Abstract
HIV risk perception is a known determinant of HIV prevention behaviors among vulnerable populations. Lesser known is the combined influence of risk perception and efficacy beliefs on PrEP use. We examined the associations between levels of risk perception and strength of efficacy beliefs on intent to use PrEP in a sample of adult Black and Latina women. Guided by the risk perception attitudes (RPA) framework, we used cluster analysis to identify four interpretable groups. We ran analysis of covariance models to determine the relationship between membership in the RPA framework groups and intention to use PrEP. Among the 908 women, the mean age was 29.9 years and participants were Latina (69.4%) and Black (25.6%). Results of the analysis show that women with low perception of HIV risk and strong efficacy beliefs had significantly less intent to use PrEP than women with high risk perception and weak efficacy beliefs.
Keywords: Minority women, HIV, pre-exposure prophylaxis (PrEP), perceived risk, self-efficacy
INTRODUCTION
Heterosexual transmission accounts for 84% of new HIV infections among women in the United States (U.S.; Centers for Disease Control and Prevention [CDC], 2019). Black and Hispanic/Latina women have a twenty- and four-fold, respectively, likelihood of HIV acquisition in their lifetime compared to White women (CDC, 2019; Hess, Hu, Lansky, Mermin, & Hall, 2017). In 2012, the FDA approved pre-exposure prophylaxis (PrEP) as a daily oral medication for HIV-negative individuals to reduce their risk of HIV infection. However, only 4.6% of PrEP users are women (Siegler et al., 2018). Women may experience multiple barriers to PrEP uptake including access to care, cost, and stigma (Calabrese et al., 2018; Collier, Colarossi, & Sanders, 2017; Raifman et al., 2019).
HIV risk perception is another potential barrier to PrEP utilization among Black and Latina women. Low HIV risk perception is a known barrier to PrEP use among men who have sex with men (MSM), but less is known about the relationship between risk perception and PrEP use among women (Biello, Edeza, Montgomery, Almonte, & Chan, 2018; Chan et al., 2016). Health behavior theories (e.g., Health belief model, protection motivation theory) posit that risk perception is a necessary precursor to adopting health promotive and protective behaviors, as they prompt and promote cues to action for behavioral changes or adaptations (Janz & Becker, 1984; Rogers, 1975; Rosenstock, 1974). Throughout health behavior research, measurement of self-perceived risk has been based on probable (likelihood from low to high risk), affective (emotional/worried feelings about risk), and comparative (more/less risk than peers) assessments (Dillard, Ferrer, Ubel, & Fagerlin, 2012; W.M.P. Klein, 2002; Sales & Sheth, 2019). Strong measurement of risk perception should include two or more of these assessments of risk. However, studies often include a single item to measure risk perception (Dillard et al., 2012).
In addition to a more comprehensive evaluation of risk perception, coexisting psychosocial factors that may influence level of risk perception, such as self-efficacy, should also be evaluated. Self-efficacy, defined as the individual’s belief and confidence in their ability to control and/or execute behaviors for favorable outcomes, is a modifiable factor that could be increased using interventions that empower women and strengthen confidence in their ability to use and adhere to PrEP for HIV prevention (DiClemente et al., 2004; El-Bassel et al., 2005; Hobfoll, Jackson, Lavin, Johnson, & Schröder, 2002; Wingood & DiClemente, 2006). Further research examining the role of self-efficacy at each stage of the PrEP care continuum is critical for PrEP scale-up for women.
The risk perception attitude (RPA) framework offers a theoretical perspective that can be used to examine the synergistic effect of risk perception and self-efficacy on the adoption of HIV prevention strategies (Rimal & Real, 2003). The RPA framework classifies people into one of four distinct attitudinal groups of risk perception and efficacy. First, individuals with responsive attitude have high perceived risk as well as high efficacy beliefs and are expected to be most motivated to adopt and execute self-protective behavior. Second, avoidance attitude is characterized by individuals with high risk perception and low efficacy beliefs who may experience conflicting emotions and great concern about their health status yet are less inclined to be motivated to address their health because of their low efficacy beliefs. Third, individuals with proactive attitude have low risk perception yet high efficacy beliefs and are expected to be motivated not by their perception of risk but by their desire to remain healthy/disease free. Finally, both low perception of risk and low efficacy beliefs comprise the indifference attitude. These individuals are likely to be the least motivated, believe they are not vulnerable, and if there were a perceived threat, would not believe in their ability to address or avert the threat. The RPA framework has been utilized predominantly in health communication research to examine information seeking behaviors and audience segmentation for targeted intervention messages in cancer and global HIV research, respectively (Rimal et al., 2009; Rimal & Juon, 2010).
The aim of this study was twofold: first, to identify distinct groups of women who demonstrate theoretically compatible combinations of HIV risk perception and efficacy beliefs based on the RPA framework; and second, to compare the groups of women in relation to intent to use PrEP.
METHODS
STUDY DESIGN
Data were collected from participants who completed the Be PrEPared! online health education curriculum and completed an accompanying online survey administered (Parker, 2018). The Be PrEPared! Education Campaign included an individual educational intervention using curriculum that was developed in partnership with community health specialists and focused on Black and Latina women who were at higher risk of HIV infection (Parker, 2018). Recruitment efforts took place over a 6-month period of time from February 2016 August 2016. Participants were recruited by a statewide web-based campaign across the state of Texas, specifically the cities of Dallas, Fort Worth, San Antonio, and Houston. Eligible participants included HIV-negative, Black and Hispanic/Latina women who were at least 18 years of age. Those targeted for participation included college students from historically Black colleges and universities, individuals receiving services from health service organizations, and peer-led health and well-being support groups for women of color. Recruitment materials included information cards and infographics and were distributed through social media postings on Facebook and Twitter. Additional recruitment included direct email mailings through HIV/AIDS and public health listservs. Participant efforts concluded once a sample size of 1,100 participants was reached. Participants completed a web-based pre-test survey, the Be PrEPared! Intervention modules that featured digital storytelling, and a post-test survey. Only pre-test data, responses from participants prior to receiving and completing the Be PrEPared! Intervention, with no more than 50% of missing data from the survey were included in the current study, resulting in a sample size of 908 women. Participants were compensated $20 for their participation. The study was approved by the Texas Women’s University institutional review board.
MEASURES
Self-reported sociodemographic information such as age, race, income, and relationship status were included to describe our sample and as covariates in our analysis. HIV knowledge was assessed using the HIV Knowledge Questionnaire (HIV-KQ-18), with higher scores indicating greater HIV knowledge (Cronbach’s alpha a = .68; Carey & Schroder, 2002). HIV testing history was assessed by asking participants, “Have you received a HIV test in the past 6 months?” HIV testing responses were dichotomized as yes/no. Interest in using PrEP daily to prevent HIV was assessed using a single item: women rated their agreement with the statement “I would take biomedical HIV prevention strategies such as PrEP to prevent the spread of HIV” on a 4-point Likert-type scale from “Strongly agree” to “Strongly disagree.” PrEP interest responses were dichotomized as yes/no and were only used to describe the study sample. To identify the RPA groups, two cluster determining variables—perceived risk and sexual health self-efficacy—were assessed using existing measures. Perceived risk was measured using the cumulative score from the Perceived Risk of HIV Scale (a = .79; Napper, Fisher, & Reynolds, 2012). The perceived risk scale assessed participants’ perceived risk for acquiring HIV based on probable risk (e.g., “I think my chances of getting infected with HIV are ‘Zero’ to ‘Very high’”), affect/feelings about risk (e.g., “I worry about getting infected with HIV”), and comparative risk (e.g., “My risk of getting infected with HIV is lower than those in my community”). Self-efficacy was measured using the cumulative score from the Sexual Health Practices Self-Efficacy Scale (SHPSES) Sexual Health Care Subscale (a = .72; Koch, Colaco, & Porter, 2013). Respondents indicated their confidence in performing sexual health practices (e.g., “Getting tested for a sexually transmitted infection”).
Our primary outcome was intent to use PrEP and was measured using an Intent to Use PrEP scale. This scale is an adapted version of the Clinical Research Involvement Scale (CRIS; a = .89; Frew et al., 2010). Intent to use PrEP was assessed by asking women to rate their agreement with statements describing PrEP attitudes and behaviors using a 4-point Likert-type scale (a = .86). A higher score indicated greater intent to use PrEP.
ANALYSIS
To explore and identify groups that were interpretable based on the RPA framework theory and prior research, nonhierarchical (k-means) cluster analysis was conducted with the perceived risk and self-efficacy standardized scores as the clustering variables in order to explore and identify groups that were interpretable based on the RPA framework theory and prior research. This cluster analysis attempts to assign respondents into exclusive groups based on within group similarities (perceived risk and self-efficacy) and also being dissimilar to instances of all other groups (Davidson, 2002). Solutions from two up to ten were considered until groups appeared redundant. The four-group solution converged in nine iterations, yielding four clusters corresponding to the four-risk perception attitude framework groups (Figure 1). To analyze the relationship between cluster membership and intent to use PrEP, analysis of covariance (ANCOVA) was conducted. A Bonferroni adjustment was used for each group of analyses. All analyses were conducted in SPSS (IBM, 2018).
FIGURE 1.
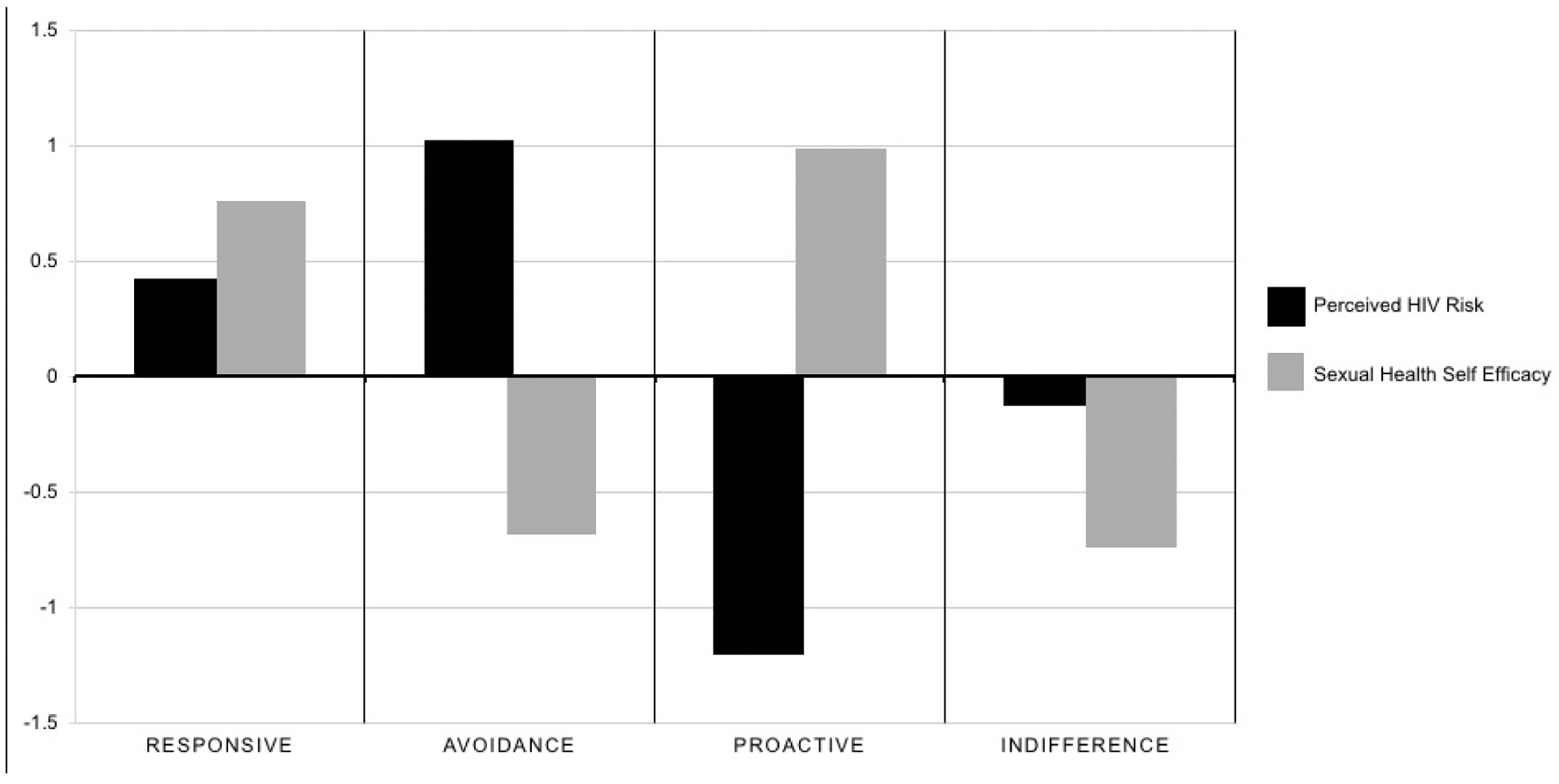
Perceived HIV risk and sexual health self-efficacy: four clusters corresponding to the four risk perception attitude framework groups.
RESULTS
RESPONDENT CHARACTERISTICS
Table 1 displays characteristics of the 908 women included in this study. The mean age was 29.9 years (range 24–35), most were Latina (73.7%) and over a quarter were Black (26.3%). Most (89.3%) were in a relationship, had at least a bachelor’s degree (60.1%) and 82.5% had an annual income of $80,000 or higher. In the prior 6 months most (82.7%) had received an HIV test. Nearly all (96.0%) reported interest in using PrEP for HIV prevention.
TABLE 1.
Participants’ Demographic Characteristics and RPA Clusters
| Characteristics, n (%) | Clusters | Total | |||
|---|---|---|---|---|---|
| Responsive | Avoidance | Proactive | Indifference | ||
| High Risk/Strong Efficacy | High Risk/Weak Efficacy | Low Risk/Strong Efficacy | Low Risk/Weak Efficacy | ||
| (n = 189) | (n = 226 ) | (n = 220) | (n = 273) | (n = 908) | |
| Age, M (SD) | 30.5 (6.0) | 27.7 (3.5) | 34.1 (6.7) | 28.0 (3.9) | 29.9 (5.7) |
| Race | |||||
| Latina | 124 (65.6) | 210 (92.9) | 118 (53.6) | 217 (79.5) | 669 (73.7) |
| Black | 65 (34.4) | 16 (7.1) | 102 (46.4) | 56 (20.5) | 239 (26.3) |
| Relationship Status | |||||
| Single | 32 (16.9) | 11 (4.9) | 25 (11.4) | 29 (10.6) | 97 (10.7) |
| In relationship/dating | 157 (83.1) | 215 (95.1) | 195 (88.6) | 244 (89.4) | 911 (89.3) |
| Education | |||||
| High school grad/some college | 67 (35.4) | 82 (36.3) | 70 (31.8) | 143 (52.4) | 362 (39.9) |
| Bachelor’s or higher degree | 122 (64.6) | 144 (63.7) | 150 (68.2) | 130 (47.6) | 546 (60.1) |
| Income (USD) | |||||
| Less than 80,000 | 42 (22.2) | 17 (7.5) | 58 (26.4) | 39 (14.3) | 156 (17.5) |
| 80,000+ | 143 (75.6) | 209 (92.5) | 156 (70.9) | 228 (83.5) | 736 (82.5) |
| HIV test in the past 6 months | |||||
| Yes | 154 (81.5) | 219 (96.9) | 146 (63.4) | 227 (83.2) | 746 (82.7) |
| No | 33 (17.5) | 7 (3.1) | 73 (33.2) | 43 (15.8) | 156 (17.3) |
| PrEP interest | |||||
| Yes | 185 (97.8) | 222 (98.2) | 208 (94.5) | 257 (94.1) | 872 (96.0) |
| No | 4 (2.1) | 4 (1.8) | 12 (5.5) | 16 (5.9) | 36 (4.0) |
| HIV knowledge, M (SD) | 8.7 (2.8) | 8.5 (1.8) | 9.3 (3.6) | 8.1 (2.4) | 8.6 (2.8) |
| Cluster-determining variables | |||||
| Perceived HIV risk, M (SD) | 23.6 (2.7) | 25.2 (1.6) | 20.3 (3.5) | 22.9 (3.2) | 23.1 (3.3) |
Note. RPA: Risk perception attitudes; HIV: human immunodeficiency virus; PrEP: pre-exposure prophylaxis.
RPA FRAMEWORK GROUPS
Characteristics of the four (4) RFA groups are shown in Table 1. The largest RPA group (n = 273) was the indifference group (low risk/low efficacy). The average age of the proactive group was 34.1 years, making it the oldest group, and the avoidant group was the youngest group (mean 27.8 years). The proactive group had the largest proportion of Black women (46.4%), lower income women (26.4%), women with a bachelor’s degree or higher (68.2%), and the smallest proportion of respondents who reported HIV testing in the past 6 months (63.4%) compared to other RPA groups. The avoidance group had the largest proportion of Latina women (92.9%), respondents who were in a relationship (95.1%), women with higher income (92.5%), and the largest proportion of respondents who reported HIV testing in the past 6 months (96.9%). HIV knowledge mean scores were highest in the proactive group (M = 9.3, SD = 3.6) and lowest in the indifference group (M = 8.1, SD = 2.4). Mean perceived HIV risk scores were highest in the avoidance group (M = 25.2, SD = 1.6) and lowest in the proactive group (M = 20.3, SD = 3.5). Self-efficacy scores were highest in the proactive group (M = 16.5, SD = 1.5) and lowest in the indifference group (M = 12.1, SD = 1.5). To further describe the sample, we used a single-item variable to assess PrEP interest and found that interest in PrEP was high across all groups (>90%). The avoidance group has the largest proportion of women interested in PrEP (98.2%) and the indifference groups has the smallest (94.1%) compared to the other RPA groups, and these proportions differed marginally.
INTENT TO USE PREP
Results from the ANCOVA model are described in Table 2. In the overall model, adjusting for age, race, income, relationship status, and HIV knowledge score, membership in an RPA group was significantly associated with intent to use PrEP (p < .0001). Risk perception attitude framework membership was associated with intent to use PrEP risk (p < .0001).
TABLE 2.
Intent to Use PrEP Outcomes of the Risk Perception Attitude (RPA) Framework Groups
| Responsive | Avoidance | Proactive | Indifference | F(3, 948)b | |
|---|---|---|---|---|---|
| High Risk/Strong Efficacy | High Risk/Weak Efficacy | Low Risk/Strong Efficacy | Low Risk/Weak Efficacy | ||
| (n = 189) | (n = 226 ) | (n = 220) | (n = 273) | ||
| Intent to use PrEP, M (SD)a | 91.1 (8.5) | 93.5 (4.5) | 86.4 (9.6) | 92.1 (7.8) | 11.6 |
Note.
Higher scores represent stronger intent to use PrEP. Covariates appearing in the model included income, relationship status, age, race, and HIV Knowledge score. The overall model was significant, F(8, 948) = 45.6, p < .000. Adj. R-squared = .273.
Risk perception attitude group membership was associated with intent to use PrEP (p < .000).
Post-hoc analyses revealed that the avoidance group had a significantly higher intent to use PrEP mean score (M = 93.5, SD = 4.5), than both the responsive and the proactive group’s mean scores (p < .001). The proactive group’s intent to use PrEP mean score was significantly lower than all other groups (M = 86.4, SD = 9.6). The proactive group’s mean scores were 7.09 points lower than the avoidant group (p < .001), 5.62 points lower than the indifference group (M = 92.1, SD = 7.8, p < .001), and 4.66 points lower than the responsive group’s mean score (M = 91.1, SD = 8.5, p < .001). The responsive, indifferent, and avoidance groups did not significantly differ from each other with respect to intent to use PrEP.
DISCUSSION
This is the first study to explore the application of the RPA framework to identify relationships between risk perception, efficacy beliefs, and intentions to use PrEP among Black and Latina women. We found that while the majority of our sample were interested in PrEP use (96%), the extent of intent to use PrEP differed significantly based on RPA group membership. Our findings suggest that HIV risk perception and sexual health self-efficacy are factors that could help identify PrEP motivated women to initiate engagement in the PrEP care continuum.
Intent to use PrEP was highest among the avoidance and indifference groups. Weak sexual health efficacy belief was the underlying characteristic of both groups, which suggests that confidence in ability to engage in sexual health decisions influences intention to use PrEP. We would expect the groups characterized by strong sexual health efficacy beliefs would have higher intent to use in PrEP scores than other groups, however the scores were the lowest among the responsive and proactive groups. Prior studies of other HIV prevention strategies (e.g., condom use) have indicated that efficacy is a key factor to consider when encouraging risk reduction behaviors (Reid, Dovidio, Ballester, & Johnson, 2014; Wingood & DiClemente, 2006). Self-efficacy is a known factor associated with condom use for HIV prevention among women (Nesoff, Dunkle, & Lang, 2016; Peipert et al., 2007). However, existing HIV prevention strategies, including condom efficacy, requires women to interact with their sexual partner (e.g., condom negotiation), as distinct from PrEP use, which presumably circumvents that interaction (e.g., it’s self-administered). Hormonal contraception is similar to once-daily PrEP in that it requires women to seek a health care provider, fill and renew prescriptions, and adhere to self-administered prescription dosages. Existing studies that have examined women’s motivations or belief in their ability to prevent pregnancy have found that strong efficacy beliefs are associated with prescription contraception use and adherence in various populations (Hamidi, Deimling, Lehman, Weisman, & Chuang, 2018; Tomaszewski, Aronson, Kading, & Morisky, 2017). Consistent with these findings, interventions to increase self-efficacy among Black and Latina women found a positive association with increased self-efficacy and HIV knowledge and condom use (Cianelli, Villegas, McCabe, de Tantillo, & Peragallo, 2017; C. H. Klein, Lomonaco, Pavlescak, & Card, 2013; Peragallo, Gonzalez-Guarda, McCabe, & Cianelli, 2012). Our findings suggest that there may be characteristics about PrEP that attract women who have weak efficacy beliefs, this may include younger women, women experiencing intimate partner violence, or those who lack support from peers and sexual partners. This may reflect the ways in which PrEP, as a woman-controlled self-administered prevention strategy, can empower women who would otherwise report lacking motivation or confidence in their ability to negotiate safe sex and control their sexual health. It is important for providers to note that PrEP intention may not reflect women’s comfort and confidence in adherence to PrEP. It is essential to understand PrEP self-efficacy among women to improve implementation for Black and Latina women at all steps of the PrEP care continuum.
We found that intent to use PrEP scores were differed significantly between groups with high and low risk perception. Intent to use PrEP was significantly lower among women in the proactive group (low risk perception) and higher among women in the avoidance group (high risk perception). Prior studies have demonstrated that low HIV risk perception is a barrier to motivating women to adopt HIV risk reduction behaviors such as HIV testing (Ford, Daniel, & Miller, 2006). However, self-assessment of risk of HIV infection among women may not accurately reflect actual HIV vulnerability, as studies have demonstrated that PrEP eligible women tend to underestimate their risk of HIV acquisition (Rutledge, Madden, Ogbuagu, & Meyer, 2018). Therefore, it is important to assess both attitudes and behaviors among women that are vulnerable to HIV infection that are PrEP-eligible. Consistent with our findings, evidence has shown that heightened HIV risk perception is associated with high PrEP acceptability among women in the U.S. (Garfinkel, Alexander, McDonald-Mosley, Willie, & Decker, 2017). These results may reflect women in our sample’s awareness of the behaviors they engage in that increase their risk of HIV infection and an interest in reducing their risk. However, women who perceive themselves to be at-risk of HIV infection, may not practice risk reduction behaviors (Sewell & Blankenship, 2019). Therefore, PrEP scale-up for women requires both consistent and tailored messaging about HIV and PrEP, and capacity building in clinical and community health care settings that serve Black and Latina women to minimize structural barriers to uptake and support PrEP engagement and adherence.
It should be noted that we used a single-item measurement of PrEP interest to describe the sample and found that the avoidance group had the highest proportion of PrEP interest and the indifference had the lowest within each group, and these proportions differed marginally. However, our outcome variable, which is a multidimensional measurement of PrEP intent, revealed significant differences in PrEP intent between groups, the avoidance remained the group with the greatest intent to use PrEP, and instead of the indifference group, the proactive group had the lowest intent to use PrEP scores. This observation in findings suggest that the multidimensional measurement of PrEP intent is distinct from the dichotomous interest in PrEP variable.
LIMITATIONS
These findings should be interpreted considering the following study limitations. The current study used cross-sectional survey data to examine potential PrEP use, which does not provide information about actual PrEP use and adherence. The recruitment strategy used convenience sampling in cities in the state of Texas of the U.S., thus potentially limiting generalizability. We were unable to assess recruitment site characteristics and potential bias caused by attrition. Our study explored attitudes about potential PrEP use without assessing indications for PrEP based on CDC criteria. Some participants who reported intentions to use PrEP may not meet CDC indications for PrEP use, while some participants who did not report intentions to use PrEP may in fact have had indications. Additional research should assess the relationship between CDC indications for PrEP and intent to use PrEP among women. Despite these limitations, this study introduced new knowledge regarding perceived risk and efficacy beliefs and potential PrEP use in an understudied sample of Black and Latina women.
CONCLUSIONS
PrEP is an effective approach for HIV prevention for Black and Latina women that has the potential to increase attitudes of empowerment and control of sexual health decisions (Bond & Gunn, 2016). The findings that sexual health efficacy may influence women’s intentions to use PrEP encourages us to consider interventions and counseling approaches that empower women to make informed and self-motivated HIV prevention choices. Self-efficacy is a modifiable factor that could be increased using interventions that empower women and strengthen confidence in their ability to use and adhere to PrEP for HIV prevention. Further research examining the role of self-efficacy at each stage of the PrEP care continuum is critical for PrEP scale-up for women. Further research is required to examine the relationship between self-efficacy and perception of HIV risk for PrEP adoption among women of color. The potential of a mediating/moderating relationship between self-efficacy and perception of HIV risk could reveal important pathways to intent to use PrEP and inform behavioral interventions to address the modifiers. Further, the application of the RPA framework and other similar models has the potential to improve PrEP scale-up strategies and implementation of HIV interventions for women.
Acknowledgments
WCS is supported by NIH grant T32 DA15035. RRP is supported by the Washington University Institute of Clinical and Translational Sciences grant UL1TR000448, subaward KL2TR000450, from the National Center for Advancing Translational Sciences of the National Institutes of Health, and NIH R25MH83620. JLM has consulted on a grant to Kaiser Permanente Northern California from Gilead Sciences, outside the submitted work. JLM is supported by the National Institute of Allergy and Infectious Diseases (K01AI122853). PAC is supported by NIH grants R34DA042648, R34MH110369, R21MH113431, R21MH109360, R34MH109371, and R01MH114657. DSK has received research support through grants from Gilead Sciences to his institution, has consulted on a grant to Fenway Health from Gilead Sciences, and has received funding for developing medical education content for Medscape, DKBmed, MED-IQ, and Uptodate, Inc. KP has received research support through grants from Gilead Sciences to her institution. SB has no funding sources to disclose. The above funding sources had no role in the study design, collection/analysis/interpretation of data, or manuscript preparation.
Footnotes
The data set associated with this article is available from the Be PrEPared! Research team in Denton, Texas.
REFERENCES
- Biello KB, Edeza A, Montgomery MC, Almonte A, & Chan PA (2018). Risk perception and interest in HIV pre-exposure prophylaxis among men who have sex with men with rectal gonorrhea and chlamydia infection. Archives of Sexual Behavior, 48, 1185–1190. 10.1007/s10508-018-1260-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bond KT, & Gunn AJ (2016). Perceived advantages and disadvantages of using pre-exposure prophylaxis (PrEP) among sexually active Black women: An exploratory study. Journal of Black Sexuality and Relationships, 3, 1–24. 10.1353/bsr.2016.0019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Calabrese SK, Dovidio JF, Tekeste M, Taggart T, Galvao RW, Safon CB, … Kershaw TS (2018). HIV pre-exposure prophylaxis stigma as a multidimensional barrier to uptake among women who attend Planned Parenthood. JAIDS: Journal of Acquired Immune Deficiency Syndromes, 79, 46–53. 10.1097/QAI.0000000000001762 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carey MP, & Schroder KEE (2002). Development and psychometric evaluation of the Brief HIV Knowledge Questionnaire. AIDS Education and Prevention, 14, 172–182. 10.1521/aeap.14.2.172.23902 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. (2019). Estimated HIV incidence and prevalence in the United States, 2010–2016. HIV Surveillance Supplemental Report 2019, 24. Retrieved from http://www.cdc.gov/hiv/library/reports/hiv-surveillance.html [Google Scholar]
- Chan PA, Glynn TR, Oldenburg CE, Montgomery MC, Robinette AE, Almonte A, … Nunn AS (2016). Implementation of preexposure prophylaxis for human immunodeficiency virus prevention among men who have sex with men at a new england sexually transmitted diseases clinic. Sexually Transmitted Diseases, 43, 717–723. 10.1097/OLQ.0000000000000514 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cianelli R, Villegas N, McCabe BE, de Tantillo L, & Peragallo N (2017). Self-efficacy for HIV prevention among refugee Hispanic women in South Florida. Journal of Immigrant and Minority Health, 19(4), 905–912. 10.1007/s10903-016-0462-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Collier KL, Colarossi LG, & Sanders K (2017). Raising awareness of pre-exposure prophylaxis (PrEP) among women in New York City: Community and provider perspectives. Journal of Health Communication, 22, 1–7. 10.1080/10810730.2016.1261969 [DOI] [PubMed] [Google Scholar]
- Davidson I (2002). Technical Report: Understanding K-means non-hierarchical clustering. SUNY Albany. [Google Scholar]
- DiClemente RJ, Wingood GM, Harrington KF, Lang DL, Davies SL, Hook III EW, … Robillard A (2004). Efficacy of an HIV prevention intervention for African American adolescent girls. JAMA, 292, 171–179. 10.1001/jama.292.2.171 [DOI] [PubMed] [Google Scholar]
- Dillard AJ, Ferrer RA, Ubel PA, & Fagerlin A (2012). Risk perception measures’ associations with behavior intentions, affect, and cognition following colon cancer screening messages. Health Psychology, 31, 106–113. 10.1037/a0024787 [DOI] [PubMed] [Google Scholar]
- El-Bassel N, Witte SS, Gilbert L, Wu E, Chang M, Hill J, & Steinglass P (2005). Long-term effects of an HIV/STI sexual risk reduction intervention for heterosexual couples. AIDS and Behavior, 9, 1–13. 10.1007/s10461-005-1677-0 [DOI] [PubMed] [Google Scholar]
- Ford CL, Daniel M, & Miller WC (2006). High rates of HIV testing despite low perceived HIV risk among African-American sexually transmitted disease patients. Journal of the National Medical Association, 98, 841–844. [PMC free article] [PubMed] [Google Scholar]
- Frew PM, Hou S-I, Davis M, Chan K, Horton T, Shuster J, … del Rio C (2010). The likelihood of participation in clinical trials can be measured: The Clinical Research Involvement Scales. Journal of Clinical Epidemiology, 63, 1110–1117. 10.1016/j.jclinepi.2009.12.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garfinkel DB, Alexander KA, McDonald-Mosley R, Willie TC, & Decker MR (2017). Predictors of HIV-related risk perception and PrEP acceptability among young adult female family planning patients. AIDS Care, 29, 751–758. 10.1080/09540121.2016.1234679 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hamidi OP, Deimling T, Lehman E, Weisman C, & Chuang C (2018). High self-efficacy is associated with prescription contraceptive use. Women’s Health Issues, 28, 509–513. 10.1016/j.whi.2018.04.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hess KL, Hu X, Lansky A, Mermin J, & Hall HI (2017). Lifetime risk of a diagnosis of HIV infection in the United States. Annals of Epidemiology, 27, 238–243. 10.1016/j.annepidem.2017.02.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hobfoll SE, Jackson AP, Lavin J, Johnson RJ, & Schröder KEE (2002). Effects and generalizability of communally oriented HIV-AIDS prevention versus general health promotion groups for single, inner-city women in urban clinics. Journal of Consulting and Clinical Psychology, 70, 950–960. 10.1037/0022-006X.70.4.950 [DOI] [PubMed] [Google Scholar]
- IBM. (2018). IBM SPSS Software.
- Janz NK, & Becker MH (1984). The Health Belief Model: A decade later. Health Education Quarterly, 11, 1–47. 10.1177/109019818401100101 [DOI] [PubMed] [Google Scholar]
- Klein CH, Lomonaco CG, Pavlescak R, & Card JJ (2013). WiLLOW: Reaching HIV-positive African-American women through a computer-delivered intervention. AIDS and Behavior, 17(9), 3013–3023. 10.1007/s10461-013-0479-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klein WMP (2002). Comparative risk estimates relative to the average peer predict behavioral intentions and concern about absolute risk. Risk Decision and Policy, 7, 193–202. 10.1017/s1357530902000613 [DOI] [Google Scholar]
- Koch PB, Colaco C, & Porter AW (2013). Sexual Health Practices Self-Efficacy Scale. In Fisher TD, Davis CM, & Yerber WL (Eds.), Handbook of sexuality-related measures (3rd ed., p. 345). New York, NY: Routledge [Google Scholar]
- Napper LE, Fisher DG, & Reynolds GL (2012). Development of the Perceived Risk of HIV scale. AIDS and Behavior, 16, 1075–1083. 10.1007/s10461-011-0003-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nesoff ED, Dunkle K, & Lang D (2016). The impact of condom use negotiation self-efficacy and partnership patterns on consistent condom use among college-educated women. Health Education and Behavior, 43, 61–67. 10.1177/1090198115596168 [DOI] [PubMed] [Google Scholar]
- Parker K (2018). Be-PrEPared: Increasing knowledge & awareness about HIV/AIDS and PrEP utilizing a comprehensive women’s health approach. Retrieved December 3, 2019, from http://be-prepared.org/
- Peipert JF, Lapane KL, Allsworth JE, Redding CA, Blume JL, Lozowski F, & Stein MD (2007). Women at risk for sexually transmitted diseases: Correlates of intercourse without barrier contraception. American Journal of Obstetrics and Gynecology, 197, 474.e1–474.e8. 10.1016/j.ajog.2007.03.032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peragallo N, Gonzalez-Guarda RM, McCabe BE, & Cianelli R (2012). The efficacy of an HIV risk reduction intervention for Hispanic women. AIDS and Behavior, 16(5), 1316–1326. 10.1007/s10461-011-0052-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Raifman JR, Schwartz SR, Sosnowy CD, Montgomery MC, Almonte A, Bazzi AR, … Chan PA (2019). Pre-exposure prophylaxis awareness and use among cisgender women at a sexually transmitted disease clinic. JAIDS: Journal of Acquired Immune Deficiency Syndromes, 80, 36–39. 10.1097/QAI.0000000000001879 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reid AE, Dovidio JF, Ballester E, & Johnson BT (2014). HIV prevention interventions to reduce sexual risk for African Americans: The influence of community-level stigma and psychological processes. Social Science & Medicine, 103, 118–125. 10.1016/j.socscimed.2013.06.028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rimal RN, Brown J, Mkandawire G, Folda L, Böse K, & Creel AH (2009). Audience segmentation as a social-marketing tool in health promotion: Use of the risk perception attitude framework in HIV prevention in Malawi. American Journal of Public Health, 99, 2224–2229. 10.2105/AJPH.2008.155234 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rimal RN, & Juon HS (2010). Use of the risk perception attitude framework for promoting breast cancer prevention. Journal of Applied Social Psychology, 40, 287–310. 10.1111/j.1559-1816.2009.00574.x [DOI] [Google Scholar]
- Rimal RN, & Real K (2003). Perceived risk and efficacy beliefs as motivators of change: Use of the risk perception attitude (RPA) framework to understand health behaviors. Human Communication Research, 29, 370–399. 10.1093/hcr/29.3.370 [DOI] [Google Scholar]
- Rogers RW (1975). A protection motivation theory of fear appeals and attitude change. Journal of Psychology, 91, 93–114. 10.1080/00223980.1975.9915803 [DOI] [PubMed] [Google Scholar]
- Rosenstock IM (1974). The Health Belief Model and preventive health behavior. Health Education Monographs, 2, 354–386. 10.1177/109019818801500203 [DOI] [PubMed] [Google Scholar]
- Rutledge R, Madden L, Ogbuagu O, & Meyer JP (2018). HIV risk perception and eligibility for pre-exposure prophylaxis in women involved in the criminal justice system. AIDS Care, 30, 1282–1289. 10.1080/09540121.2018.1447079 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sales JM, & Sheth AN (2019). Associations among perceived HIV risk, behavioral risk and interest in PrEP among black women in the southern US. AIDS and Behavior, 23, 1871–1876. 10.1007/s10461-018-2333-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sewell WC, & Blankenship SA (2019). Perceived HIV risk as a predictor of sexual risk behaviors and discrimination among high-risk women. AIDS Care, 31, 675–680. 10.1080/09540121.2018.1533234 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Siegler AJ, Mouhanna F, Giler RM, Weiss K, Pembleton E, Guest J, … Sullivan PS (2018). The prevalence of pre-exposure prophylaxis use and the pre-exposure prophylaxis–to-need ratio in the fourth quarter of 2017, United States. Annals of Epidemiology, 28, 841–849. 10.1016/j.annepidem.2018.06.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tomaszewski D, Aronson BD, Kading M, & Morisky D (2017). Relationship between self-efficacy and patient knowledge on adherence to oral contraceptives using the Morisky Medication Adherence Scale (MMAS-8). Reproductive Health, 14, 1–7. 10.1186/s12978-017-0374-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wingood GM, & DiClemente RJ (2006). Enhancing adoption of evidence-based HIV interventions: Promotion of a suite of HIV prevention interventions for African American women. AIDS Education and Prevention, 18(Suppl. A), 161–170. 10.1521/aeap.2006.18.supp.161 [DOI] [PubMed] [Google Scholar]


