Abstract
Objective
The purpose of this study was retrospectively to analyze the risk factors for non-union in Anderson–D’Alonzo type III odontoid fractures with conservative treatment.
Methods
25 patients with type III fractures were analyzed. Coronal and sagittal tilt as well as sagittal and lateral mass gaps were measured by using computed tomography.
Results
The non-union group had significantly higher age, greater coronal tilt and lateral mass gap. Especially, the lateral mass gap was >2 mm in all cases with non-union.
Conclusions
Higher age, coronal tilt, and lateral mass gap were significant risk factors for non-union.
Keywords: Anderson–D’Alonzo type III odontoid Fractures, Non-union, Risk factors, Conservative treatment
1. Introduction
With the aging of many populations, the number of osteoporotic vertebral fractures has been increasing. Odontoid fracture is the most common isolated spinal fracture in the elderly,1 and the Anderson–D’Alonzo classification is the most well-known and widely used system.2 Type I fractures are avulsion fractures at the tip of the dens; type II fractures are located at the junction of the odontoid base with the central body of the axis, and type III fractures pass through the cranial cancellous body of the axis. In general, surgical treatment is recommended in type II fractures because of a high risk of non-union, whereas type I and type III fractures are managed with conservative treatment.3,4 However, non-union after conservative treatment occasionally occurs in type III fractures,5 so an appropriate decision-making strategy to decide if conservative or surgical treatment in type III fractures is necessary.
Anderson and D'Alonzo initially reported a high union rate of >90% for type III fractures.2 However, Clark and White argued that the union rate was not very high and the non-union rate with conservative treatment was ≤13% in conservative treatment.5 Hence, type III fractures were not benign, and the researchers suggested that patients with these fractures should undergo rigid external immobilization using a halo vest. Considering this non-union rate in conservative treatment of type III fractures, it is crucial for surgeons to appropriately select either conservative or surgical treatment, but only a few reports have investigated the risk factors of non-union in conservative treatment.6, 7, 8
It is clinically important to know the degree of instability of the fracture area to assess the risk of non-union, and the majority of papers have focused on the gap distance of the fracture.6,8 However, fracture instability is affected by not only the size of the fracture, but also by the extent of the fracture to the C2 vertebral body. Especially, the lateral mass greatly contributes to the stability of the C2 vertebral body, and if the fracture extends to a lateral mass, the fracture could become unstable.9 However no reported study has evaluated these fractures in detail, including the size and extent of a fracture. The study aim was to collect conservative treatment cases of type III fractures from a database of multicenter studies and analyze the risk factors for non-union by reviewing the fracture patterns.
2. Material and methods
2.1. Study population
We conducted 68 patients with type III odontoid fractures who were nonoperatively treated with either a hard collar or halo vest were selected from a database of patient records from 2009 to 2018 at 11 participating institutions in the Nagoya Spine Group. This study and all of its protocols were approved by our Institutional Review Board. Three patients with incomplete radiographical data and one with malignancy were excluded. Furthermore, 39 patients with <6 months of follow-up were excluded. Finally, a total of 25 patients were investigated, including eight males and 17 females with an average age of 67.6 ± 17.8 years.
2.2. Data collection and evaluation
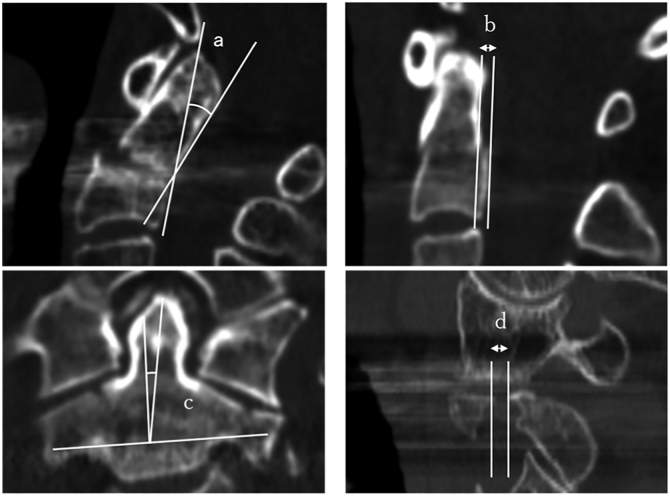
The C2 fracture morphology was retrospectively assessed by using computed tomography (CT), and fractures were classified according to the Anderson–D’Alonzo classification. Coronal and sagittal tilt were defined as the inclination of the axial vertebrae due to fractures in the coronal and sagittal cross-sections of the CT images of the cervical spine, respectively. Coronal tilt, sagittal tilt, sagittal gap, and largest lateral mass gap were measured from the CT images of the cervical spine (Fig. 1). Demographic and clinical data, including age, sex, follow-up, types of external immobilization, and mechanism of injury were reviewed. Fracture union was judged by observation of solid bony bridging on cervical spine coronal and sagittal CT images.
Fig. 1.
The measurement of (A) sagittal tilt, (B) sagittal gap, (C) coronal tilt, and (D) lateral mass gap on computed tomography.
2.3. Statistical analysis
All statistical analyses were performed by using SPSS v24 software (IBM Corp., Armonk, NY, USA). The Mann–Whitney U test was used to compare the mean values of continuous variables, and the chi-square test was used to compare categorical variables between groups. The threshold for significance was set at P < 0.05.
3. Results
The chief complaint was neck pain in all patients, and there were no cases with neurological deficits. The most frequent cause of injury was a fall (64.0%), and the most frequently provided treatment was hard collar immobilization (80.0%; Table 1).
Table 1.
Summary of demographic data.
| Variable | |
|---|---|
| Number of patients | 25 |
| Mean age (years old) | 67.6 ± 17.8 |
| Sex (male/female) | 8/17 |
| Mean follow-up (days) | 317.0 ± 288.9 |
| External immobilization (hard collar/halo vest) | 20 (80.0%)/5 (20.0%) |
| Mechanism of injury | |
| Fall down | 16 (64.0%) |
| Fall from height | 4 (16.0%) |
| Traffic accident | 4 (16.0%) |
| Injured in mountain bike | 1 (4.0%) |
Values are shown as the mean ± standard deviation.
Bony union was confirmed in 22 (88.0%) patients (Table 2). Comparison of the patients with bony union and non-union showed that there were no significant differences in sex, follow-up period, external immobilization, sagittal tilt, or sagittal gap. In contrast, the mean age (85.7 ± 6.0 years) was significantly higher in the non-union group than in the union group (65.1 ± 17.5 years; P < 0.05). The coronal tilt and lateral mass gap were also significantly greater (P < 0.01 and P < 0.05, respectively) in the non-union group (9.9 ± 0.8° and 3.9 ± 3.0 mm) than in the union group (2.9 ± 3.2° and 1.0 ± 0.9 mm; Fig. 2, Table 2). Especially, the lateral mass gap was >2 mm in all patients with non-union, whereas the gap was <2 mm in the union group. Thus, this lateral mass gap could be a significant risk factor for non-union.
Table 2.
Comparative analysis between union group and non-union group.
| Union (N = 22) | Non-Union (N = 3) | P value | |
|---|---|---|---|
| Mean age in years | 65.1 ± 17.5 | 85.7 ± 6.0 | <0.05 |
| Sex (male/Female) | 8/14 | 0/3 | n.s. |
| Mean follow-up days | 325.8 ± 306.6 | 252.3 ± 86.3 | n.s. |
| External immobilization (Hard collar/Halo vest) | 17/5 | 3/0 | n.s. |
| Coronal tilt (°) | 2.9 ± 3.2 | 9.9 ± 0.8 | <0.01 |
| Sagittal tilt (°) | 8.6 ± 9.4 | 11.8 ± 4.0 | n.s. |
| Sagittal gap (mm) | 1.2 ± 1.3 | 2.2 ± 2.6 | n.s. |
| Lateral mass gap (mm) | 1.0 ± 0.9 | 3.9 ± 3.0 | <0.05 |
Values are shown as the mean ± standard deviation.
n.s. = not significant.
Fig. 2.
Computed tomography (CT) images from a 92-year-old female who fell and diagnosed as an Anderson–D’Alonzo type III odontoid fracture. Sagittal and coronal CT showed (A) the sagittal gap: 0 mm, sagittal tilt angle: 8.0° (B), and lateral mass gap was 2.0 mm(C). The coronal tilt angle was 9.0°. The patient had neck pain without neurologic impairments. (D–F) Sagittal and coronal CT images at the final follow-up showed non-union despite hard collar treatment for 6 months. The white arrows indicate fracture lines for each panel.
4. Discussion
This study demonstrated that older age, a greater coronal angle of the C2 dens, and the lateral mass gap were risk factors for non-union in patients with type III odontoid fractures treated conservatively. Although older age and coronal tilt have been reported as risk factors, the lateral mass gap could be another significant risk factor for non-union. Therefore, before considering treatment strategies for patients with type III fractures, a detailed CT analysis, including assessment of the coronal tilt and lateral mass gap, could help prevent non-union.
Several studies have reported a recent increase in the incidence of odontoid fractures secondary to low-energy trauma in elderly patients.10, 11, 12 Amling et al.13 found that type III odontoid fractures among the elderly were the most frequently caused by an osteoporotic fracture mechanism. The bony union rate for conservative treatment using external immobilization of type III odontoid fractures is relatively high because of the contact area of the large cancellous surface14 and the presence of two robust nutritional arteries.15 On the other hand, a few reports showed that non-union cases as a problem in the conservative management of type III odontoid fractures and analyzed risk factors for non-union. Older age has been found to be an independent risk factor for non-union, and Müller et al.7 reported a higher fibrous union risk for patients >65 years old. In the present study, all of the patients were >65 years old in the non-union group, so we were more cautious in selecting the treatment for these older patients.
The degree of fracture dislocation can also be a risk for non-union. Niemeier et al.8 reported a complex type of type III odontoid fractures characterized by >50% comminution of the lateral mass or secondary fracture lines extending into the vertebral body or pars interarticularis. They reported that patients with complex type III odontoid fractures had a 21% failure rate with conservative management and required delayed surgery. The majority of these patients had a risk of non-union if they had either a progressive sagittal gap >2 mm or tilt >5°. Müller et al.7 also reported unstable type III fractures characterized by a sagittal gap >2 mm or tilt >11°. The present study revealed that two (66.7%) non-union patients had sagittal tilt > 11° and a lateral mass fracture gap > 2 mm. The sagittal gap was approximately 2 mm even in non-union cases, and patients with severe dislocation were not included. This may explain why we did not identify the sagittal gap as a risk factor in this study, in contrast to the findings of some previous reports. However, even if the sagittal gap appears to be stable, a lateral mass fracture gap >2 mm could be a risk factor of non-union, so the size and extent of the lateral mass of the fracture gap should be solely assessed on CT at admission.
With respect to the indication for surgical intervention, a fracture sagittal gap > “5 mm of vertical” distraction has been reported. Kirkpatric et al.6 reported three patients with vertically unstable type III odontoid fractures who required posterior C1–C2 arthrodesis because of persistent vertical instability after use of a halo vest. The researchers reported that type III odontoid fractures with a gap >5 mm of vertical distraction were unstable and required surgery with C1–C2 posterior arthrodesis by using transarticular screws. Jung et al.16 described one patient with vertically unstable type III odontoid fractures who had a severe neurological deficit after traction treatment. The vertical dislocation of the axis was approximately 5.7 mm, and the patient needed surgical treatment. Although no patients had severe vertical displacement of the dens in the current study, vertical dislocation >5 mm is unstable and could be another important issue in the decision-making process to select either conservative or surgical treatment.
Our study had several limitations that should be considered. First, the number of cases was small because many patients were transferred to another hospital for rehabilitation during the treatment period. Second, we did not evaluate clinical outcomes because our primary focus was CT evaluation of bony union. Lastly, we did not analyze damage to soft tissues, such as the posterior ligament or cervical instability following axis fractures.
5. Conclusion
Although conservative therapy is an effective approach for type III odontoid fractures, non-union was observed in 12.0% of the patients in this study. Higher age, coronal tilt, and the lateral mass gap were significant risk factors for non-union. Radiographical parameters should be solely assessed by CT at admission.
Footnotes
No funds were received in support of this work. No benefits in any form have been or will be received from a commercial party related directly or indirectly to the subject of this manuscript. The authors declare no conflict of interest.
References
- 1.Ryan M.D., Henderson J.J. The epidemiology of fractures and fracture-dislocations of the cervical spine. Injury. 1992;23:38–40. doi: 10.1016/0020-1383(92)90123-a. [DOI] [PubMed] [Google Scholar]
- 2.Anderson L.D., D'Alonzo R.T. Fractures of the odontoid process of the axis. J Bone Jt Surg Am Vol. 1974;56:1663–1674. [PubMed] [Google Scholar]
- 3.Grasso G., Leone L., Torregrossa F. Management of odontoid cervical fracture. World Neurosurg. 2019;123:246–247. doi: 10.1016/j.wneu.2018.12.038. [DOI] [PubMed] [Google Scholar]
- 4.Iyer S., Hurlbert R.J., Albert T.J. Management of odontoid fractures in the elderly: a review of the literature and an evidence-based treatment algorithm. Neurosurgery. 2017;82:419–430. doi: 10.1093/neuros/nyx546. [DOI] [PubMed] [Google Scholar]
- 5.Clark C.R., White A.A., 3rd Fractures of the dens. A multicenter study. J Bone Joint Surg Am. 1985;67:1340–1348. [PubMed] [Google Scholar]
- 6.Kirkpatrick J.S., Sheils T., Theiss S.M. Type-III dens fracture with distraction: an unstable injury. A report of three cases. J Bone Joint Surg Am. 2004;86:2514–2518. [PubMed] [Google Scholar]
- 7.Muller E.J., Schwinnen I., Fischer K., Wick M., Muhr G. Non-rigid immobilisation of odontoid fractures. Eur Spine J. 2003;12:522–525. doi: 10.1007/s00586-003-0531-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Niemeier T.E., Dyas A.R., Manoharan S.R., Theiss S.M. Type III odontoid fractures: a subgroup analysis of complex, high-energy fractures treated with external immobilization. J Craniovertebral Junction Spine. 2018;9:63–67. doi: 10.4103/jcvjs.JCVJS_152_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Martín-Ferrer S. Odontoid fractures. J Neurosurg. 2001;95:158–159. doi: 10.3171/spi.2001.95.1.0158. [DOI] [PubMed] [Google Scholar]
- 10.Huybregts J.G., Jacobs W.C., Vleggeert-Lankamp C.L. The optimal treatment of type II and III odontoid fractures in the elderly: a systematic review. Eur Spine J. 2013;22:1–13. doi: 10.1007/s00586-012-2452-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Platzer P., Thalhammer G., Oberleitner G., Schuster R., Vecsei V., Gaebler C. Surgical treatment of dens fractures in elderly patients. J Bone Joint Surg Am. 2007;89:1716–1722. doi: 10.2106/JBJS.F.00968. [DOI] [PubMed] [Google Scholar]
- 12.Wisoff H.S. Fracture of the dens in the aged. Surg Neurol. 1984;22:547–555. doi: 10.1016/0090-3019(84)90430-0. [DOI] [PubMed] [Google Scholar]
- 13.Amling M., Wening V.J., Posl M., Grote H.J., Hahn M., Delling G. [Structure of the axis--key to the etiology of the dens fracture] Chirurg. 1994;65:964–969. [PubMed] [Google Scholar]
- 14.Hanssen A.D., Cabanela M.E. Fractures of the dens in adult patients. J Trauma. 1987;27:928–934. doi: 10.1097/00005373-198708000-00013. [DOI] [PubMed] [Google Scholar]
- 15.Althoff B., Goldie I.F. The arterial supply of the odontoid process of the axis. Acta Orthop Scand. 1977;48:622–629. doi: 10.3109/17453677708994808. [DOI] [PubMed] [Google Scholar]
- 16.Jung M.H., Lee J.K., Hur H., Jang J.W., Kim J.H., Kim S.H. Traction induced vertical displacement of odontoid due to type III odontoid fracture with unrecognized ligamentous injury: a case report. Korean J Nutr. 2014;10:149–151. doi: 10.13004/kjnt.2014.10.2.149. [DOI] [PMC free article] [PubMed] [Google Scholar]