Abstract
Background:
Tools and systems to improve mental health have been understudied in low-resource environments, such as sub-Saharan Africa. This study explores depression amongst women participating in a community-based intervention combining savings- and lending-groups, entrepreneurial training and other skills training.
Aims:
This study aims to determine whether depression decreases with more program participation, and the extent to which social capital variables may explain these changes.
Method:
Survey data were gathered in June 2018, within 6 months of group formation, and again in June 2019 from 400 women participants in the program. Data between 2018 and 2019 were compared using Wilcoxon rank-sum and Chi square tests. Inferential statistics included random effects regression models and general structural equation models.
Results:
At 1-year follow-up, depression and loneliness amongst Kenyan women (n = 400) participating in the program had decreased. Social capital remained higher within groups than within the broader community, and mediated the association between program participation and decreased depression.
Conclusions:
Findings suggest this novel, community-based intervention has the potential to benefit mental health. Future research, including a randomised control trial, is required to establish (1) the extent of the program’s benefits and (2) the program’s application to particular subject areas and population segments.
Keywords: Depression, social capital, community-based intervention, Kenya, Women
Background
Depression affects over 4% of the global population with higher burden in sub-Saharan Africa compared to other World Health Organization regions (World Health Organization, 2017). Depression prevalence data from Kenyan rural community samples are largely non-existent, with most studies targeting population segments – for example, people with HIV, adolescents, etc. (Kingori et al., 2015; Osborn et al., 2020). Individuals with depression have 60% higher all-cause mortality risk, and heightened risk for many comorbid conditions (Chesney et al., 2014; Grote et al., 2010).
Recent studies show microfinance groups produce social capital (Sanyal, 2009). A multifaceted concept, social capital includes dimensions of civic engagement, collective action, social cohesion, trust, and accessible social resources (Siisiainen, 2003). Higher individual cognitive social capital (ICSC) – mental frameworks positing the accessibility of social resources, typically represented as trust, group cohesion and expectations of mutual support – is consistently associated with lower depression (Ehsan & De Silva, 2015; Islam et al., 2006). Higher ICSC facilitates the exchange of social support, strengthening stress coping mechanisms (Ehsan & De Silva, 2015). ICSC enables collective action to produce collectively desirable ends (Author own, 2020). Increasing ICSC may protect against mental health disorders and significantly improve communities’ capacity to resist extreme challenges such as poverty and environmental changes (Ehsan & De Silva, 2015). Loneliness, the painful sense of social disconnection, predicts depression (Hawkley & Cacioppo, 2010). Thus, loneliness may mediate relationships between ICSC and depression.
Interventions to build social capital have been designed to promote education, public health, and community-driven development (Sommer et al., 2017; Villalonga-Olives et al., 2018). Though high levels of ICSC within a community are positively associated with mental health, there have been few social capital-based interventions targeting the improvement of mental health (Flores et al., 2018). This study presents cohort data from women participating in a Kenyan community-based program with elements previously identified as improving ICSC (i.e. trust, mutual support and cohesion).
Kuja Pamoja/Come Together Intervention
Kuja Pamoja (KPJ), Swahili for ‘Come Together’, is a community-based intervention aiming to improve family capacity to care for children in semi-rural Kenya. Outcomes of interest for the intervention include psychological and psychosocial well-being and social capital. At the heart of the intervention is an internal-lending microfinance approach.
Group lending interventions have recently been analysed as social functions (Sanyal, 2009; Wydick, 2001). The KPJ program relies on group members providing loans to each other at weekly meetings. Group lending programs can increase ICSC, for example, trust, information flow, and mutual willingness to help one another by expanding social networks and familiarity (Feigenberg et al., 2010; Pronyk et al., 2008; Sanyal, 2009).
The present intervention was developed by a non-governmental organisation, Sodzo International, to strengthen Kenyan families of children who are reintegrating from the streets and to improve community capacity to care for families with children at risk of moving to the streets (Goodman et al., 2020). Families form groups of 25–30 and collectively determine the amount of weekly contribution for group members, repayment terms and lending conditions. Families undergo 2 weeks of training before group formation, during which paid social workers educate families on the lending process. Each group joins the program by deciding upon a name and agreeing to abide by the pillars of the program – love, transparency and trust. Typically, families bring $0.20 each week to loan to other members of their respective group at 10% interest, which is recorded in a shared ledger filled by literate group members. All positions in the group rotate weekly, including the group facilitator and record keeper, amongst interested group members. The program began in February 2017 with a group of 30 families and had grown to over 4200 families across 17 village locations by July 2019. Recruitment to the program begins with a family of a child who has lived on the streets and who is currently being served by Sodzo International’s centre for children who formerly lived on the streets. After establishing a presence in the village through the first family, all other program recruitment occurs through word of mouth. The program seeks to serve families in the community who are the most vulnerable. After groups have been functioning for 6 months, they are invited to join village-level resource committees representing the interests of other groups in the village.
Study aim
This study aims to determine whether depression improves amongst a cohort of randomly selected female participants in the KPJ intervention between Time 1 (T1) and Time 1 (T2). Further, the study aims to determine whether frequency of attendance at weekly meetings predicts improvements in depression, and whether this association is mediated by ICSC and loneliness.
Methods
Study design
A 1-year cohort design without control group was chosen due to financial limitations.
Sample selection
Study participants were selected through a multistage process. Program participants were randomly selected from the first five village locations where the KPJ intervention began in Meru County, Kenya. The intervention targeted home villages of children who were transitioning back from life on the streets. We believe these villages were typical for the area, though perhaps more disadvantaged since their children were first identified on the streets. All groups in each selected village were eligible for interview. All willing participants drew a piece of paper from an opaque bag indicating whether they had been selected. Seven group members were selected from each group. A total of 470 women were selected for interview in June 2018, of whom 5% refused and were replaced by women participating in the program chosen through another round of random selection. Program participants had been enrolled for a median 8 months, with a range 0 to 16 months, when the first questionnaire was administered.
Survey respondents were re-interviewed in June 2019 (N = 400). Of those originally interviewed, 2.6% were absent on interview days but otherwise still participating in the program, 2.6% were away on maternity leave, 7.2% had dropped from the program, and 1% had either moved away, died or become terminally ill.
Program setting
The program operates throughout three sub-counties of Meru County, Kenya. These sub-counties are generally rural with townships ranging in population size from 5000 to 50,000. The typically longer seasonal rains (March-May) were much later and lower volume in 2019 than previous years, affecting food security across the village (Holland, 2019). Groups meet weekly in public spaces of villages or townships across the village at an established time; study interviews were conducted in these public spaces.
Measures
Survey measures included validated scales pertinent to study constructs and utilised in other diverse cultural contexts. Local female interviewers administered the survey in the local language – Kimeru. Questionnaires were created in English, translated into Kimeru and back translated for refinement and validation.
Outcome variables.
Depression is a mood disorder accompanied by persistent feelings of sadness, emptiness, irritability, somatic and cognitive changes affecting one’s capacity to function (American Psychiatric Association, 2013). Depression was measured at T1 and T2 using the 21-item Beck’s Depression Inventory-II (BDI-II; Beck et al., 1996; α = 0.83 in 2018; α = 0.80 in 2019). The BDI-II has been used in several countries in Sub-Saharan Africa (including Kenya) (Bernard et al., 2017), and a Swahili version of the scale demonstrated a Cronbach’s alpha of 0.89 and strong correlation with locally identified symptoms of depression (Abubakar et al., 2016).
Mediation variables.
Individual cognitive social capital (ICSC) was measured using multiple items to assess different aspects of the construct: trust, expectation of mutual support, and entitativity (c.f. Islam et al., 2006; Murayama et al., 2012). Trust was measured at T1 and T2 using the single question ‘generally speaking, would you say most people can be trusted or you cannot be too careful in dealing with people’ (Knack & Keefer, 1997). This item was also adapted to refer specifically to ‘members of your KPJ group.’ Trust was measured for both categories of people – the general population and members of the KPJ group. For trust measures, ‘1’ indicated the presence of trust and ‘0’ represented its absence. Expectation of mutual support was measured at T1 and T2 using one item for the general population and another item for fellow group members in the KPJ program. The question was taken from Poortinga (2006), and read ‘this area is a place where neighbours look after each other.’ This item was modified to measure the presence of support within the KPJ groups by rephrasing the question ‘my KPJ group is a place where members look after each other.’ Responses to these items were recorded on a 6-point Likert-type scale with higher responses indicating stronger agreement. Entitativity was measured only in 2019 using the Group Entitativity Measure (GEM; Gaertner & Schopler, 1998). The GEM is a one-item visual analogue scale assessing members’ perception of group cohesiveness, or the sense of being a single entity rather than separate individuals. The scale contains six diagrams with five circles (one representing self and the four surrounding circles representing the other group members) moving closer to one another as the diagrams progress from 1–6. Participants are instructed to choose the one best representing their perception of the group. Higher numbers on the scale indicate a greater sense of group cohesion.
Loneliness was measured at T1 and T2 using the Three-Item Loneliness Scale developed by Hughes et al. (2004). The three-item scale includes the questions ‘how often do you feel that you lack companionship?’, ‘how often to you feel left out?’, and ‘how often do you feel isolated from others?’, and is measured on a three-point Likert scale. The internal reliability of the loneliness scale was acceptable for the 2018 and 2019 surveys (Cronbach’s α = 0.53 and 0.64, respectively; Spearman-Brown prediction coefficient = 0.89 and 0.92, respectively). The Three-Item Loneliness scale has reliably been used in various cultures and languages (Rico-Uribe et al., 2016).
Additionally, time (months) in group at baseline and cash borrowed from group in past 6 months (at follow-up) were assessed as potential mediators but not used in the final model due to non- significance.
Exposure variables.
Attendance was recorded using a single self-report item ‘in the past 6 months, how often would you say you attended your group meetings?’ Responses were coded ‘every week’ versus less than every week (i.e. ‘a few times each month, but miss sometimes,’ ‘about half the meetings,’ ‘only a few meetings,’ and ‘almost never’).
Control variables.
Control variables were factors known to be associated with depression – wealth, education and age (Patel et al., 2018). Wealth was measured using a common household good index of household assets – electricity, radio, television, wristwatch, computer, refrigerator, bicycle, motorcycle, car and land (Morris et al., 2000). Age was recorded as years of life completed, and education was recorded as the number of formal school years completed.
All control variables were recorded through respondent self-report and were used as continuous variables.
Data analysis
Bivariate analyses were used to compare outcome and mediating variables between 2018 and 2019, except entitativity which was recorded only in 2019. Wilcoxon signed-rank tests and McNemar’s Chi square tests were used to determine statistical differences between 2018 and 2019 data (α = 0.05).
Random effects regression models were fit to assess the effects of weekly program attendance, ICSC variables (T2), and loneliness (T2) on depression at follow-up. First, depression at follow-up (T2) was regressed on all measures of in-group social capital (group trust, group expectation of mutual support, and entitativity) individually. Secondly, the two significantly associated measures of social capital (in this case, group trust and entitativity) were included in subsequent mediation models. All random effects models account for anticipated group membership and village-level homogeneity.
A generalised structural equation model (GSEM) was calculated to explore potential pathways between weekly attendance and depression (T2). It was hypothesised loneliness (T2) would mediate the ICSC variables (T2) and depression (T2), and that ICSC variables would reflect social benefits of program participation – that is, by proxy through frequency of attendance at group meetings. The order of social capital variables (group trust and entitativity) in the GSEM was determined based on how well each variable explained the association between weekly attendance and the other social capital variable, placing closer to the exposure variable the mediating variable that most reduced the magnitude of association between weekly attendance and the other social capital variable (in this case, entitativity preceding group trust).
All multivariable models controlled for depression and loneliness recorded at T1 (in addition to wealth, age, and education at T2). All statistical analyses were conducted using STATA v.14.2 (College Station, TX).
Compliance with ethical standards
Research involving human participants
The Ethics Committee at Maua Methodist Hospital in Meru County, Kenya, provided ethical review and approval for the study prior to data collection. The Institutional Review Board at the University of Texas Medical Branch determined analysis of program-collected data was exempted from ethical review.
Informed consent.
All respondents were informed their participation in the program was completely independent of their willingness or refusal to participate in the evaluation and all respondents provided informed consent prior to data collection.
Results
Bivariate results are presented in Table 1, below. Depression and loneliness were significantly lower between baseline and follow-up (p < 0.001). There was no significant difference between expectation of mutual support between baseline and follow-up, though at both time-points respondents reported a significantly higher level of expected support and trust within their program groups than within the community at large. There was a significant decline in the percentage of respondents who trusted their group and who trusted the general community at follow-up compared to baseline. The percentage of respondents (1) reporting their group was trustworthy reduced 7.7%, and (2) reporting their broader community was trustworthy reduced 11%, between baseline and follow-up. Seventy-two percent of respondents reported they attended the program every week, while 21.6% of respondents attended most weeks. Just over 6% of respondents came less frequently than most weeks. The average amount of funding received in the prior 6 months was $67.38 (100 Kenyan shillings = 1 US dollar). The average respondent was 42 years old and had finished 4 years of schooling.
Table 1.
Model variables at Time 1 and Time 2.
| Time 1 variables (2018) | Time 2 variables (2019) | p-value | |||||
|---|---|---|---|---|---|---|---|
| Mean (%) | 95% CI | Mean (%) | 95% CI | ||||
| Depression | 1.64 | 1.6 | 1.68 | 1.52 | 1.49 | 1.56 | <.001*** |
| Loneliness | 2.35 | 2.28 | 2.43 | 1.86 | 1.8 | 1.91 | <.001*** |
| Mutual support, general | 4.47 | 4.31 | 4.63 | 4.63 | 4.5 | 4.76 | .38 |
| Mutual support, group | 5.23 | 5.11 | 5.34 | 5.14 | 5.02 | 5.25 | .17 |
| Difference, group - general | 0.76 | 0.6 | 0.91 | 0.51 | 0.38 | 0.64 | .07 |
| p-value, difference | <.001*** | <.001*** | |||||
| Trust, general | 33.90% | 28.30% | 37.60% | 22.90% | 18.70% | 27.00% | <.001*** |
| Trust, group | 62.70% | 57.90% | 67.50% | 55.00% | 50.12% | 59.93% | .02 * |
| Difference, group - general | 29.70% | 24.60% | 34.80% | 32.20% | 27.20% | 37.10% | .64 |
| p-value, difference | <0.001*** | <0.001*** | |||||
| Entitativity (group cohesion) | 5.29 | 5.19 | 5.4 | ||||
| Frequency of attendance | |||||||
| Every week | 72.10% | 67.50% | 76.30% | ||||
| Attend most weeks | 21.60% | 17.80% | 25.90% | ||||
| Half the meetings | 0.80% | 0.20% | 2.30% | ||||
| Only attend a few meetings | 2.80% | 1.50% | 4.90% | ||||
| Almost never | 2.80% | 1.50% | 4.90% | ||||
| Loans received, past 6 months, USD | $67.38 | $61.12 | $73.65 | ||||
| Months participating in program | 7.84 | 7.46 | 8.24 | ||||
| Wealth, index 0–8 | 2.4 | 2.26 | 2.53 | ||||
| Age, years | 42.6 | 41.1 | 44 | ||||
| Years of school completed | 4.09 | 3.76 | 4.42 | ||||
Notes. Data shown for 2018 (baseline) and 2019 (1-year follow-up) interview questionnaires. Depression measured using Beck’s Depression Inventory-II (Beck et al., 1996). Loneliness measured using the three-item adapted UCLA loneliness scale (Hughes et al., 2004). Mutual support and trust were measured using single-item measures adapted for group-level dynamics and community-level dynamics. Entitativity (group cohesion) measured using the Group Entitativity Measure (Gaertner & Schopler, 1998).
Emboldened numerical values signify p<0.05.
p<0.05;
p<0.001.
Table 2, below, shows the outcome of random effects linear regression of depression (T2). Model 1 shows respondents who attend meetings every week have 0.28 standard deviations lower depression than respondents who attend meetings less than every week, controlling for wealth, age, education, baseline depression, and baseline loneliness. Respondents who were more depressed at baseline, had less wealth, and were older reported significantly higher depression at follow-up.
Table 2.
Random effects linear regression model of depression at follow-up (T2).
| Model 1: Exposure | Model 2: Mediation | |||||
|---|---|---|---|---|---|---|
| Coef. | 95% CI | Coef. | 95% CI | |||
| Loneliness, T2, standardised | 0.30 *** | 0.21 | 0.39 | |||
| Group trust, T2 | −0.23* | −0.41 | −0.05 | |||
| Entitativity, T2 | −0.14*** | −0.22 | −0.06 | |||
| 6-month loan total, T2 | 0 | 0 | 0 | |||
| Time in program, T2 | 0.03** | 0.01 | 0.05 | |||
| Attend meetings every week, T2 | −0.28** | −0.5 | −0.07 | −0.2* | −0.4 | 0 |
| Depression, T1, standardised | 0.14** | 0.04 | 0.24 | 0.14** | 0.05 | 0.23 |
| Loneliness, T1, standardised | 0.05 | −0.04 | 0.15 | 0 | −0.08 | 0.1 |
| Wealth index, T2 | −0.l** | −0.18 | −0.03 | −0.05 | −0.12 | 0.01 |
| Age, T2 | 0.01** | 0 | 0.02 | 0.01 * | 0 | 0.01 |
| Education, T2 | 0.01 | −0.03 | 0.04 | −0.01 | −0.04 | 0.03 |
| Constant | −0.03 | −0.53 | 0.4 | 0.67* | 0.05 | 1.3 |
| Regional location, random effect | 0.013 | 0 | 0.35 | 0 | 0 | 0 |
| Group membership, random effect | 0 | 0 | 0 | 0 | 0 | 0 |
| Wald Chi square | 41.21 | 131.81 | ||||
| p-value | <.001 | <.001 | ||||
Notes. Random effects regression models shown for standardised depression at follow-up (T2). The first model shows the antecedent model with only exposure and control variables. The second model includes individual cognitive social capital variables, a measure of total loans received in the past 6 months, and a measure of time in program (months) at baseline. Social capital variables in Table 1 that do not appear in Table 2 were not significantly associated with depression (T2) in bivariate analysis. Depression measured using Beck’s Depression Inventory-II (Beck et al., 1996). Loneliness measured using the three-item adapted UCLA loneliness scale (Hughes et al., 2004). Trust measured using single item measure adapted for group members (Knack & Keefer, 1997). Entitativity (group cohesion) measured using the Group Entitativity Measure (Gaertner & Schopler, 1998).
Emboldened numerical values signify p<0.05.
p<0.05;
p<0.001.
Model 2 in Table 2 depicts the results of including loneliness and the social capital variables (group trust; entitativity) that were associated with depression (T2) in bivariate analysis. A standard deviation increase in loneliness (T2) was associated with a 0.3 standard deviation increase in depression (T2). Respondents who trusted their fellow group members had 0.23 lower standard deviation depression (T2), and for each increase in the 6-point visual analogue scale depicting group entitativity, depression was predicted to decrease 0.13 standard deviations. The amount of loans received in the previous 6 months was not associated with depression (T2), and the time in program was associated with a slight increase in depression (T2); neither variable was included as a mediator in the GSEM. The magnitude of association for weekly attendance and depression (T2) decreased to 0.2 standard deviations after including the social capital variables. The magnitude of associations between depression at baseline and age were not influenced by the inclusion of social capital, though the association between wealth and depression (T2) waned 40% after including social capital variables.
Figure 1 depicts the generalised structural equation model of weekly attendance and depression (T2), controlling for wealth, age, education, depression (T1) and loneliness (T1). Respondents who attended group every week had significantly higher proportional odds of reporting higher group entitativity (pOR: 1.67). Each increase in the group entitativity scale predicted increased odds of reporting group trust by 38%, and decreased T2 loneliness and depression (0.09 sd and 0.13 sd, respectively). Respondents who trusted their groups reported significantly less T2 loneliness and depression (−0.24 sd and −0.23 sd, respectively).
Figure 1.
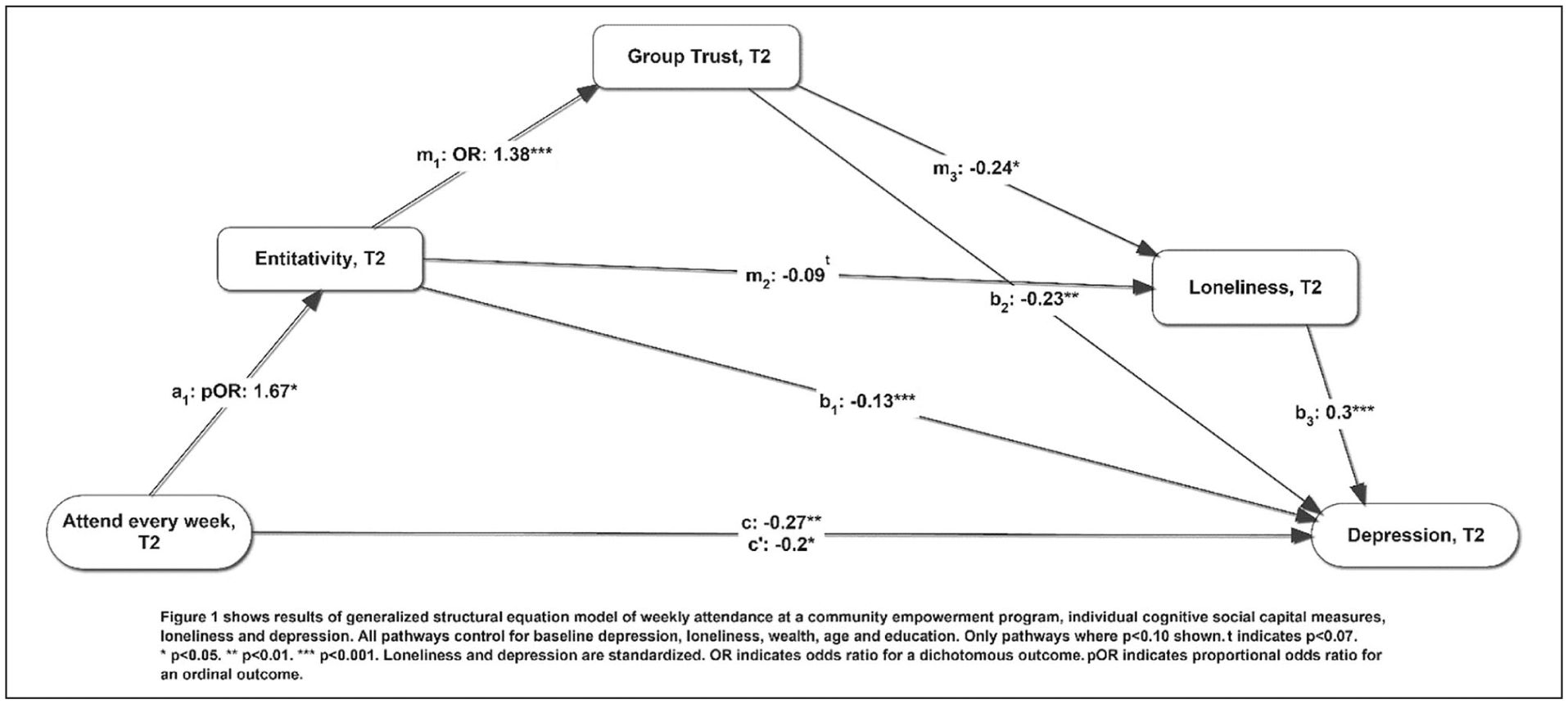
Generalised structural equation model of weekly program attendance and depression at time 2.
Discussion
This study found participation in the Kenyan community-based empowerment program, Kuja Pamoja (Swahili for ‘Come Together’) was linked to significantly lower depression amongst women between baseline in June 2018 and follow-up in June 2019. More frequent participation amongst the women in the program was associated with lower depression at follow-up, even after controlling for baseline depression. More frequent participation in the program was also associated with higher levels of group entitativity (cohesion), trust towards group members, lower levels of loneliness and depression, respectively, in a serial mediation model.
Data show depression and loneliness were significantly lower at follow-up compared to baseline (p < .001).Participants who attended weekly meetings, as opposed to less frequently, reported significantly less depression; 26% of this association that was mediated by social capital variables. Due to study design, we found that women who more regularly attend the KPJ groups experience less depression and that this association is mediated by increased entitativity, trust, and less loneliness cannot be examined in terms of causal mechanisms. However, there is empirical and theoretical evidence supporting our observations as well as potential implications of the observed associations between these constructs.
Weekly attendance and group cohesion
Weekly attendance may have strengthened entitativity through regular expression of shared values, interdependence, and more regular identification (Hogg & Reid, 2006). Previous research by Sanyal (2009) found that Indian women in similar groups ‘highly value enhanced reputation and public recognition of their moral authority and collective sanctioning power’ (p. 544). Values held by women in KPJ groups may reinforce weekly participation, and participation in the weekly meetings may recursively strengthen their shared values. Recognising the commonality of these values amongst group members may increase their perceived entitativity. Social theorists posit that entitativity increases with shared identity – or, believing we are a group because we say we are a group (Hogg & Reid, 2006). Regular attendance and group practices may strengthen the belief that ‘we are a group’ as a performative statement, strengthening entitativity.
Time in the program was associated with higher depression at T2, which may reflect more challenging life circumstances and earlier recruitment to the program or an unfortunate feature of the program itself. Absent randomisation and multiple measurements, it is impossible to know the kinetics of depression and other observed variables within the program. As the program first recruited families whose children had migrated to the streets and were reintegrating with the community, it is fully possible these families face more challenges than other nearby families and these challenges are reflected in depression outcomes.
Entitativity, group trust, and loneliness
The present analysis placed trust after entitativity in the generalised structural equation model for two statistical reasons: (1) trust explained more of the association between entitativity and loneliness than entitativity explained of the association between trust and loneliness, and (2) entitativity explained more of the association between weekly attendance and trust than trust explained of the association between weekly attendance and entitativity. Though not a theoretical choice, the literature supports this ordering.
Crawford and Salaman (2012) found that higher entitativity in various groups predicted an increase in psychological need fulfilment, with the type of group (e.g. intimacy, task-oriented, or social category groups) impacting the sort of need fulfilled (affiliative, achievement, or identity). KPJ groups form with the explicit interest in strengthening their families through gaining skills relevant to finance, savings, business development, parenting and other socioeconomic areas (i.e. task-oriented motivations). Groups form with heterogeneous composition with respect to personal familiarity – some groups form with members who are personally familiar to each other, while other groups form with complete strangers. The association between entitativity and loneliness suggests groups may serve affiliative needs (e.g. connectedness, emotional attachment, and acceptance) in addition to achievement needs, and weekly attendance may facilitate the transformation of groups from task-oriented groups to intimacy groups. Consistent with Crawford and Salaman (2012), higher entitativity was associated with the greater expectation that one’s needs may be met, as expressed in a higher likelihood to express trust (La Guardia et al., 2000).
Beckes and Coan (2011) proposed that social networks characterised by familiarity, joint attention, shared goals and interdependence strengthen one’s social baseline, permitting one to distribute risk and share functional, emotional and psychological loads with peers. Social networks provide these benefits through trust that one’s social network will act in the face of novelty and uncertainty similarly to past behaviour of one’s social network. Reliability, familiarity and supportiveness are features of groups with high entitativity (Hogg & Reid, 2006). It may therefore be the feature of interpersonal trust that allows entitativity to decrease loneliness, which is itself the painful recognition of being unable to rely on others for support and connection (Hawkley & Cacioppo, 2010). While there is likely recursion between trust and entitativity, trust in the persistent benefits offered by KPJ groups may be the element that most reduces loneliness amongst group members.
Limitations
Limitations of the study include (1) inability to provide counterfactual data via randomised trials, (2) the imposition of temporal ordering on model variables, (3) under-representation of people who attend the program infrequently, (4) non-randomised recruitment of participants, and (5) misclassification of model variables via social desirability bias and other self- report biases.
Further study should randomise villages to the intervention or a control arm to develop a counter- factual. Model variables likely relate recursively rather than only in one direction as analysed. Higher entitativity groups likely have higher attendance at meetings; more trusting groups more likely have higher entitativity. Temporal ordering is essential for establishing causal relations and beyond the scope and intent of this study. Statistical models here explore potential pathways by which program participation may benefit mental health. Further study should consider other social capital constructs within this context, e.g. number of social connections, degree of participation in program and other social activities, and engagement in specific instances of support; similarly, future study should investigate which elements of ICSC are more associated with depression and modifiable by group-led microfinance. Future study should identify predictors of program attrition, and disproportionate benefits within the program.
Further research should explore the differences between participants and non-participants at the village-level. It is possible that only better-off villagers can participate as they alone have $0.20 to share each week; it is also possible that better-off villagers participate in the formal economy and do not have time available for the group meetings. It is also possible that willingness to be interviewed was influenced by variations in social capital and depression, and we are not able to know how this would influence study findings without further research. This represents only 5% of the original sample however, minimising variation. Social desirability bias may lead to under-reporting potentially embarrassing psychological characteristics, like depression, loneliness and dearth of social resources. Social desirability bias would lead towards the null hypothesis of no observed difference. Finally, other wealth and social measures will likely influence findings, and these should be explored.
Conclusion
Depression reduces quality of life and impacts a range of physical, social and behavioural health outcomes globally. Despite high global prevalence, many countries like Kenya have little health system capacity to reduce depression (Jenkins et al., 2010). This study evaluates a community-based program combining group-led microfinance with empowerment methodologies, called Kuja Pamoja (‘Come Together’ in Swahili). Depression amongst Kenyan women (n = 400) significantly decreases from baseline to 1-year follow-up. Regular program attendance predicts a significant decrease in depression, mediated by increased group entitativity, group trust and decreased loneliness. Individual cognitive social capital, as reported by group members, was consistently higher for the group than for the larger community. Implications of these initial results from the program are far-reaching, as depression and social capital affect a wide range of health, behavioural, and social outcomes. Further experimental research is required to establish novel benefits of this program within the general population; its capacity to diffuse knowledge, attitudes and practices relevant to health; and its benefits to other population segments like patients with HIV and pregnant women.
Acknowledgements
We are grateful to donors who support the program evaluated in this study. Namely, the Moody Methodist Permanent Endowment Fund in Galveston, TX and the Baxter Family Trust in Houston, TX have provided generous support that has made possible the work evaluated here. Additionally, the program staff who work diligently with families and communities to find together a brighter future, and the study participants who gave of their time to enable better understanding of the program.
Funding
The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: Funding for the study was provided by private donors of Sodzo International, while funding for the program was provided by Moody Methodist Permanent Endowment Fund and Baxter Trust. MG receives salary support from NIH K01MH119973.
Footnotes
Data availability
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Conflict of interest
The author(s) declared no potential conflicts of interest with respect to the research, authorship and/or publication of this article.
References
- Abubakar A, Kalu RB, Katana K, Kabunda B, Hassan AS, Newton CR, & Van de Vijver F (2016). Adaptation and latent structure of the Swahili version of Beck Depression Inventory-II in a low literacy population in the context of HIV. PLoS One, 11(6), e0151030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (DSM-5®). American Psychiatric Pub. [Google Scholar]
- Beck AT, Steer RA, & Brown GK (1996). Beck Depression Inventory1-II (BDI1-II). The Psychological Corporation. [Google Scholar]
- Beckes L, & Coan JA (2011). Social baseline theory: The role of social proximity in emotion and economy of action. Social and Personality Psychology Compass, 5(12), 976– 988. [Google Scholar]
- Bernard C, Dabis F, & de Rekeneire N (2017). Prevalence and factors associated with depression in people living with HIV in sub-Saharan Africa: A systematic review and meta-analysis. PLoS One, 12(8), e0181960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chesney E, Goodwin GM, & Fazel S (2014). Risks of all-cause and suicide mortality in mental disorders: A meta-review. World Psychiatry, 13(2), 153–160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crawford MT, & Salaman L (2012). Entitativity, identity, and the fulfilment of psychological needs. Journal of Experimental Social Psychology, 48(3), 726–730. [Google Scholar]
- Ehsan AM, & De Silva MJ (2015). Social capital and common mental disorder: A systematic review. Journal of Epidemiology and Community Health, 69(10), 1021–1028. [DOI] [PubMed] [Google Scholar]
- Feigenberg B, Field EM, & Pande R (2010). Building social capital through microfinance (No. w16018) National Bureau of Economic Research. [Google Scholar]
- Flores EC, Fuhr DC, Bayer AM, Lescano AG, Thorogood N, & Simms V (2018). Mental health impact of social capital interventions: A systematic review. Social Psychiatry and Psychiatric Epidemiology, 53(2), 107–119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gaertner L, & Schopler J (1998). Perceived ingroup entitativity and intergroup bias: An interconnection of self and others. European Journal of Social Psychology, 28(6), 963–980. [Google Scholar]
- Goodman ML, Gibson DC, Baker L, & Seidel SE (2020). Family-level factors to reintegrate street-involved children in low-and middle-income countries: A scoping review. Children and Youth Services Review, 109, 104664. [Google Scholar]
- Grote NK, Bridge JA, Gavin AR, Melville JL, Iyengar S, & Katon WJ (2010). A meta-analysis of depression during pregnancy and the risk of preterm birth, low birth weight, and intrauterine growth restriction. Archives of General Psychiatry, 67(10), 1012–1024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hawkley LC, & Cacioppo JT (2010). Loneliness matters: A theoretical and empirical review of consequences and mechanisms. Annals of Behavioral Medicine, 40(2), 218–227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hogg MA, & Reid SA (2006). Social identity, self-categorization, and the communication of group norms. Communication Theory, 16(1), 7–30. [Google Scholar]
- Holland H (2019, April 16). Kenyan food, water scarcity will worsen as rains fail: Met Department. Reuters. Retrieved July 30, 2019, from https://www.reuters.com/article/us-kenya-drought/kenyan-food-water-scarcity-will-worsen-as-rains-fail-met-department- [Google Scholar]
- Hughes ME, Waite LJ, Hawkley LC, & Cacioppo JT (2004). A short scale for measuring loneliness in large surveys: Results from two population-based studies. Research on Aging, 26(6), 655–672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Islam MK, Merlo J, Kawachi I, Lindström M, & Gerdtham UG (2006). Social capital and health: Does egalitarianism matter? A literature review. International Journal for Equity in Health, 5, 3. 10.1186/1475-9276-5-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jenkins R, Kiima D, Njenga F, Okonji M, Kingora J, Kathuku D, & Lock S (2010). Integration of mental health into primary care in Kenya. World Psychiatry, 9(2), 118–120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kingori C, Haile ZT, & Ngatia P (2015). Depression symptoms, social support and overall health among HIV-positive individuals in Kenya. International Journal of STD & AIDS, 26(3), 165–172. [DOI] [PubMed] [Google Scholar]
- Knack S, & Keefer P (1997). Does social capital have an economic payoff? A cross-country investigation. The Quarterly Journal of Economics, 112(4), 1251–1288. [Google Scholar]
- La Guardia JG, Ryan RM, Couchman CE, & Deci EL (2000). Within-person variation in security of attachment: A self-determination theory perspective on attachment, need fulfillment, and well-being. Journal of Personality and Social Psychology, 79(3), 367. [DOI] [PubMed] [Google Scholar]
- Morris SS, Carletto C, Hoddinott J, & Christiaensen LJ (2000). Validity of rapid estimates of household wealth and income for health surveys in rural Africa. Journal of Epidemiology and Community Health, 54(5), 381–387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murayama H, Fujiwara Y, & Kawachi I (2012). Social capital and health: A review of prospective multilevel studies. Journal of Epidemiology, 22(3), 179–187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Osborn TL, Venturo-Conerly KE, Wasil AR, Schleider JL, & Weisz JR (2020). Depression and anxiety symptoms, social support, and demographic factors among Kenyan high school students. Journal of Child and Family Studies, 29(5), 1432–1443. [Google Scholar]
- Patel V, Burns JK, Dhingra M, Tarver L, Kohrt BA, & Lund C (2018). Income inequality and depression: A systematic review and meta-analysis of the association and a scoping review of mechanisms. World Psychiatry, 17(1), 76–89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Poortinga W (2006). Social relations or social capital? Individual and community health effects of bonding social capital. Social Science and Medicine, 63(1), 255–270. [DOI] [PubMed] [Google Scholar]
- Pronyk PM, Harpham T, Busza J, Phetla G, Morison LA, Hargreaves JR, Kim JC, Watts CH, & Porter JD (2008). Can social capital be intentionally generated? A randomized trial from rural South Africa. Social Science and Medicine, 67(10), 1559–1570. [DOI] [PubMed] [Google Scholar]
- Rico-Uribe LA, Caballero FF, Olaya B, Tobiasz-Adamczyk B, Koskinen S, Leonardi M, Haro JM, Chatterji S, Ayuso-Mateos JL, & Miret M (2016). Loneliness, social networks, and health: A cross-sectional study in three countries. PLoS One, 11(1), e0145264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sanyal P (2009). From credit to collective action: The role of microfinance in promoting women’s social capital and normative influence. American Sociological Review, 74(4), 529–550. [Google Scholar]
- Siisiainen M (2003). Two concepts of social capital: Bourdieu vs. Putnam. International Journal of Contemporary Sociology, 40(2), 183–204. [Google Scholar]
- Sommer TE, Sabol TJ, Chase-Lansdale PL, Small M, Wilde H, Brown S, & Huang ZY (2017). Promoting parents’ social capital to increase children’s attendance in Head Start: Evidence from an experimental intervention. Journal of Research on Educational Effectiveness, 10(4), 732–766. [Google Scholar]
- Villalonga-Olives E, Wind TR, & Kawachi I (2018). Social capital interventions in public health: A systematic review. Social Science and Medicine, 212, 203–218. [DOI] [PubMed] [Google Scholar]
- World Health Organization. (2017). Depression and other common mental disorders: Global health estimates (No. WHO/MSD/MER/2017.2). World Health Organization. [Google Scholar]
- Wydick B (2001). Can social cohesion be harnessed to repair market failures? Evidence from group lending in Guatemala. The Economic Journal, 109(457), 463–475. [Google Scholar]


