Abstract
Mania, the core feature of bipolar disorder, is associated with heightened and positive emotion responding. Yet, little is known about the underlying cognitive processes that may contribute to heightened positive emotionality observed. Additionally, while previous research has investigated positive emotion biases in non-clinical samples, few if any, account for subthreshold clinical symptoms or traits, which have reliably assessed psychopathological risk. The present study compared continuous scores on a widely used self-report measure of hypomania proneness (HPS-48) with a dot-probe task to investigate attentional biases for happy, angry, fearful, and neutral faces among 66 college student participants. Results suggested that hypomania proneness was positively associated with attentional bias towards happy, but not angry or fearful faces. Results remained robust when controlling for positive affect and did not appear to be affected by negative affect or current symptoms of depression, anxiety, and stress. Findings provide insight into potential behavioural markers that co-occur with heightened positive emotional responding and hypomania in emerging adults.
Keywords: Mania, bipolar disorder, positive emotion, attention, emerging adults
Emerging Adulthood (EA; ages 18–25) is a unique lifespan period when individuals frequently encounter major life transitions – including beginning and attending college – and associated vulnerability to emotional disorders. Moreover, risk for and diagnosis of mania or hypomania (cardinal symptoms of bipolar disorder) is associated with persistent and dys-regulated emotion responding (e.g. Gruber, 2011; Gruber et al., 2008; Johnson et al., 2007). Facial affect processing has been identified as one of the most consistent affective cognition deficits in bipolar disorder (BD; for review see Miskowiak et al., 2019). Hence, there is a critical need to prioritise research that examines affective processes that may help better understand mania propensity in college students during the EA period. One promising route towards identifying such mechanisms is to explore attentional related biases in the context of emotional stimuli. Yet few studies to date have specifically examined attention related biases in the context of hypomania and mania proneness and the maintenance of disorders of dysfunctional positive emotion. This is particularly important when identifying potential domains of mood-related vulnerability in emerging adults.
Hypomania proneness and positive emotion disturbance in emerging adults
Individuals at increased vulnerability or proneness for hypomania experience exaggerated and persistent positive emotionality across contexts as measured by self-report and physiological reactivity (e.g. Gruber, 2011; Gruber et al., 2008). For example, increased proneness to mania was associated with increased self-report greater positive affect in everyday life (Gruber & Johnson, 2009) as well as when viewing emotionally evocative films in high risk compared to low mania risk adults (Gruber et al., 2008). These findings are consistent with related studies of adults with a clinical history of mania (i.e. diagnosis of BD), currently inter-episode (i.e. not currently manic, depressed or mixed-episode), which also suggest an increased magnitude of positive emotion responding as measured by self-reports to images (M’Bailara et al., 2009) and while responding to pleasant stimuli in laboratory settings and in their daily lives (Johnson et al., 2007). In sum, both an increase in proneness for hypomania in subclinical individuals and a clinical history of mania in clinically diagnosed adults has been associated with heightened positive emotion responding across positive, negative and neutral contexts.
Attention Bias for Emotional Stimuli in Hypomania. One important next step in understanding positive emotion disturbance in hypomania and mania involves isolating cognitive processes such as attention that may contribute to, or be affected by, emotional states. One well-validated tool to measure positive emotion attentional biases is with the “modified” dot-probe task (Wirth & Wentura, 2020). Modified dot-probe tasks require participants to discriminate between two types of target stimuli rather than merely detecting the presence of a target and have been used to assess attentional biases for emotional faces (Leyman et al., 2009; Putman et al., 2007). While varying versions of probe tasks have not demonstrated a consistent positive emotion bias in non-clinical samples (for review see Wirth & Wentura, 2020), versions of the dot-probe task have enabled important insights into the role of positive-emotion attentional biases when accounting for affective risk and in the neurobiology of affective disorders (e.g. Fox et al., 2009; Putman et al., 2007).
Initial research examining attention biases in the context of positive affectivity suggests that after a positive emotion induction, healthy adults spent significantly less time looking at negative stimuli (Wadlinger & Isaacowitz, 2008). Similarly, optimism, which is often coupled with high levels of positive emotion, is associated with gaze preferences away from negative health-related images (e.g. cancer tumour images; Isaacowitz, 2005) and trait happiness is associated with increased sustained attention towards positive versus neutral images (Raila et al., 2015). In sum, positive-emotion related attention biases have been explored in non-clinical samples, yet comparably less work has investigated how subclinical variables such as hypomanic, depressive, or anxious traits may be associated with attentional biases due to sustained positive affectivity and difficulties managing positive mood.
In recent years visual attentional biases in populations characterised by positive emotion disturbance, such as BD, have begun to be examined. Studies using dot-probe tasks report no significant group differences between inter-episode BD patients and healthy controls in attentional biases for positive or negative emotional words (Jabben et al., 2012) or human faces (Peckham et al., 2015). We note, however, that one study using a combined spatial cueing dot-probe task reported that both inter-episode and mildly depressed BD patients demonstrate attentional bias away from positive words compared to healthy controls (Jongen et al., 2007). Taken together, however, studies examining clinically diagnosed BD populations have not found robust group differences in attention-related biases to emotional stimuli.
There are comparably fewer studies examining hypomania proneness in emerging adults to address whether these patterns generalise to clinically high risk or subclinical groups prior to the emergence of clinical mood symptoms. One study examining youth at-risk for mania (i.e. with a parent with a clinical diagnosis of BD) suggested deficits in face emotion recognition (e.g. Brotman et al., 2008). Another study examining undergraduate students at putative high or low risk for bipolar spectrum disorders (using the Mood Disorder Questionnaire) reported no group differences using an attentional dot-probe task for emotionally threatening negative, positive words matched with a neutral word (Rock et al., 2010). Despite these initial results, it remains inconclusive whether patterns of attentional biases to emotional stimuli might exist along dimensional variation in hypomania proneness as well as prior to the formal onset of BD among adults at risk for mania. It is critical to conduct investigations in this area observed findings prior to onset can significantly inform etiological conceptualizations, as they occur prior to medication usage, and are needed to better flesh out potential attentional biases that may be apparent in vulnerable developmental periods for affective difficulties in emerging adults.
The present investigation
The goal of the present study is to examine whether attentional biases for emotional stimuli among college students in association with severity of self-reported hypomania proneness. Specifically, we examined attentional biases for emotionally relevant stimuli using a modified dot-probe task that measured attentional bias for happy, angry, and fearful emotional faces. This approach enabled us to test two non-mutually exclusive hypotheses. The first hypothesis (positive amplification) predicts that increased hypomania proneness would be associated with attentional biases towards positive (i.e. happy faces), but not for negative (i.e. fearful or angry faces), emotional stimuli (for discussion Gruber, 2011). The second hypothesis (negative attenuation) predicts that increased hypomania proneness would be associated with attentional biases away from negative emotional stimuli (i.e. fearful and angry faces), grounded in research suggesting that patients with a clinical history of BD exhibit impaired recognition of negative facial expressions and fail to demonstrate attentional biases towards negative stimuli and demonstrate difficulties maintaining negative emotional information (Gruber et al., 2013; Lembke & Ketter, 2002). The present investigation sought to examine potential sources of evidence for these non-mutually exclusive perspectives.
Method
Participants and procedure
Participants were 66 college students at least 18 years of age (14 males, Mage = 18.68 years, SD = 2.02) recruited from the University of Western Australia who were tested individually in a quiet room. Participants self-reported positive (PA) and negative (NA) affect using the Positive and Negative Affect Schedule (PANAS), and depressive and anxious symptomatology using the Depression Anxiety Stress Scales (DASS-21). They then completed the emotional faces dot-probe task. In the task two faces of the same individual appearing simultaneously on either side of the fixation cross for 500 ms. Immediately after the presentation of face pairs, two black target dots (: or ..) appeared behind one of the faces and participants identified the orientation (vertical or horizontal) by pressing one of two labelled keys. On emotion trials, one face displayed happiness, fear, or anger while the other displayed a neutral expression. On baseline trials, two faces were displayed with a neutral expression (Figure 1). Following the task participants self-reported hypomania proneness using the well-validated Hypomanic Personality Scale (HPS-48). Further details on these measures, procedures, and task parameters are included in supplementary materials.
Figure 1.
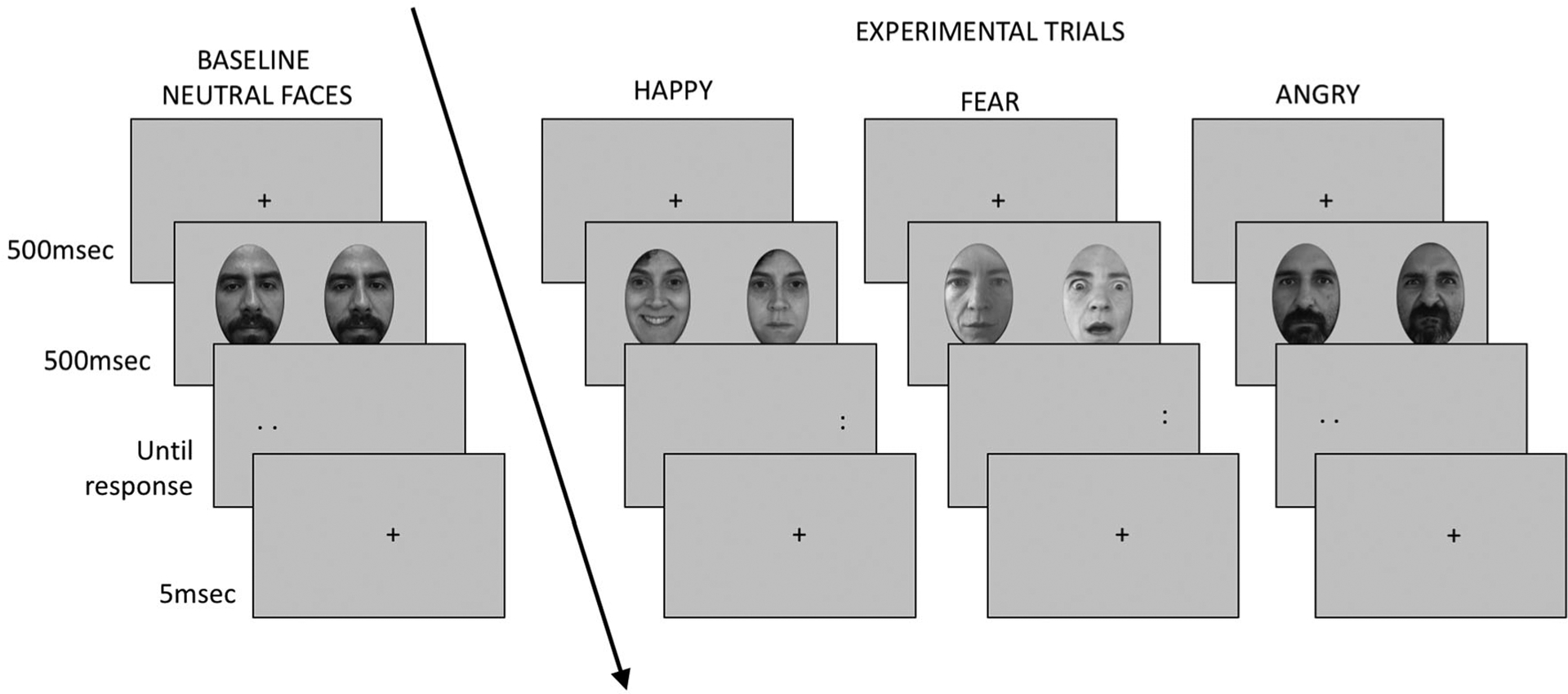
Example of Dot-Probe Task Trials.
Results
Preliminary analyses
Participants were accurate at discriminating the probes (M = 95.78, SE = 0.33). Mean correct reaction times (RTs) were calculated for each individual for each condition, after excluding RTs more or less than 3 SDs. These were converted to attentional bias scores, calculated by subtracting the mean RT for congruent trials from the mean RT for incongruent trials (Fox et al., 2009) whereby a positive attention bias score value is interpreted to reflect vigilance for the emotional face, whereas a negative value indicates avoidance of the emotional face.1 Prior to the main analyses, ten outlying values were identified; three on the DASS-21 depression scale, one on the DASS-21 Anxiety Scale, three on the PANAS Negative scale, and one each for Happy, Fear and Angry bias scores. These were winsorized by assigning values 1% higher or lower than the next non-outlying value.
Main analyses
To address our first hypothesis (positive amplification), we first examined the bivariate relationship between HPS-48 scores and happy bias scores. As predicted, we observed a significant, though modest, positive correlation2 between HPS-48 scores and happy bias scores (r = .29, p = .02; see Figure 2). To confirm that this effect was not simply a product of positive affect or of other factors relating to hypomania proneness, we ran a stepwise regression entering HPS-48, PANAS-PA, PANAS-NA, and DASS-21 Depression, Anxiety and Stress scores as independent variables. The resulting model included PANAS-PA as a predictor at step one and PANAS-PA and HPS-48 as predictors at step two (see Table 1). While there was a significant, positive effect of PANAS-PA on happy bias scores, the unique effect of HPS-48 scores on happy bias scores remained significant.
Figure 2.
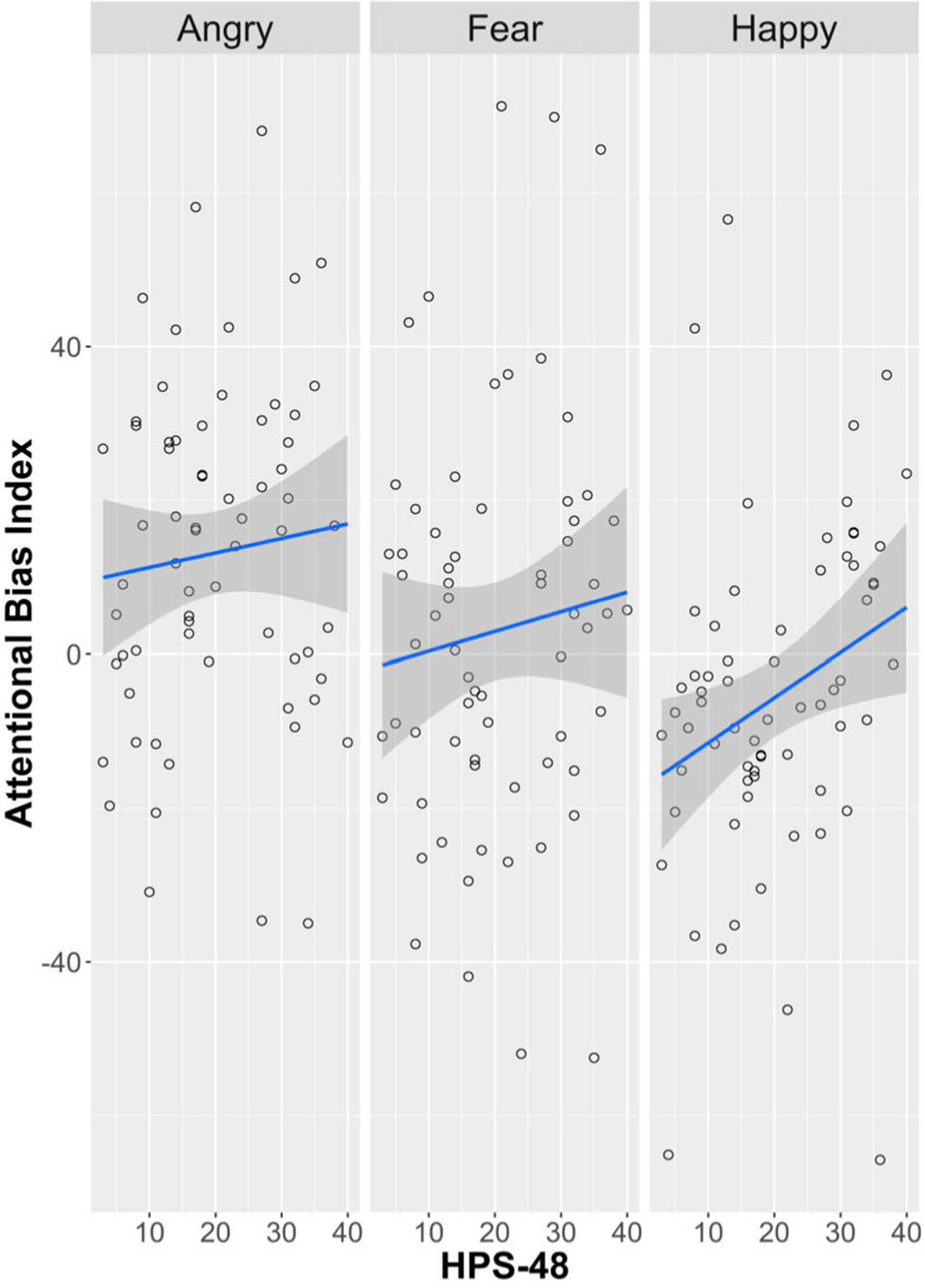
Scatterplot of hypomania (HPS-48) risk and angry, fear, and happy attention bias scores.
Table 1.
Regression analysis predicting happy bias scores.
| b | SE b | β | t | p | LLCI | ULCI | |
|---|---|---|---|---|---|---|---|
| HAPPY BIAS SCORE* | |||||||
| Step 1 | |||||||
| Constant | −29.94 | 9.27 | |||||
| PANAS-PA | 8.60 | 3.16 | 0.32 | 2.72 | .008 | 2.29 | 14.92 |
| Step 2 | |||||||
| Constant | −37.80 | 9.73 | |||||
| PANAS-PA | 7.76 | 3.10 | 0.29 | 2.51 | .015 | 1.57 | 13.96 |
| HPS-48 | 0.51 | 0.24 | 0.25 | 2.16 | .035 | 0.04 | 0.99 |
| β | t | p | Partial r | |
|---|---|---|---|---|
| HAPPY BIAS SCORE (Variables excluded from stepwise regression model above) | ||||
| Step 1 | ||||
| HPS-48 | 0.25 | 2.16 | .035 | 0.26 |
| DASS21 Depression | 0.13 | 1.08 | .284 | 0.13 |
| DASS21 Anxiety | 0.09 | 0.74 | .464 | 0.09 |
| DASS21 Stress | 0.10 | 0.88 | .384 | 0.11 |
| PANAS-NA | 0.08 | 0.70 | .483 | 0.09 |
| Step 2 | ||||
| DASS21 Depression | 0.08 | 0.63 | .532 | 0.08 |
| DASS21 Anxiety | 0.00 | 0.01 | .989 | 0.00 |
| DASS21 Stress | 0.01 | 0.05 | .960 | 0.01 |
| PANAS-NA | 0.01 | 0.07 | .942 | 0.01 |
Note: Model resulted from HPS-48, PANAS-PA, PANAS-NA, and DASS-21 scores as independent variables in a stepwise regression.
To address our second hypothesis (negative attenuation), we then examined the bivariate relationships between HPS-48 scores and anger and fear bias scores (see Figure 2). We found no evidence that HPS-48 scores were associated with reduced bias towards angry (r = 0.09, p = 0.466) or fearful faces (r = 0.10, p = .404).3 In sum, HPS-48 scores appeared to be associated with attentional bias toward happy, but not angry or fearful, faces.
Discussion
Hypomanic proneness, and a clinical history of hypomania or mania as a core component of bipolar disorder, has been associated with heightened and problematic positive affect, yet the extent to which these processes may be associated with attention-related biases for positive or negative emotional stimuli remains less clear, especially among college-aged young adults at putative vulnerability for future onset of hypomania or mania (e.g. Gruber, 2011; Gruber et al., 2008). Two perspectives were tested, examining whether hypomania proneness was associated with attentional bias towards positive stimuli, or attentional bias away from negative stimuli. Support for the positive amplification perspective was found, whereby self-reported hypomania proneness was associated with increased attentional biases for happy faces, but not angry or fearful faces. Results, which were not accounted for by other affective or mood factors, provide insight into potential attention markers that correlate with heightened risk for hypomania or mania.
The current study is one of the first to examine increased automatic attention for positive emotional stimuli using a spectrum approach among emerging adults at potential risk for hypomania, which may co-occur with heightened positive affectivity observed among emerging adults at increased propensity for, or with a clinical history of, hypomania or mania (Gruber, 2011). Results also provide some of the first support for a better understanding of processes that may be associated with a positive amplification perspective on positive emotion persistence in mania, as evidenced by heightened attentional biases to positive emotion stimuli. These findings are consistent with, and extend previous work by Putman et al. (2007), who concluded from a small sample of 16 high trait-hypomanic individuals compared to 12 controls that high trait hypomania proneness was associated with a significant cueing effect for happy, but not fearful, faces. Our study importantly differed from Putman and colleagues’ early findings by recruiting a larger sample size, adopting a spectrum versus categorical approach to hypomania proneness, and utilising a clinically distinct measure that focuses on psychologically-relevant (cognitive, affective, and behavioural) processes as opposed to mood disorder symptoms (i.e. General Behavioural Inventory), and examining a broader range of emotional faces (i.e. including sad faces). Furthermore, although we found evidence that positive affect was also associated with greater bias toward happy faces, our results were robust when accounting for this effect. Further, we measured, but found no evidence that our results were driven by, several additional and theoretically important confounds including negative affect, or depression, anxiety, and stress symptom measures.
We also note that these results diverge from studies that have not reported group differences in visual attentional biases to emotional stimuli among euthymic adults with a clinical history of mania (i.e. bipolar disorder; e.g. García-Blanco et al., 2014; 2017; Leyman et al., 2009; Purcell et al., 2018). Our participants likely differ in several important dimensions from the clinically recruited BD populations in these studies that may explain observed differences, including age, medication status, prior depression history and common comorbid disorders, as well as the effects of sustained illness duration. Findings from the present study diverge from Rock et al. (2010) who found no group differences in attention bias to positive stimuli for undergraduate students at high versus low risk for bipolar spectrum disorders; however, we note that this study differed from the present investigation by using of emotional words in the dot probe task and a different measure of hypomania proneness. Future work is warranted in larger samples ideally adopting longitudinal study designs that sample adults at high clinical risk and track those who versus do not go on to develop bipolar disorder to examine developmental differences in the emergence and absence of attention related biases.
Although an important first step, we acknowledge several study limitations. First, scores on our measure of hypomania proneness were generally quite low as would be expected in an analogue student sample (i.e. approximately 9 participants [13%] scored above stringent high-risk clinical cutoffs of ≥33). We note that this limits the generalizability of these findings to clinical samples. Indeed, we did not conduct formal clinical interviews to ascertain whether participants had a history of manic episodes as such, future studies should replicate these findings in adults diagnosed with a clinical history of mania and extend it to other emerging adult populations including youth with a parent diagnosed with bipolar disorder. At the same time, this study design enabled us to utilise an individual differences approach allowing for examination of hypomania on a broader spectrum, mirroring its presentation in the wider population consistent with recent initiatives to examine clinical phenomena dimensionally. Second, participants were predominately female and thus it is unclear whether potential gender differences in attentional biases may have driven the obtained results. Third, although the validity of the Radboud Faces Database has been extensively examined, still face images may lack ecological validity as compared to an authentic and dynamic interpersonal interaction. Fourth, the ability of attentional bias tasks, such as the dot-probe, to reliably and stably measure attentional biases in individuals is a current topic of interest (see Supplementary Materials). Fourth, although our results present a modest correlation of potential small effect that is consistent with individual differences research in this domain, it is important for understanding attention biases as one piece of a larger puzzle towards better understanding proneness towards, and risk for, developing hypomania and mania.
Taken together, these findings provide initial support that attentional biases co-occur with self-reported mania proneness, consistent with the possibility that such individuals have a visual bias toward positive faces. Future work to expand upon this initial pilot investigation are warranted to continue to unpack the nature of cognitive processes on normative and clinically relevant indices of positive emotionality, specifically to aid in identifying the interplay, or potential causal relationship, between positive emotion and attention.
Supplementary Material
Funding
This work was supported by the Australian Research Council (ARC) Centre of Excellence for Cognition and its Disorders (CE110001021) http://www.ccd.edu.au (RP), ARC Discovery Project grant (DP110100850) (RP), a NARSAD Young Investigator Grant from the Brain & Behavior Research Foundation (JG), a CTSA Grant Number UL1 RR024139 from the National Center for Research Resources (NCRR) and the National Center for Advancing Translational Science (NCATS) (JG), NIMH T32MH103213 & F31MH122122 (JP), and Indiana CTSI Predoctoral Award Grant UL1TR001108 & TL1TR002531 (JP). Its contents are solely the responsibility of the authors and do not necessarily represent the official view of NIH. PSG is supported by a CNPq researcher fellowship (309905/2019-2) and CAPES - PRINT (Pro-grama Institucional de Internacionalização; Grant 88887.310255/2018-00).
Footnotes
Supplemental data for this article can be accessed at https://doi.org/10.1080/02699931.2020.1810638
Single t tests against zero revealed significant overall attentional biases for happy (t = −2.13, p = 0.037) and angry (t = 4.90, p < .001) but not for fearful faces (t = 0.92, p = 0.361).
Importantly, this pattern was also present when comparing happy bias scores between groups of participants scoring at, or within, the first (scores ≤ 11) and fourth quartiles (scores ≥ 30.25) on the HPS-48, t(31) = −2.15, p = 0.040.
There remained no evidence of a difference when comparing anger and fear bias scores between groups of participants scoring at or within the first (scores ≤ 11) and fourth quartiles (scores ≥ 30.25) on the HPS-48 for both anger: t(31) = −0.91, p = .368, and fear: t(31) = −0.48, p = .631.
Disclosure statement
No potential conflict of interest was reported by the author(s).
References
- Brotman MA, Skup M, Rich BA, Blair KS, Pine DS, Blair JR, & Leibenluft E (2008). Risk for bipolar disorder is associated with face-processing deficits across emotions. Journal of the American Academy of Child & Adolescent Psychiatry, 47(12), 1455–1461. doi: 10.1097/CHI.0b013e318188832e [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fox E, Ridgewell A, & Ashwin C (2009). Looking on the bright side: Biased attention and the human serotonin transporter gene. Proceedings of the Royal Society B: Biological Sciences, 276(1663), 1747–1751. doi: 10.1098/rspb.2008.1788 [DOI] [PMC free article] [PubMed] [Google Scholar]
- García-Blanco A, Salmerón L, & Perea M (2017). Inhibitory control for emotional and neutral scenes in competition: An eye-tracking study in bipolar disorder. Biological Psychology, 127, 82–88. doi: 10.1016/j.biopsycho.2017.05.006 [DOI] [PubMed] [Google Scholar]
- García-Blanco A, Salmerón L, Perea M, & Livianos L (2014). Attentional biases toward emotional images in the different episodes of bipolar disorder: An eye-tracking study. Psychiatry Research, 215(3), 628–633. doi: 10.1016/j.psychres.2013.12.039 [DOI] [PubMed] [Google Scholar]
- Gruber J (2011). Can feeling too good be bad? Positive emotion persistence (PEP) in bipolar disorder. Current Directions in Psychological Science, 20(4), 217–221. doi: 10.1177/0963721411414632 [DOI] [Google Scholar]
- Gruber J, & Johnson SL (2009). Positive emotional traits and ambitious goals among people at risk for mania: The need for specificity. International Journal of Cognitive Therapy, 2(2), 176–187. doi: 10.1521/ijct.2009.2.2.176 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gruber J, Johnson SL, Oveis C, & Keltner D (2008). Risk for mania and positive emotional responding: Too much of a good thing? Emotion, 8(1), 23–33. doi: 10.1037/1528-3542.8.1.23 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gruber J, Purcell AL, Perna MJ, & Mikels JA (2013). Letting go of the bad: Deficit in maintaining negative, but not positive, emotion in bipolar disorder. Emotion, 13(1), 168–175. doi: 10.1037/a0029381 [DOI] [PubMed] [Google Scholar]
- Isaacowitz DM (2005). The gaze of the optimist. Personality and Social Psychology Bulletin, 31(3), 407–415. doi: 10.1177/0146167204271599 [DOI] [PubMed] [Google Scholar]
- Jabben N, Arts B, Jongen EMM, Smulders FTY, van Os J, & Krabbendam L (2012). Cognitive processes and attitudes in bipolar disorder: A study into personality, dysfunctional attitudes and attention bias in patients with bipolar disorder and their relatives. Journal of Affective Disorders, 143(1), 265–268. doi: 10.1016/j.jad.2012.04.022 [DOI] [PubMed] [Google Scholar]
- Johnson SL, Gruber J, & Eisner L (2007). Emotion in bipolar disorder. In Rottenberg J & Johnson SL (Eds.), Emotion and psychopathology: Bridging affective and clinical science (pp. 168–200). American Psychological Association. 10.1037/11562-000 [DOI] [Google Scholar]
- Jongen EM, Smulders FT, Ranson SM, Arts BM, & Krabbendam L (2007). Attentional bias and general orienting processes in bipolar disorder. Journal of Behavior Therapy and Experimental Psychiatry, 38(2), 168–183. doi: 10.1016/j.jbtep.2006.10.007 [DOI] [PubMed] [Google Scholar]
- Lembke A, & Ketter TA (2002). Impaired recognition of facial emotion in mania. American Journal of Psychiatry, 159(2), 302–304. doi: 10.1176/appi.ajp.159.2.302 [DOI] [PubMed] [Google Scholar]
- Leyman L, De Raedt R, & Koster E (2009). Attentional biases for emotional facial stimuli in currently depressed patients with bipolar disorders. International Journal of Clinical and Health Psychology, 9(3), 393–410. [Google Scholar]
- M’Bailara K, Demotes-Mainard J, Swendsen J, Mathieu F, Leboyer M, & Henry C (2009). Emotional hyper-reactivity in normothymic bipolar patients. Bipolar Disorders, 11(1), 63–69. doi: 10.1111/j.1399-5618.2008.00656.x [DOI] [PubMed] [Google Scholar]
- Miskowiak KW, Seeberg I, Kjaerstad HL, Burdick KE, Martinez-Aran A, Bonnin CM, Bowie CR, Carvalho AF, Gallagher P, Hasler G, Lafer B, López-Jaramillo C, Sumiyoshi T, McIntyre RS, Schaffer A, Porter RJ, Purdon S, Torres IJ, Yatham,… Lafer B (2019). Affective cognition in bipolar disorder: A systematic review by the ISBD targeting cognition task force. Bipolar Disorders, doi: 10.1111/bdi.12834 [DOI] [PubMed] [Google Scholar]
- Peckham AD, Johnson SL & Gotlib IH (2015). Attentional bias in euthymic bipolar I disorder. Cognition and Emotion, Advance online publication. 10.1080/02699931.2015.1014313 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Purcell JR, Lohani M, Musket C, Isaacowitz D, & Gruber J (2018). Lack of emotional gaze preferences using eye-tracking in bipolar disorder. International Journal of Bipolar Disorders, 6 (1), 15. doi: 10.1186/s40345-018-0123-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Putman P, Saevarsson S, & van Honk J (2007). Hypomanic trait is associated with a hypovigilant automatic attentional response to social cues of danger. Bipolar Disorders, 9(7), 779–783. doi: 10.1111/j.1399-5618.2007.00425.x [DOI] [PubMed] [Google Scholar]
- Raila H, Scholl BJ, & Gruber J (2015). Seeing the world through rose-colored glasses: People who are happy and satisfied with life preferentially attend to positive stimuli. Emotion, 15(4), 449–462. doi: 10.1037/emo0000049 [DOI] [PubMed] [Google Scholar]
- Rock PL, Goodwin GM, & Harmer CJ (2010). The common adolescent bipolar phenotype shows positive biases in emotional processing. Bipolar Disorders, 12(6), 606–615. doi: 10.1111/j.1399-5618.2010.00859.x [DOI] [PubMed] [Google Scholar]
- Wadlinger HA, & Isaacowitz DM (2008). Looking happy: The experimental manipulation of a positive visual attention bias. Emotion, 8(1), 121–126. doi: 10.1037/1528-3542.8.1.121 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wirth BE, & Wentura D (2020). It occurs after all: Attentional bias towards happy faces in the dot-probe task. Attention, Perception, & Psychophysics, 1–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


