Abstract
Whether meteorological factors influence COVID-19 transmission is an issue of major public health concern, but available evidence remains unclear and limited for several reasons, including the use of report date which can lag date of symptom onset by a considerable period. We aimed to generate reliable and robust evidence of this relationship based on date of onset of symptoms. We evaluated important meteorological factors associated with daily COVID-19 counts and effective reproduction number (Rt) in China using a two-stage approach with overdispersed generalized additive models and random-effects meta-analysis. Spatial heterogeneity and stratified analyses by sex and age groups were quantified and potential effect modification was analyzed. Nationwide, there was no evidence that temperature and relative humidity affected COVID-19 incidence and Rt. However, there were heterogeneous impacts on COVID-19 risk across different regions. Importantly, there was a negative association between relative humidity and COVID-19 incidence in Central China: a 1% increase in relative humidity was associated with a 3.92% (95% CI, 1.98%–5.82%) decrease in daily counts. Older population appeared to be more sensitive to meteorological conditions, but there was no obvious difference between sexes. Linear relationships were found between meteorological variables and COVID-19 incidence. Sensitivity analysis confirmed the robustness of the association and the results based on report date were biased. Meteorological factors play heterogenous roles on COVID-19 transmission, increasing the possibility of seasonality and suggesting the epidemic is far from over. Considering potential climatic associations, we should maintain, not ease, current control measures and surveillance.
Keywords: COVID-19, Temperature, Humidity, Meteorological factor, Two-stage approaches, Time series
1. Introduction
The novel coronavirus disease (COVID-19), caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), has been rapidly spreading across the world. The first case was reported in Wuhan, China in December 2019 (Wu et al., 2020), and the global pandemic, causing huge numbers of infected cases and deaths, was announced on March 11, 2020 by the World Health Organization (WHO). So far, effective vaccines have been developed and used. However, it will take some time to protect the entire global community from SARS-CoV-2 by vaccinating an extraordinarily large number of individuals. Hence, one of the major challenges is to understand what factors can influence the risk of COVID-19 transmission and whether there are seasonal-specific risks. If COVID-19 has the ability to develop into a seasonal disease, understanding the factors that promote seasonality allows public health interventions and capacity to be planned and implemented to reduce disease impact.
Human-to-human transmission of SARS-CoV-2 is thought to occur via (1) direct contact with contaminated surfaces (e.g., skin-to-skin, touching contaminated surfaces and objects), (2) inhalation of exhaled virus in respiratory droplets, and (3) fecal-oral transmission (2020; Ding and Liang, 2020). Abiotic factors such as temperature and relative humidity have been shown to affect airborne the survival of infectious organisms via in-vitro experiments (Tang, 2009). However, the few studies that have been conducted so far with respect to meteorological factors have drawn different, even contradictory, conclusions on their associations with COVID-19 transmission (Liu et al., 2020; Ma et al., 2020; Qi et al., 2020b; Yao et al., 2020; Zhu and Xie, 2020), in terms of which factors are important and the nature of these relationships. The probable reasons for these different conclusions include: 1) diverse study periods: too short (the peak period was excluded), or too long (the epidemic in the descending phase); 2) different hemispheres and regions: these uncertain factors (different control measures and climates vary from region to region) could prevent the effect of meteorological factors on COVID-19 being apparent; 3) spatial scales: mostly based on provincial or national scales; 4) fidelity of meteorological data: mostly based the crude provincial or national average values; and 5) inconsistent modelling approaches. In addition, previous studies used publicly released aggregated COVID-19 datasets based on date of case reports, which includes around a 10-day delay from the date of symptom onset (WHO, 2020). This can potentially cause an important bias, which needs to be carefully addressed. Therefore, the effect of meteorological factors on the spread of COVID-19 remains unclear and the possible effect modification of demographic characteristics (including sex and age) on COVID-19 is unknown.
In this study, we collected information on date of symptom onset and demographic characteristics of COVID-19 cases, and aggregated confirmed cases based on the date of symptom onset instead of the date of case reporting. We used a widely applied standard two-stage time-series modelling approach (Liu et al., 2019) to examine the association between short-term exposure to meteorological factors and COVID-19 risk, and also determined for the first time the modifying effects of sex and age on the association.
2. Materials and method
2.1. Case definitions
The Guidelines on the Diagnosis and Treatment Scheme for COVID-19 patients were officially issued by the National Health Commission of China and the case definitions for suspected, clinically diagnosed and laboratory confirmed cases follows those guidelines; detailed descriptions have been reported in previous studies (Li et al., 2020; Pan et al., 2020; Zhang et al., 2020).
A waiver of informed consent for collecting epidemiological data from patients with COVID-19 was granted by the National Health Commission of China as part of the infectious disease outbreak investigation.
2.2. Data sources
Individual information on COVID-19 cases from December 1, 2019 to March 31, 2020, including age, sex, date of onset of symptoms and report date were retrieved from the official reports of national, provincial and municipal health commissions (Deng et al., 2020; Dong et al., 2020; Pan et al., 2020; Zhang et al., 2020) and news flashes issued by local governments. Daily aggregated counts for each city were calculated − beginning from the onset date of the first case to the epidemic peak − for all the patients and for different subgroups of sex and age (0–64 years and ≥65 years). Furthermore, the effective reproduction number (R t) (Mubayi et al., 2009) defined as the mean number of secondary cases infected by a typical primary case at any specific time in a population where there is some immunity or intervention measures in place, was calculated for each city to measure the transmission rate of SARS-COV-2. Calculations were based on standard SIR disease transmission models analogous to the time-series SIR (TSIR) approach using an algorithm of real time Bayesian estimation (Bettencourt and Ribeiro, 2008). The serial interval (SI) was estimated with a gamma distribution (mean 7.5, SD 3.4 days) (Li et al., 2020).
Meteorological variables including daily relative humidity (%), temperature (mean, minimum and maximum, °C), sunshine hours (h), wind speed (m/s), and rainfall (mm) from November 1, 2019 to March 31, 2020 from 824 monitoring stations were retrieved from the China Meteorological Data Sharing Service System. Missing values (only 0.07%) were imputed using the mean values from the day before and after the day with a missing value at individual weather stations. An ordinary Kriging approach was first applied to interpolate the daily meteorological factors to a surface covering mainland China and then the mean values of meteorological factors were extracted for each city using raster calculation algorithms. Daily temperature range, i.e., the difference between maximum and minimum temperatures, was then calculated to represent the temperature variation. Population data for each city was collected from the China Statistical Yearbook 2018. Road density (China) for each city was calculated as the area of each city divided by the sum of the length of national roads, provincial roads, county roads and highways; this was used as a proxy for traffic conditions.
2.3. Statistical analysis
The associations between meteorological factors and COVID-19 in each city were first assessed with a standard time-series approach and then the region-specific (7 geographical regions based on the comprehensive physical regionalization − North, Northeast, East, South, Central, Southwest, and Northwest China) and national-average associations were calculated via meta analysis.
In the first stage, a quasi-Poisson generalized additive model (GAM) was applied. Considering the validity and stability of the results, only cities with >100 cases were included in the analyses. We calculated the Spearman correlation coefficient matrix among meteorological factors for each city, and the correlation matrices were then pooled by averaging the correlation coefficients. A correlation coefficient threshold of 0.6 (Qi et al., 2018) was used to exclude covariates to avoid multicollinearity. The inclusion of meteorological variables − other than temperature and relative humidity − was assessed using the method of Wald tests. Considering the incubation period of COVID-19 and the impact of meteorological factors on the disease is lagged, the incidence of the disease on a specific day may be influenced by the weather several days before the incidence. So, we used the moving average of meteorological factors to model the lagged effects on the incidence of COVID-19 (Qi et al., 2020a). The optimum lag days and the forms of moving averages (linear or nonlinear) were chosen according to quasi Akaike's information criterion (QAIC). Natural splines of time were also considered to control for the time trend of the COVID-19 incidence, and its optimum degrees of freedom was determined based on QAIC. The GAM is as follows:
where is the daily count of comfirmed cases at day in city , is the expected value of daily count at day in city , is the intercept, denotes the effect of moving average of temperature, is the effect of moving average of relative humidity, and , and are the regression coefficients of natural splines of time with three degrees of freedom.
In the second stage, a random effects meta regression model was used to obtain the national-average associations between meteorological factors and COVID-19 by pooling association estimates across cities, thus accounting for between-city heterogeneity that was tested and quantified with Cochran Q test and I 2 statistic. We applied the above two-stage approach to each of 7 geographical regions to obtain region-specific effect estimates. The formula in the second stage was as followed:
where denotes the effect of temperature or relative humidity of city j in regions in GAM, denotes the overall mean of the effect, is the city-specific effect for city j, and is the random error term.
We also fitted meta regression models with population size, longitude, latitude, road density, and distance from Wuhan as meta predictors to explain the between-city heterogeneity of the effects of meteorological variables on COVID-19. Furthermore, we used the same two-stage approach to estimate the associations between meteorological factors and the R t of COVID-19.
To estimate the overall shape of the association between the meteorological variables and COVID-19 in China, country-level exposure-response curves were plotted by including the chosen variables in the GAM with the natural spline knot set at its median (df = 2).
In addition, stratified analyses were conducted by sex and age group to investigate whether these group variables modify the effects of the association between meteorological factors and COVID-19.
2.4. Sensitivity analysis
The robustness of results was examined through specifying different minimum numbers of cases (80, 120) during the study period to select the cities for modelling, and the daily aggregated count of cases based on the date of reporting instead of the date of symptom onset.
The statistical analyses were performed with mgcv and mixmeta packages in R software, version 3.6.1 (R Foundation for Statistical Computing, Vienna, Austria) and ArcGIS software, version 10.0 (Environmental Systems Research Institute Inc, Redlands, CA, USA). A P-value of less than 0.05 was considered to be statistically significant.
3. Results
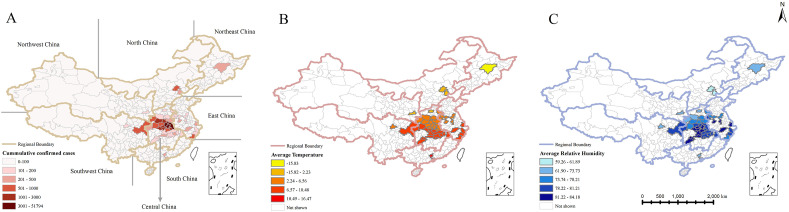
There was a total of 86,576 confirmed cases from December 1 to March 31, 2020 with most cases occurring in the cities of Central and East China. The study periods from December 1 to the epidemic peak (February 15, 2020) were selected in the analysis. Cases from February 15th, 2020 to March 31, 2020 were not included in the analysis due to sparse cases per city per day in this period. A total of 70,836 cases (81.82%) occurred before the epidemic peak. There were 47 cities with >100 cases, varying from 105 (Loudi) to 46,498 (Wuhan), with 93.73% of all confirmed cases reported in Central China (Fig. 1 A). Three quarters of all cases (74.74%) were aged ≤65 years and the male/female sex ratio was 0.97:1.
Fig. 1.
The distribution of (A) cumulative confirmed cases, (B) average temperature, and (C) average relative humidity in 47 cities with case numbers >100 in seven geographic regions in mainland China.
Sunshine hour, temperature range, rainfall and wind speed were excluded due to multilinearity or the Wald test (Table A1). A 14-day moving average (lag 0 to 13) for daily average temperature, a 15-day moving average (lag 0 to 14) for relative humidity (Table A2), and the natural splines of time with 3 degrees of freedom were determined to be optimal according to QAIC (Table A3). The spatial distributions of temperature and relative humidity are shown in Fig. 1B & C, varying from −15.83 °C to 16.47 °C and from 59.26% to 84.18%, respectively (Table A4).
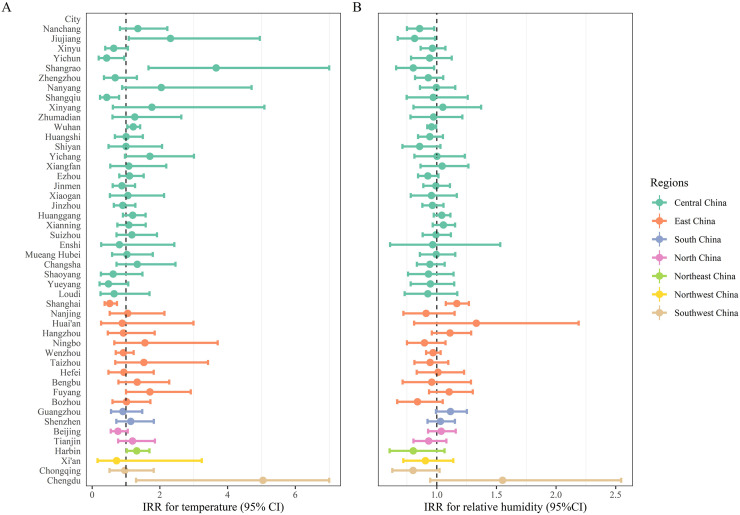
We observed no associations between temperature or relative humidity and the incidence and transmission rate (R t) of COVID-19 nationwide if ignoring potential spatial variations (Table 1 ). However, the associations varied in different cities (Fig. 2 ) and there was considerable spatial heterogeneity across regions, ranging from −28.11% (Northwest China) to 71.6% (Southwest China) of the COVID-19 incidence in association with a 1 °C increase in temperature, and from −19.75% (Northeast China) to 7.25% (South China) in association with a 1% increase in relative humidity. Statistically significant effects of relative humidity on COVID-19 incidence was found in Central China with a −3.92% (95% CI, −5.82% to −1.98%) change per 1% increase in relative humidity. A positive relationship between temperature and the incidence of COVID-19 was found in Harbin, a north-western city, with a 31% (95% CI, 2.02%–68.2%) change per 1 °C increase. However, we neither found a region-specific association between R t and temperature nor between R t and relative humidity (Table 1).
Table 1.
Percentage change of daily count of COVID-19 with one centigrade increase of temperature and one percent increase of relative humidity and the effects on Rt in country-based and region-based scales.
| Variables | Region | Daily count |
I2 (%) | Cochran Q test |
Rt |
||
|---|---|---|---|---|---|---|---|
| Pooled Estimate % (95%CI) | Stat | df | p | Pooled Estimate (95%CI) | |||
| Temperature | Total | 4.08 (−5.82, 15.03) | 47.90 | 88.29 | 46 | <0.01 | −0.03 (−0.11, 0.05) |
| Central China | 5.13 (−8.61, 20.92) | 48.03 | 51.95 | 27 | <0.01 | −0.06 (−0.16, 0.04) | |
| East China | 2.02 (−19.75, 29.69) | 51.52 | 20.63 | 10 | 0.02 | 0.1 (−0.12, 0.32) | |
| North China | −9.52 (−32.29, 20.92) | 61.65 | 2.59 | 1 | 0.11 | 0.52 (−0.24, 1.28) | |
| Northeast China | 31.00 (2.02, 68.2) | – | 0 | 0 | 1 | 0.74 (−0.16, 1.64) | |
| Northwest China | −28.11 (−84.12, 225.44) | – | 0 | 0 | 1 | −0.07 (−0.85, 0.71) | |
| South China | 2.02 (−26.66, 41.91) | 0 | 0.43 | 1 | 0.51 | −0.11 (−0.31, 0.09) | |
| Southwest China | 71.6 (−39.35, 385.5) | 78.61 | 4.76 | 1 | 0.03 | 0.33 (−0.22, 0.88) | |
| Relative humidity | Total | −1.98 (−3.92, 0.1) | 32.86 | 68.51 | 46 | 0.02 | −0.02 (−0.04, 0.0001) |
| Central China | −3.92 (-5.82, -1.98) | 0 | 24.12 | 27 | 0.62 | −0.02 (−0.04, 0.001) | |
| East China | 1.01 (−4.88, 7.25) | 56.83 | 23.17 | 10 | 0.01 | −0.02 (−0.06, 0.02) | |
| North China | 0 (−9.52, 10.52) | 21.17 | 1.27 | 1 | 0.26 | −0.01 (−0.11, 0.09) | |
| Northeast China | −19.75 (−38.74, 5.13) | – | 0 | 0 | 1 | −0.29 (−0.64, 0.06) | |
| Northwest China | −9.52 (−28.82, 15.03) | – | 0 | 0 | 1 | −0.01 (−0.11, 0.09) | |
| South China | 7.25 (−1, 16.18) | 0 | 0.92 | 1 | 0.34 | 0.01 (−0.05, 0.07) | |
| Southwest China | 3.05 (−32.97, 58.41) | 81.78 | 5.49 | 1 | 0.02 | 0.04 (−0.08, 0.16) | |
Fig. 2.
Forest plots for IRRs of (A) temperature and (B) relative humidity in the 47 cities with case numbers >100.
Road density explained a small part of the heterogeneity among cities with respect to the effect of temperature, with the related I 2 statistic decreasing from 47.90% to 43.19%. Regarding the effect of relative humidity, population size and road density explained a moderate level of the spatial heterogeneity in the effect of relative humidity − I 2 statistics dropped 10.44% and 14.13%, respectively (Table A5). Region-specific analysis also confirmed their modification effects (Table 1, Table A6).
There were similar region-specific effects of meteorological factors between the genders, but individuals aged ≥65 years tended to be more vulnerable to the impacts of meteorological factors compared to those aged 0–64 years, although most of the differences in effect did not reach statistical significance (Table 2 ).
Table 2.
Percentage change of daily count of COVID-19 with one centigrade increase of temperature and one percent increase of relative humidity by sex and age group.
| Variables | Region | Pooled Estimate (95% CI) |
|||
|---|---|---|---|---|---|
| Male | Female | 0–64 years | ≥65 years | ||
| Temperature | Central China | 9.42 (−1, 20.92) | 7.25 (−4.88, 20.92) | 5.13 (−8.61, 20.92) | 7.25 (−6.76, 23.37) |
| East China | 13.88 (−11.31, 46.23) | −17.3 (−39.35, 12.75) | 4.08 (−16.47, 29.69) | −23.66 (−57.68, 37.71) | |
| North China | −9.52 (−37.5, 31) | −13.06 (−38.74, 23.37) | −3.92 (−28.11, 28.4) | −34.3 (−60.54, 9.42) | |
| Northeast China | 58.41 (18.53, 111.7) | 3.05 (−27.39, 46.23) | 27.12 (−1, 63.23) | 0 (−45.66, 84.04) | |
| Northwest China | −44.01 (−91.95, 289.62) | −16.47 (−89.97, 595.88) | −14.79 (−84.59, 371.15) | −42.31 (−92.79, 361.82) | |
| South China | 23.37 (−21.34, 93.48) | −15.63 (−41.73, 22.14) | 7.25 (−24.42, 52.2) | −35.6 (−66.38, 23.37) | |
| Southwest China | 40.49 (−23.66, 158.57) | 84.04 (−50.34, 582.1) | 52.2 (−51.32, 375.88) | 203.44 (20.92, 661.41) | |
| Relative | Central China | −3.92 (-7.69, -0.1) | −2.96 (-4.88, -1) | −3.92 (-7.69, -0.1) | −4.88 (-8.61, -1) |
| humidity | East China | 0 (−5.82, 6.18) | 2.02 (−5.82, 10.52) | 2.02 (−3.92, 8.33) | −5.82 (−16.47, 6.18) |
| North China | −3.92 (−14.79, 8.33) | 4.08 (−7.69, 17.35) | −1.98 (−11.31, 8.33) | 2.02 (−16.47, 24.61) | |
| Northeast China | −34.95 (-53.23, -9.52) | 4.08 (−29.53, 53.73) | −18.94 (−39.35, 8.33) | −8.61 (−44.01, 49.18) | |
| Northwest China | −3.92 (−28.11, 28.4) | −14.79 (−38.74, 18.53) | −7.69 (−28.11, 18.53) | −13.93 (−38.12, 19.72) | |
| South China | 2.02 (−7.69, 12.75) | 11.63 (1.01, 23.37) | 6.18 (−1.98, 15.03) | 15.03 (−1.98, 34.99) | |
| Southwest China | −1.98 (−33.63, 44.77) | 11.63 (−27.39, 71.6) | −5.82 (−36.24, 39.1) | 31 (−7.69, 85.89) | |
Overall, temperature and relative humidity were associated with daily case counts in an approximately linear fashion without discernible thresholds (Fig A1).
Sensitivity analysis indicated that the results in general were robust. However, the use of aggregated counts based on the date of reporting instead of the date of symptom onset could generate biased results and a higher uncertainty (Table 3 ).
Table 3.
Percentage change of daily count of COVID-19 with one centigrade increase of temperature and one percent increase of relative humidity with respect to the cities with different number of cases (80, 120), and the daily aggregated count of cases based on report date.
| Variables | Region |
Estimate (95%CI) |
||
|---|---|---|---|---|
| Cases>80 | Cases>120 | Report date | ||
| Temperature | Total | 4.08 (−5.82, 15.03) | 5.13 (−4.88, 16.18) | 10.52 (−5.82, 29.69) |
| Central China | 5.13 (−8.61, 20.92) | 7.25 (−4.88, 20.92) | 9.42 (−13.93, 39.1) | |
| East China | 2.02 (−19.75, 29.69) | 3.05 (−21.34, 34.99) | 2.02 (−22.12, 33.64) | |
| North China | −9.52 (−32.29, 20.92) | −9.52 (−32.29, 20.92) | 2.02 (−19.75, 29.69) | |
| Northeast China | 31 (2.02, 68.2) | 31 (2.02, 68.2) | 80.4 (−17.3, 293.54) | |
| Northwest China | −28.11 (−84.12, 225.44) | −28.11 (−84.12, 225.44) | −25.17 (−85.34, 281.9) | |
| South China | 2.02 (−26.66, 41.91) | 2.02 (−26.66, 41.91) | 19.72 (−20.55, 80.4) | |
| Southwest China | 71.6 (−39.35, 385.5) | 71.6 (−39.35, 385.5) | 113.83 (2.02, 348.17) | |
| Relative humidity | Total | −1.98 (−3.92, 0.001) | −1.98 (−3.92, 0.001) | −1.98 (−5.82, 22.14) |
| Central China | −3.92 (-5.82, -1.98) | −2.96 (-4.88, -1) | −2.96 (−8.61, 3.05) | |
| East China | 1.01 (−4.88, 7.25) | 2.02 (−3.92, 8.33) | 6.18 (−1.98, 15.03) | |
| North China | 0 (−9.52, 10.52) | 0 (−9.52, 10.52) | −13.06 (-22.89, -1.98) | |
| Northeast China | −19.75 (−38.74, 5.13) | −19.75 (−38.74, 5.13) | −13.93 (−40.55, 24.61) | |
| Northwest China | −9.52 (−28.82, 15.03) | −9.52 (−28.82, 15.03) | −4.88 (−28.82, 27.12) | |
| South China | 7.25 (−1, 16.18) | 7.25 (−1, 16.18) | 2.02 (−7.69, 12.75) | |
| Southwest China | 3.05 (−32.97, 58.41) | 3.05 (−32.97, 58.41) | −1.98 (−25.17, 28.4) | |
4. Discussion
We examined the associations between short-term exposure to meteorological factors and COVID-19 incidence and transmission rate (R t) based on the date of symptom onset, instead of the date of reporting, which is commonly available. In general, temperature and relative humidity neither showed any effect on the R t of COVID-19 at the national nor at regional scales, but it was associated with COVID-19 incidence in some areas.
In this study, spatial heterogeneity in effects of temperature and relative humidity on COVID-19 incidence was found. Our data showed a negative correlation between relative humidity and COVID-19 incidence in Central China, which is consistent with the results from previous studies (Ahmadi et al., 2020; Juni et al., 2020; Qi et al., 2020b; Ward et al., 2020a, b). Higher relative humidity (Feng et al., 2020) can increase the size of droplets and the deposition fractions, and reduce the transmission distance, while lower relative humidity can increase suspended matter in the atmosphere, thus facilitating virus attachment and creating ideal conditions for its replication and transmission (Casanova et al., 2010; Chan et al., 2011; Tan et al., 2005), which may be related with pollution to human transmission mechanism such as particulate matter can act as virus carrier, promoting its diffusion through the air and low humidity can lead to slower settling of air pollution and longer suspension (E. Bontempi, 2020a, 2020b). However, there was a positive correlation between temperature and COVID-19 incidence in Northeast China, while previous studies showed contradictory results for this association (Al-Rousan and Al-Najjar, 2020; Qi et al., 2020b; Shi et al., 2020). The average temperature was very low (−15.83 °C) in this region. Increased temperature might affect the human immune system and virus activity, leading to an increased infection risk of COVID-19. However, there was no such correlation in other regions with relatively high average temperature (4–22 °C). SARS-CoV-2 (Chin et al., 2020) was found to be highly stable at 4 °C, and can retain viability for over 7 days at temperatures between 4 and 22 °C. This might be the reason for the absence of an association between temperature and COVID-19 incidence in warmer areas. This spatial heterogeneity in the associations between meteorological factors and COVID-19 was also found in another multi-city study (He et al., 2020), but the factors leading to this heterogeneity was not explored. In our study, we found that population size and road density attenuated the effect of relative humidity in the comparison between Central China and East China. A previous study conducted in Iran (Ahmadi et al., 2020) also reported that higher population density and intra-provincial movement were associated with a higher provincial infection rate. The attenuation of the effects of meteorological factors on the incidence of COVID-19 by greater population size and road density highlights the negative effect of person-to-person contacts during this pandemic. The correlation between meteorological factors and infection supports the hypothesis that transmission from person to person might be seasonal, i.e., there is high probability of COVID-19 becoming a seasonal disease, which will affect COVID-19 control strategies. Considering the comparatively low seroprevalence estimated among people so far, China is still at high risk for a resurgence of the SARS-COV-2 epidemic if public health measures are relaxed.
Previous studies (Livadiotis, 2020; Yao et al., 2020) evaluated the relationship between climate variables and R 0 or the exponential growth rate of COVID-19, but produced different results. However, R 0 measures the disease transmission before any control interventions are taken. Since we are interested in temporal changes of meteorological factors in relation to COVID-19 transmission, R t is a more suitable measure in our analysis. The current study is the first to evaluate the relationship between R t and meteorological factors using the standard two-stage time-series approach, providing reliable evidence that at both the national and region scales no notable impacts of temperature and relative humidity on the transmission of COVID-19 were found. This may be due to the favorable meteorological conditions during the epidemic period in China (see their ranges in Table A4).
The association between meteorological factors and COVID-19 incidence was modified by age, but not sex. Elderly people were more susceptible to the impacts of meteorological factors on COVID-19, that might result from immunosenescence, which changes the innate and adaptive immune systems in a number of ways. Studies have documented that patients with severe COVID-19 have low levels of CD4+ and CD8+ T cells, and T-cell immune deficiency (Qin et al., 2016; Wu et al., 2020) can lead to increased susceptibility to infection in the elderly (Alqahtani et al., 2018; Qin et al., 2016). In addition, many older people suffer from chronic diseases such as high blood pressure, diabetes and heart disease, which further weakens the function of the immune system. Older age groups should be paid more attention in the public health response to COVID-19 due to their higher susceptibility to climate variations.
The exposure-response curves justified the rationale for the inclusion of meteorological factors as linear terms in the model. Linear relationships between temperature/relative humidity and COVID-19 mortality were also found in another study from Wuhan. However, non-linear relationships between meteorological factors and the incidence of COVID-19 were also reported in previous studies, which might be due to their use of daily counts based on report date (Liu et al., 2020; Ma et al., 2020; Qi et al., 2020b; Shi et al., 2020; Zhu and Xie, 2020) or a difference in GAM distribution assumptions. More importantly, it is better to use meteorological factors as linear terms to avoid model overfitting due to the short duration of the study period and low variations in meteorological variables. Population density and road density could partly explain the heterogeneity. Other factors like city-specific lockdown policies (Bontempi, 2021) and human global activities (Bontempi, 2020a, Bontempi, 2020b; Bontempi et al., 2020) could also contributed to this heterogeneous role.
Through sensitivity analysis, significant changes in the results were found for the data aggregated based on report date, providing the first evidence that results could be biased if publicly reported COVID-19 datasets are used, since a 10-day lag exists between these two dates (WHO, 2020). Hence, we should be cautious with the conclusions from studies conducted based on report date.
This study has several limitations. First, COVID-19 case definitions changed several times over the study period, which might have an impact on the estimate of effect. However, new uncertainties will be introduced if efforts are made to correct the data. Second, we only considered the most important factors − such as population size and road density − in the model to explain spatial heterogeneity since this is complicated to do and worthy of further study. Finally, the monitoring results of meteorological factors were used as proxies, which might not accurately represent the personal exposure levels and be influenced by the utilization of air conditioner, humidifier and ventilation systems. Unfortunately, we were unable to measure true exposure accurately in these Chinese cities, so we could not determine the direction of the bias and its impact on our conclusions.
5. Conclusion
Temperature and relative humidity show heterogeneous impacts on COVID-19 risk across regions, which can be explained partly by population size and road density. A negative association between relative humidity and COVID-19 incidence was found in Central China, suggesting that regions that experience periods of low humidity are potentially at greater risk of SARS-CoV-2 transmission. Before the effective vaccine global promotion, social quarantine and personal protection measurements, especially for high-risk populations such as older people, need to be maintained in the high risk regions for COVID-19.
Authors’ contributions
Shuang Xiao, Ying Qin: Data curation, Methodology, Software, Visualization, Writing – original draft; Hongchao Qi: Methodology, Software, Writing – original draft, Formal analysis; Michael P. Ward: Writing – review & editing, Methodology, Validation; Wenge Wang: Data curation, Software, Validation, Investigation; Jun Zhang: Data curation, Investigation; Yue Chen: Writing – review & editing, Methodology, Validation; Robert Bergquist: Writing – review & editing, Methodology, Validation; Wei Tu: Writing – review & editing, Methodology, Validation; Runye Shi: Data curation, Software, Validation; Jie Hong: Data curation, Software, Validation; Qing Su: Data curation, Software, Validation; Zheng Zhao: Data curation, Software, Validation; Jianbo Ba: Writing – review & editing, Methodology, Validation; Zhijie Zhang: Supervision, Funding acquisition.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgement
This research was supported by the Major Project of Scientific and Technical Winter Olympics from National Key Research and Development Program of China(2021YFF0306000), National Major Infectious Disease Project of the Ministry of Science and Technology of China (2017ZX10305501002), Public Health Talents Training Program of Shanghai Municipality (GWV-10.2-XD21), the National Natural Science Foundation of China (81973102) and Key projects of the PLA logistics Scientific research Program (BHJ17J013).
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.envres.2021.111182.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- Ahmadi M., et al. Investigation of effective climatology parameters on COVID-19 outbreak in Iran. Sci. Total Environ. 2020;729:138705. doi: 10.1016/j.scitotenv.2020.138705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Al-Rousan N., Al-Najjar H. The correlation between the spread of COVID-19 infections and weather variables in 30 Chinese provinces and the impact of Chinese government mitigation plans. Eur. Rev. Med. Pharmacol. Sci. 2020;24:4565–4571. doi: 10.26355/eurrev_202004_21042. [DOI] [PubMed] [Google Scholar]
- Alqahtani F.Y., et al. Prevalence of comorbidities in cases of Middle East respiratory syndrome coronavirus: a retrospective study. Epidemiol. Infect. 2018;147:1–5. doi: 10.1017/S0950268818002923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bettencourt L.M., Ribeiro R.M. Real time bayesian estimation of the epidemic potential of emerging infectious diseases. PloS One. 2008;3 doi: 10.1371/journal.pone.0002185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bontempi E. Commercial exchanges instead of air pollution as possible origin of COVID-19 initial diffusion phase in Italy: more efforts are necessary to address interdisciplinary research. Environ. Res. 2020;188:109775. doi: 10.1016/j.envres.2020.109775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bontempi E. First data analysis about possible COVID-19 virus airborne diffusion due to air particulate matter (PM): the case of Lombardy (Italy) Environ. Res. 2020;186:109639. doi: 10.1016/j.envres.2020.109639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bontempi E. The europe second wave of COVID-19 infection and the Italy “strange” situation. Environ. Res. 2021;193:110476. doi: 10.1016/j.envres.2020.110476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bontempi E., et al. Understanding COVID-19 diffusion requires an interdisciplinary, multi-dimensional approach. Environ. Res. 2020;188:109814. doi: 10.1016/j.envres.2020.109814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Casanova L.M., et al. Effects of air temperature and relative humidity on coronavirus survival on surfaces. Appl. Environ. Microbiol. 2010;76:2712–2717. doi: 10.1128/AEM.02291-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chan K.H., et al. The effects of temperature and relative humidity on the viability of the SARS coronavirus. Adv Virol. 2011;2011:734690. doi: 10.1155/2011/734690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chin A.W.H., et al. Stability of SARS-CoV-2 in different environmental conditions. Lancet Microbe. 2020;1:e10. doi: 10.1016/S2666-5247(20)30003-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deng X., et al. Case fatality risk of the first pandemic wave of novel coronavirus disease 2019 (COVID-19) in China. Clin. Infect. Dis. 2020 doi: 10.1093/cid/ciaa578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ding S., Liang T.J. Is SARS-CoV-2 also an enteric pathogen with potential fecal–oral transmission? A COVID-19 virological and clinical review. Gastroenterology. 2020;159:53–61. doi: 10.1053/j.gastro.2020.04.052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dong E., et al. An interactive web-based dashboard to track COVID-19 in real time. Lancet Infect. Dis. 2020;20:533–534. doi: 10.1016/S1473-3099(20)30120-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Diagnosis and Treatment Protocol of COVID-19 (the 6th Tentative Version), 2020.
- Feng Y., et al. Influence of wind and relative humidity on the social distancing effectiveness to prevent COVID-19 airborne transmission: a numerical study. J. Aerosol Sci. 2020;147:105585. doi: 10.1016/j.jaerosci.2020.105585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- He Z., et al. medRxiv; 2020. Meteorological Factors and Domestic New Cases of Coronavirus Disease (COVID-19) in Nine Asian Cities: A Time-Series Analysis. [Google Scholar]
- Juni P., et al. Impact of climate and public health interventions on the COVID-19 pandemic: a prospective cohort study. CMAJ (Can. Med. Assoc. J.) 2020;192:E566–E573. doi: 10.1503/cmaj.200920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li Q., et al. Early transmission dynamics in wuhan, China, of novel coronavirus-infected pneumonia. N. Engl. J. Med. 2020;382:1199–1207. doi: 10.1056/NEJMoa2001316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu C., et al. Ambient particulate air pollution and daily mortality in 652 cities. N. Engl. J. Med. 2019;381:705–715. doi: 10.1056/NEJMoa1817364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu J., et al. Impact of meteorological factors on the COVID-19 transmission: a multi-city study in China. Sci. Total Environ. 2020;726:138513. doi: 10.1016/j.scitotenv.2020.138513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Livadiotis G. Statistical analysis of the impact of environmental temperature on the exponential growth rate of cases infected by COVID-19. PloS One. 2020;15 doi: 10.1371/journal.pone.0233875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ma Y., et al. Effects of temperature variation and humidity on the death of COVID-19 in Wuhan, China. Sci. Total Environ. 2020;724:138226. doi: 10.1016/j.scitotenv.2020.138226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mubayi A., et al. 2009. The Control Reproduction Number and Case-Underreporting of Visceral Leishmaniasis in Bihar. (India) [Google Scholar]
- Pan A., et al. Association of public health interventions with the epidemiology of the COVID-19 outbreak in wuhan, China. J. Am. Med. Assoc. 2020;323:1–9. doi: 10.1001/jama.2020.6130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qi H., et al. Impact of meteorological factors on the incidence of childhood hand, foot, and mouth disease (HFMD) analyzed by DLNMs-based time series approach. Infect Dis Poverty. 2018;7:7. doi: 10.1186/s40249-018-0388-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qi H., et al. Quantifying the risk of hand, foot, and mouth disease (HFMD) attributable to meteorological factors in East China: a time series modelling study. Sci. Total Environ. 2020;728:138548. doi: 10.1016/j.scitotenv.2020.138548. [DOI] [PubMed] [Google Scholar]
- Qi H., et al. COVID-19 transmission in Mainland China is associated with temperature and humidity: a time-series analysis. Sci. Total Environ. 2020;728:138778. doi: 10.1016/j.scitotenv.2020.138778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qin L., et al. Aging of immune system: immune signature from peripheral blood lymphocyte subsets in 1068 healthy adults. Aging (Albany NY) 2016;8:848–859. doi: 10.18632/aging.100894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shi P., et al. Impact of temperature on the dynamics of the COVID-19 outbreak in China. Sci. Total Environ. 2020;728:138890. doi: 10.1016/j.scitotenv.2020.138890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tan J., et al. An initial investigation of the association between the SARS outbreak and weather: with the view of the environmental temperature and its variation. J. Epidemiol. Community Health. 2005;59:186–192. doi: 10.1136/jech.2004.020180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tang J.W. The effect of environmental parameters on the survival of airborne infectious agents. J. R. Soc. Interface. 2009;6(Suppl. 6):S737–S746. doi: 10.1098/rsif.2009.0227.focus. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ward M.P., et al. Humidity is a consistent climatic factor contributing to SARS-CoV-2 transmission. Transbound Emerg Dis. 2020 doi: 10.1111/tbed.13766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ward M.P., et al. The role of climate during the COVID-19 epidemic in New South Wales, Australia. Transbound Emerg Dis. 2020 doi: 10.1111/tbed.13631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- WHO . 2020. Report of the WHO-China Joint Mission on Coronavirus Disease 2019 (COVID-19) [Google Scholar]
- Wu J., et al. Nowcasting and forecasting the potential domestic and international spread of the 2019-nCoV outbreak originating in Wuhan, China: a modelling study. Lancet 395, 689-697. Lancet. 2020;395:689–697. doi: 10.1016/S0140-6736(20)30260-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yao Y., et al. No association of COVID-19 transmission with temperature or UV radiation in Chinese cities. Eur. Respir. J. 2020;55 doi: 10.1183/13993003.00517-2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang J., et al. Evolving epidemiology and transmission dynamics of coronavirus disease 2019 outside Hubei province, China: a descriptive and modelling study. Lancet Infect. Dis. 2020;20:793–802. doi: 10.1016/S1473-3099(20)30230-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhu Y., Xie J. Association between ambient temperature and COVID-19 infection in 122 cities from China. Sci. Total Environ. 2020:138201. doi: 10.1016/j.scitotenv.2020.138201. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.