Abstract
Background/Objectives:
Older adults (>75 years of age) represent two-thirds of ASCVD deaths. The 2013 and 2018 American multi-society cholesterol guidelines recommend using at least moderate intensity statins for older adults with atherosclerotic cardiovascular disease (ASCVD). We examined annual trends and statin prescribing patterns in a multiethnic population of older adults with ASCVD.
Design:
Retrospective longitudinal study using electronic health record (EHR) data from 2007–2018.
Setting:
A large multi-specialty health system in Northern California.
Participants:
A total of 24,651 adults older than 75 years with ASCVD.
Measurements:
Statin prescriptions for older adults with known ASCVD were trended over time. Multivariable regression models were used to identify predictors of statin prescription (logistic) after controlling for relevant demographic and clinical factors.
Results:
The study cohort included 24,651 patients older than 75 years; 48% were women. While prescriptions for moderate/high intensity statins increased over time for adults over 75, fewer than half of the patients (45%) received moderate/high intensity statins in 2018. Women (OR: 0.77, [95% CI: 0.74, 0.80]), patients who had heart failure (OR: 0.69, [95% CI: 0.65, 0.74]), those with dementia (OR: 0.88, [95% CI: 0.82, 0.95]) and patients who were underweight (OR: 0.64, [95% CI: 0.57, 0.73]) were less likely to receive moderate/high intensity statins.
Conclusions:
Despite increasing prescription rates between 2007 and 2018, guideline-recommended statins remained underused in older adults with ASCVD, with more pronounced disparities among women and those with certain comorbidities. Future studies are warranted to examine reasons for statin underuse in older adults with ASCVD.
Keywords: Secondary prevention, statins, ASCVD, coronary artery disease, stroke
INTRODUCTION
The aging population is rapidly growing, with over 20 million older adults in the United States over 75 years old.1 Atherosclerotic cardiovascular disease (ASCVD) is the leading cause of death in the United States and age is the single strongest predictor of ASCVD.2 Indeed, two-thirds of ASCVD deaths in the United States are among those over the age of 75.3
Older adults have been underrepresented in randomized trials that inform clinical practice strategies for optimal secondary prevention and cholesterol management.4,5,6 A recent individual person data meta-analysis by the cholesterol trial collaboration showed benefit to statin use in older adults for both primary and secondary prevention.7 Both the 2013 and 2018 multi-society cholesterol guidelines recommend at least moderate intensity statin therapy for patients over 75 with atherosclerotic cardiovascular disease.8,9 While ASCVD is the leading cause of death in this the population, statin use in older adults continues to be debated and real-world statin prescribing patterns are not well-known.3,4 Identifying trends and gaps in statin prescribing patterns may help identify opportunities to optimize statin therapy and related ASCVD outcomes in this high-risk population.
Using data from a large multi-specialty outpatient care organization in Northern California, we sought to evaluate temporal statin prescribing patterns and predictors of guideline-concordant statin prescription in a multiethnic population of older adults with ASCVD.
METHODS
The study population was selected from a large multi-specialty outpatient care organization in Northern California which serves more than a million patients each year. Epic® Electronic Health Records (EHR) from 2007–2018 comprised the data source for the study. We included patients who were over 75 years of age with ASCVD and had at least two outpatient visits in two consecutive years to ensure that patients received care within the healthcare system and to improve ascertainment. For comparison, we used the same criteria to identify a cohort of adults 65–75 years of age.
For each year, the index date was defined as the last visit date of the year. Patient clinical characteristics (clinical conditions, medication prescriptions, anthropometric measures, and laboratory values) were assessed as of the index date. A diagnosis of ASCVD was ascertained by problem lists as defined by the International Classification of Diseases (ICD), 9th and 10th revisions codes for coronary artery disease (CAD), cerebrovascular disease (CVD), and peripheral artery disease (PAD) (Supplementary Table).
Patient demographic characteristics and smoking status were self-reported and recorded in the EHR. Ages above 89 are aggregated for privacy reasons, therefore mean age is not reported. Race/ethnicity classifications followed the U.S. census criteria. When missing, we inferred their race/ethnicity by applying name-list based on the Social Security database.10 Clinical comorbidities included a diagnosis of hypertension, diabetes, heart failure, malignancy, renal disease, and dementia identified by ICD codes (Supplementary Table). Medication burden was captured as the total number of medications on the index date. Laboratory data included the total cholesterol and low-density lipoprotein cholesterol (LDL-C) values nearest to and at least within one year of index date and at least 30 days after statin prescription initiation (for those who were on statin therapy). Body mass index (BMI) was captured from vital signs at the encounter; BMI <18.5 kg/m2 was classified as underweight, 18.5 to <25 kg/m2 was classified as normal, 25 to <30 kg/m2 was classified as overweight and, 30 kg/m2 or greater was classified as obese.
Prescription orders were extracted from the patient’s last visit within the study period (2007–2018). Statin intensity was coded according to the American College of Cardiology/American Heart association (ACC/AHA) guidelines as follows: high intensity (daily dosage of Atorvastatin 40–80mg, Rosuvastatin 20–40mg, Lovastatin 80mg, Simvastatin 80mg); moderate intensity (Atorvastatin 10–39mg, Fluvastatin 80mg, Lovastatin 40–60mg, Pitavastatin 2–4mg, Pravastatin 40–80mg, Rosuvastatin 5–19mg, Simvastatin 20–40mg); and low intensity (Atorvastatin <10mg, Rosuvastatin <5m, Fluvastatin <80mg, Lovastatin <40mg, Pravastatin <40mg, Pitavastatin 1mg, Simvastatin <20mg).9 Prescriptions of non-statin lipid lowering agents including ezetimibe or proprotein convertase subtilisin/kexin type 9 (PCSK9) inhibitors (evolocumab, alirocumab) were also collected.
We identified the annual trend of moderate/high intensity statin prescriptions from 2007–2018 with person-year as the unit of analysis. The annual trend was plotted separately for each age category: 65–75 and 76 or over. Linear regressions were used to test if the slope of the trend was different from zero, for each age category, controlling for sex and adjusting standard errors to take into account patients over multiple years.
We compared demographic and clinical characteristics of patients by statin intensity as of the last patient-year. Logistic regressions were used to identify predictors of moderate/high intensity statin prescriptions. The predictors included patient age (65–75 versus 76+), sex, race/ethnicity, LDL-C and total cholesterol levels, selected comorbid conditions, and number of concurrent medications, separated by the median value. All predictors were adjusted for in the multivariable regression as listed in Table 2. We further assessed the association between statin use and LDL-C with simple linear regression and plotted average LDL level (and 95% confidence interval) by statin intensity.
Table 2.
Predictors of moderate and high-intensity statin prescription
| OR | Lower 95%CI | Upper 95%CI | P value | |
|---|---|---|---|---|
| Female (ref = Male) | 0.77 | 0.74 | 0.80 | <0.001 |
| Race (ref = NHW) | ||||
| Black | 0.96 | 0.82 | 1.13 | 0.654 |
| Asian | 1.20 | 1.14 | 1.26 | <0.001 |
| Hispanic | 0.94 | 0.87 | 1.02 | 0.127 |
| Other | 0.94 | 0.83 | 1.07 | 0.360 |
| ASCVD (ref = CAD) | ||||
| CVD | 1.38 | 1.30 | 1.47 | <0.001 |
| PAD | 1.14 | 1.05 | 1.25 | 0.002 |
| Polyvascular | 1.27 | 1.16 | 1.39 | <0.001 |
| Comorbidities | ||||
| Hypertension | 1.36 | 1.31 | 1.42 | <0.001 |
| Diabetes | 1.59 | 1.52 | 1.66 | <0.001 |
| Heart Failure | 0.69 | 0.65 | 0.74 | <0.001 |
| Cancer | 1.00 | 0.96 | 1.04 | 0.916 |
| Renal disease | 1.02 | 0.97 | 1.06 | 0.486 |
| Dementia | 0.88 | 0.82 | 0.95 | 0.001 |
| Polypharmacy | 1.28 | 1.23 | 1.33 | <0.001 |
| BMI (ref = normal BMI) | ||||
| Underweight | 0.64 | 0.57 | 0.73 | <0.001 |
| Overweight | 1.35 | 1.30 | 1.41 | <0.001 |
| Obese | 1.49 | 1.41 | 1.57 | <0.001 |
| Current smoker | 1.25 | 1.10 | 1.42 | 0.001 |
Abbreviations and definitions: OR, odds ratio; ref, reference; NHW, non-Hispanic white; ASCVD, atherosclerotic cardiovascular disease; CAD, coronary artery disease; CVD, cerebrovascular disease, PAD, peripheral artery disease; polyvascular, 2 or more types of atherosclerotic cardiovascular disease; polypharmacy, >9 prescription medications; BMI, body mass index. Odds ratios adjusted for all other covariates presented as well as being in the top 5 percentile of number of office visits in the preceding year.
Data management and statistical analyses were conducted with Stata 14.2 (College Station, TX) and a p-value <0.01 was considered statistically significant. The study was approved by the Internal Review Boards of Stanford University and Sutter Health.
RESULTS
There was a total of 109,029 adults over 75 years of age in our study cohort; of these 86,965 (80%) had primary care or specialty visits for two consecutive years in the Sutter Health system. A total of 24,651 had a diagnosis of ASCVD. Almost half of the patients were women (11,949 [48%]), 15,295 (62%) were non-Hispanic white (NHW), 3,263 (13%) were Asian, 1,293 (5%) were Hispanic, and 307 (1%) were black. The most common indication for statin therapy was coronary artery disease, followed by cerebrovascular disease. Most patients (16,804 [68%]) had concomitant hypertension, almost half (7,223 [46%]) had concomitant renal disease, 6,870 (28%) had malignancies and, 2,385 (10%) had dementia. Only 519 patients (2%) were current smokers, 780 patients (4%) were underweight and 12,554 (56%) were overweight or obese. Patients had a median number of 9 prescription medications not including lipid-lowering agents. When pooled across years, fewer than half (10,264 [42%]) received statins (Table 1); and 8,814 [36%] received moderate/high intensity statins. Only 364 (1%) of patients received Ezetimibe or a PCSK9 inhibitor. Statin intensity was inversely associated with LDL-C level at index date (Figure 1). Other demographic and clinical patient characteristics are detailed in Table 1.
Table 1.
Characteristics of patients with atherosclerotic cardiovascular disease by lipid lowering therapya
| Characteristic | All | No lipid lowering therapy | Low Intensity | Moderate Intensity | High intensity | Ezetemibe or PCSK-9 inhibitor (with or without statin)* |
|---|---|---|---|---|---|---|
| 24,651 | 14,387 | 1,283 | 5,624 | 3,190 | 364 | |
| Female No (%) | 11,949 (48%) | 7,298 (51%) | 694 (54%) | 2,645 (47%) | 1,232 (39%) | 161 (44%) |
| Race/ethnicity | ||||||
| NHW | 15,295 (62%) | 8,810 (61%) | 744 (58%) | 3,520 (63%) | 2,111 (66%) | 244 (67%) |
| Asian | 3,263 (13%) | 1,704 (12%) | 242 (19%) | 896 (16%) | 411 (13%) | 23 (6%) |
| Hispanic | 1,293 (5%) | 746 (5%) | 73 (6%) | 284 (5%) | 180 (6%) | 21 (6%) |
| Black | 307 (1%) | 171 (1%) | 10 (1%) | 68 (1%) | 54 (2%) | 7 (2%) |
| Other | 4,493 (18%) | 2,856 (21%) | 214 (17%) | 856 (15%) | 434 (14%) | 69 (19%) |
| ASCVD type | ||||||
| CAD | 14,765 (60%) | 8,102 (56%) | 641 (50%) | 3,518 (63%) | 2,367 (74%) | 302 (83%) |
| Stroke | 10,779 (44%) | 6,591 (46%) | 612 (48%) | 2,352 (42%) | 1,167 (37%) | 122 (34%) |
| PAD | 3,951 (37%) | 2,349 (16%) | 237 (18%) | 876 (16%) | 468 (15%) | 48 (14%) |
| Polyvascular | 4,384 (18%) | 2,398 (17%) | 192 (15%) | 1,023 (39%) | 729 (23%) | 95 (26%) |
| Clinical comorbidities | ||||||
| Hypertension | 16,804 (68%) | 9,634 (67%) | 851 (66%) | 3,903 (69%) | 2,295 (72%) | 267 (73%) |
| Dementia | 2,385 (10%) | 1,593 (11%) | 123 (10%) | 319 (9%) | 186 (6%) | 14 (4%) |
| Diabetes | 6,338 (26%) | 3,384 (24%) | 347 (27%) | 1,590 (28%) | 974 (31%) | 94 (26%) |
| Heart failure | 4,520 (18%) | 2,835 (20%) | 212 (17%) | 907 (16%) | 537 (17%) | 51 (14%) |
| Malignancy | 6,870 (28%) | 3,874 (27%) | 410 (32%) | 1,652 (29%) | 883 (28%) | 96 (26%) |
| Renal disease | 7,223 (46%) | 4,113 (29%) | 417 (33%) | 1,654 (31%) | 988 (31%) | 101 (28%) |
| Current smokers | 519 (2%) | 286 (2%) | 24 (2%) | 119 (2%) | 80 (2%) | 8 (2%) |
| Laboratory values | ||||||
| T chol, mean (SD)b | 161 (41) | 171 (45) | 162 (37) | 153 (34) | 149 (35) | 162 (44) |
| LDL, mean (SD)c | 81 (35) | 91 (39) | 80 (30) | 73 (28) | 71 (29) | 83 (39) |
| LDL, % ≥70mg/dLc | 7,544 (57%) | 3,757 (68%) | 571 (60%) | 2,049 (49%) | 1,088 (46%) | 145 (56%) |
| Polypharmacy | 11,308 (46%) | 5,962 (41%) | 676 (53%) | 2,872 (51%) | 1,704 (53%) | 191 (53%) |
| Other characteristicsd | ||||||
| -BMI, mean (SD) | 26 (5) | 26 (5) | 26 (5) | 27 (5) | 27 (5) | 27 (4.7) |
| -%Underweight | 780 (4%) | 551 (4%) | 32 (3%) | 136 (3%) | 55 (2%) | 10 (3%) |
| -%Normal weight | 8,837 (40%) | 5,266 (42%) | 520 (44%) | 2,009 (38%) | 1,001 (33%) | 94 (27%) |
| -%Overweight | 8,243 (37%) | 4,404 (35%) | 439 (37%) | 2,058 (39%) | 1,271 (41%) | 152 (44%) |
| -%Obese | 4,311 (19%) | 2,221 (18%) | 200 (17%) | 1,097 (21%) | 754 (24%) | 93 (27%) |
Summary statistics are based on the last patient-year, which was used in the main analysis presented in Table 2.
Data available for 13,182 patients;
Data available for 13,132 patients;
Data available for 22,171 patients
Abbreviations and definitions: NHW, non-Hispanic white; ASCVD, atherosclerotic cardiovascular disease; CAD, coronary artery disease; PAD, peripheral artery disease; T chol, total cholesterol; SD, standard deviation; LDL, low-density lipoprotein; polypharmacy, >9 prescription medications; BMI, body mass index.
Figure 1. LDL-C levels by statin intensity.
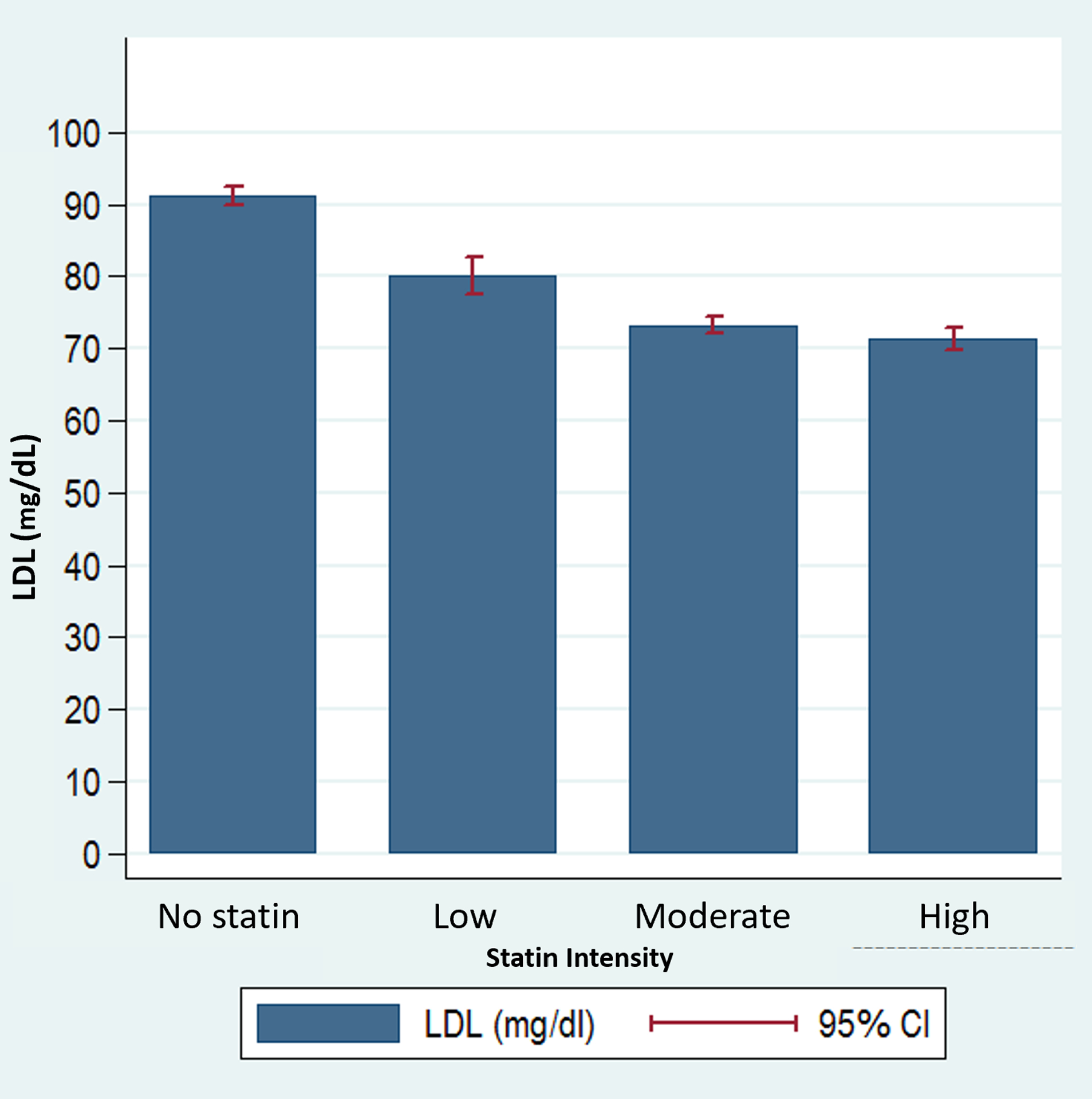
LDL-C level is negatively correlated with statin intensity. 95% confidence intervals are provided by the error bands. Abbreviations and definitions: LDL, low-density lipoprotein; CI, confidence interval.
Prescriptions of moderate/high intensity statins for secondary ASCVD prevention increased over time; 35% of adults over 75 received moderate/high intensity statins in 2007 versus 45% in 2018. Statin prescription rates remained significantly lower for patients >75 years old as compared with those 65–75 years old (OR: 0.87, [95% CI: 0.85, 0.89]) (Figure 2).
Figure 2. Time trend of moderate to high intensity statin prescription, by age group.
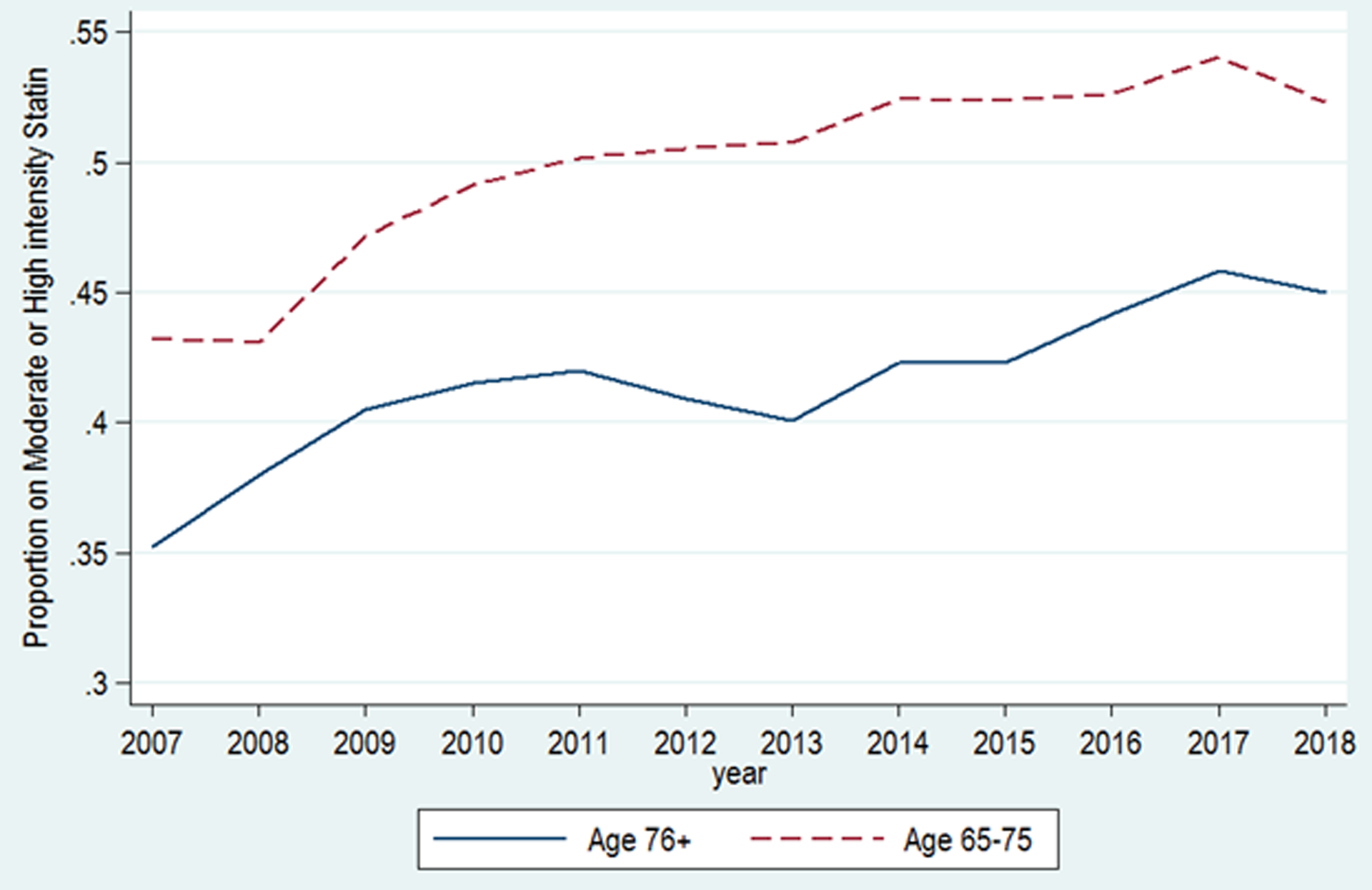
Guideline-concordant statin prescription has increased over time but remains low, particularly in older adults.
Among those >75 years old, patients with CAD only, women (OR: 0.77, [95% CI: 0.74, 0.80]), patients with heart failure (OR: 0.69, [95% CI: 0.65, 0.74]), dementia (OR: 0.88, [95% CI: 0.82, 0.95]) or who were underweight (OR: 0.64, [95% CI: 0.57, 0.73]) were less likely to receive moderate/high intensity statins (Table 2). Asian patients were more likely to receive moderate/high intensity statins than NHW (OR: 1.20, [95% CI: 1.14, 1.26]) as were patients with polypharmacy (>9 prescription medications) (OR: 1.28, [95% CI: 1.23, 1.33]). Patients with CAD were less likely to receive moderate/high intensity statins than patients with other forms of ASCVD (Table 2).
DISCUSSION
In a large contemporary cohort of multiethnic older adults receiving regular care in Northern California, we found that while statin prescriptions increased over time from 2007 to 2018, fewer than half were prescribed moderate/high intensity statins in 2018. Being female, underweight or having CAD, dementia, or heart failure were associated with lower prescription rates of moderate/high intensity statins. In contrast, being Asian, having diabetes, hypertension and more prescription medications were associated with higher prescription rates of moderate/high intensity statins. These findings may have implications for future efforts to optimize guideline-recommended statin use among older adults with ASCVD.
Statins have shown efficacy and safety across the age spectrum of ASCVD patients. A pre-specified secondary analysis from the Improved Reduction of Outcomes: Vytorin Efficacy International Trial (IMPROVE-IT) trial showed that simvastatin and ezetimibe resulted in an 8.7% absolute risk reduction in the composite outcome of cardiovascular death, nonfatal myocardial infarction, unstable angina leading to hospitalization, coronary revascularization after 30 days, or stroke in adults over 75 compared to simvastatin alone. The investigators documented a statistically significant interaction between age category and treatment effect (NNT=11 in adults >75).11 However, a meta-analysis of secondary cardiovascular preventions in the older adults found only four trials that included exclusively people aged 65 years or older. An additional eight trials included age-specific subgroup data on secondary prevention with statins.6 A population-based study of the French National Healthcare database found that de-prescribing statins for primary prevention of CVD at age 75 was associated with a 33% increase in hospital admissions for cardiovascular events.12 Our study documented suboptimal rates of moderate/high intensity prescription throughout the study period, though these increased over time, likely reflecting overall increase in population trends13 and increasing awareness of the safety and efficacy of statins in older adults, including perhaps in the context of the 2013 US multi-society cholesterol guidelines.
Older adults make up two-thirds of ASCVD deaths in the US.3 Identifying gaps in contemporary prescribing patterns is key to formulating strategies to bridge prevalent gaps and optimize ASCVD outcomes in this high-risk population. Our findings are consistent with and complementary to prior studies that have identified low high intensity statin prescription rates.14,15 Of note, the rates of statin prescription in this study population of patients who had regular access to medical care may be higher than those in the general population. Prior studies have also reported a treatment-risk paradox; older adults, with the highest risk for cardiovascular events, are less likely to receive appropriate statin therapy.16–18 For example, a study of veterans with severe hypercholesterolemia (without ASCVD), showed they were less likely to be on statin therapy than their middle-aged counterparts.19 However, another registry-based study in Belgium documented higher prescription rates in adults 60–79 years old than those 50–59 years old with a declining trend at more extreme older age (80 years and older).20
Ezetimibe and PCSK9 inhibitor prescriptions were low as in prior studies.15 We note, however, that PSCK9 inhibitors were not FDA approved until 2015 (9 years into the 12-year study period) and were not present in the 2013 multi-society guidelines. Similarly, ezetimibe did not become generic until the end of 2016 and the 2013 multi-society guidelines recommended administration to patients with suboptimal statin response in patients less than 75 years old with clinical ASCVD.9 Practice patterns have likely continued to evolve after the publication of the IMPROVE-IT trial in 2019 and the release of the 2018 multi-society guidelines.
In addition to overall statin under-use, we found that certain patient groups were less likely to receive guideline-directed statins. Women and patients with certain comorbidities (underweight, dementia, and heart failure) were less likely to receive statins. Similar to our findings, Zullo et al. found that under-prescription of secondary prevention medications following a myocardial infarction was associated with older age and female sex.5 Markers of frailty, dementia and underweight were associated with lower rates of moderate/high intensity statins in our study; “do not resuscitate” orders, poor physical functioning, and cognitive impairment have had similar associations in prior studies.5 Lower rates of statin prescription in women have been consistently reported in contemporary analyses.16,18,20 The lower rates of statin prescription for patients with heart failure may reflect the uncertainty about the benefit of statins in patients with heart failure with reduced ejection fraction.21–23
Our study differs from prior studies in that patients with CAD were less likely to receive statin therapy than those with other forms of ASCVD.19,24 One hypothesis for this surprising result is that older adults with CVD or PAD are diagnosed later in their course when statins are more consistently used as part of intensive disease-modifying therapy. Examples include diagnosis after developing advanced signs/symptoms requiring specialist referral or after acute hospitalizations. A second hypothesis is that in older patients undergoing evaluation for common, stable symptoms such as shortness of breath, CAD diagnoses may be entered in EHRs as part of their workup (such as coding for stress tests). Especially in the setting of comorbidities, however, these older adults may not ultimately receive statins based on perceived clinical stability, non-severe or equivocal test results, and/or risk-benefit discussions. Future studies may explore whether the specialty of the clinician (e.g. primary care, cardiology, neurology, vascular surgery) influences prescription rates by indication.
Interestingly, despite reported increased sensitivity to lower doses of certain statins in certain Asian population and recommendations for slower up-titration of statin intensity in this group,8 Asians had higher odds or receiving moderate/high intensity statins. While Japanese patients may have increased sensitivity to statin therapy, South Asian patients are considered to be at high cardiovascular risk.8 Therefore, disaggregated data by Asian subgroup in future studies may provide insight into this finding.
Prescribing statins for older adults requires special considerations which include polypharmacy, multimorbidity, and higher likelihood of frailty and advanced incurable disease.25–27 Polypharmacy was associated with increased moderate/high statin prescriptions. Possible reasons for this finding include that polypharmacy is an indirect measure of comorbidity and, per our findings, patients with certain comorbidities, such as diabetes and hypertension were more likely to receive statins. Alternatively, polypharmacy may be a marker of tolerability where patients that are able to tolerate multiple medications are also able to tolerate statins. It is noteworthy that the median number of prescriptions in our study cohort was 9. While this is likely reflective of a population more connected to healthcare, in prior studies, polypharmacy and a complex medication burden have been associated with poor medication adherence.28 Importantly, despite public concern, recent analyses have failed to identify associations between statin therapy and increased adverse effects or cognitive decline in older adults.7,27,29 Indeed, the body of evidence appears to support relative safety to statin therapy and possible increased mortality after statin discontinuation in older adults. Measuring and reporting measures like quality of life, frailty, and burden of treatment (the workload of healthcare and how it impacts patients’ functioning and well-being) may help guideline panelists, patients, and clinicians individualize statin therapy for older adults.28,30,31
Our findings should be interpreted in the context of several limitations. Our cohort included insured patients who had regular care in a health system in Northern California, thereby limiting the generalizability of our findings to other contexts, including to patients without a regular source of care or those in different geographic regions. The prevalence of dementia may be underestimated in our cohort as physicians and patients may tend to underreport cognitive impairment.32,33 Our study period does not examine the impact of the 2018 US multi-society cholesterol guidelines on statin prescription, although it includes the 2013 US multi-society guidelines which recommend moderate intensity statin use in adults with ASCVD over 75 years of age. Our data does not differentiate between de novo high intensity statin prescriptions and statin intensification (changes from low intensity to moderate/high intensity statins). Cross-sectional laboratory values obtained from the EHR may not reflect longitudinal averages. We were unable to ascertain reasons for statin nonprescription which may have included patient preferences and/or side-effects due to limitations in EHR data. Similarly, we did not include direct measures of patients’ mobility and functional status, which may influence statin prescriptions. However, we also describe use of non-statin therapies for LDL-C lowering including ezetimibe and PCSK-9 inhibitors.
In a large multiethnic, real-world population of older adults (greater than 75 years of age) with ASCVD, we found increasing rates of moderate/high intensity prescription from 2007 through 2018 but that less than half of patients were prescribed guideline-recommended statin therapy in 2018. Patients with ASCVD over > 75 years of age were consistently less likely to receive moderate/high intensity statin therapy compared to those 65 to 75 years of age. Future studies will need to unpack reasons for statin under-prescription and generate evidence tailored to improving guideline-recommended statin use in the growing population of older adults with ASCVD.
Supplementary Material
Supplementary Table. International Classification of Diseases for ASCVD and co-morbidities.
ACKNOWLEDGEMENTS
Sponsor’s Role
Dr. Rodriguez was funded by a grant from the National Heart, Lung, and Blood Institute, NIH (1K01HL144607) and Stanford Aging & Ethnogeriatrics Transdisciplinary Collaborative Center (SAGE) funded by the National Institute on Aging (P30AG059307). Dr. Chung and Dr. Palaniappan were funded by grants from the National Heart, Lung, and Blood Institute (1R01HL126172-01A1, K24 HL150476-01A1).
Footnotes
Conflict of Interest
The authors declare no relevant disclosures or competing interests.
REFERENCES
- 1.Roberts AW, Ogunwole SU, Blakeslee L, Rabe MA. The population 65 years and older in the United States: 2016. Am Community Surv Reports. Published online 2018:ACS–38. [Google Scholar]
- 2.Benjamin EJ, Muntner P, Alonso A, Bittencourt MS, Callaway CW, Carson AP, et al. Heart Disease and Stroke Statistics-2019 Update: A Report From the American Heart Association. Vol 139.; 2019. doi: 10.1161/CIR.0000000000000659 [DOI] [PubMed] [Google Scholar]
- 3.Mozaffarian D, Benjamin E, Go A, Arnett D, Blaha M, Cushman M, et al. Heart disease and stroke statistics—2016 update: a report from the American Heart Association. Circulation. 2016;133(4):e38–e360. www.heart.org/statistics [DOI] [PubMed] [Google Scholar]
- 4.Ruscica M, Macchi C, Pavanello C, Corsini A, Sahebkar A, Sirtori CR. Appropriateness of statin prescription in the elderly. Eur J Intern Med. Published online 2018. doi: 10.1016/j.ejim.2017.12.011 [DOI] [PubMed] [Google Scholar]
- 5.Zullo AR, Sharmin S, Lee Y, Daiello LA, Shah NR, John Boscardin W, et al. Secondary Prevention Medication Use After Myocardial Infarction in U.S. Nursing Home Residents. J Am Geriatr Soc. Published online 2017. doi: 10.1111/jgs.15144 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ponce OJ, Larrea-Mantilla L, Hemmingsen B, Serrano V, Rodriguez-Gutierrez R, Spencer-Bonilla G, et al. Lipid-Lowering Agents in Older Individuals: A Systematic Review and Meta-Analysis of Randomized Clinical Trials. J Clin Endocrinol Metab. 2019;104(5). doi: 10.1210/jc.2019-00195 [DOI] [PubMed] [Google Scholar]
- 7.Armitage J, Baigent C, Barnes E, Betteridge DJ, Blackwell L, Blazing M, et al. Efficacy and safety of statin therapy in older people: a meta-analysis of individual participant data from 28 randomised controlled trials. Lancet. Published online 2019. doi: 10.1016/S0140-6736(18)31942-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Grundy SM, Stone NJ, Bailey AL, Beam C, Birtcher KK, Blumenthal RS, et al. 2018. AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA Guideline on the Management of Blood Cholesterol. J Am Coll Cardiol. 10.1016/j.jacc.2018.11.003 [DOI] [Google Scholar]
- 9.Stone NJ, Robinson JG, Lichtenstein AH, Bairey Merz CN, Blum CB, Eckel RH, Goldberg AC, Gordon D, Levy D, Lloyd-Jones DM, McBride P, Schwartz JS, Shero ST, Smith SC Jr, Watson KWP. 2013. ACC/AHA Guideline on the Treatment of Blood Cholesterol to Reduce Atherosclerotic Cardiovascular Risk in Adults A Report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. Published online 2014:63853. doi: 10.1161/01.cir.0000437738.63853.7a [DOI] [PubMed] [Google Scholar]
- 10.Wong EC, Palaniappan LP, Lauderdale DS, Care SM, June N, Wong EC, et al. Using Name Lists to Infer Asian Racial / Ethnic Subgroups in the Healthcare Setting. Med Care. 2020;48(6):540–546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bach RG, Cannon CP, Giugliano RP, White JA, Lokhnygina Y, Bohula EA, et al. Effect of Simvastatin-Ezetimibe Compared With Simvastatin Monotherapy After Acute Coronary Syndrome Among Patients 75 Years or Older. JAMA Cardiol. Published online 2019. doi: 10.1001/jamacardio.2019.2306 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Giral P, Neumann A, Weill A, Coste J. Cardiovascular effect of discontinuing statins for primary prevention at the age of 75 years: a nationwide population-based cohort study in France. Eur Heart J. Published online 2019:3516–3525. doi: 10.1093/eurheartj/ehz458 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bin Abdulhak AA, Vaughan-Sarrzin M, Kaboli P, Horwitz PA, Mosher H, Sigurdsson G, et al. Temporal Trends of High-Intensity Statin Therapy Among Veterans Treated With Percutaneous Coronary Intervention. J Am Heart Assoc. 2018;7(5):1–7. doi: 10.1161/JAHA.117.007370 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Chamberlain AM, Cohen SS, Killian JM, Monda KL, Weston SA, Okerson T. Lipid-Lowering Prescription Patterns in Patients With Diabetes Mellitus or Cardiovascular Disease. Am J Cardiol. 2019;124(7):995–1001. doi: 10.1016/j.amjcard.2019.07.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sidebottom AC, Vacquier MC, Jensen JC, Bradley SM, Knickelbine T, Strauss C, et al. Trends in prevalence of guideline-based use of lipid-lowering therapy in a large health system. Clin Cardiol. 2020;43(6):560–567. doi: 10.1002/clc.23347 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Van Peet PG, Gussekloo J, Den Elzen WPJ, Blom JW, De Waal MWM, De Ruijter W. Drug prescription rates in secondary cardiovascular prevention in old age: Do vulnerability and severity of the history of cardiovascular disease matter? Scand J Prim Health Care. 2015;33(4):260–268. doi: 10.3109/02813432.2015.1117281 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ko DT, Mamdani M, Alter DA. Lipid-Lowering Therapy with Statins in High-Risk Elderly Patients: The Treatment-Risk Paradox. J Am Med Assoc. Published online 2004. doi: 10.1001/jama.291.15.1864 [DOI] [PubMed] [Google Scholar]
- 18.Rodriguez F, Knowles JW, Maron DJ, Virani SS, Heidenreich PA. Frequency of Statin Use in Patients With Low-Density Lipoprotein Cholesterol ≥190 mg/dl from the Veterans Affairs Health System. Am J Cardiol. Published online 2018. doi: 10.1016/j.amjcard.2018.05.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Rodriguez F, Lin S, Maron DJ, Knowles JW, Virani SS, Heidenreich PA. Use of high-intensity statins for patients with atherosclerotic cardiovascular disease in the Veterans Affairs Health System: Practice impact of the new cholesterol guidelines. Am Heart J. Published online 2016. doi: 10.1016/j.ahj.2016.09.007 [DOI] [PubMed] [Google Scholar]
- 20.Laleman N, Henrard S, Van Den Akker M, Goderis G, Buntinx F, Van Pottelbergh G, et al. Time trends in statin use and incidence of recurrent cardiovascular events in secondary prevention between 1999 and 2013: A registry-based study 11 Medical and Health Sciences 1117 Public Health and Health Services. BMC Cardiovasc Disord. 2018;18(1):1–13. doi: 10.1186/s12872-018-0941-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Al-Gobari M, Le HH, Fall M, Gueyffier F, Burnand B. No benefits of statins for sudden cardiac death prevention in patients with heart failure and reduced ejection fraction: A meta-analysis of randomized controlled trials. PLoS One. 2017;12(2):1–24. doi: 10.1371/journal.pone.0171168 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.GISSI-HF investigators. Effect of rosuvastatin in patients with chronic heart failure (the GISSI-HF trial): a randomised, double-blind, placebo-controlled trial. Lancet. 2008;372(9645):1231–1239. doi: 10.1016/S0140-6736(08)61240-4 [DOI] [PubMed] [Google Scholar]
- 23.Kjekshus J, Apetrei E, Barrios V, Böhm M, Cleland JGF, Cornel JH, et al. Rosuvastatin in older patients with systolic heart failure. N Engl J Med. 2007;357(22):2248–2261. doi: 10.1056/NEJMoa0706201 [DOI] [PubMed] [Google Scholar]
- 24.McBride CL, Akeroyd JM, Ramsey DJ, Nambi V, Nasir K, Michos ED, et al. Statin prescription rates and their facility-level variation in patients with peripheral artery disease and ischemic cerebrovascular disease: Insights from the Department of Veterans Affairs. Vasc Med (United Kingdom). Published online 2018. doi: 10.1177/1358863X18758914 [DOI] [PubMed] [Google Scholar]
- 25.Musich S, Wang SS, Schwebke K, Slindee L, Waters E, Yeh CS. Underutilization of Statin Therapy for Secondary Prevention of Cardiovascular Disease Among Older Adults. Popul Health Manag. 2019;22(1):74–82. doi: 10.1089/pop.2018.0051 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ofori-Asenso R, Jakhu A, Zomer E, Curtis AJ, Korhonen MJ, Nelson M, et al. Adherence and Persistence among Statin Users Aged 65 Years and Over: A Systematic Review and Meta-analysis. Journals Gerontol - Ser A Biol Sci Med Sci. Published online 2018. doi: 10.1093/gerona/glx169 [DOI] [PubMed] [Google Scholar]
- 27.Strandberg TE, Kolehmainen L, Vuorio A. Evaluation and treatment of older patients with hypercholesterolemia: A clinical review. JAMA - J Am Med Assoc. 2014;312(11):1136–1144. doi: 10.1001/jama.2014.10924 [DOI] [PubMed] [Google Scholar]
- 28.Eton DT, Yost KJ, Lai J shei, Ridgeway JL, Egginton JS, Rosedahl JK, et al. Development and validation of the Patient Experience with Treatment and Self-management (PETS): a patient-reported measure of treatment burden. Qual Life Res. Published online 2017. doi: 10.1007/s11136-016-1397-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Samaras K, Makkar SR, Crawford JD, Kochan NA, Slavin MJ, Wen W, et al. Effects of Statins on Memory, Cognition, and Brain Volume in the Elderly. J Am Coll Cardiol. 2019;74(21):2554–2568. doi: 10.1016/j.jacc.2019.09.041 [DOI] [PubMed] [Google Scholar]
- 30.Spencer-Bonilla G, Quiñones AR, Montori VM. Assessing the Burden of Treatment. J Gen Intern Med. 2017;32(10). doi: 10.1007/s11606-017-4117-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Tran VT, Harrington M, Montori VM, Barnes C, Wicks P, Ravaud P. Adaptation and validation of the Treatment Burden Questionnaire (TBQ) in English using an internet platform. BMC Med. Published online 2014. doi: 10.1186/1741-7015-12-109 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Goebeler S, Jylhä M, Hervonen A. Self-reported medical history and self-rated health at age 90. Agreement with medical records. Aging Clin Exp Res. Published online 2007. doi: 10.1007/BF03324692 [DOI] [PubMed] [Google Scholar]
- 33.Crowther GJE, Bennett MI, Holmes JD. How well are the diagnosis and symptoms of dementia recorded in older patients admitted to hospital? Age Ageing. Published online 2017. doi: 10.1093/ageing/afw169 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Table. International Classification of Diseases for ASCVD and co-morbidities.


