Cir Ortop Traumatol. 2019;63:132–137. doi: 10.1016/j.recot.2018.05.008. [DOI] [PubMed] [Google Scholar]
- 19.Deyo R.A., Cherkin D.C., Ciol M.A. Adapting a clinical comorbidity index for use with ICD-9-CM administrative databases. J Clin Epidemiol. 1992;45:613–619. doi: 10.1016/0895-4356(92)90133-8. [DOI] [PubMed] [Google Scholar]
- 20.World Health Organization . 2020. Emergency use ICD codes for COVID-19 disease outbreak.https://www.who.int/classifications/icd/covid19/en/#:∼:text=The%20COVID%2D19%20disease%20outbreak,19%20confirmed%20by%20laboratory%20testing [Google Scholar]
- 21.Austin P.C. An introduction to propensity score methods for reducing the effects of confounding in observational studies. Multivariate Behav Res. 2011;46:399–424. doi: 10.1080/00273171.2011.568786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Malik-Tabassum K., Crooks M., Robertson A., To C., Maling L., Selmon G. Management of hip fractures during the COVID-19 pandemic at a high-volume hip fracture unit in the United Kingdom. J Orthop. 2020;20:332–337. doi: 10.1016/j.jor.2020.06.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Slullitel P.A., Lucero C.M., Soruco M.L. Prolonged social lockdown during COVID-19 pandemic and hip fracture epidemiology. Int Orthop. 2020;44:1887–1895. doi: 10.1007/s00264-020-04769-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Patel R., Hainsworth A.J., Devlin K., Patel J.H., Karim A. Frequency and severity of general surgical emergencies during the COVID-19 pandemic: single-centre experience from a large metropolitan teaching hospital. Ann R Coll Surg Engl. 2020;102:1–6. doi: 10.1308/rcsann.2020.0147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Cuthbert R., Ferguson D., Bhamra J.S., Sharma A., Bates P., Haddad F.S. The effects of COVID-19 on perioperative morbidity and mortality in patients with hip fractures. Bone Jt J. 2020;102-B:1136. doi: 10.1302/0301-620X.102B9.BJJ-2020-1127.R1. 45. [DOI] [PubMed] [Google Scholar]
- 26.Yu P., Wu C., Zhuang C. The patterns and management of fracture patients under COVID-19 outbreak in China. Ann Transl Med. 2020;8:932. doi: 10.21037/atm-20-4174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lim M.A., Pranata R. Coronavirus disease 2019 (COVID-19) markedly increased mortality in patients with hip fracture—a systematic review and meta-analysis. J Clin Orthop Trauma. 2021;12:187–193. doi: 10.1016/j.jcot.2020.09.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Sinvani L. The COVID-19 pandemic: experiences of a geriatrician-hospitalist caring for older adults. J Am Geriatr Soc. 2020;68:934–935. doi: 10.1111/jgs.16481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Sinvani L., Goldin M., Roofeh R. Implementation of hip fracture co-management program (AGS CoCare: ortho®) in a large health system. J Am Geriatr Soc. 2020;68:1706–1713. doi: 10.1111/jgs.16483. [DOI] [PubMed] [Google Scholar]
- 30.Mi B., Chen L., Tong D. Delayed surgery versus nonoperative treatment for hip fractures in post-COVID-19 arena: a retrospective study of 145 patients. Acta Orthop. 2020;91:639–643. doi: 10.1080/17453674.2020.1816617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Dupley L., Oputa T.J., Bourne J.T., North West COVID NOF Study Group 30-Day mortality for fractured neck of femur patients with concurrent COVID-19 infection. Eur J Orthop Surg Traumatol. 2021;31:341–347. doi: 10.1007/s00590-020-02778-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.