Abstract
The spleen is the most commonly injured organ in blunt abdominal trauma. Patients who are hemodynamically unstable due to splenic trauma undergo definitive operative management. Interventional radiology plays an important role in the multidisciplinary management of the hemodynamically stable trauma patient with splenic injury. Hemodynamically stable patients selected for nonoperative management have improved clinical outcomes when splenic artery embolization is utilized. The purpose of this article is to review the indications, technical aspects, and clinical outcomes of splenic artery embolization for patients with high-grade splenic injuries.
Keywords: interventional radiology, trauma, hemorrhage, embolization, spleen
The spleen is the most commonly injured organ in blunt abdominal trauma. 1 As the largest secondary lymphoid organ, the spleen plays an important role in immunologic and hematologic functions. 2 Typically, traumatic splenic injuries are managed in two cohorts, nonoperative and operative management. Patients who are hemodynamically unstable due to splenic trauma should undergo definitive operative management. 1 3 For hemodynamically stable patients, the management of splenic trauma has evolved toward splenic preservation in order to retain its important physiologic functions and avoid complications from splenectomy. In fact, the majority of patients with splenic trauma are now managed nonoperatively. 4 To this end, splenic artery embolization (SAE) has emerged as a powerful adjunct to the nonoperative management of splenic injuries. SAE improves splenic preservation rates in trauma patients selected for nonoperative management. 5 6 7 8 9 10 11 SAE can be performed proximally or distally within the splenic artery. Both techniques demonstrate similar clinical efficacy; however, proximal SAE (pSAE) is associated with lower rates of minor complications. 12 13 14 In this article, we discuss the role of SAE in the nonoperative management of blunt splenic trauma. We review the indications, relevant anatomy, technical aspects of SAE, and clinical outcomes of SAE in the trauma patient.
Diagnosis
Patients with blunt splenic trauma can present with left upper quadrant (LUQ) pain, abdominal distension, and/or hypotension. 15 They may exhibit referred pain to the left shoulder due to irritation of the phrenic nerve that innervates the ipsilateral diaphragm (i.e., Kehr's sign). 16 Abdominal wall or left lower chest wall tenderness, contusion, or instability are typical physical findings associated with splenic trauma. 17 However, it should be remembered that some patients with traumatic splenic injuries have an unremarkable physical examination. Therefore, proper evaluation and monitoring of blunt trauma patients must be conducted to detect less obvious injuries.
Common imaging modalities utilized to evaluate splenic trauma include radiography, ultrasound, and computed tomography (CT). Rib fractures secondary to blunt abdominal trauma, especially ribs 9 to 11, are a common cause of splenic injury, as the spleen is encapsulated by these lower ribs ( Fig. 1 ). 18 Plain radiography is helpful in evaluating the character of these ribs in the setting of trauma and provides a rapid method of chest and upper abdominal evaluation. Radiography may show other features associated with splenic trauma such as a left pleural effusion and medial displacement of the gastric bubble. 19 Yet, plain radiography is neither specific nor sensitive for splenic injury. Therefore, the initial examination typically includes the focused assessment with sonography in trauma (FAST) exam. 20 The FAST exam identifies the presence of intraperitoneal fluid, a sign of more serious injury that may necessitate aggressive management strategies. Signs of splenic injury identified on FAST exam include a hypoechoic rim around the spleen, which may represent subcapsular fluid or intraperitoneal perisplenic fluid, or fluid in Morrison's pouch (i.e., hepatorenal space). 21 Based on the results of the FAST exam, patients undergo CT to further elucidate and characterize splenic injuries. For simplicity in the acute setting, CT is often performed using intravenous (IV) iodinated contrast in the portal venous phase, but recent data suggest that the sensitivity of the examination for splenic injury improves with the use of an additional arterial phase. 22 The American Academy of Surgery and Trauma (AAST) has developed criteria to grade splenic injury on CT, which can be utilized to guide management of splenic trauma patients. 23 24 Commonly, grade III or higher injuries are considered high grade. Splenic injury is categorized by the degree of capsular laceration, subcapsular hematoma, intraparenchymal hematoma, vascular injury, and/or devascularization ( Table 1 ).
Fig. 1.
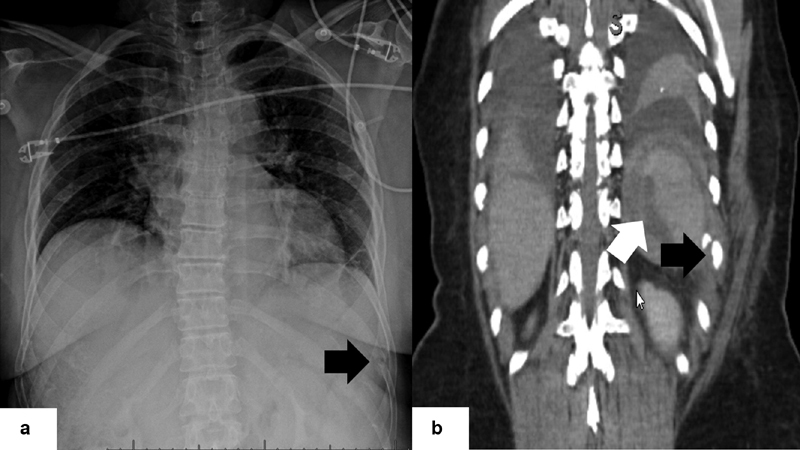
( a ) Chest radiograph obtained after a motor vehicle collision demonstrates a fracture of the left 10th rib (black arrow). ( b ) Coronal reformat image from a contrast-enhanced CT scan in the same patient demonstrates the fracture seen on radiography (black arrow) and hemoperitoneum from associated splenic trauma in the left upper quadrant (white arrow).
Table 1. The AAST Organ Injury Scale for the spleen.
| Grade | Injury type | Description of injury |
|---|---|---|
| I | Hematoma | Subcapsular, < 10% surface area |
| Laceration | Capsular tear, < 1 cm parenchymal depth | |
| II | Hematoma | Subcapsular, 10–50% surface area Intraparenchymal, < 5 cm in diameter |
| Laceration | 1–3 cm parenchymal depth, not involving a trabecular vessel | |
| III | Hematoma | Subcapsular, > 50% surface area or expanding Intraparenchymal, > 5 cm or expanding Ruptured subcapsular or parenchymal hematoma |
| Laceration | > 3 cm parenchymal depth or involving trabecular vessels | |
| IV | Laceration | Involving segmental or hilar vessels and producing > 25% devascularization |
| V | Laceration | Shattered spleen |
| Vascular | Hilar vascular injury that devascularizes spleen |
Abbreviation: AAST, American Association for the Surgery of Trauma.
Source: Adapted from Rowell et al. 24
Indications for Splenic Artery Embolization
Patients with hemodynamic instability due to splenic injury should be managed with splenectomy. 1 3 Apart from that, there is relative wide variability with regard to the management of hemodynamically stable patients with splenic injuries. Unfortunately, there is a lack of robust data in the literature to help guide patient selection in this clinical scenario. For example, case series, multivariate analyses, and one randomized trial have shown that SAE helps improve splenic preservation rates, although these prior reports have significant heterogeneity in patient selection from institution to institution. 5 6 7 8 9 10 11 Thus, patient selection for SAE in the trauma setting is largely institution dependent. When considering a patient for SAE, some important factors to consider include hemodynamic status, the grade of splenic injury, and any direct signs of vascular injury on CT, such as arteriovenous fistula (AVF), pseudoaneurysm (PSA), or contrast extravasation ( Figs. 2 and 3 ). Of course, the interventional radiologist should evaluate the patient for contraindications to SAE, such as uncorrectable coagulopathies. Our institutional approach to the management of patients with splenic trauma is summarized in Fig. 4 . In short, all hemodynamically stable patients with high-grade splenic injury (i.e., grade III or higher injury) are referred to interventional radiology for SAE. Additionally, patients with CT evidence of contrast extravasation are treated with embolization, irrespective of the grade of injury. Alternatively, the Western Trauma Association has also published an algorithmic approach to the management of blunt splenic trauma. 25 Briefly, this algorithm directs hemodynamically stable patients to a contrast-enhanced CT. Patients with grade I to III injuries without direct signs of vascular injury are observed. Patients with grade I to III injuries with direct signs of vascular injury and patients with grade IV to V injuries regardless of direct signs of vascular injury are referred for angiography. Nonetheless, establishing and adhering to a multidisciplinary protocol for patients with splenic trauma has been shown to improve patient outcomes. 26
Fig. 2.

Axial slice from a contrast-enhanced CT obtained after a motor vehicle collision demonstrates a splenic laceration with a pseudoaneurysm (white arrow).
Fig. 3.
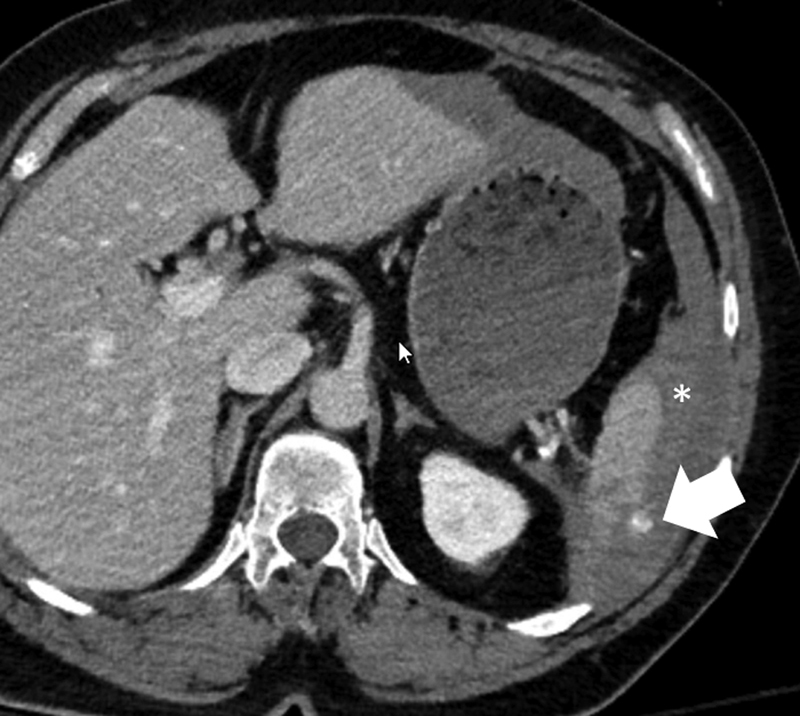
Axial slice from a contrast-enhanced CT obtained after a motor vehicle collision demonstrates a splenic laceration with contrast extravasation from the spleen (white arrow) and associated hemoperitoneum (asterisk).
Fig. 4.
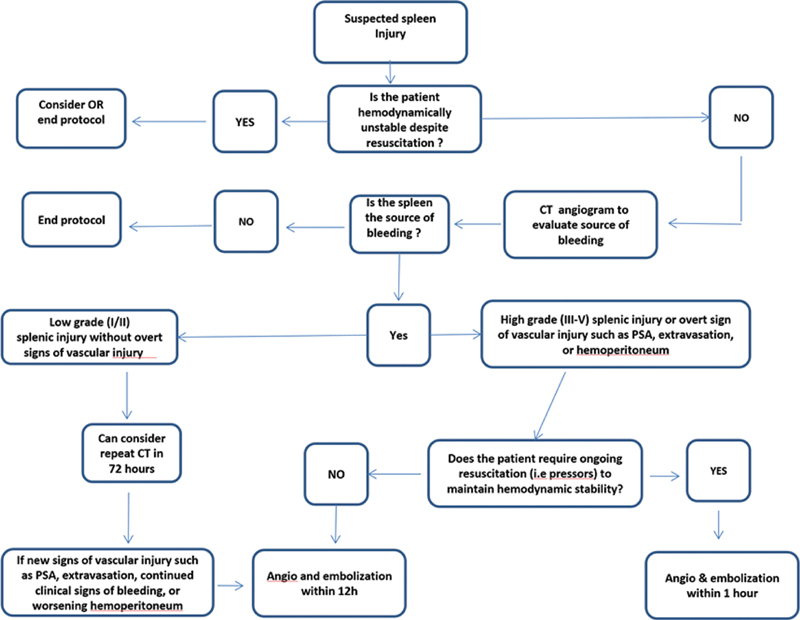
Institutional protocol for the management of patients with splenic trauma.
Anatomy
The splenic artery is the primary blood supply to the spleen, and the site of therapeutic embolization in SAE. Successful evaluation and treatment of blunt splenic trauma with SAE necessitates an understanding of the vascular anatomy ( Fig. 5 ). The most common origin of the splenic artery is the celiac trunk, which often arises from the abdominal aorta around the level of the 12th vertebra. 27 Less common origins include directly off the abdominal aorta (∼8%; Fig. 6 ) and off the superior mesenteric artery (<1%). 28 The dorsal pancreatic artery is the first large branch of the splenic artery, often arising within the first few centimeters from the splenic artery origin. Less common origins of the dorsal pancreatic artery include the celiac trunk, common hepatic artery, and superior mesenteric artery. 29 It is important to recognize the most distal origin of the greater pancreatic artery as its connection to the dorsal pancreatic artery via the transverse pancreatic artery is an important collateral pathway for SAE. Other important vascular supply to the spleen includes the short gastric arteries and gastroepiploic arteries ( Fig. 7 ). 30 31 The right gastroepiploic artery is the terminal branch of the gastroduodenal artery (GDA) and has an anastomosis with the left gastroepiploic artery, a distal branch of the splenic artery. 28 The short gastric arteries are a group of small arteries that connect the splenic artery with left gastric artery. 31
Fig. 5.
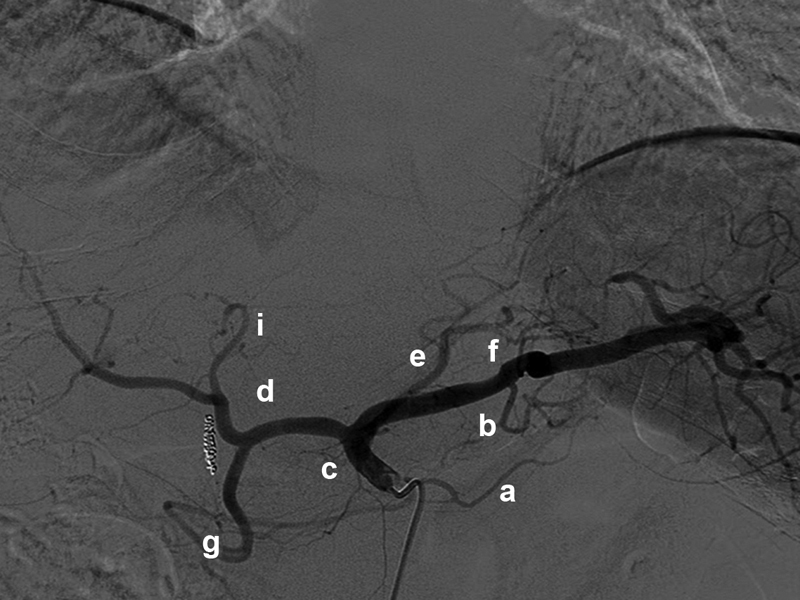
Digital subtraction angiography of the celiac trunk demonstrates classic arterial anatomy, including the dorsal pancreatic artery ( a ), the greater pancreatic artery ( b ), the celiac trunk ( c ), the common hepatic artery ( d ), the left gastric artery ( e ), the splenic artery ( f ), the gastroduodenal artery ( g ), the right hepatic artery ( h ), and the left hepatic artery ( i ). The midsplenic artery in between the dorsal pancreatic artery and the greater pancreatic artery is the ideal site for proximal splenic artery embolization.
Fig. 6.

Digital subtraction angiography obtained during splenic artery embolization for trauma shows the splenic artery arising directly from the abdominal aorta (white arrow), an anatomic variant. A splenic laceration with small pseudoaneurysms is seen in the upper pole of the spleen (black arrow).
Fig. 7.
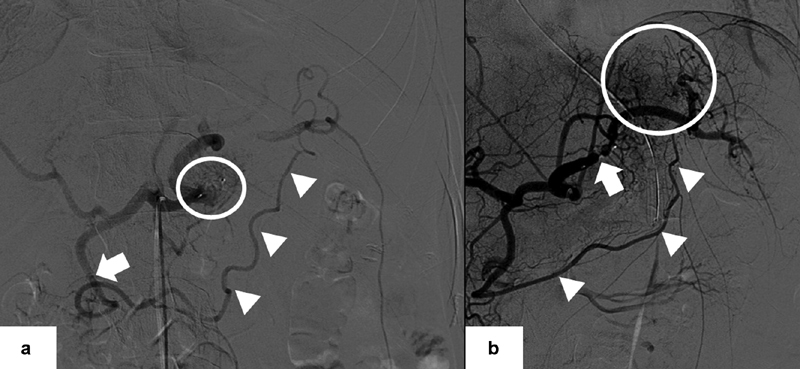
( a ) Digital subtraction angiography obtained during splenic artery embolization for trauma shows the gastroduodenal artery (white arrow) giving rise to the right gastroepiploic artery that anastomoses with the left gastroepiploic artery (white arrow heads) that provides collateral flow to the spleen after vascular plug deployment (white circle). ( b ) Digital subtraction angiography obtained during splenic artery embolization for trauma shows the short gastric arteries (white circle) and the right to left gastroepiploic artery pathway (white arrow heads) supplying the spleen after vascular plug deployment (white arrow).
Embolization Technique
At our institution, arterial access is obtained using a micropuncture set (Terumo, Tokyo, Japan) under sonographic guidance. The right common femoral artery is the most common site for vascular access, but patient conditions such as the presence of arterial lines or pelvic binders could necessitate the use of the left common femoral artery or a transradial approach, respectively. After placing a vascular sheath over a wire, a 5-Fr diagnostic catheter such as a Simmons 1 (Terumo), RC2 (Cook, Bloomington, IN), or Cobra 2 (Cook) is used to select the celiac trunk. Celiac angiography at a rate of 5 cc/second for a total of 25 cc is performed to evaluate the arterial anatomy and to identify direct signs of vascular injury such as contrast extravasation, PSA, or AVF.
At this point, the operator must decide whether to perform a pSAE or a distal SAE (dSAE). The decision to proceed with either pSAE or dSAE is largely operator dependent but can be influenced by two primary factors. First, prior studies have shown that both techniques result in similar rates of splenic salvage; however, pSAE is associated with a slightly lower rate of minor complications and shorter procedural times. 12 13 14 32 Second, some operators base their decision on the type of injury within the spleen. For example, patients with diffuse parenchymal injury may be treated with pSAE, while patients with focal areas of extravasation and/or a PSA might be treated with dSAE. 33 It should be noted that patients treated with both pSAE and dSAE have somewhat poorer outcomes compared to those treated with either pSAE or dSAE. 34 At our institution, all hemodynamically stable patients with grade III or higher splenic injuries, regardless of direct signs of vascular injury, are treated with pSAE. Some of the differences between pSAE and dSAE are summarized in Table 2 .
Table 2. Summary of the main differences between proximal splenic artery embolization and distal splenic artery embolization.
| Proximal | Distal | |
|---|---|---|
| When | Multifocal injury No angiographic abnormality but splenic injury of grade III–V on CT |
Focal vascular injury |
| Goal | Decrease splenic parenchymal perfusion pressure | Treat bleeding vessel |
| Advantages | Short procedure time Low radiation time |
Selective embolization |
| Disadvantages | Inability to easily perform future embolization | Long procedure time Infarction, abscess |
| Embolic material | Coils, plugs | Coils, particles, gelatin sponge slurry, N-butyl cyanoacrylate |
| Complications | Coil migration | Splenic infarct, abscess |
Abbreviation: CT, computed tomography.
In pSAE, vascular plugs or endovascular coils are placed in the midsplenic artery, distal to the origin of the dorsal pancreatic artery but proximal to the origin of the greater pancreatic artery ( Fig. 8 ). pSAE reduces the systolic arterial pressure experienced in the spleen, allowing it to heal, while a rich collateral supply from the dorsal pancreatic-transverse pancreatic-greater pancreatic artery pathway, the gastroepiploic arteries, and the short gastric arteries maintain adequate perfusion to the parenchyma. 32 33 Regarding the selection of an embolic agent for pSAE, both vascular plugs and endovascular coils have advantages and disadvantages. For instance, coils are familiar to most endovascular specialists, have a long history of efficacy, and can be deployed through a standard catheter or microcatheter. Yet, the use of coils within the high-flow splenic artery might lead to migration of the coil pack. On the other hand, the deployment of a single vascular plug is usually sufficient to provide hemostasis in the midsplenic artery but requires selective catheterization with a larger delivery system, which may be difficult or impossible in patients with atherosclerotic narrowing of the celiac artery or extreme tortuosity of the splenic artery. If appropriate stasis within the midsplenic artery is not achieved within a reasonable time, secondary embolic agents such as a gelatin sponge slurry can be administered. In theory, pSAE could complicate reintervention should the need arise, but this has not been a common occurrence in our institutional experience.
Fig. 8.

( a ) Digital subtraction angiography obtained during splenic artery embolization for trauma shows collateral flow to the spleen via the dorsal pancreatic-transverse pancreatic-greater pancreatic artery pathway (white arrow) after vascular plug deployment (black arrow). ( b ) Digital subtraction angiography obtained during splenic artery embolization for trauma shows collateral flow to the spleen via the dorsal pancreatic-transverse pancreatic-greater pancreatic artery pathway (white arrow) after endovascular coil deployment (black arrow).
For dSAE, general embolotherapy principles are applied. The site or sites of vascular injury are selectively catheterized using a combination of wires and catheters. Once the catheter (or microcatheter) is appropriately positioned, embolization is performed. dSAE can be accomplished using a variety of embolic agents including N-butyl cyanoacrylate, gelatin sponge slurry, particles, vascular plugs, or endovascular coils. The endpoint for dSAE is stasis within the target vessel.
Clinical Outcomes
Studies show high success rates for the nonoperative management of splenic trauma using SAE compared to nonoperative management without SAE. 5 6 7 8 9 10 11 A summary of meta-analyses and the single randomized trial are found in Table 3 . In a recently published prospective trial, 133 patients were randomized to either SAE or observation. 11 To be included, patients had to have a grade III injury and an injury severity score of ≥15 and/or large volume hemoperitoneum, grade IV injury, or a grade V injury with persistent vascularization of the spleen. Patients with a grade V injury without vascularization to the spleen or with direct signs of vascular injury were excluded. Investigators found that 32.3% of patients in the observation group eventually required either splenectomy or embolization. Additionally, patients in this cohort had a longer length of stay compared to those who underwent SAE. A multivariate analysis of more than 10,000 patients found that the overall failure rate of nonoperative management was 8.3%. 7 In this analysis, the failure of nonoperative management showed a statistically significant increase for patients with grade IV and V injuries when SAE was not used. In a retrospective multicenter study involving 1,275 patients, SAE was found to significantly increase the likelihood of splenic salvage. 5 Studies have also shown that the immunologic functions of the spleen are preserved after SAE. 35 36 37 Preserving the immunologic function of the spleen after SAE is of particular importance as postsplenectomy sepsis is a potentially fatal infection. 38 Pneumococcal, meningococcal, and Haemophilus influenzae type B (Hib) vaccinations are required after splenectomy, as these patients are particularly susceptible to encapsulated organisms due to diminished phagocytic function. 39 Splenectomy patients also typically receive prophylactic antibiotics to accommodate the immunologic deficiency. These prophylactic measures are not necessary after SAE, which further highlights the value in this nonoperative intervention. 40
Table 3. Summary of meta-analyses and a single randomized controlled trial evaluating outcomes of splenic artery embolization in blunt splenic trauma.
| Study | No. of patients | Study type | Outcomes |
|---|---|---|---|
| Banerjee et al 5 | 1,275 | Meta-analysis | Splenic artery embolization improves splenic salvage and results in fewer failures of nonoperative management |
| Requarth et al 7 | 10,157 | Meta-analysis | Splenic artery embolization increases splenic salvage in patients with grade IV and V injuries with fewer failures of nonoperative management |
| Arvieux et al 11 | 133 | Randomized controlled trial | 32.3% of patients randomized to observation eventually required splenectomy or embolization and splenic artery embolization decreased length of stay |
| Schnüriger et al 12 | 479 | Meta-analysis | No difference in splenic salvage, rebleeding, or major complications between distal and proximal embolization. Distal embolization had more minor complications |
| Rong et al 34 | 876 | Meta-analysis | Lowest complications with proximal embolization but highest with combined proximal and distal embolization |
Major complications of SAE include infection, infarction, device migration, or rebleeding that necessitate splenectomy. 41 Minor complications can include pleural effusions, fever, and device migrations that do not require splenectomy. 42 One multicenter analysis found the rates of major and minor complications to be 20 and 23%, respectively. 43 When considering complications, patient selection for SAE is paramount. As an example, retrospective analyses have found that as many as 40% of patients who experienced a major complication after SAE were likely inappropriately triaged to nonoperative management. 44 45 When comparing pSAE and dSAE, one meta-analysis including 476 patients found no statistical difference between the two techniques with regard to major complications, but dSAE had higher rates of minor complications, particularly splenic infarction. 12 A more recent meta-analysis including more than 800 patients demonstrated that major complications were higher in patients undergoing dSAE (28%) than pSAE (18%). 34
Conclusion
Interventional radiology plays an important role in the multidisciplinary management of the trauma patient with splenic injury. Hemodynamically stable patients who are selected for nonoperative management have improved clinical outcomes when SAE is utilized. Patient selection is influenced by institution-specific referral patterns; however, all hemodynamically stable patients with high-grade splenic injuries are referred to interventional radiology for SAE in our institution. Both pSAE and dSAE are associated with high rates of technical and clinical success, an acceptable safety profile, and preservation of the immunologic functions of the spleen.
Footnotes
Conflict of Interest A.J.G. is a speaker and consultant for Boston Scientific, a consultant for Varian, a speaker for Terumo, and receives research support from Penumbra. None of the other authors have conflicts of interest to disclose.
References
- 1.Powell M, Courcoulas A, Gardner M. Management of blunt splenic trauma: significant differences between adults and children. Surgery. 1997;122(04):654–660. doi: 10.1016/s0039-6060(97)90070-2. [DOI] [PubMed] [Google Scholar]
- 2.Mebius R E, Kraal G. Structure and function of the spleen. Nat Rev Immunol. 2005;5(08):606–616. doi: 10.1038/nri1669. [DOI] [PubMed] [Google Scholar]
- 3.Peitzman A B, Heil B, Rivera L.Blunt splenic injury in adults: multi-institutional study of the Eastern Association for the Surgery of Trauma J Trauma 20004902177–187., discussion 187–189 [DOI] [PubMed] [Google Scholar]
- 4.Stein D M, Scalea T M. Nonoperative management of spleen and liver injuries. J Intensive Care Med. 2006;21(05):296–304. doi: 10.1177/0885066606290854. [DOI] [PubMed] [Google Scholar]
- 5.Banerjee A, Duane T M, Wilson S P.Trauma center variation in splenic artery embolization and spleen salvage: a multicenter analysis J Trauma Acute Care Surg 2013750169–74., discussion 74–75 [DOI] [PubMed] [Google Scholar]
- 6.Haan J M, Bochicchio G V, Kramer N, Scalea T M. Nonoperative management of blunt splenic injury: a 5-year experience. J Trauma. 2005;58(03):492–498. doi: 10.1097/01.ta.0000154575.49388.74. [DOI] [PubMed] [Google Scholar]
- 7.Requarth J A, D'Agostino R B, Jr, Miller P R.Nonoperative management of adult blunt splenic injury with and without splenic artery embolotherapy: a meta-analysis J Trauma 20117104898–903., discussion 903 [DOI] [PubMed] [Google Scholar]
- 8.Ahuja C, Farsad K, Chadha M. An overview of splenic embolization. AJR Am J Roentgenol. 2015;205(04):720–725. doi: 10.2214/AJR.15.14637. [DOI] [PubMed] [Google Scholar]
- 9.Bessoud B, Denys A, Calmes J M. Nonoperative management of traumatic splenic injuries: is there a role for proximal splenic artery embolization? AJR Am J Roentgenol. 2006;186(03):779–785. doi: 10.2214/AJR.04.1800. [DOI] [PubMed] [Google Scholar]
- 10.Rajani R R, Claridge J A, Yowler C J.Improved outcome of adult blunt splenic injury: a cohort analysis Surgery 200614004625–631., discussion 631–632 [DOI] [PubMed] [Google Scholar]
- 11.Arvieux C, Frandon J, Tidadini F. Splenic arterial embolization to avoid splenectomy (SPLASH) study group - effect of prophylactic embolization on patient with blunt trauma at high risk of splenectomy: a randomized clinical trial. JAMA Surg. 2020;155(12):1102–1111. doi: 10.1001/jamasurg.2020.3672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Schnüriger B, Inaba K, Konstantinidis A, Lustenberger T, Chan L S, Demetriades D. Outcomes of proximal versus distal splenic artery embolization after trauma: a systematic review and meta-analysis. J Trauma. 2011;70(01):252–260. doi: 10.1097/TA.0b013e3181f2a92e. [DOI] [PubMed] [Google Scholar]
- 13.Bessoud B, Duchosal M A, Siegrist C A. Proximal splenic artery embolization for blunt splenic injury: clinical, immunologic, and ultrasound-Doppler follow-up. J Trauma. 2007;62(06):1481–1486. doi: 10.1097/TA.0b013e318047dfb8. [DOI] [PubMed] [Google Scholar]
- 14.Killeen K L, Shanmuganathan K, Boyd-Kranis R, Scalea T M, Mirvis S E. CT findings after embolization for blunt splenic trauma. J Vasc Interv Radiol. 2001;12(02):209–214. doi: 10.1016/s1051-0443(07)61827-2. [DOI] [PubMed] [Google Scholar]
- 15.Jabbour G, Al-Hassani A, El-Menyar A. Clinical and radiological presentations and management of blunt splenic trauma: a single tertiary hospital experience. Med Sci Monit. 2017;23:3383–3392. doi: 10.12659/MSM.902438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Khan S A, Muhammad I, Laabei F, Rothwell J. An unusual presentation of non pathological delayed splenic rupture: a case report. Cases J. 2009;2:6450. doi: 10.4076/1757-1626-2-6450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Chadburn A. The spleen: anatomy and anatomical function. Semin Hematol. 2000;37(01) 01:13–21. doi: 10.1016/s0037-1963(00)90113-6. [DOI] [PubMed] [Google Scholar]
- 18.Rostas J W, Lively T B, Brevard S B, Simmons J D, Frotan M A, Gonzalez R P. Rib fractures and their association with solid organ injury: higher rib fractures have greater significance for solid organ injury screening. Am J Surg. 2017;213(04):791–797. doi: 10.1016/j.amjsurg.2016.08.002. [DOI] [PubMed] [Google Scholar]
- 19.Makoba I G. Splenic injury following trauma: the role of ultrasonography. Afr Health Sci. 2001;1(01):23–25. [PMC free article] [PubMed] [Google Scholar]
- 20.Savatmongkorngul S, Wongwaisayawan S, Kaewlai R. Focused assessment with sonography for trauma: current perspectives. Open Access Emerg Med. 2017;9:57–62. doi: 10.2147/OAEM.S120145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Doody O, Lyburn D, Geoghegan T, Govender P, Munk P L, Torreggiani W C. Blunt trauma to the spleen: ultrasonographic findings. Clin Radiol. 2005;60(09):968–976. doi: 10.1016/j.crad.2005.05.005. [DOI] [PubMed] [Google Scholar]
- 22.Uyeda J W, LeBedis C A, Penn D R, Soto J A, Anderson S W. Active hemorrhage and vascular injuries in splenic trauma: utility of the arterial phase in multidetector CT. Radiology. 2014;270(01):99–106. doi: 10.1148/radiol.13121242. [DOI] [PubMed] [Google Scholar]
- 23.Coccolini F, Montori G, Catena F. Splenic trauma: WSES classification and guidelines for adult and pediatric patients. World J Emerg Surg. 2017;12:40. doi: 10.1186/s13017-017-0151-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Moore E E, Cogbill T H, Jurkovich G J, Shackford S R, Malangoni M A, Champion H R. Organ injury scaling: spleen and liver (1994 revision) J Trauma. 1995;38(03):323–324. doi: 10.1097/00005373-199503000-00001. [DOI] [PubMed] [Google Scholar]
- 25.Rowell S E, Biffl W L, Brasel K. Western Trauma Association Critical Decisions in Trauma: management of adult blunt splenic trauma-2016 updates. J Trauma Acute Care Surg. 2017;82(04):787–793. doi: 10.1097/TA.0000000000001323. [DOI] [PubMed] [Google Scholar]
- 26.Miller P R, Chang M C, Hoth J J. Prospective trial of angiography and embolization for all grade III to V blunt splenic injuries: nonoperative management success rate is significantly improved. J Am Coll Surg. 2014;218(04):644–648. doi: 10.1016/j.jamcollsurg.2014.01.040. [DOI] [PubMed] [Google Scholar]
- 27.White R D, Weir-McCall J R, Sullivan C M. The celiac axis revisited: anatomic variants, pathologic features, and implications for modern endovascular management. Radiographics. 2015;35(03):879–898. doi: 10.1148/rg.2015140243. [DOI] [PubMed] [Google Scholar]
- 28.Pandey S K, Bhattacharya S, Mishra R N, Shukla V K. Anatomical variations of the splenic artery and its clinical implications. Clin Anat. 2004;17(06):497–502. doi: 10.1002/ca.10220. [DOI] [PubMed] [Google Scholar]
- 29.Bertelli E, Di Gregorio F, Mosca S, Bastianini A. The arterial blood supply of the pancreas: a review. V. The dorsal pancreatic artery. An anatomic review and a radiologic study. Surg Radiol Anat. 1998;20(06):445–452. doi: 10.1007/BF01653138. [DOI] [PubMed] [Google Scholar]
- 30.Gregorczyk M, Dabkowska A, Tarka S, Ciszek B. The anatomy of the fundic branches of the stomach: preliminary results. Folia Morphol (Warsz) 2008;67(02):120–125. [PubMed] [Google Scholar]
- 31.Jean-Philippe Adam, Alexandre Jacquin, Christophe Laurent. Laparoscopic spleen-preserving distal pancreatectomy: splenic vessel preservation compared with the Warshaw technique. JAMA Surg. 2013;148(03):246–252. doi: 10.1001/jamasurg.2013.768. [DOI] [PubMed] [Google Scholar]
- 32.Imbrogno B F, Ray C E. Splenic artery embolization in blunt trauma. Semin Intervent Radiol. 2012;29(02):147–149. doi: 10.1055/s-0032-1312577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Bessoud B, Denys A. Main splenic artery embolization using coils in blunt splenic injuries: effects on the intrasplenic blood pressure. Eur Radiol. 2004;14(09):1718–1719. doi: 10.1007/s00330-004-2234-3. [DOI] [PubMed] [Google Scholar]
- 34.Rong J J, Liu D, Liang M. The impacts of different embolization techniques on splenic artery embolization for blunt splenic injury: a systematic review and meta-analysis. Mil Med Res. 2017;4:17. doi: 10.1186/s40779-017-0125-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Malhotra A K, Carter R F, Lebman D A.Preservation of splenic immunocompetence after splenic artery angioembolization for blunt splenic injury J Trauma 201069051126–1130., discussion 1130–1131 [DOI] [PubMed] [Google Scholar]
- 36.Olthof D C, Lammers A J, van Leeuwen E M, Hoekstra J B, ten Berge I J, Goslings J C. Antibody response to a T-cell-independent antigen is preserved after splenic artery embolization for trauma. Clin Vaccine Immunol. 2014;21(11):1500–1504. doi: 10.1128/CVI.00536-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Pirasteh A, Snyder L L, Lin R. Temporal assessment of splenic function in patients who have undergone percutaneous image-guided splenic artery embolization in the setting of trauma. J Vasc Interv Radiol. 2012;23(01):80–82. doi: 10.1016/j.jvir.2011.09.009. [DOI] [PubMed] [Google Scholar]
- 38.Okabayashi T, Hanazaki K. Overwhelming postsplenectomy infection syndrome in adults - a clinically preventable disease. World J Gastroenterol. 2008;14(02):176–179. doi: 10.3748/wjg.14.176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Tahir F, Ahmed J, Malik F. Post-splenectomy sepsis: a review of the literature. Cureus. 2020;12(02):e6898. doi: 10.7759/cureus.6898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Olthof D C, van der Vlies C H, Goslings J C. Evidence-based management and controversies in blunt splenic trauma. Curr Trauma Rep. 2017;3(01):32–37. doi: 10.1007/s40719-017-0074-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Ekeh A P, Khalaf S, Ilyas S, Kauffman S, Walusimbi M, McCarthy M C.Complications arising from splenic artery embolization: a review of an 11-year experience Am J Surg 201320503250–254., discussion 254 [DOI] [PubMed] [Google Scholar]
- 42.Parihar M L, Kumar A, Gamanagatti S. Role of splenic artery embolization in management of traumatic splenic injuries: a prospective study. Indian J Surg. 2013;75(05):361–367. doi: 10.1007/s12262-012-0505-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Western Trauma Association Multi-Institutional Trials Committee . Haan J M, Biffl W, Knudson M M. Splenic embolization revisited: a multicenter review. J Trauma. 2004;56(03):542–547. doi: 10.1097/01.ta.0000114069.73054.45. [DOI] [PubMed] [Google Scholar]
- 44.Eastern Association for the Surgery of Trauma Multiinstitutional Trials Workgroup . Peitzman A B, Harbrecht B G, Rivera L, Heil B. Failure of observation of blunt splenic injury in adults: variability in practice and adverse consequences. J Am Coll Surg. 2005;201(02):179–187. doi: 10.1016/j.jamcollsurg.2005.03.037. [DOI] [PubMed] [Google Scholar]
- 45.McIntyre L K, Schiff M, Jurkovich G J.Failure of nonoperative management of splenic injuries: causes and consequences Arch Surg 200514006563–568., discussion 568–569 [DOI] [PubMed] [Google Scholar]


