Abstract
A 59-year-old woman with nail patella syndrome (NPS) presented with progressive and severe right knee pain for the past 3 years. Imaging demonstrated laterally dislocated patella, with asymmetric femoral trochlea, and advanced lateral compartment arthritis. The patient underwent robotic-assisted lateral unicompartmental knee arthroplasty (RAUKA). The patient saw marked improvements in patient-reported outcome measurements from her initial visit to the last follow-up visit. While treatment of knee osteoarthritis in patients with NPS can be difficult, especially with attempts of patellar realignment, we present a case of a patient who underwent RAUKA, with sustained improvements in patient outcomes and range of motion, at the 2-year follow-up visit. This study is the first of its kind to demonstrate the use of a novel technology in a rare condition.
Keywords: Nail patella syndrome, Robotic-assisted, Unicompartmental knee surgery, MAKO, Haptic
Introduction
Nail patella syndrome (NPS) also known as hereditary onycho-osteodysplasia, Turner-Keizer disease, or Fong disease is a rare autosomal dominant genetic condition affecting 1 in 50,000 newborns [1,2]. The condition was initially termed by Chatelain et al. in 1820 [3]. While nail changes are the most uniform features of NPS, the elbow, hips, and knees are also impacted from the condition [4]. Elbow abnormalities impact range of motion (ROM) by limiting extension, pronation, and supination [4]. Bony processes project posteriorly and laterally from the iliac bones of the pelvis which are generally bilateral and conical [5]. With knee manifestations, the patella may be small, irregularly shaped, or absent in patients with NPS [5]. In addition, most patients with NPS present with knee symptoms with complaints of anterior knee pain and bilateral patellar instability [5]. These changes are attributed to genetic mutations in the LIM homeobox transcription factor 1-beta (LIMX1B) gene, located on the long arm of chromosome 9 in the 9q34.1 locus, close to the ABO blood group locus [4,[6], [7], [8]]. Loss-of-function mutations of LMX1B causes NPS [[6], [7], [8]]. As such, we present a rare and unique approach in a case of a patient with NPS presenting with knee pain and patellar instability with genu valgum deformity, who subsequently underwent robotic-assisted lateral unicompartmental knee arthroplasty (UKA).
The patient was informed the data concerning the case would be submitted for potential publication and provided her consent.
Case history
A 59-year-old Caucasian female was referred to our clinic with right knee pain and instability for the past 3 years, which she describes as worsening and hindering her activities of daily living. The patient had participated in full sports and daily activities with a known chronically dislocated patella since her diagnosis with NPS as a teenager. The patient’s height was 170.2 centimeters, weight 65.77 kilograms, and body mass index 22.71 kg/m2. The patient described the pain as being sharp with symptoms of swelling, weakness, and giving away; rating the pain as an 8 out of 10, worsening with physical activity. Relevant past medical history included a torn meniscus of the right knee requiring a meniscectomy which occurred approximately 4 years before the office visit date. The patient mentioned she had tried conservative management to alleviate her knee pain by undergoing physical therapy from 2014 to 2017, trying various pain medications, and having tried corticosteroid injections annually from 2015 to 2018, but these interventions were unsuccessful in mitigating her knee pain. Preoperative patient-reported outcome measurements of the Short-Form 12 Physical Component Score (SF12-PCS) and Mental Component Score (SF12-MCS) were 23.51 and 59.31, respectively. Western Ontario and McMaster Universities Arthritis Index total score was 60 with physical functional score being 41, pain score being 13, and stiffness being 6.
On physical examination, the patient ambulated with an antalgic gait without an assisted walking device. Muscular examination showed 5/5 muscle strength in the right lower extremity. The patient had intact sensations and 2+ palpable dorsalis pedis and posterior tibial pulses in the right lower extremity. The right knee demonstrated a ROM of 2° to 126°, a correctable valgus deformity, lateral joint line tenderness, and laterally tracking dislocated patella. Radiography and computed tomography (CT) scan revealed valgus deformity of the right lower extremity, a laterally dislocated patella with intact cartilage, and a deep femoral trochlear groove with asymmetric condyles (Fig. 1a–e). Posteroanterior radiographic views demonstrated bone on bone in the lateral compartment with a pristine medial compartment and an intact anterior cruciate ligament, per physical examination (Fig. 1b).
Figure 1.
Radiographic images of a patient with Nail-Patella syndrome with anteroposterior view lateral compartment osteoarthritis (a) and lateral compartment bone on bone osteoarthritis in the posteroanterior view (b). Lateral (c) and skyline views (d) showing the laterally dislocated patella. Axial computed tomography scans (e) of the right knee demonstrating a hypoplastic and laterally dislocated patella.
Owing to failure in conservative management, we discussed options with the patient, considering either a lateral UKA or total knee arthroplasty (TKA). As the patient’s quadriceps was functional, the patient was subsequently consented to undergo robotic-assisted lateral UKA using the Stryker MAKO Robotic-Assisted system (Stryker MAKO Corporation, Davie, Florida). In addition, other case reports of patients with NPS undergoing primary TKA have shown improper patellar tracking requiring soft tissue releases [2,9]. With adequate quadricep function and wanting to avoid extensive lateral retinacular releases or tibial tubercle transfer, we felt a lateral UKA would provide better results. Preoperative CT scans of the patient’s operative knee were used to accurately template the sizes of the prosthetic components necessary. Imaging revealed the presence of a hypoplastic patella dislocated laterally and deep femoral trochlea (Fig. 1e). The MAKO graphical user interface revealed the patient to have a mechanical axis alignment of 3.5° of valgus, with a correctable deformity to 1° valgus alignment. A central-patellar surgical approach (ie, medial approach) revealed a laterally dislocated patella (Fig. 2), advanced grade 4 Kellgren and Lawrence changes in the posterior lateral compartment, an intact anterior cruciate ligament, and pristine patellofemoral joint and medial joint cartilage. After implant customization, stable gaps and kinematic rollback were defined before bony resections. Cemented components after trialing revealed optimized alignment and balance of the knee (Fig. 2).
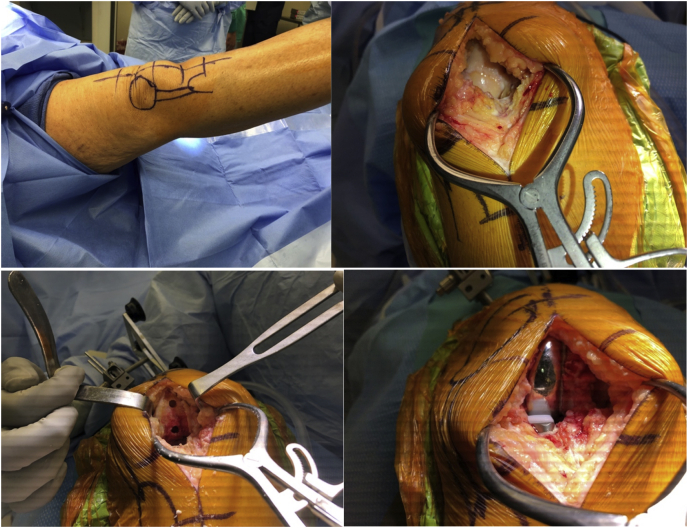
Figure 2.
Operative pictures of the right knee in a patient with Nail Patella syndrome demarcating presence of patella on the lateral side (top-left). Intraoperative images showing the lateral femoral compartment (top-right). Bone preparation for cementing of the lateral compartment (bottom-left). Final pictures of the cemented MCK lateral onlay implants (bottom-right).
At the 2-week postoperative follow-up visit, the patient stated she was doing well and had discontinued the use of her walking device. ROM at this visit was 0° to 75° and improved to 0° to 100° by the 6-week follow-up visit. Six months postoperatively, the patient showed marked improvement with her ROM increasing to 0° to 116°. Long leg weight-bearing radiographs demonstrated a mechanical axis alignment of +0.69° from neutral. At the 24-month follow-up visit, the patient stated she was exercising up to 3 times per week by cycling, walking, or performing pilates. ROM at this office visit was 0° to 118°. Patient-reported outcome measurements completed during this visit demonstrated improvement compared with the preoperative visit with SF12-PCS and SF12-MCS of 55.50 (preoperatively: 23.51) and 61.82 (preoperatively: 59.31), respectively, and total Western Ontario and McMaster Universities Arthritis Index score of 2 (pain: 0, stiffness: 0, physical functioning: 2) (preoperatively: 60). Forgotten Joint Score of the operative knee was 98. Long leg, anteroposterior, lateral, and skyline view radiographs were taken to confirm adequate mechanical alignment, implant position, and absence of radiolucencies. Long leg weight-bearing radiographs demonstrated a mechanical axis alignment of +0.12° valgus (Fig. 3a). Radiographs of the operative knee in three views demonstrated stable implant position without any subsidence or radiolucencies around the prostheses and lateral patellar dislocation. The patient was recommended to follow-up as needed.
Figure 3.
Radiographic images at the most recent follow-up visit demonstrating a neutral mechanical alignment of +0.12° valgus by measuring the mechanical axis alignment (a). Lateral (b) and skyline views (c) demonstrating proper implant positioning without any signs of subsidence or radiolucent lines. Red star = laterally dislocated patella.
Discussion
We report a case of a 59-year-old female presenting with NPS with knee pain successfully treated with robotic-assisted lateral UKA. While the prevalence of NPS is rare, this case demonstrates the ability to properly treat these patients with robotic-assisted UKA for isolated compartment arthritis. Most of the existing literature regarding the knee manifestations of NPS have been limited to radiographic assessment; however, no studies have discussed the surgical treatment and clinical outcomes of these patients (Table 1) [2,9,10]. To the best of our knowledge, we believe this is the first case representing a patient with NPS undergoing primary robotic-assisted UKA demonstrating excellent outcomes 24 months after the index procedure, based on improvements of ROM and outcome measurements.
Table 1.
Existing literature of other investigations of nail-patella syndrome patients undergoing either total knee arthroplasty or unicompartmental knee arthroplasty.
| Author | Year | Sample size | Procedure performed | Laterality |
|---|---|---|---|---|
| Yang et al. [15] | 2020 | n = 1 | UKA | Right medial |
| Curbo et al. [2] | 2019 | n = 1 | TKA | Right |
| Khaimov et al. [16] | 2018 | n = 2 | TKA | Bilateral |
| Louboutin et al. [9] | 2017 | n = 1 | TKA | Right |
| Lachiewicz and Herndon [17] | 1997 | n = 1 | TKA | N/A |
N/A, not applicable; TKA, total knee arthroplasty; UKA, unicompartmental knee arthroplasty.
Initially termed in the 1800s, Chatelin et al. described the presence of nail dysplasia being associated with knee and elbow dysplasia [5]. The familial and genetic nature of the condition was not recognized until the late 1800s by Pye-Smith and Little [6,11]. Recently, NPS and its involvement in other skeletal areas such as the ankles, feet, and spine have been reported [5,12,13]. Ankle and foot manifestations can present with talipes equinovarus, calcaneovarus, calcaneovalgus, equinovalgus, or hyperextension of the foot. Tightening of the Achilles tendon is also common. Spinal and chest wall deformities include increased lumbar lordosis, scoliosis, spondylolisthesis, or pectus excavatum [13]. NPS patients have also been reported to have reduced bone mineral density in the hips, predisposing these patients to increased fractures [13]. With respect to the knee, the anatomic abnormalities in these patients often lead to either subluxation or dislocation of the patellae causing knee instability and pain [2,9,14]. The midline synovial septum, which divides the knee into the medial and lateral parts of the knee, is the cause of this dislocation. In patients with NPS, this septum cuts a deep grove into the trochlea preventing the patella from being properly seated in the trochlear groove [14].
We believe implementing the robotic-assisted system facilitated the ability to resurface the affected compartment and refrain from issues related to patellar realignment which could cause flexion stiffness or continued instability. The CT planning allowed anatomic positioning, and the implants were adjusted to compensate for the screw-home mechanism with congruency through the full ROM. The gaps were optimized to adjust for the coronal alignment target. The haptics enabled a mini-medial approach to compensate for the laterally dislocated patella. These patients can function at a high level with a chronically dislocated patella, and her recovery was uneventful.
Conclusion
Our case adds to the literature of treatment strategies for patients with NPS with isolated knee osteoarthritis. This case demonstrates an excellent early recovery and continued improvement at the 24-month visit in a 59-year-old patient with NPS. In addition, longer term outcomes and whether conversion to TKA becomes necessary in the future will be determined. This will enhance the literature by determining whether performing conversion to TKA without addressing the patellar dislocation can be equally successful and even potentially offer a longer term solution.
Conflicts of interest
The authors declare the following financial interests/personal relationships which may be considered as potential competing interests: Dr. Martin W. Roche is a paid consultant and stock ownership in Stryker.
Appendix A. Supplementary data
References
- 1.Witzgall R. Nail-patella syndrome. Pflugers Arch Eur J Physiol. 2017;469:927. doi: 10.1007/s00424-017-2013-z. [DOI] [PubMed] [Google Scholar]
- 2.Curbo M.E., Park K.J., Brown L.D., Incavo S.J. Total knee arthroplasty in a patient with nail-patella syndrome (NPS) Knee. 2019;26:273. doi: 10.1016/j.knee.2018.11.014. [DOI] [PubMed] [Google Scholar]
- 3.Ghoumid J., Petit F., Holder-Espinasse M. Nail-Patella Syndrome: clinical and molecular data in 55 families raising the hypothesis of a genetic heterogeneity. Eur J Hum Genet. 2016;24:44. doi: 10.1038/ejhg.2015.77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.McIntosh I., Dunston J.A., Liu L., Hoover-Fong J.E., Sweeney E. Nail patella syndrome revisited: 50 years after linkage. Ann Hum Genet. 2005;69:349. doi: 10.1111/j.1529-8817.2005.00191.x. [DOI] [PubMed] [Google Scholar]
- 5.Chen H. Springer New York; New York, NY: 2016. Nail-patella syndrome. Atlas Genet. Diagnosis Couns. p. 1. [Google Scholar]
- 6.Bongers E.M.H.F., de Wijs I.J., Marcelis C., Hoefsloot L.H., Knoers N.V.A.M. Identification of entire LMX1B gene deletions in nail patella syndrome: evidence for haploinsufficiency as the main pathogenic mechanism underlying dominant inheritance in man. Eur J Hum Genet. 2008;16:1240. doi: 10.1038/ejhg.2008.83. [DOI] [PubMed] [Google Scholar]
- 7.Dreyer S.D., Morello R., German M.S. LMX1B transactivation and expression in nail-patella syndrome. Hum Mol Genet. 2000;9:1067. doi: 10.1093/hmg/9.7.1067. [DOI] [PubMed] [Google Scholar]
- 8.Sato U., Kitanaka S., Sekine T., Takahashi S., Ashida A., Igarashi T. Functional characterization of LMX1B mutations associated with nail-patella syndrome. Pediatr Res. 2005;57:783. doi: 10.1203/01.PDR.0000157674.63621.2C. [DOI] [PubMed] [Google Scholar]
- 9.Louboutin L., Wascher D., Neyret P. Management of patellar problems in skeletally mature patients with nail–patella syndrome. Knee Surg Sports Traumatol Arthrosc. 2017;25:3012. doi: 10.1007/s00167-016-4044-y. [DOI] [PubMed] [Google Scholar]
- 10.Total knee arthroplasty for osteoarthritis in hereditary onycho-osteodysplasia (nail-patella syndrome): a case report - PubMed n.d. https://pubmed.ncbi.nlm.nih.gov/9040887/ [accessed 30.12.20] [PubMed]
- 11.West J.A., Louis T.H. Radiographic findings in the nail-patella syndrome. Baylor Univ Med Cent Proc. 2015;28:334. doi: 10.1080/08998280.2015.11929265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Nail-Patella Syndrome - PubMed. https://pubmed.ncbi.nlm.nih.gov/20301311/ [accessed 30.12.20]
- 13.Towers A.L., Clay C.A., Sereika S.M., McIntosh I., Greenspan S.L. Skeletal integrity in patients with nail patella syndrome. J Clin Endocrinol Metab. 2005;90:1961. doi: 10.1210/jc.2004-0997. [DOI] [PubMed] [Google Scholar]
- 14.Lippacher S., Mueller-Rossberg E., Reichel H., Nelitz M. Correction of malformative patellar instability in patients with nail-patella syndrome: a case report and review of the literature. Orthop Traumatol Surg Res. 2013;99:749. doi: 10.1016/j.otsr.2013.03.031. [DOI] [PubMed] [Google Scholar]
- 15.Yang J.W., Heckmann N.D., Della Valle C.J. Unicompartmental knee arthroplasty in a patient with nail-patella syndrome: a case report. JBJS Case Connect. 2020;10:e2000216. doi: 10.2106/JBJS.CC.20.00216. [DOI] [PubMed] [Google Scholar]
- 16.Khaimov M., Fakhoury J., Karim F., Bitterman A., Alpert S. Total knee arthroplasty in patients with familial patellar absentia syndrome: a 40-year update. JBJS Case Connect. 2018;8:e100. doi: 10.2106/JBJS.CC.17.00329. [DOI] [PubMed] [Google Scholar]
- 17.Lachiewicz P., Herndon C. Total knee arthroplasty for osteoarthritis in hereditary onycho-osteodysplasia (nail-patella syndrome): a case report. Am J Orthop (Belle Mead NJ) 1997 [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.