Abstract
The pediatric population accounts for a small portion of those with severe disease related to COVID-19. There are few published reports of hypercoagulable states in children with COVID-19. We describe an 11-year-old male with nephrotic syndrome who required inpatient treatment for COVID-19 pneumonia eight weeks prior. He returned to the emergency department with vomiting, tachypnea and was found to have a pulmonary embolism. In this case report, we discuss the risk factors for, presentation and evaluation of hypercoagulable state and its relation to COVID-19 in a pediatric patient.
1. Background
In 2019, severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) spread globally from Wuhan, China and resulted in an acute respiratory illness pandemic. This virus was renamed COVID-19 by The World Health Organization (WHO). The clinical course of COVID-19 is often accompanied by a hyperinflammatory response and systemic coagulation derangement [1], with elevated inflammatory markers including a markedly elevated D-dimer level [2].
Pulmonary embolism (PE) is rare in children, with a reported incidence of 8.6–57 in 100,000 in hospitalized children and 0.14–0.9 in 100,000 when studying the general population of non-hospitalized children [4]. Patients with a severe presentation of COVID-19 infection, in addition to those with COVID-19 and underlying risk factors for thromboembolism, may benefit from prophylactic anticoagulation. We aim to discuss the risk factors, presentation and evaluation of pulmonary embolism and to support the importance for pharmacologic prophylaxis.
2. Case
An 11-year-old male with obesity, recently diagnosed nephrotic syndrome (four months prior) and COVID-19 pneumonia (eight weeks prior) presented to the pediatric emergency department with a chief complaint of non-bloody, non-bilious vomiting for the past three days. Associated symptoms were shortness of breath, fatigue, weight gain, lower extremity swelling, and pain in the right buttocks. His only active home medication was prednisone 40 mg every other day.
Vital signs on arrival were notable for tachycardia to 173 beats per minute and tachypnea to 48 breaths per minute, blood pressure 100/50, oxygen saturation 95–96% on room air, although would decrease to 91–92% intermittently. His body mass index was 39. Physical exam was significant for ill appearance, tachycardia, tachypnea, and poor distal perfusion with cool extremities, but no adventitious heart or lung sounds, and palpable central and peripheral pulses.
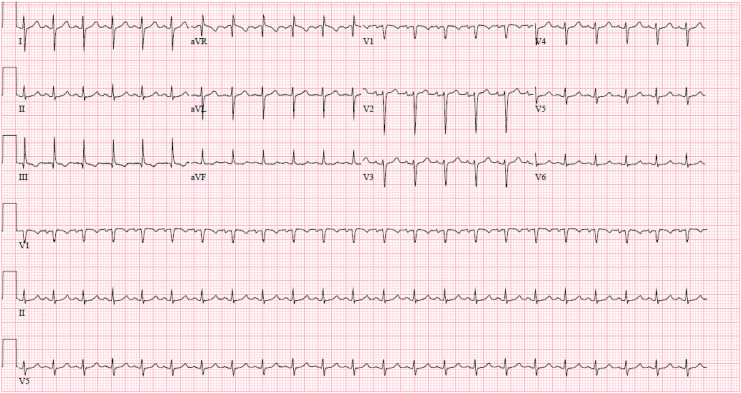
Chest and abdominal X-rays were unremarkable. POCUS revealed no ascites, no pleural effusion and no pericardial effusion. Laboratory evaluation revealed leukocytosis of 17,900/ul, hemoglobin of 16.8 g/dL, mild thrombocytopenia of 155,000/ul, hypoalbuminemia of 1.6 g/dl and proteinuria of 3+ protein with a urine protein-to-creatinine ratio of 3.7, consistent with his nephrotic syndrome. Electrocardiogram (ECG) was indicative of right heart strain. (Fig. 1 ) D-dimer was markedly elevated at 74,443 ng/ml. CT-angiography of his chest was obtained and revealed a saddle pulmonary embolism extending into the segmental and subsegmental branches bilaterally with evidence of right heart strain. (Fig. 2 ) The patient was treated with heparin and tissue plasminogen activator (tPA). He was admitted to the Pediatric Intensive Care Unit where he was also treated with systemic glucocorticoids, antithrombin III infusions, and enalapril for hypertension and to decrease protein wasting. He was successfully transitioned to warfarin and discharged home on day 21.
Fig. 1.
EKG.
EKG showing sinus tachycardia as well as classic “S1Q3T3” pattern of acute cor pulmonale. Note large S wave in lead I, a Q wave in lead III and an inverted T wave in lead III that together indicate acute right heart strain.
Fig. 2.
CT Angio.
Saddle pulmonary embolism with CT evidence for right heart strain.
3. Discussion
Evidence suggests coagulation function is significantly deranged during COVID-19 infection and may predispose patients to arterial and venous thrombotic complications due to excessive inflammation, platelet activation, endothelial dysfunction, and stasis [3].
Nephrotic syndrome is one of the most common pediatric kidney diseases, with an incidence of 2–7 per 100,000 [4]. Venous thromboembolism (VTE) occurs in roughly 3% of children with nephrotic syndrome, though incidence approaches 25% in high-risk groups [4].
Nephrotic syndrome produces a hypercoagulable state due to thrombocytosis, and hemostatic abnormalities, including decreased levels of antithrombin III, free protein S, and plasminogen secondary to urinary losses. In addition, our patient was at increased risk for thromboembolic events due to obesity, second-hand smoke exposure, prolonged immobilization due to virtual school, and multiple recent hospital admissions.
Currently, there are no standardized recommendations for pharmacologic prophylaxis of VTE for pediatric patients diagnosed with COVID-19. A handful of children's hospitals across the United States have implemented algorithms for anticoagulation in COVID-19 patients. Recommendations for initiation of pharmacologic prophylactic anticoagulation include patients with COVID-19 plus risk factors for severe disease, such as patients admitted to the ICU or those with Multisystem Inflammatory Syndrome in Children (MIS-C), d-dimer over two times the upper limit of normal or those with significant elevation of markers of inflammation (CRP, ESR, or fibrinogen), or additional VTE risk factors in personal or family medical history, medications or immobility.
4. Conclusion
This case highlights the risk of subsequent thrombotic complications in pediatric patients following COVID-19 infection and supports the need for standardized guidelines for pharmacologic prophylaxis for VTE in patients with COVID-19 and risk factors for thromboembolism. Pulmonary embolism is a rare yet potentially fatal finding in the pediatric population. Due to its rarity, it is crucial to raise awareness about its increased risk in combination with COVID-19 to avoid potential misdiagnoses on initial presentation [5].
Declaration of Competing Interest
None.
References
- 1.Rotzinger D.C., Beigelman-Aubry C., von Garnier C., Qanadli S.D. Pulmonary embolism in patients with COVID-19: time to change the paradigm of computed tomography. Thromb Res. 2020;190:58–59. doi: 10.1016/j.thromres.2020.04.011. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7151364/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Price L.C., McCabe C., Garfield B., Wort S.J. Thrombosis and COVID-19 pneumonia: the clot thickens! Eur Respir J. 2020;56(1) doi: 10.1183/13993003.01608-2020. Published 2020 Jul 30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Di Tano G., Moschini L., Loffi M., Galeazzi G., Testa S., Danzi G.B. Late pulmonary embolism after COVID-19 pneumonia despite adequate rivaroxaban treatment. EJCRIM. 2020:7. doi: 10.12890/2020_001790. https://www.ejcrim.com/index.php/EJCRIM/article/view/1790 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Agha B.S., Sturm J.J., Simon H.K., Hirsh D.A. Pulmonary embolism in the pediatric emergency department. Pediatrics. 2013 Oct;132(4):663–667. doi: 10.1542/peds.2013-0126. https://pediatrics.aappublications.org/content/132/4/663.short Epub 2013 Sep 2. PMID: 23999960. [DOI] [PubMed] [Google Scholar]
- 5.Porfidia A., Valeriani E., Pola R., Porreca E., Rutjes A.W.S., Di Nisio M. Venous thromboembolism in patients with COVID-19: systematic review and meta-analysis. Thromb Res. 2020;196:67–74. doi: 10.1016/j.thromres.2020.08.020. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7420982/ [DOI] [PMC free article] [PubMed] [Google Scholar]