Highlights
-
•
Infectious complication following chimeric antigen receptor T-cell (CAR-T) therapy is not uncommon.
-
•
Our case illustrated significant findings of acute invasive fungal rhinosinusitis (AIFR) from Fusarium species after CAR-T therapy.
-
•
The diagnosis of AIFR is usually challenging due to unrecognized clinical presentation leading to significant morbidity.
Keywords: Chimeric antigen receptor, Neutropenia, Invasive fungal rhinosinusitis, Fusarium
Abstract
Chimeric antigen receptor T-cell (CAR-T) therapy is a novel treatment for various types of hematologic malignancy. We presented a case of refractory diffuse large B cell lymphoma patient who developed acute invasive fungal rhinosinusitis (AIFR) from Fusarium species after CAR-T therapy. Our photos illustrated the classic clinical, endoscopic, and histopathologic findings of AIFR.
Case illustrated
A 64-year-old male with a history of refractory diffuse large B cell lymphoma presented with a two-week history of new hard palate lesion and epistaxis. One month before presentation, he underwent chimeric antigen receptor T cell (CAR-T) therapy after failing salvage chemotherapy regimens. Post-CAR-T, he required tocilizumab and high dose steroid for cytokine release and hemophagocytic lymphohistiocytosis syndrome. Antifungal prophylaxis was fluconazole. Physical examination revealed a left circular lesion at the hard palate (Fig. 1) with signs of inflammation. Computed Tomography scan demonstrated a dense material at the right nasal cavity extending into the ethmoid sinuses and maxillary sinus. Subsequently, nasal endoscopy revealed black necrotic area at the middle turbinate (Fig. 2). Biopsies from left hard palate and nasal cavity lesions were obtained (Fig. 3). The diagnosis of acute invasive fungal rhinosinusitis from Fusarium species was made. The patient underwent extensive surgical resection, in addition to liposomal amphotericin B and voriconazole.
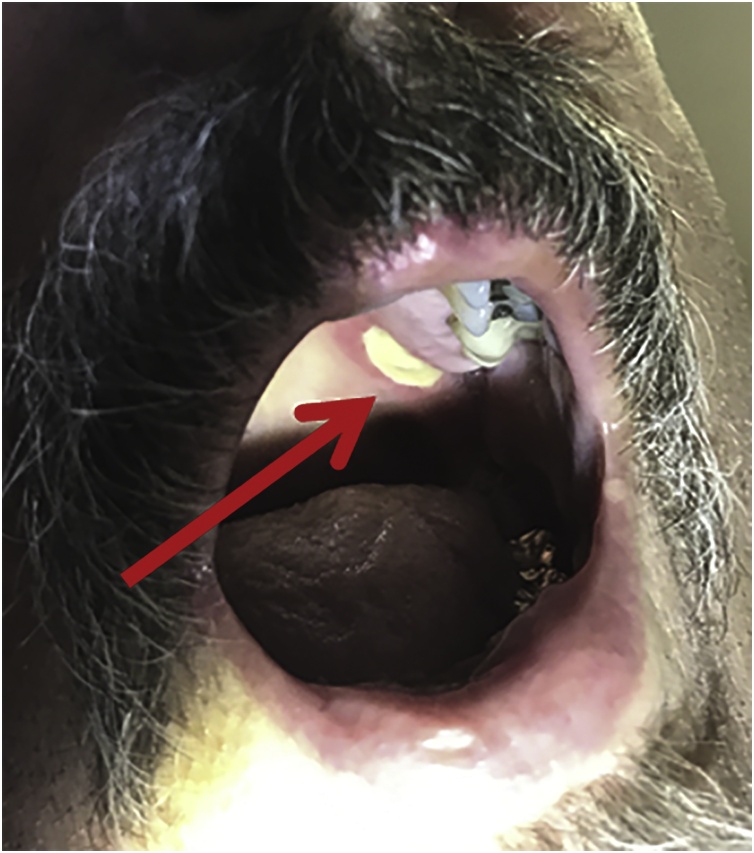
Fig. 1.
Physical examination illustrated a white, one-centimeter circular lesion of the left hard palate.
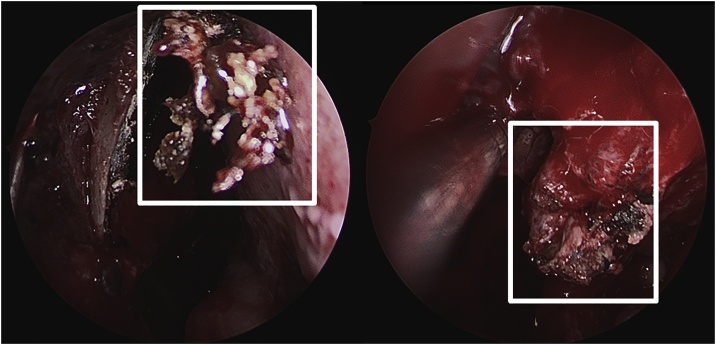
Fig. 2.
Nasal endoscopy revealed black/gray necrotic appearing tissue at the head of the middle turbinate.
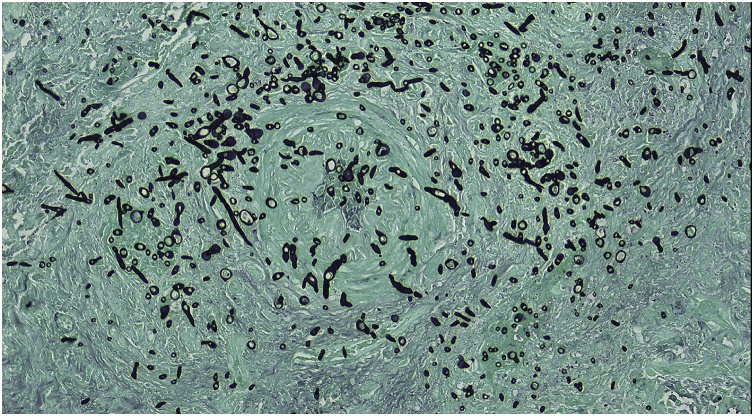
Fig. 3.
Pathology of nasal cavity lesion with Grocott’s methenamine silver (GMS) stain illustrated a filamentous fungus invading blood vessels.
Acute invasive fungal rhinosinusitis (AIFR) is a life-threatening condition. In patients with hematologic malignancies, the severity of neutropenia confers additional risk to develop AIFR [1]. Despite a higher risk of AIFR with chemotherapy and steroids, CAR-T therapy is not typically associated with invasive fungal infections [2]. Our patient had prolonged and severe neutropenia due to chemotherapy. AIFR diagnosis depends on radiographic and histopathologic evidence of invasive fungal infection [3]. In a patient with high clinical suspicion for AIFR, a nasal endoscopy with biopsy should be pursued urgently. The most common causative fungal species of AIFR are Aspergillus, Fusarium, and Mucorales [4]. Surgery is critical for AIFR management and may provide the best survival outcomes [5]. Initial therapy consists of liposomal amphotericin B and voriconazole while awaiting susceptibilities. For immunocompromised patients, neutrophil recovery and immunosuppression reduction are also crucial for clinical recovery. Treatment duration is based mainly on host characteristics, clinical improvement, and extent of surgical resection.
Funding
The authors received no financial support for the publication of this article.
Consent
The authors have the patient's written consent for the publication of this case.
CRediT authorship contribution statement
Supavit Chesdachai: Conceptualization, Methodology, Data curation, Writing - original draft, Writing - review & editing, Project administration. Natalia E. Castillo Almeida: Conceptualization, Data curation, Writing - original draft, Writing - review & editing. Isin Y. Comba: Methodology, Data curation, Writing - review & editing. Prasuna Muppa: Data curation, Visualization, Writing - review & editing. Matthew J. Thoendel: Conceptualization, Methodology, Data curation, Writing - original draft, Writing - review & editing, Project administration, Supervision.
Declaration of Competing Interest
The authors report no declarations of interest.
Contributor Information
Supavit Chesdachai, Email: chesdachai.supavit@mayo.edu.
Matthew J. Thoendel, Email: thoendel.matthew@mayo.edu.
References
- 1.Walsh T.J., Gamaletsou M.N. Treatment of fungal disease in the setting of neutropenia. Hematology Am Soc Hematol Educ Program. 2013;2013(1):423–427. doi: 10.1182/asheducation-2013.1.423. [DOI] [PubMed] [Google Scholar]
- 2.Wudhikarn K., Palomba M.L., Pennisi M. Infection during the first year in patients treated with CD19 CAR T cells for diffuse large B cell lymphoma. Blood Cancer J. 2020;10(8):79. doi: 10.1038/s41408-020-00346-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.deShazo R.D., O’Brien M., Chapin K., Soto-Aguilar M., Gardner L., Swain R. A new classification and diagnostic criteria for invasive fungal sinusitis. Arch Otolaryngol Head Neck Surg. 1997;123(11):1181–1188. doi: 10.1001/archotol.1997.01900110031005. [DOI] [PubMed] [Google Scholar]
- 4.Chang C., Gershwin M.E., Thompson G.R. Fungal disease of the nose and sinuses: an updated overview. Curr Allergy Asthma Rep. 2013;13(2):152–161. doi: 10.1007/s11882-012-0320-1. [DOI] [PubMed] [Google Scholar]
- 5.Roxbury C.R., Smith D.F., Higgins T.S. Complete surgical resection and short-term survival in acute invasive fungal rhinosinusitis. Am J Rhinol Allergy. 2017;31(2):109–116. doi: 10.2500/ajra.2017.31.4420. [DOI] [PubMed] [Google Scholar]