Abstract
While there is evidence of morbidity compression in many countries, temporal patterns of non-communicable diseases (NCDs) in developing countries, such as India, are less clear. Age at onset of disease offers insights to understanding epidemiologic trends and is a key input for public health programs. Changes in age at onset and duration of major NCDs were estimated for 2004 (n = 38,044) and 2018 (n = 43,239) using health surveys from the India National Sample Survey (NSS). Survival regression models were used to compare trends by sociodemographic characteristics. Comparing 2004 to 2018, there were reductions in age at onset and increases in duration for overall and cause-specific NCDs. Median age at onset decreased for NCDs overall (57 to 53 years) and for diabetes, hypertension, heart disease, asthma, mental diseases, eye disease, and bone disease in the range of 2–7 years and increased for cancer, neurological disorders, some genitourinary disorders, and injuries/accidents in the range of 2–14 years. Hazards of NCDs were higher among females for cancers (HR 1.51, 95% CI 1.19–1.90) and neurological disorders (HR 1.18, 95% CI 1.06–1.32) but lower for heart diseases (HR 0.88, 95% CI 0.79–0.97) and injuries/accidents (HR 0.87, 95% CI 0.77–0.99). Hazards were greater among those with lower educational attainment at younger ages and higher educational attainment later in life. Unlike many countries, chronic disease morbidity may be expanding in India for many chronic diseases, indicating excess strain on the health system. Public health programs should focus on early diagnosis and prevention of NCDs.
Supplementary Information
The online version contains supplementary material available at 10.1007/s11357-020-00296-9.
Keywords: Non-communicable diseases, Onset, NSS, India, Duration of disease
Introduction
Global life expectancy increased dramatically over the twentieth and twenty-first centuries, as many countries observed a shift in disease and mortality patterns away from infectious diseases [1]. Non-communicable diseases (NCDs) are now the leading cause of premature morbidity and mortality—both within India and globally [1–4]. However, as with infectious diseases before them, NCDs are not distributed equally. Globally, an estimated 57 million deaths were attributable to NCDs in 2016, of which three-quarters occurred in low- and middle-income countries (LMICs) [2]. The epidemiologic transition from infectious to chronic disease, and the corresponding increase in life expectancy, may have implications for perceived quality life for the additional years of life lived, depending upon whether those years are spent healthy or diseased [3].
A key framework for understanding this transition and its effect on quality of life is known as the “compression or morbidity” hypothesis, which postulates that, on average, there will be fewer years living with disease and disability as the age at onset of disease becomes delayed at a faster rate than the age of death [5]. However, the “morbidity compression” hypothesis is primarily based on evidence from high-income countries. It is unclear if the compression of morbidity hypothesis can be equally applied to all countries, especially in developing countries which may experience NCDs differently [6–9]. For example, the NCD-related disease burden has been increasing rapidly in LMICs and the probability of death due to NCDs is twice as high among adults in LMICs compared with adults in high-income countries [10–16].
India accounts for a quarter of global NCD deaths (9.6 million), and NCDs are the leading cause of morbidity, disability, hospitalization, and mortality [1, 4, 17, 18]. From 1990 to 2016, the proportion of total disability-adjusted life years (DALYs) attributable to NCDs in India increased from 30.5 to 55.4% [19]. Similarly, out-of-pocket payments (OOP), catastrophic health spending (CHS), and distress financing for treating NCDs have also been on the rise [20–23]. In response to these trends, governmental and non-governmental health organizations have called for prevention and control of NCDs in India [24, 25]. In particular, the National Health Policy (NHP) 2017 aims to reduce premature mortality from cardiovascular diseases, cancers, diabetes, and chronic respiratory diseases by 25% by 2025 [24].
However, despite evidence of an increasing overall burden of NCDs in India, details of this trend remain unclear. For example, it is unclear how age at onset and duration of NCDs have changed over time [21, 26–29]. Estimates of the age at onset and duration of NCDs are key inputs for public health programs, health planning, and health budgeting. Understanding trends in these metrics for NCDs can help in understanding who is being affected by NCDs, when, and for how long [30, 31]. That is, trends in age at onset and duration of NCDs can also aid in clarifying whether morbidity in India is expanding or contracting.
Thus, understanding trends in the age at onset of NCDs not only provides insight into whether the compression of morbidity hypothesis can be equally applied to diverse contexts, such as India, but also has important practical implications for public health programming. Each of these represents important gaps in the understanding of NCD trends in India. To this end, we examined changes in the age at onset and duration of 12 major categories of NCDs from 2004 to 2018 for the population of India, as well as variation in these changes by individual sociodemographic characteristics. The 12 NCDs are diabetes, hypertension, heart disease, asthma, genitourinary, cancer, neurological, mental disease, blood disease, eye disease, bone disease, and injury/accident. The classification of these categories is guided by the adequacy of sample, comparability over surveys, international classification of disease, and literature.
Methods
Data and study population
Data for this study derived from 2 years of health surveys (Schedule 25.0) corresponding to the 60th and 75th rounds of the National Sample Survey (NSS), conducted in 2004 and 2017–18 (hereafter abridged to “2018”), respectively. The NSS is the official statistical survey of the Government of India, set up in 1950 with the primary objective of collecting data on various socioeconomic aspects of the population, and each year focusing on specific subjects such as education, health, or consumption. Data collected by the Nation Sample Surveys (NSS) are reliable and extensively used in policy and research worldwide. These population-based surveys include observations from all states and union territories of India via multistage stratified sampling. Details of the sampling procedure, instruments, and preliminary findings are available in the respective survey report [32, 33].
For the purposes of this study, we focused on the two surveys conducted in 2004 and 2018 in order to maintain comparability in instruments while allowing for a sufficient length of time to capture changes in disease trends. The survey year 2018 is the latest round of NSS containing health surveys while 2004 is the earliest comparable year as surveys prior to 2000 utilized different health instruments. Since we were interested in examining changing trends in the age at onset of NCDs, we determined that a 14-15 year period would be a reasonable time period. Surveys for both years collected comprehensive information on household characteristics (household consumption expenditure, source of energy for cooking, sanitation facility etc.), individual characteristics (age, sex, marital status, educational attainment, coverage of health insurance scheme etc.), and hospitalization and ailment particulars. Information on self-reported ailments (either diagnosed and/or symptomatic) was collected in 15-day reference periods and coded into 42 categories in 2004 and 63 categories in 2018. Further information on the original survey data including instruments and technical reports are publicly available at the government website (www.mospi.gov.in). A total of 38,044 ailments corresponding to 34,930 individuals were recorded in 2004, and 43,239 ailments for 39,777 individuals were logged in 2018. In 2004, the NSS provided the morbidities associated with 42 individual ailments (5 major categories), whereas in 2018, morbidities were classified into 63 individual ailments and 15 major categories. We reclassified these ailments into 24 categories including 14 NCDs by taking into account disease similarity, classification schemes adopted in prior studies, and sample size. Table 2 presents the details of disease reclassifications including the number of cases for 2004 and 2018. There were insufficient sample sizes for asthma and back/body ache in 2004. Therefore, our analysis was limited to 12 categories of NCDs, accounting for 36% of total ailments in 2004 and 46% in 2018. Morbidity rates were defined as the number of morbidity cases per 100,000 individuals.
Table 2.
Classification of morbidity, morbidity rate, and duration of alignment in India, 2004 and 2018
| 2004 | 2018 | ||||||
|---|---|---|---|---|---|---|---|
| Sr. No. | Morbidity category | Morbidity rate per 1,000,000 | Duration of ailment in days | Number of cases | Morbidity rate per 1,000,000 | Duration of ailment in days | Number of cases |
| 1 | Diabetes | 339 | 999 | 1691 | 1006 | 1440 | 6568 |
| 2 | Hypertension | 495 | 720 | 2287 | 1076 | 1270 | 6379 |
| 3 | Heart Disease | 257 | 365 | 1501 | 258 | 975 | 2028 |
| 4 | Asthma | 345 | 320 | 1540 | 217 | 960 | 1242 |
| 5 | Thyroid | 11 | 109 | 51 | 149 | 1065 | 820 |
| 6 | Genitourinary (disease of kidney/urinary system, prostatic disorders, gynaecological disorders) | 220 | 50 | 1184 | 98 | 215 | 686 |
| 7 | Cancer | 50 | 180 | 379 | 26 | 570 | 400 |
| 8 | Neurological | 193 | 200 | 1015 | 286 | 365 | 1680 |
| 9 | Mental disease | 64 | 450 | 309 | 58 | 2190 | 399 |
| 10 | Blood disease | 45 | 80 | 199 | 65 | 60 | 400 |
| 11 | Eye disease | 498 | 365 | 2260 | 87 | 120 | 476 |
| 12 | Bone disease | 624 | 350 | 2564 | 510 | 700 | 2503 |
| 13 | Back or body aches | NA | NA | NA | 170 | 300 | 846 |
| 14 | Injury accident | 256 | 10 | 1222 | 193 | 20 | 1316 |
| 15 | Fever | 2032 | 5 | 6440 | 2351 | 4 | 9904 |
| 16 | Cough but not TB | 236 | 6 | 788 | 121 | 6 | 583 |
| 17 | Diarrhoea | 509 | 4 | 1823 | 126 | 4 | 566 |
| 18 | skin disease | 214 | 30 | 693 | 183 | 35 | 798 |
| 19 | Acute upper respiratory infection | 673 | 6 | 2532 | 485 | 5 | 2572 |
| 20 | Gastrointestinal | 496 | 16 | 1929 | 344 | 45 | 1817 |
| 21 | Tuberculosis | 111 | 180 | 669 | 38 | 240 | 276 |
| 22 | Obstetric | NA | NA | NA | 20 | 25 | 181 |
| 23 | Child birth | NA | NA | NA | 6 | 12 | 107 |
| 24 | Others | 1849 | 11 | 6968 | 102 | 45 | 692 |
| Total | 9518 | 223 | 38,044 | 7977 | 880 | 43,239 | |
Age at onset of disease
Both survey years included information on current age and total duration (in days) of each ailment. Age at onset of disease was defined as the difference between current age and duration of disease. It should be noted that definitions of age at onset of disease are inconsistent in the literature. For instance, some studies have defined it using the first symptom of illness, while others have used time of first hospitalization, or first symptom in connection with first hospitalization [30]. In the Health and Retirement Study (HRS), age at onset was derived from a question on the age at diagnosis by a trained health professional [31].
Statistical analysis
Descriptive statistics, Kaplan-Meier survival estimation, and Cox proportional hazards models were used to estimate the onset and duration of NCDs. Morbidity rates were computed as the number of morbid cases excluding child birth and death cases per 100,000 individuals. The distribution and median age of disease are indicators of the progression of disease in a population. Median onset time was defined as the average age below which half of the population experienced a specific morbidity (among those who had a morbidity). To examine the change in median age for a specific disease over the two survey time periods, we performed two sample non-parametric tests of medians. Changes in median age at onset of disease were also classified into 2 × 2 contingency tables, with Fisher’s exact tests and Pearson’s chi-squared tests calculated to test for significant differences.
Kaplan-Meier survival functions were utilized to estimate the probability of a specific morbidity not occurring until a certain age. Each Kaplan-Meier estimator used age at the time of onset (in years) at the time of disease onset as the measure of time, and a binary disease onset variable (1 = disease onset; 0 = no disease/censored) as the final event (failure) measure. The Kaplan-Meier estimate of survival time S(t) is given by:
| 1 |
where ni is the number of subjects observed at time ti, and di is the number of a subject who experienced the event of interest at time ti. This gives the probability that a person survives the age duration (up to age x) without the occurrence of a given disease.
Cox proportional hazards regression models were used to predict the time (age in years) of first onset of disease based on a set of sociodemographic factors. The Cox proportional hazards model estimates the risk of an individual developing a disease at a specific point in time, t, given that the individual was disease-free prior to time t. A set of disease-specific Cox proportional hazards regression models was estimated in order to assess the role of sociodemographic factors on each of the 12 NCD categories. The event of interest in these models was the initial onset of a specific disease, coded as a binary variable (1 = diseased; 0 = disease-free). Once an individual within the risk group experienced first onset of an NCD, they were no longer considered at-risk for that event again. The proportional hazards model is specified by:
| 2 |
where hi(ti; xi) is the hazard function of the comparison of diseased to disease-free individuals at time ti with a specified set of independent variables denoted by xi, and an accompanying set of parameters, βi, to be estimated [34]. The Kaplan-Meier and Cox proportional hazards survival curves are presented for 7 of the 12 NCDs, namely, diabetes, high blood pressure, heart disease, cancer, neurological, mental disease, and injury/accident for dispositional clarity.
Results
Table 1 presents the sample profile of households and individuals surveyed in 2004 and 2018. The average household size was 5.18 in 2004 and 4.35 in 2018. Approximately 70% of the sample was literate. The median age of the population was 24 years in 2004 and 27 years in 2018. The monthly per capita consumption expenditures (MPCE) increased by 30% over the study period.
Table 1.
Sample profile of participants from the India National Sample Survey, 2004 and 2018
| Variables | 2004 | 2018 |
|---|---|---|
| Total population covered | 383,338 | 555,351 |
| Number of households | 73,868 | 113,823 |
| Average household size | 5.18 | 4.35 |
| Sex ratio (number of females per 1000 males) | 952 | 935 |
| Percent urban | 25.43% | 29.46% |
| Percent SC and ST | 28.44% | 28.25% |
| Educational attainment | ||
| No formal schooling | 34.13% | 26.06% |
| Up to primary | 61.11% | 29.96% |
| Middle/secondary | 3.81% | 25.99% |
| Higher secondary and above | 0.95% | 17.99% |
| Monthly per capita consumption expenditure (at 2018 prices) | 1838 | 2617 |
| Median age (years) | 24 | 27 |
| Morbidity rate (per 100,000 population) | 8743 | 7465 |
| Median age of any NCD | 57 | 53 |
| Number of morbidity cases (15 days of reference period) | 34,930 | 39,777 |
SC schedule castes, ST schedule tribes
Morbidity rates and duration of NCDs
While the all-cause morbidity rate decreased from 9518 to 7977 per 100,000 individuals from 2004 to 2018, the overall morbidity rate for non-communicable diseases increased from 3045 to 3782 (per 100,000 population), as well as for most of the 12 cause-specific NCDs (Table 2). In particular, cause-specific morbidity rates increased for diabetes, high blood pressure, neurological disorders, and bone diseases. In 2004, among the listed NCDs, the cause-specific morbidity rates were the highest for bone disease (624), eye disease (498), and hypertension (495). By 2018, morbidity rates were the highest for hypertension (1076), followed by diabetes (1006) and bone disease (510), suggesting a change in disease patterns over time. The mean duration of ailment (number of days) increased for most of the NCDs during the period of 2004 to 2018. In 2004 the mean duration of ailment (number of days) was the highest for diabetes (999) followed by hypertension (720) and mental disease (450). By 2018, cause-specific mean durations increased for most NCDs and were the highest for mental disease (2190) followed by diabetes (1440) and hypertension (1270).
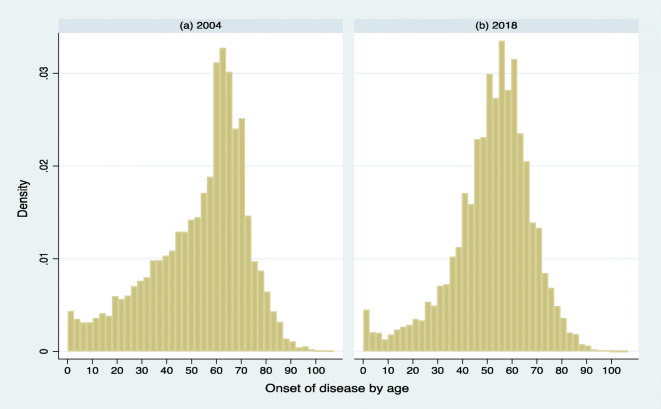
Changing distributions of age at onset of NCDs
Figure 1 shows the changing distribution for the age at onset of all NCDs combined for 2004 and 2018. The distribution shifted to the left, suggesting that NCDs overall are increasingly affecting individuals at younger working ages. Table 3 summarizes changes in the average age of onset for each of the 12 NCDs from 2004 to 2018. In particular, the median age of onset for NCDs as a whole declined from 57 years in 2004 to 53 years by 2018 (Table 1). The median age of onset declined for most (7 of 12) individual NCD categories over this period: diabetes from 58 to 53 years, hypertension decreased from 61 to 55 years, heart disease decreased from 58 to 55 years, and asthma from 61 to 54 years. The largest reductions in the median age of onset were for eye disease (14 years), asthma (7 years), diabetes (5 years), bone disease (5 years), and heart diseases (3 years). However, median age of onset increased for injuries/accidents (from 36 to 40 years) and genitourinary conditions (from 37 to 39 years). The changes in median age over time are found significant for all the NCDs except mental and neurological diseases. Changes in age of onset can also be seen at the left and right tails of the distributions (e.g., 25th and 75th percentiles) in a similar line of median age (Table 3). The mean age of onset of these diseases is also similar to that of median age.
Fig. 1.
Histograms of age at onset for any non-communicable diseases in India, 2004 and 2018
Table 3.
Distribution of age at onset of non-communicable diseases in India, 2004 and 2018
| Age at onset in 2004 | Age at onset in 2018 | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Sr. No. | Disease | P25 | Median | P75 | Mean | 95% CI | P25 | Median | P75 | Mean | 95% CI | Median test 2004–2018 Pearson chi2 (p value) | Change in median age of onset (2018–2004) |
| 1 | Diabetes | 50 | 58 | 65 | 57 | 56.91–58.01 | 46 | 53 | 60 | 53 | 52.81–53.36 | 172.77 (0.000) | − 5 |
| 2 | Hypertensions | 52 | 61 | 67 | 57 | 56.62–57.7 | 47 | 55 | 62 | 55 | 54.33–54.90 | 256.91 (0.000) | − 6 |
| 3 | Heart disease | 47 | 58 | 67 | 55 | 53.74–55.39 | 45 | 55 | 64 | 54 | 53.29–54.66 | 5.47 (0.019) | − 3 |
| 4 | Asthma | 46 | 61 | 68 | 53 | 52.28–54.35 | 40 | 54 | 64 | 51 | 49.48–51.56 | 58.02 (0.000) | − 7 |
| 5 | Genitourinary | 27 | 37 | 54 | 38 | 37.00–39.05 | 27 | 39 | 52 | 41 | 39.79–42.57 | 27.77 (0.000) | + 2 |
| 6 | Cancer | 35 | 48 | 61 | 48 | 45.81–49.73 | 41 | 54 | 58 | 50 | 48.55–51.42 | 6.72 (0.01) | + 6 |
| 7 | Neurological | 26 | 45 | 63 | 43 | 41.82–44.54 | 34 | 46 | 59 | 45 | 43.82–45.61 | 1.48 (0.223) | + 1 |
| 8 | Mental disease | 23 | 35 | 51 | 37 | 34.92–39.18 | 16 | 28 | 44 | 31 | 28.86–32.83 | 0.0012 (0.972) | − 7 |
| 9 | Blood disease | 21 | 38 | 58 | 33 | 30.22–36.54 | 20 | 45 | 60 | 42 | 39.29–43.87 | 4.01 (0.045) | + 7 |
| 10 | Eye disease | 53 | 64 | 70 | 57 | 55.84–57.56 | 29 | 50 | 65 | 46 | 44.34–48.44 | 81.19 (0.000) | − 14 |
| 11 | Bone disease | 49 | 61 | 68 | 56 | 55.46–56.73 | 48 | 56 | 64 | 55 | 54.73–55.79 | 170.97 (0.000) | − 5 |
| 12 | Injury/accident | 19 | 36 | 55 | 34 | 32.56–34.95 | 20 | 40 | 57 | 39 | 37.65–39.93 | 18.26 (0.000) | + 4 |
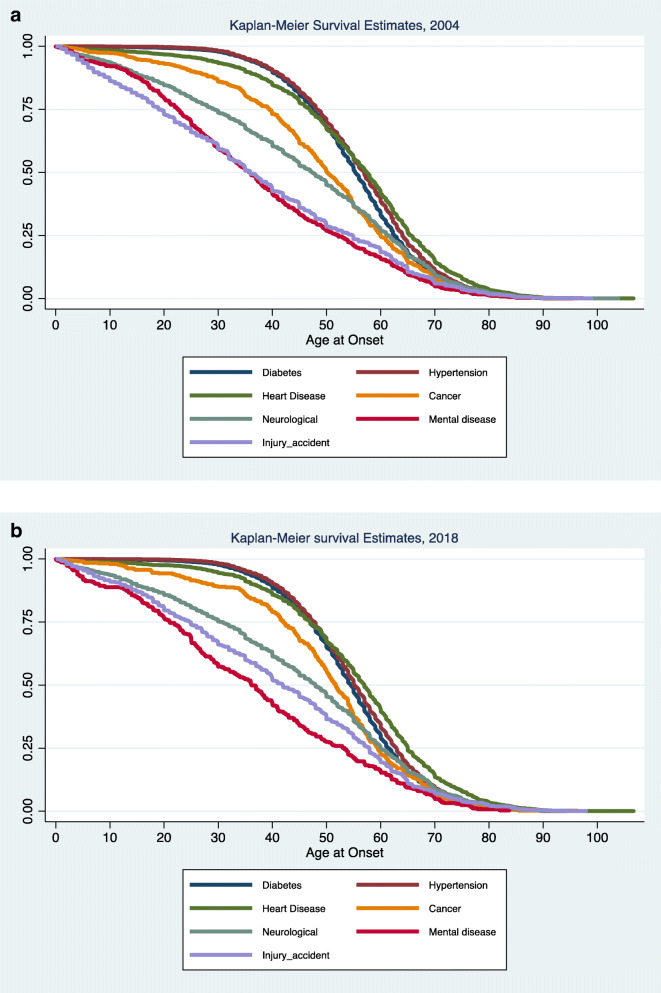
K-M survival estimates of selected NCDs
Figure 2 a and b present Kaplan-Meier (K-M) survival estimates for diabetes (navy blue), heart disease (foster green), high blood pressure (maroon), cancers (dark orange), neurological disorders (teal), mental diseases (cranberry), and injuries/accidents (lavender) in 2004 and 2018, respectively. The probability of “survival,” or maintaining disease-free status (K-M curve) consistently decreases with age, ultimately approaching zero for all conditions beyond age 80 in India. The position of the curves highlights variation in the ages associated with each NCD category. For example, the red curve, representing mental conditions, shifted diagonally downward to the left relative to other curves, suggesting that these conditions affect individuals at younger ages. In particular, in 2018, the probability of onset (1-Pr(survival)) of mental disease by age 40 was 0.6 (1.0–0.4), while that of diabetes and hypertension were each less than 0.2 (1.0–0.8). Further, by comparing K-M survival curves for 2004 (a) and 2018 (b), we can also observe nuances in the changing distributions of NCDs over time, for example, the red curve for mental diseases shows a dip in probability of survival especially among younger ages (e.g., < 20 years). At the same time, accidents/injuries and neurological disorders showed late onset than mental disorders, but younger ages than the remaining NCD categories. Diabetes, hypertension, and heart disease occurred at relatively older ages. Yet, every NCD category was more likely to occur by age 60.
Fig. 2.
Kaplan-Meier survival curves for selected NCDs in India, 2004 (a) and 2018 (b)
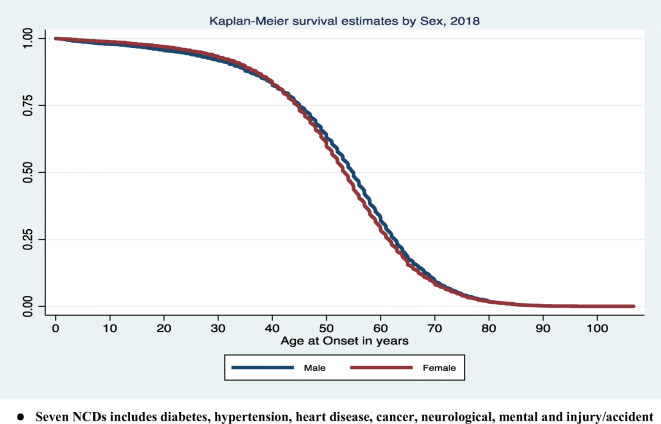
K-M survival estimates by sex and education
Figures 3 and S1 (a) through S1 (f) (in “Supplementary Materials”) display K-M survival curves for all NCDS combined and by NCD categories (diabetes, high blood pressure, heart disease, cancers, neurological, mental disease, and injuries/accidents), stratified by sex (males vs. females). The probability of remaining disease-free of any NCDs was lower among males than females up to age 40 years, but beyond age 40 the probabilities were higher for male than female. On the other hand, curves for diabetes, hypertension, heart disease, and cancers showed the opposite pattern, i.e., the female survival curve shifted to the left of the male curve. Thus, contrary to general pattern of NCDs as a whole, age of onset for diabetes, hypertension, heart disease, and cancers were lower among females than males. Lastly, the survival curves for neurological disorders and mental health conditions varied by life stage. For example, the chance of occurrence of neurological disorders was higher among males up to age 30; beyond age 30, the chance of occurrence was greater for females. The pattern was reversed for mental health conditions: females experienced earlier onset during the initial stages of life, whereas males experienced earlier onset in later life stages.
Fig. 3.
Kaplan-Meier (K-M) survival curves for any of the seven NCDs in India by sex, 2018. Seven NCDs include diabetes, hypertension, heart disease, cancer, neurological, mental and injury/accident
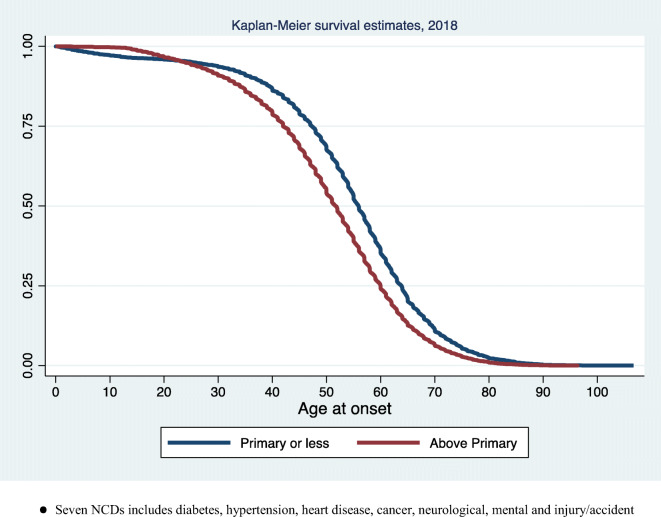
Figures 4 and S2 (in “Supplementary Materials”) show K-M survival curves for all NCDs and each of NCD category by the level of education. The onset of any NCDs was earlier among those whose educational attainment was below primary up to around age 25, after which the age of onset became lower for those with above primary education (Fig. 4). The survival curves were similar for diabetes, high blood pressure, and heart disease. Though a variation in survival by education is distinct, the curves correspond to these NCDs show a smooth sigmoid pattern showing an onset of the disease after age 20. The rest of the survival curves are not so systematic and showed a distinct stepwise downfall in the survival probability with an underlying variation by education. In this direction, the corresponding survival pattern of injury/accident showed an almost diagonal pattern suggesting a very quick reduction in the survival probability over the ages. The survival curve also shows that one-fourth of the total population who are up to primary educated experienced some forms of injury/accident by age 20, and the corresponding survival probability is observed the highest among higher secondary and above educated till age 20 with a gradual sharp decrease in the survival probability over the ages for this particular group of population. In particular, individuals of lower education experienced lower survival earlier in life (less than 10–20 years), yet experienced increased survival later in life for injuries/accidents, neurological disorders, and mental health conditions. Trends were more consistent for diabetes, high blood pressure, and heart diseases, each of which showed a graded, positive relationship with educational attainment. That is, age of onset for these NCDs occurred earlier among those with the middle, secondary, and higher secondary and above education levels compared with those with less than primary education.
Fig. 4.
Kaplan-Meier (K-M) survival curves for any of the seven NCDs in India by education, 2018. Seven NCDs include diabetes, hypertension, heart disease, cancer, neurological, mental, and injury/accident
Variation in median age at onset of NCDs by sociodemographic characteristics
Variation in the median age (in terms of years) of onset of NCDs by selected characteristics is presented in Tables S1 (diabetes, heart disease, and high blood pressure) and S2 (cancer, neurological, mental disease, and injury/accident). Median onset time (MOT) of NCDs varied by region, place of residence, educational attainment, religious belief, social group, gender, and MPCE and with employment status. In particular, the regional variation in age of onset was found largest for mental health conditions followed by, injuries/accidents and cancers. A rural-urban differential in median age of onset was also evident for caners (50 for rural, 53 for urban), neurological disorders (46 for rural, 48 for urban), mental diseases (30 for rural, 36 for urban), and injuries/accidents (38 for rural, 42 for urban).
Hazard rates of NCDs by sociodemographic characteristics
Table 4 presents hazard rates from the Cox proportional hazards models. The estimated hazards show that, compared with the Northern region, populations in the Southern and Western regions were 1.73 (HR = 2.72; 95% CI 2.12–3.49) and 1.75 (HR = 3.38; 95% CI 2.56–4.45) times more likely to develop both diabetes and heart disease, respectively. There was a clear gradient in an increased risk of developing NCDs among those with higher educational attainments for all NCDs except high blood pressure. Females had higher hazards of developing diabetes, high blood pressure, heart disease, cancers, and neurological disorders. On the other hand, hazards of experiencing mental health conditions and injuries/accidents were higher among males. Hazards were higher among the highest MPCE tertile group (relative to the lowest) for heart disease, diabetes, and cancers, but lower for all other NCD categories.
Table 4.
Hazards ratio and 95% confidence interval of selected NCDs in India in 2018
| Background characteristics | Diabetes | Hypertension | Heart disease | Cancer | Neurological disease | Mental disease | Injury/accident | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Hazard ratio | 95% CI | Hazard ratio | 95% CI | Hazard ratio | 95% CI | Hazard ratio | 95% CI | Hazard ratio | 95% CI | Hazard ratio | 95% CI | Hazard ratio | 95% CI | |
| Region | ||||||||||||||
| Northern region | 1 | 1 | 1 | 1 | 1 | 1 | 1 | |||||||
| Eastern region | 1.62 | 1.26–2.1 | 0.83 | 0.67–1.02 | 0.50 | 0.30–0.83 | 0.50 | 0.19–1.36 | 1.04 | 0.67–1.61 | 2.27 | 0.78–6.59 | 2.58 | 1.29–5.17 |
| Northeast | 1.50 | 1.06–2.13 | 0.40 | 0.27–0.6 | 0.90 | 0.49–1.67 | 1.60 | 0.61–4.17 | 1.14 | 0.63–2.08 | 1.52 | 0.30–7.65 | 3.68 | 1.67–8.11 |
| Western Central | 3.38 | 2.56–4.45 | 0.68 | 0.49–0.94 | 1.16 | 0.64–2.08 | 0.25 | 0.03–1.97 | 0.54 | 0.21–1.37 | 2.27 | 0.45–11.51 | 0.32 | 0.04–2.51 |
| Southern region | 2.72 | 2.12–3.49 | 1.34 | 1.09–1.64 | 0.48 | 0.26–0.89 | 0.77 | 0.27–2.13 | 1.48 | 0.91–2.39 | 1.94 | 0.57–6.58 | 5.69 | 2.84–11.38 |
| Residence | ||||||||||||||
| Rural | 1 | 1 | 1 | 1 | 1 | 1 | 1 | |||||||
| Urban | 1.26 | 1.19–1.34 | 1.13 | 1.06–1.2 | 0.95 | 0.85–1.06 | 0.82 | 0.64–1.06 | 0.75 | 0.66–0.84 | 0.83 | 0.65–1.07 | 0.87 | 0.76–0.99 |
| Education | ||||||||||||||
| No education | 1 | 1 | 1 | 1 | 1 | 1 | 1 | |||||||
| Up to primary | 1.57 | 1.45–1.7 | 1.37 | 1.27–1.48 | 1.55 | 1.35–1.79 | 1.69 | 1.22–2.35 | 1.52 | 1.31–1.77 | 0.80 | 0.58–1.1 | 2.05 | 1.71–2.46 |
| Middle/secondary | 2.17 | 2.00–2.35 | 2.04 | 1.88–2.21 | 2.09 | 1.80–2.42 | 2.39 | 1.71–3.35 | 2.38 | 2.04–2.77 | 1.24 | 0.91–1.69 | 2.62 | 2.17–3.16 |
| Higher secondary and above | 2.73 | 2.49–2.99 | 2.16 | 1.97–2.37 | 2.35 | 1.99–2.79 | 3.67 | 2.54–5.32 | 1.78 | 1.46–2.17 | 1.06 | 0.72–1.54 | 2.76 | 2.23–3.43 |
| Religion | ||||||||||||||
| Hindu | 1 | 1 | 1 | 1 | 1 | 1 | 1 | |||||||
| Muslim | 1.39 | 1.28–1.5 | 1.38 | 1.27–1.5 | 1.58 | 1.37–1.82 | 1.10 | 0.75–1.62 | 1.36 | 1.15–1.6 | 1.46 | 1.08–1.98 | 1.10 | 0.91–1.34 |
| Others | 0.88 | 0.80–0.96 | 0.96 | 0.87–1.06 | 0.91 | 0.77–1.08 | 1.12 | 0.76–1.65 | 1.04 | 0.84–1.29 | 0.70 | 0.42–1.17 | 1.08 | 0.85–1.36 |
| Social group | ||||||||||||||
| ST | 1 | 1 | 1 | 1 | 1 | 1 | 1 | |||||||
| SC | 1.27 | 1.05–1.53 | 1.30 | 1.08–1.57 | 1.20 | 0.85–1.71 | 1.28 | 0.65–2.51 | 0.98 | 0.74–1.3 | 1.75 | 0.73–4.18 | 0.56 | 0.41–0.76 |
| OBC | 1.04 | 0.87–1.25 | 1.17 | 0.98–1.4 | 0.99 | 0.71–1.39 | 0.87 | 0.46–1.65 | 0.74 | 0.57–0.97 | 1.81 | 0.78–4.18 | 0.59 | 0.44–0.79 |
| Others | 1.00 | 0.84–1.2 | 1.03 | 0.86–1.23 | 0.82 | 0.59–1.15 | 0.83 | 0.44–1.56 | 0.54 | 0.41–0.7 | 1.73 | 0.75–4.02 | 0.42 | 0.31–0.56 |
| Sex | ||||||||||||||
| Male | 1 | 1 | 1 | 1 | 1 | 1 | 1 | |||||||
| Female | 1.24 | 1.17–1.31 | 1.49 | 1.41–1.58 | 0.88 | 0.79–0.97 | 1.51 | 1.19–1.9 | 1.18 | 1.06–1.32 | 0.84 | 0.67–1.06 | 0.87 | 0.77–0.99 |
| MPCE tertile | ||||||||||||||
| Poor | 1 | 1 | 1 | 1 | 1 | 1 | 1 | |||||||
| Middle | 1.11 | 1.02–1.2 | 1.23 | 1.13–1.34 | 1.06 | 0.91–1.24 | 0.86 | 0.61–1.21 | 1.02 | 0.88–1.18 | 0.90 | 0.67–1.21 | 0.88 | 0.75–1.04 |
| Rich | 1.18 | 1.08–1.28 | 1.26 | 1.15–1.37 | 1.18 | 1.01–1.37 | 1.02 | 0.73–1.42 | 0.72 | 0.61–0.84 | 0.70 | 0.51–0.96 | 0.71 | 0.60–0.85 |
| Employment | ||||||||||||||
| Labour | 1 | 1 | 1 | 1 | 1 | 1 | 1 | |||||||
| Self-employed | 1.06 | 0.94–1.2 | 0.88 | 0.78–1 | 0.80 | 0.65–0.99 | 0.54 | 0.35–0.84 | 0.70 | 0.57–0.87 | 1.08 | 0.65–1.8 | 0.84 | 0.65–1.09 |
| Regular wage/salary | 1.08 | 0.96–1.23 | 0.92 | 0.82–1.04 | 0.87 | 0.70–1.07 | 0.55 | 0.35–0.86 | 0.71 | 0.57–0.89 | 1.06 | 0.62–1.79 | 0.89 | 0.69–1.16 |
| Others | 0.71 | 0.62–0.81 | 0.61 | 0.54–0.7 | 0.57 | 0.45–0.72 | 0.31 | 0.18–0.51 | 0.45 | 0.35–0.58 | 1.06 | 0.60–1.88 | 0.40 | 0.29–0.55 |
Italics indicates significance
HR hazards ratio, 95% CI 95% confidence interval, SC schedule castes, ST schedule tribes, MPCE monthly per capita consumption expenditure
Discussion
Results from this study have a number of important implications for understanding and prevention of NCDs in India. First, the age of onset of NCDs in India is lower than many developing and developed countries [33]. About one-fourth of NCDs occur before age 42, half of these before 52 and three-fourth by 61, suggesting that working adults are largely affected by NCDs. Second, trends in the age at onset are distinct for each NCD. One-fourth of mental illnesses showed an onset prior to age 16, and one-fourth of neurological disorders before age 33. Third, we observed distinct sex differentials in NCDs, with higher hazard ratios among females in terms of cancer and neurological disorder, whereas hazard ratios were greater for males for in the cases of heart disease and injury/accident. Fourth, the probability of onset of NCDs is often greater among those with lower educational attainment at younger ages, whereas the probability becomes relatively higher among those with higher education levels later in life.
We provide some plausible explanations in support of these findings. A decade ago, awareness regarding health was lower in India, and health facilities were less equipped with modern diagnostics facilities than today. The lack of awareness, accessibility, and resources could have prevented care seeking and diagnosis of NCDs [35]. With increase in awareness, the rising income level and accessibility to healthcare, people may have increased use of health facilities. However, it is likely that a significant proportion of less educated and poor populations, residing in remote geographical places, remain undiagnosed. This may account for some of the observations of a lower probability of NCDs among less educated. Similarly, the probability of early onset of cancer and neurological disorder among females may be due to the interplay of behavioural and household risk factors [36]. The lower hazard ratio among female for heart disease can be explained by the protective effect of oestrogen. Similarly, the lower hazard ratio of accidents and injuries may be due to lower mobility among females compared with males. Risk factors of NCDs among males and females are similar except alcohol consumption and smoking patterns among females. At the same time, women’s health, especially regarding reproductive health issues, had not been prioritized in the past [37]. Hypertension was the leading morbidity in 2018 compared may be due to the shift in the onset of disease, early screening of chronic conditions, and an increase in awareness of the diseases.
Our findings also have implications for discussions regarding compression of morbidity [5, 37]. While some high-income countries, such as the USA, are experiencing older ages of onset of NCDs, leading to the development of a “compression of morbidity,” it is unclear if this phenomenon extends to other countries, especially LMICs [5–7]. Contrary to trends reported in the USA, our findings demonstrate the possibility of an “expansion of morbidity,” indicated by fewer disease-free years (i.e., younger ages of onset of disease), which, if ages of mortality remain stable (or increase), will result in a larger number of years with disease, disability, and suffering. Thus, the compression of morbidity hypothesis does not seem to be currently operating within the India context. It should also be mentioned that some literature suggests that the compression of morbidity in the USA may not be consistent over time. For example, during 1966–76, expansions of morbidity were observed for visual and hearing impairments among younger adults, for diabetes, musculoskeletal disorders, hypertension, and diseases of the circulatory system among middle age (45–64 years) adults, and for diabetes and circulatory diseases among adults aged 65+ years [38]. Another study also demonstrated expansion of morbidity in the USA over the period 1962–84 [39]. A recent study using data from two age-matched cohorts in 1992 and 2004 from the US Health and Retirement Study using self-reported chronic health conditions found no evidence of compression (or expansion) of morbidity [7]. Future research should continue investigating this question using alternate measures of morbidity, including diverse contexts and populations, and incorporating ages of death.
We acknowledge the following limitations of the study. First, due to data limitations, we could not examine genetic, biological, behavioural, and environmental factors that may affect the age of onset of NCDs. For instance, obesity, physical inactivity, poor diet, tobacco, and alcohol use are risk factors known to be associated with NCDs [40, 41] but were not collected as part of the NSS. Second, we have examined only two widely separated time points, and trend analyses would shed more light on morbidity pattern. The sample size did not permit state-level analyses. We could not analyse stroke as no specific categorisation was available. Third, though majority of diseases are classified as per NCDs, there are a few exceptions due to data limitation.
Our findings have important implications for a number of ongoing programmes in India, including the National Program for Prevention and Control of Cancer, Diabetes, CVD, and Stroke (NPCDCDS), the National Mental Health Programme (NMHP), and the National Programme for Health Care of the Elderly (NPHCE). Recently, the Government of India prepared the National Multispectral Action Plan, 2017–22, for prevention and control of NCDs, which aims to promote synergies among various programmes within the health sector and integrate with non-health stakeholders [24]. The National Health Policy 2017 is particularly focused on increasing budgetary allocations and improving the public sector tertiary centre for prevention, treatment, and control of NCDs [24]. The recent introduction of Ayushman Bharat scheme aimed to provide health insurance coverage of up to 5 lakh rupees to the bottom 40% of households is the largest such initiative in the world [42]. Yet, the coverage of these prevention strategies remains low, particularly for poor and rural populations. The treatment of NCDs in private health centres is expensive, so strengthening the social and policy framework would help meet the needs of poor households [43]. Thus, we recommend continued, strong political commitment, increased budgetary spending, and generating awareness of preventive measures among the general population in order to prevent early onset of NCDs.
Supplementary information
(DOCX 845 kb)
Compliance with ethical standards
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval/informed consent
Study used preexisting and de-identified data; formal approval from the ethics committee is not required. Informed consent not applicable.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Sanjay K. Mohanty, Email: sanjayiips@yahoo.co.in
Justin Rodgers, Email: jrogers@hsph.harvard.edu.
Rajeev R. Singh, Email: rajeevs210@gmail.com
Radhe Shyam Mishra, Email: radheshyammishra111@gmail.com.
Rockli Kim, Email: rocklikim@korea.ac.kr.
Junaid Khan, Email: statjun@gmail.com.
Priyamadhaba Behera, Email: priya.madhaba@gmail.com.
S. V. Subramanian, Email: svsubram@hsph.harvard.edu
References
- 1.World Health Organization. Noncommunicable Diseases Country Profiles 2018. World heal. Organ. 2018.
- 2.Forouzanfar MH, Afshin A, Alexander LT, Biryukov S, Brauer M, Cercy K, et al. Global, regional, and national comparative risk assessment of 79 behavioural, environmental and occupational, and metabolic risks or clusters of risks, 1990–2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet. 2016;388:1659–1724. doi: 10.1016/S0140-6736(16)31679-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cao B, Bray F, Ilbawi A, Soerjomataram I. Effect on longevity of one-third reduction in premature mortality from non-communicable diseases by 2030: a global analysis of the Sustainable Development Goal health target. Lancet Glob Heal [Internet]. The Author(s). Published by Elsevier Ltd. This is an Open Access article under the CC BY-NC-ND 4.0 license; 2018;6:e1288–96. Available from: 10.1016/S2214-109X(18)30411-X [DOI] [PubMed]
- 4.Mahal A, Karan A, Engelgau M. The economic implications of non-communicable disease for India. 2010.
- 5.Fries J. The compression of morbidity the finite life span. Milbank Q Publ by Blackwell Publ Repr from Milbank Meml Fund Q. 2005;83:801–823. doi: 10.1111/j.1468-0009.2005.00401.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Beltrán-Sánchez H, Razak F, Subramanian S V. Going beyond the disability-based morbidity definition in the compression of morbidity framework. Glob Health Action. 2014;7. [DOI] [PMC free article] [PubMed]
- 7.Beltrán-Sánchez H, Jiménez MP, Subramanian SV. Assessing morbidity compression in two cohorts from the health and retirement study. J Epidemiol Community Health. 2016;70:1011–1016. doi: 10.1136/jech-2015-206722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mirelman AJ, Rose S, Khan JA, Ahmed S, Peters DH, Niessen LW, et al. The relationship between non-communicable disease occurrence and poverty – evidence from demographic surveillance in Matlab, Bangladesh. Health Policy Plan. 2016;31:785–792. doi: 10.1093/heapol/czv134. [DOI] [PubMed] [Google Scholar]
- 9.Allen L, Williams J, Townsend N, Mikkelsen B, Roberts N, Foster C, et al. Poverty and risk factors for non-communicable diseases in developing countries: a systematic review. Lancet. 2016;388:S17. doi: 10.1016/S0140-6736(16)32253-X. [DOI] [Google Scholar]
- 10.Abegunde DO, Mathers CD, Adam T, Ortegon M, Strong K. The burden and costs of chronic diseases in low-income and middle-income countries. Lancet. 2007;370:1929–1938. doi: 10.1016/S0140-6736(07)61696-1. [DOI] [PubMed] [Google Scholar]
- 11.Islam SMS, Purnat TD, Phuong NTA, Mwingira U, Schacht K, Fröschl G. Non communicable diseases (NCDs) in developing countries: a symposium report. Glob Health. 2014;10:81. doi: 10.1186/s12992-014-0081-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gowshall M, Taylor-Robinson SD. The increasing prevalence of non-communicable diseases in low-middle income countries: the view from Malawi. Int J Gen Med. 2018;11:255–264. doi: 10.2147/IJGM.S157987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Chen S, Kuhn M, Prettner K, Bloom DE. The macroeconomic burden of noncommunicable diseases in the United States: estimates and projections. PLoS One. 2018;13:1–14. doi: 10.1371/journal.pone.0206702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Nikolic IA, Stanciole AE, Zaydman M. Chronic emergency : why NCDs matter – Health Nutrition and Population (HPN) discussion paper [Internet]. 2011. Available from: http://siteresources.worldbank.org/%5CnHEALTHNUTRITIONANDPOPULATION/Resources/281627-%5Cn1095698140167/ChronicEmergencyWhyNCDsMatter.pdf. Accessed 16 Nov 2019, 17:52:29
- 15.Bennett JE, Stevens GA, Mathers CD, Bonita R, Rehm J, Kruk ME, Riley LM, Dain K, Kengne AP, Chalkidou K, Beagley J, Kishore SP, Chen W, Saxena S, Bettcher DW, Grove JT, Beaglehole R, Ezzati M. NCD countdown 2030: worldwide trends in non-communicable disease mortality and progress towards Sustainable Development Goal target 3.4. Lancet. 2018;392:1072–1088. doi: 10.1016/S0140-6736(18)31992-5. [DOI] [PubMed] [Google Scholar]
- 16.Niessen LW, Mohan D, Akuoku JK, Mirelman AJ, Ahmed S, Koehlmoos TP, et al. Tackling socioeconomic inequalities and non-communicable diseases in low-income and middle-income countries under the Sustainable Development agenda. Lancet. 2018;391:2036–2046. doi: 10.1016/S0140-6736(18)30482-3. [DOI] [PubMed] [Google Scholar]
- 17.Bloom DE, Cafiero-Fonseca ET, Candeias V, Adashi E, Bloom L, Gurfein L, et al. Economics of non-communicable diseases in India – a report by the World Economic Forum and the Harvard School of Public Health. World Econ Forum Harvard Sch Public Heal [Internet]. 2014;64. Available from: http://www.sciencedirect.com/science/article/pii/S0305750X9800059X/5Cn. http://www.jstor.org/stable/4405541%5Cn. http://documents.worldbank.org/curated/en/2010/10/12932732/prevention-control-selected-chronic-ncds-sri-lanka-policy-options-action/5Cn.http://mail. Accessed 20 Nov 2019, 13:52:30
- 18.Dandona L, Dandona R, Kumar GA, Shukla DK, Paul VK, Balakrishnan K, Swaminathan S. Nations within a nation: variations in epidemiological transition across the states of India, 1990–2016 in the Global Burden of Disease Study. Lancet. 2017;390(10111):2437–2460. doi: 10.1016/S0140-6736(17)32804-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.ICMR PI. India: health of the nation’s states: the India state-level disease burden initiative. New Delhi, 2017.
- 20.Engelgau MM, Karan A, Mahal A. The economic impact of non-communicable diseases on households in India. Glob Health. 2012;8:9–12. doi: 10.1186/1744-8603-8-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kastor A, Mohanty SK. Disease-specific out-of-pocket and catastrophic health expenditure on hospitalization in India: do Indian households face distress health financing? PLoS One. 2018;13:1–18. doi: 10.1371/journal.pone.0196106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Pandey A, Anil Kumar G, Dandona R, Dandona L. Variations in catastrophic health expenditure across the states of India: 2004 to 2014. PLoS One. 2018;13:1–15. doi: 10.1371/journal.pone.0205510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Pandey A, Ploubidis GB, Clarke L, Dandona L. Trends in catastrophic health expenditure in India: 1993 to 2014. Bull World Health Organ. 2018;96:18–28. doi: 10.2471/BLT.17.191759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.MoHFW. National Health Policy 2017. New Delhi, India. 2017 https://mohfw.gov.in/sites/default/files/9147562941489753121.pdf. Accessed 20 Jan 2020, 14:52:22
- 25.Srivastava RK, Bachani D. Burden of NCDs, policies and programme for prevention and control of NCDs in India. Indian J. Community Med. 2011. [DOI] [PMC free article] [PubMed]
- 26.Srivastav S, Mahajan H, Goel S, Mukherjee S. Prevalence of risk factors of noncommunicable diseases in a rural population of district Gautam-Budh Nagar, Uttar Pradesh using the World Health Organization STEPS approach. J Fam Med Prim Care. 2017;6:491. doi: 10.4103/2249-4863.222027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Subramanian S, Gakunga R, Kibachio J, Gathecha G, Edwards P, Ogola E, et al. Cost and affordability of non-communicable disease screening, diagnosis and treatment in Kenya: patient payments in the private and public sectors. PLoS One. 2018;13:1–16. doi: 10.1371/journal.pone.0190113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Huffman MD, Rao KD, Pichon-Riviere A, Zhao D, Harikrishnan S, Ramaiya K, Ajay VS, Goenka S, Calcagno JI, Caporale JE, Niu S, Li Y, Liu J, Thankappan KR, Daivadanam M, van Esch J, Murphy A, Moran AE, Gaziano TA, Suhrcke M, Reddy KS, Leeder S, Prabhakaran D. A cross-sectional study of the microeconomic impact of cardiovascular disease hospitalization in four low- and middle-income countries. PLoS One. 2011;6:e20821. doi: 10.1371/journal.pone.0020821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kjeldsen SE, Julius S, Mancia G, McInnes GT, Hua T, Weber MA, Larochelle P. Effects of valsartan compared to amlodipine on preventing type 2 diabetes in high-risk hypertensive patients: the VALUE trial. J Hypertens. 2006;24(7):1405–1412. doi: 10.1097/01.hjh.0000234122.55895.5b. [DOI] [PubMed] [Google Scholar]
- 30.Capistrant BD, Berkman LF, Glymour MM. Does duration of spousal caregiving affect risk of depression onset? Evidence from the Health and Retirement Study. Am J Geriatr Psychiatry. 2014;22(8):766–770. doi: 10.1016/j.jagp.2013.01.073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.NSSO . Morbidity, health care and the condition of the aged. Report No 507 (60/25.0/1) New Delhi: Ministry of Statistics and Programme Implementation, Government of India; 2006. [Google Scholar]
- 32.NSSO (2019). Health in India. Report No 586 (75/25.0). New Delhi: Ministry of Statistics and Programme Implementation, Government of India: 2019.
- 33.Cox BDR. Regression models and life-tables Author ( s ): D. R. Cox Source : Journal of the Royal Statistical Society. Series B ( Methodological ), Vol. 34 , No. 2 Published by : Blackwell Publishing for the Royal Statistical Society Stable URL : http://www.js. Society. 2009;34:187–220. Accessed 25 Feb 2020, 15:55:06
- 34.Arokiasamy P India’s escalating burden of non-communicable diseases. Lancet Glob Heal. The Author(s). Published by Elsevier Ltd. This is an Open Access article under the CC BY-NC-ND 4.0 license; 2018;6:e1262–3. Available from: 10.1016/S2214-109X(18)30448-0 [DOI] [PubMed]
- 35.Nethan S, Sinha D, Mehrotra R. Non communicable disease risk factors and their trends in India. Asian Pac J Cancer Prev. 2017;18:2005–2010. doi: 10.22034/APJCP.2017.18.7.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Beaglehole R, Bonita R, Horton R, Adams C, Alleyne G, Asaria P, et al. Priority actions for the non-communicable disease crisis. Lancet. 2011;377:1438–1447. doi: 10.1016/S0140-6736(11)60393-0. [DOI] [PubMed] [Google Scholar]
- 37.Cai L, Lubitz J. Was there compression of disability for older Americans from 1992 to 2003? Demography. 2007;44(3):479–495. doi: 10.1353/dem.2007.0022. [DOI] [PubMed] [Google Scholar]
- 38.Colvez A, Blanchet M. Disability trends in the United States population 1966-76: analysis of reported causes. Am. J. Public Health. 1981;71(5):464–71. [DOI] [PMC free article] [PubMed]
- 39.Rothenberg R, Lentzner HR, Parker RA. Population aging patterns: The expansion of mortality. J. Geronto. 1991;46(2):S66–S70. [DOI] [PubMed]
- 40.Allen L, Cobiac L, Townsend N. Quantifying the global distribution of premature mortality from non-communicable diseases. J. Public Health, 2017;39(4):698-703. [DOI] [PubMed]
- 41.Patel V, Chatterji S, Chisholm D, Ebrahim S, Gopalakrishna G, Mathers, C., ... & Reddy KS. Chronic diseases and injuries in India. The Lancet, 2011;377(9763), 413-428. [DOI] [PubMed]
- 42.Bakshi H, Sharma R, Kumar P. Ayushman Bharat initiative (2018): What we stand to gain or lose! Indian J. Community Med. 2018. P. 63–6. [DOI] [PMC free article] [PubMed]
- 43.Tim Adair. Progress towards reducing premature NCD mortality. The Lancet Global Health 2018;6(12):e1254–e1255. [DOI] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOCX 845 kb)