In a study published in The Lancet Respiratory Medicine, Andrew Letizia and colleagues1 analysed the subsequent infection risk for SARS-CoV-2 in healthy young adults with and without previous antispike IgG antibodies. They followed Marine recruits for 6 weeks after a 2-week supervised quarantine period. Serology and PCR tests for SARS-CoV-2 were performed upon arrival to supervised quarantine, and PCR was repeated on weeks 1 and 2 of quarantine, and then every other week (weeks 2, 4, and 6) thereafter.
A positive PCR test after quarantine in this setting most likely represents a new viral infection. However, a positive PCR test from nasopharyngeal swabs merely reflects the detection of RNA fragments that might be related to a new viral infection, viral persistence with reappearance of virus in mucosae, or non-viable viral debris. Recurrent infections have already been reported for patients with previous infections of a different coronavirus2 and have been convincingly demonstrated for SARS-CoV-2.3 In addition, new positive PCR tests might reflect persistence of viral replication from reservoir tissues, as has been described for coronaviruses and other RNA viruses such as Zika or Ebola.4 Waning immunity can be the reason for reinfection, viral persistence, or reactivation but seems unlikely in the context of young healthy individuals.
In the absence of viral sequencing with phylogenetic analyses, viral cultures, or information regarding different SARS-CoV-2 variants, a positive PCR test cannot be assumed to represent new viral infections in all settings. Strict scientific criteria for the definition of reinfection might have contributed to an underestimation of the real rate of reinfection. A pragmatic approach for a clinical classification of subsequent PCR-positive cases as reinfection, relapse, or PCR re-positivity has been proposed.5
This study1 was conducted in a closed setting but provides some interesting insights regarding the risk of subsequent SARS-CoV-2 infection in the general population or other settings. First, the rate of new SARS-CoV-2 PCR positive results is about 80% lower among seropositive individuals (incidence rate ratio 0·18 [95% CI 0·11–0·28]; p<0·001). These data confirm that seropositive individuals have an important, albeit limited, protection for new infections. The degree of protection is somewhat lower than that described for health-care workers (adjusted incidence rate ratio [RR] 0·11 [0·03–0·44])6 but similar to that of the general population (adjusted RR 0·195 [0·155–0·246]).7 The degree of protection reduces with advancing age.7 The high risk of recurrence among recruits might be related to close contact in platoons or rooms, or to the programmed screening in asymptomatic individuals.8 Second, the rate of new SARS-CoV-2 PCR detection among seropositive Marines cases is not negligible (1·1 cases per person-year), even in this young and healthy population. Overall, these results indicate that COVID-19 does not provide an almost universal and long-lasting protective immunity, unlike that seen in measles, for example.
Letizia and colleagues1 show that recurrent SARS-CoV-2 infection is inversely related to the titre of antispike IgG antibodies. In addition, neutralising antibodies were lower among subsequently PCR-positive participants than in negative participants. It has been shown that the severity of the clinical presentation is associated with a higher titre of neutralising antibodies. As the authors acknowledge, they do not provide information regarding SARS-CoV-2 infection before the supervised quarantine.1 Given the heterogeneity of the immunological response after SARS-CoV-2 infection, seropositivity cannot guarantee effective SARS-CoV-2 neutralisation activity or protection against subsequent infection. The level of antibody titre needed to confer protection is at present unknown. Moreover, immunity induced against previous SARS-CoV-2 infection might confer a limited protection against new variants of concern.
Of note, most cases with a new or subsequent SARS-CoV-2 positive test were asymptomatic or oligosymptomatic and thus were detected by repeated PCR tests rather than because of new symptoms.1 Since there is a high percentage of asymptomatic infection among young adults, they might be an important source of transmission in the community. Reports suggest that vaccine-induced immune response might be higher than that elicited by SARS-CoV-2 infection,9, 10 suggesting that vaccination might be more effective in preventing new infections.
Efforts must be made to reduce the risk of SARS-CoV-2 transmission from young oligosymptomatic individuals. Results from Letizia and colleagues1 suggest that even young individuals with a previous SARS-CoV-2 infection should be vaccinated to target a recognised source of transmission. However, the most adequate vaccination schedule following SARS-CoV-2 infection remains unknown. Reports have described robust responses to a single dose of an mRNA vaccine among patients with previous SARS-CoV-2 infection that exceeds that of the full 2-dose vaccination among SARS-CoV-2-naive individuals.9, 10 In times of worldwide vaccine shortage, a single-dose vaccination among SARS-CoV-2 seropositive individuals is worth considering.
In summary, well conducted studies from closed settings, such as the study from Letizia and colleagues, offer useful information for the general population. Despite a wealth of information regarding SARS-CoV-2 infection, important questions remain unanswered: the frequency and clinical relevance of reinfection and its associated risk of transmission, the impact of reinfection on the immune response, and the most adequate vaccination options that might help to control the COVID-19 pandemic.
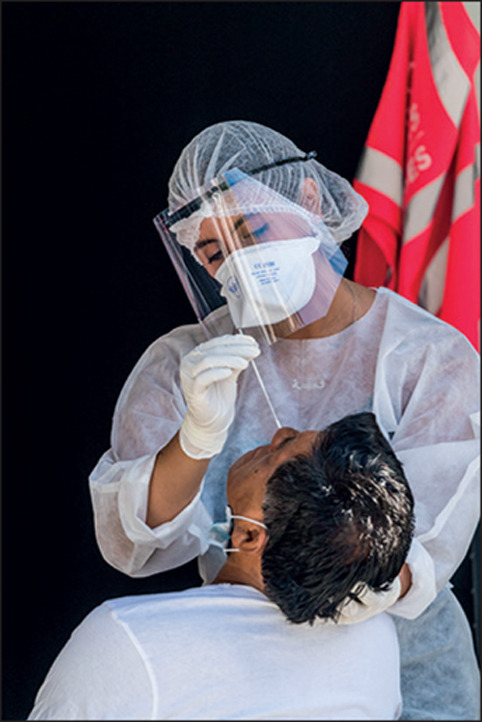
© 2021 Voisin/Phanie/Science Photo Library
We declare no competing interests.
References
- 1.Letizia AG, Ge Y, Vangeti S, et al. SARS-CoV-2 seropositivity and subsequent infection risk in healthy young adults: a prospective cohort study. Lancet Respir Med. 2021 doi: 10.1016/S2213-2600(21)00158-2. published online April 15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Edridge AWD, Kaczorowska J, Hoste ACR, et al. Seasonal coronavirus protective immunity is short-lasting. Nat Med. 2020;26:1691–1693. doi: 10.1038/s41591-020-1083-1. [DOI] [PubMed] [Google Scholar]
- 3.Tillett RL, Sevinsky JR, Hartley PD, et al. Genomic evidence for reinfection with SARS-CoV-2: a case study. Lancet Infect Dis. 2021;21:52–58. doi: 10.1016/S1473-3099(20)30764-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kalkeri R, Goebel S, Sharma GD. SARS-CoV-2 Shedding from asymptomatic patients: contribution of potential extrapulmonary tissue reservoirs. Am J Trop Med Hyg. 2020;103:18–21. doi: 10.4269/ajtmh.20-0279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Yahav D, Yelin D, Eckerle I, et al. Definitions for coronavirus disease 2019 reinfection, relapse and PCR re-positivity. Clin Microbiol Infect. 2021;27:315–318. doi: 10.1016/j.cmi.2020.11.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lumley SF, O'Donnell D, Stoesser NE, et al. Antibody status and incidence of SARS-CoV-2 infection in health care workers. N Engl J Med. 2021;384:533–540. doi: 10.1056/NEJMoa2034545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hansen CH, Michlmayr D, Gubbels SM, Mølbak K, Ethelberg S. Assessment of protection against reinfection with SARS-CoV-2 among 4 million PCR-tested individuals in Denmark in 2020: a population-level observational study. Lancet. 2021;397:1204–1212. doi: 10.1016/S0140-6736(21)00575-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Letizia AG, Ramos I, Obla A, et al. SARS-CoV-2 Transmission among marine recruits during quarantine. N Engl J Med. 2020;383:2407–2416. doi: 10.1056/NEJMoa2029717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ebinger JE, Fert-Bober J, Printsev I, et al. Antibody responses to the BNT162b2 mRNA vaccine in individuals previously infected with SARS-CoV-2. Nat Med. 2021 doi: 10.1038/s41591-021-01325-6. published online April 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Velasco M, Galán MI, Casas ML, et al. Impact of previous COVID-19 on immune response after a single dose of BNT162b2 SARS-CoV-2 vaccine. medRxiv. 2021 doi: 10.1101/2021.03.08.21253065. published online March 14. (preprint). [DOI] [Google Scholar]


