Most state-of-the-art CT scanners have some type of iterative reconstruction program that allows for lower patient radiation exposure. At my institution we use it, when available, for most neuroimaging studies. Six levels in 100 CT iterative reconstruction studies were compared with conventional CT obtained previously in the same patients. SNR and CNR were computed and the studies were blindly and qualitatively evaluated. The results showed that iterative reconstruction studies had lower image noise and increased low-contrast resolution while allowing lower radiation doses without affecting spatial resolution.
Abstract
BACKGROUND AND PURPOSE:
To safeguard patient health, there is great interest in CT radiation-dose reduction. The purpose of this study was to evaluate the impact of an iterative-reconstruction algorithm, ASIR, on image-quality measures in reduced-dose head CT scans for adult patients.
MATERIALS AND METHODS:
Using a 64-section scanner, we analyzed 100 reduced-dose adult head CT scans at 6 predefined levels of ASIR blended with FBP reconstruction. These scans were compared with 50 CT scans previously obtained at a higher routine dose without ASIR reconstruction. SNR and CNR were computed from Hounsfield unit measurements of normal GM and WM of brain parenchyma. A blinded qualitative analysis was performed in 10 lower-dose CT datasets compared with higher-dose ones without ASIR. Phantom data analysis was also performed.
RESULTS:
Lower-dose scans without ASIR had significantly lower mean GM and WM SNR (P = .003) and similar GM-WM CNR values compared with higher routine-dose scans. However, at ASIR levels of 20%–40%, there was no statistically significant difference in SNR, and at ASIR levels of ≥60%, the SNR values of the reduced-dose scans were significantly higher (P < .01). CNR values were also significantly higher at ASIR levels of ≥40% (P < .01). Blinded qualitative review demonstrated significant improvements in perceived image noise, artifacts, and GM-WM differentiation at ASIR levels ≥60% (P < .01).
CONCLUSIONS:
These results demonstrate that the use of ASIR in adult head CT scans reduces image noise and increases low-contrast resolution, while allowing lower radiation doses without affecting spatial resolution.
The use of CT is increasing rapidly at a rate of approximately 10% per year, and >68 million CT studies were performed in the United States during 2008.1–3 The foremost concern with the increasing use of CT technology is the associated dose of ionizing radiation and the potential risk of cancer development later in life.1 The situation is even more worrisome in the pediatric population, which is at greater risk than adults from a given dose of radiation.1 However, dose reduction in CT is hindered by the increased image noise in lower radiation-dose protocols by using the current FBP reconstructions.
CT imaging demands the development of more efficient reconstruction techniques to diminish radiation dose. Iterative reconstruction techniques promise to drastically reduce image noise and artifacts, thereby allowing significant dose reduction. Most of these techniques are computationally intensive and require long reconstruction times. The most comprehensive iterative-reconstruction algorithm models the system optics by taking into account the finite size of the pixel and the focal spot as well as the shape and size of the detector-cell spacing. In addition, it also models the photon statistics in x-ray attenuation. ASIR (GE Healthcare, Chalfont St. Giles, UK) is a modified iterative-reconstruction technique that is time-efficient and already clinically available. It models the photon statistics in x-ray attenuation but does not model the system optics. Thus, it is more computationally complex than FBP but considerably less computationally complex than more comprehensive iterative-reconstruction methods.3 This technique produces significant noise reduction that potentially improves image quality and allows reduction in radiation dose. High levels of ASIR processing create image texture (smooth appearance) and noise characteristics unfamiliar to radiologists.3,4 In clinical practice, one can use variably blended images created with FBP and ASIR techniques to produce different levels of ASIR.
The purpose of this study was to evaluate the impact of ASIR on both qualitative and quantitative measures of image quality in reduced-dose head CT scans for adult patients. Our hypothesis was that the use of ASIR decreases CT image noise resulting in increased SNR and CNR ratios as well as improved qualitative scores of contrast resolution without compromising spatial resolution. We evaluated its effect on quantitative and qualitative measures of brain image quality in adult reduced-dose head CT scans at multiple ASIR levels in comparison with regular-dose CT studies.
Materials and Methods
Patient Selection
Institutional review board approval was obtained for this retrospective analysis of CT datasets, and Health Insurance Portability and Accountability Act−compliant practices were used during this study. We selected 100 consecutive non-contrast reduced-dose adult head CT studies performed during April and May 2009 for all indications by using a 64-section Discovery CT750HD CT scanner (GE Healthcare) with ASIR reconstruction capability. These were compared with 50 consecutive regular-dose adult head CT scans obtained on the same scanner during March 2009 before the availability of ASIR. A total of 150 CT scans were obtained from 140 patients. Ten patients had scans with reduced- and regular-dose techniques.
Image Acquisition
One hundred scans obtained on the ASIR-capable scanner were acquired by using a reduced-dose protocol. Imaging parameters for these studies were as follows: 120 kV, fixed tube current of 200 mA (140 mAs), pitch of 0.531:1, table speed of 10.62, gantry rotation speed of 0.7 seconds, CTDIvol of 49.7 mGy (reported on the scanner console), FOV of 22 cm, and matrix of 512 × 512. The scanning raw data were used for FBP (standard kernel) reconstruction, which was blended with varying degrees of the ASIR algorithm (0%, 20%, 40%, 60%, 80%, and 100%). This blending is a linear combination of FBP and ASIR images, depending on the percentage of ASIR chosen (eg, 30% ASIR would be a blend of 30% ASIR and 70% FBP images). The 50 head CTs performed on the same scanner before ASIR availability were performed at a relatively higher radiation dose in keeping with our routine clinical protocols with imaging parameters as follows: 120 kV, fixed tube current of 250 mA (175 mAs), pitch of 0.531:1, table speed of 10.62, gantry rotation speed of 0. 7 seconds, CTDIvol of 66.51 mGy, FOV of 22 cm, and matrix of 512 × 512 with a standard FBP kernel. Images were reconstructed as 5-mm-thick contiguous sections.
CT Radiation-Dose Calculation
The CTDIvol of a single CT section of both protocols (low and higher routine doses) was reported on the basis of scanner output (dose report), which is a fixed number when a fixed tube current is used in the protocol. The average DLP, calculated as the CTDIvol multiplied by the scan length (section thickness × number of sections) in centimeters was also reported. The ED DLP can be estimated from the DLP, which is reported on most CT systems: ED (mSv) = k × DLP. The conversion factor (k) for adult head is 0.0021.5
Phantom Study
A phantom study was performed independently from the assessment of clinical CT scans. The effect of ASIR on image noise, low contrast resolution, and high contrast resolution was evaluated by using an ACR CT phantom following recommended guidelines.6,7 Phantom raw data were acquired by using FBP reconstruction (with a standard kernel) blended with varying degrees of ASIR algorithm (0%–100%, 10 blending levels) by using reduced-dose and higher routine radiation dose CT protocols. CNR was assessed quantitatively following ACR guidelines.6,7 CNR measurements were compared between the reduced-dose and routine higher-dose protocols and among different ASIR levels. We also qualitatively assessed high contrast resolution comparing the identification of high-resolution bar patterns between the reduced-dose and routine higher radiation dose groups and with different levels of ASIR. This blinded assessment was performed by 2 experienced neuroradiologists (M.H.L. and S.R.P.).
Clinical CT Dataset Analysis
CT attenuation measurements were acquired by using circular ROIs placed in normal deep GM (lentiform nucleus) and adjacent normal WM structures (internal capsule) by using soft-tissue algorithm brain images. ROIs were slightly adjusted to fit the measured anatomic structure to avoid volume-averaging artifacts. SNR, defined as mean attenuation (in Hounsfield units) divided by the SD8 was calculated for each ROI. We calculated CNR, defined as the difference in mean attenuation for 2 regions divided by the square root of the sum of their variance,8 comparing GM with adjacent WM (GM-WM CNR). The ratio of the intensity of a signal to the intensity of the noise (SNR) indicates the quality of the signal intensity within an anatomic region, and CNR indicates the capability of differentiating tissues of different electron attenuation in relation to the background noise.
The qualitative analysis was performed in 10 cases that had head CT studies by using both reduced- and regular-dose techniques.
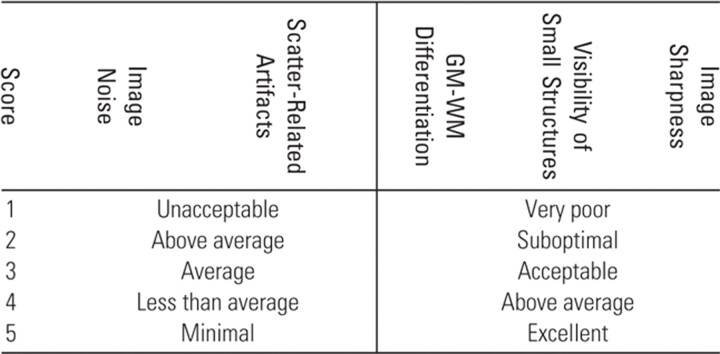
Anonymized image datasets were created at 0%, 30%, 60%, and 100% ASIR levels. The blinded qualitative visual analysis of these datasets was performed by 2 experienced board-certified neuroradiologists (O.R. and S.R.P). The reviewers were blinded to the radiation dose and reconstruction algorithm. Evaluation parameters and the 5-point grading system are summarized in Table 1.
Table 1:
Evaluation parameters and 5-point grading system
Statistical Analysis
ANOVA was used to determine statistical significance among the reduced-dose subgroups at each ASIR level and for determination of the statistical significance of differences in SNR and CNR measurements between the routine higher-dose non-ASIR datasets and the reduced-dose datasets at each ASIR level. A nonparametric Kruskal-Wallis test was used to determine statistical significance for the qualitative analysis data (Table 2).
Table 2:
Summary of image-reconstruction subgroups and statistical analysis
| Clinical CT Datasets |
Statistical Analysis for GM-SNR, WM-SNR, and GM-WM CNR | ||
|---|---|---|---|
| Protocol | Image Reconstruction | ||
| Routine dose (n = 50) | 100% FBP | Control group | Dunnett multiple comparison test |
| Reduced dose (n = 100) | 100% FBP | Repeated-measures ANOVA | |
| 80% FBP + 20% ASIR | |||
| 60% FBP + 40% ASIR | |||
| 40% FBP + 60% ASIR | |||
| 20% FBP + 80% ASIR | |||
| 100% ASIR | |||
All values were expressed as means ± standard error of the mean. STATA software Version 10.0 (StataCorp, College Station, Texas) was used for statistical analysis.
Results
Patient Demographics
A total of 150 adult patients were included; 100 were scanned by using a reduced-dose head CT protocol (mean age, 64 ± 1.69 years; range, 21–93 years; 39 men, 61 women), and 50 patients underwent routine higher-dose head CT scans as a part of their clinical evaluation (mean age, 65 ± 2.49 years; range, 23–89 years; 21 men, 29 women).
There was no significant difference in mean age (unpaired t test, P = .35) between the groups.
CT Radiation Dose
The CTDIvol of a single CT section at 140 mAs (reduced-dose group: fixed tube current of 200 mA at 0.7 s/rotation) and 175 mAs (routine higher-dose group: fixed tube current of 250 mA at 0.7 s/rotation) was 49.07 and 66.51 mGy, respectively. The average DLP and the ED at 140 mAs (reduced-dose protocol) were 932.25 ± 11.46 mGy.cm and 1.95 ± 0.02 mSv; the same values at 175 mAs (routine higher-dose protocol) were 1270.34 ± 24.46 mGy.cm and 2.66 ± 0.05 mSv, respectively (Tables 3 and 4). The total dose in the reduced-dose group was approximately 26.2% lower compared with the routine higher-dose protocol (based on CTDIvol).
Table 3:
Acquisition parameters of routine and lower-dose CT groups
| Radiation Dose | Reconstruction Technique | CTDIvol(mGy)a | DLP (mGy.cm) | Effective Dose (mSv) |
|---|---|---|---|---|
| Regular dose (175 mAs) | 100% FBP | 66.51 | 1270.34 ± 24.46 | 2.66 ± 0.05 |
| Lower dose (140 mAs) | 100% FBP | 49.7 | 932.25 ± 11.46 | 1.95 ± 0.02 |
| 20% ASIR + 80% FBP | ||||
| 40% ASIR + 60% FBP | ||||
| 60% ASIR + 40% FBP | ||||
| 80% ASIR + 20% FBP | ||||
| 100% ASIR |
Clinical scans were below the recommended ACR levels (CTDIvol) of 75 mGy.20
Table 4:
Statistical differences (P values) between the regular- and lower-dose CT groups
| Radiation Dose | Reconstruction Technique | Quantitative Measurements (P values) |
||
|---|---|---|---|---|
| GM-SNR | WM-SNR | GM-WM CNR | ||
| Regular (175 mAs) | 100% FBP | Control group | ||
| 100% FBP | .003a | .003a | .4 | |
| 20% ASIR + 80% FBP | .649 | .541 | 1 | |
| Lower-Dose (140 mAs) | 40% ASIR + 60% FBP | .302 | .668 | .03a |
| 60% ASIR + 40% FBP | <.0001a | <.0001a | <.0001a | |
| 80% ASIR + 20% FBP | <.0001a | <.0001a | <.0001a | |
| 100% ASIR | <.0001a | <.0001a | <.0001a | |
Statistical significance between the lower-dose (with different ASIR/FBP levels) and regular-dose groups.
Phantom Results
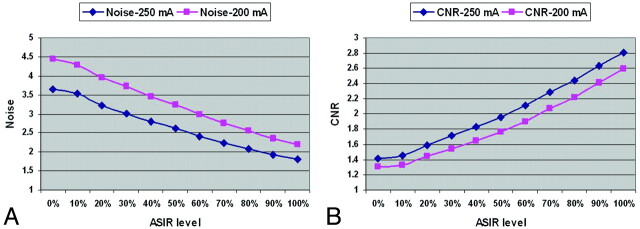
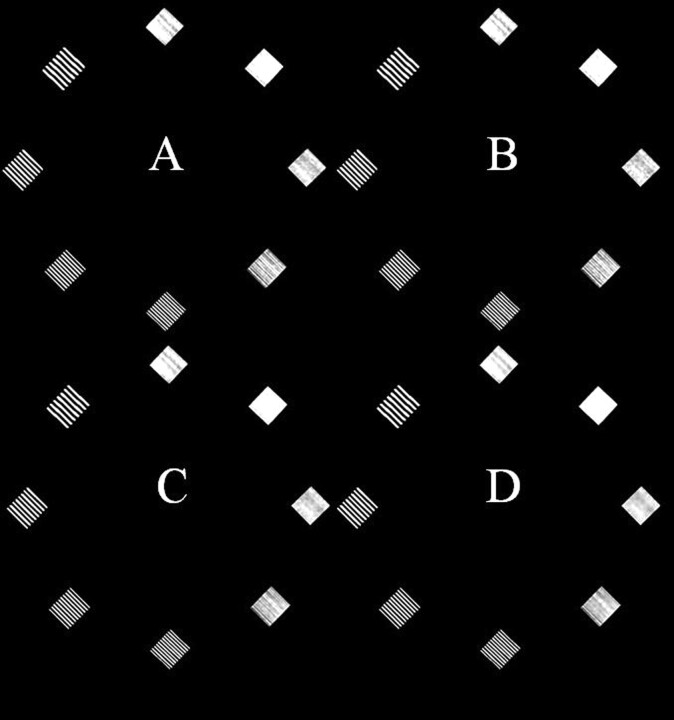
Noise measurements showed a gradual decrease in image noise with higher ASIR levels with both protocols (reduced-dose and higher routine radiation dose protocols) (Fig 1A). Noise measurements at a 30%–40% ASIR level with the reduced-dose technique were comparable with the higher routine radiation dose protocol without ASIR (Fig 1A). CNR progressively increased with higher ASIR levels in both the reduced-dose and higher routine-dose groups. CNR values were comparable between reduced-dose scans at 20%–30% ASIR and routine higher-dose scans without ASIR. Reduced-dose scans with >30% ASIR levels resulted in higher CNR in comparison with routine higher-dose scans without ASIR (Fig 1B). For the assessment of high-contrast resolution, ≤7 lp/cm bar patterns were resolved (higher than the required 5 lp/cm bar pattern based on ACR CT phantom guidelines). There were no differences in the identification of these high-contrast-resolution bar patterns between the reduced-dose (with different levels of ASIR blending) and higher routine-dose groups (Fig 2).
Fig 1.
ACR phantom quantitative study.7 A, Noise-level comparison between lower-dose and routine higher-dose protocols at different ASIR levels. Lower dose (200 mA) images at an ASIR level of 30% have image noise comparable with that of routine higher-dose (250 mA) scans without ASIR. B, CNR analysis. Lower-dose scans at an ASIR level of 20% have CNR comparable with that of routine higher-dose scans without ASIR.
Fig 2.
High-contrast-resolution assessment by using the ACR phantom.7 CT images obtained at a regular dose without ASIR (A), at a lower dose without ASIR (B), and at a lower dose with 60% (C) and 100% (D) of ASIR blending demonstrate the effect of different ASIR levels and the lower-dose technique in comparison with the regular-dose technique on high-contrast-resolution bar patterns. There are no apparent differences in the ability to discriminate individual bar patterns between these techniques.
Clinical CT Dataset Analysis
Quantitative Assessment.
The mean ROI area for GM and WM was 38.85 ± 1.25 mm2. The mean GM and WM attenuation values for the reduced-dose group (140 mAs) were 34.5 and 24.2 HU, respectively, and for the routine higher-dose group (175 mAs), they were 35.5 and 25.6 HU, respectively.
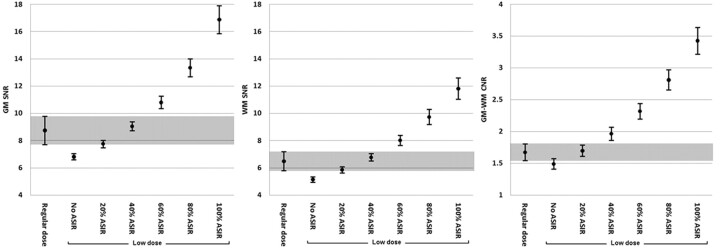
There was a significant increase in GM and WM SNR with increasing ASIR levels in the reduced-dose subgroups (P < .01, repeated-measures ANOVA) (Fig 3). GM-SNR and WM-SNR increased from 6.61 ± 0.11 and 5.06 ± 0.11, respectively, in the reduced-dose without ASIR subgroup to 16.87 ± 0.52 and 11.81 ± 0.39 in the reduced-dose with 100% ASIR subgroup (P < .0001) (Fig 3). Mean GM-SNR and WM-SNR in adult head CTs at 175 mAs (higher-dose) were 7.94 ± 0.20 and 6.22 ± 0.14, respectively, which were not significantly different from the mean GM-SNR and WM-SNR of scans acquired at 140 mAs (reduced-dose) with ASIR level of 20% and 40% (ANOVA, Dunnett multiple comparison test). The SNR values in the routine higher-dose group were significantly lower compared with reduced-dose scans with ≥60% ASIR blending (all P < .0001) and significantly higher when ASIR was not applied in the reduced-dose group (all P = .003) (Tables 3 and 4).
Fig 3.
Comparison of average SNR and CNR values between regular- and lower-dose (with variable ASIR) groups. GM-SNR (left), WM-SNR (middle), and GM-WM CNR (right) measurements are plotted in the y-axis. The x-axis depicts the regular-dose group (without ASIR) and different lower-dose subgroups with increasing ASIR levels (0%–100%). Shaded areas demonstrate equivalent average SNR and CNR values between the regular- and lower-dose groups.
There was a progressive increase in GM-WM CNR with increasing ASIR levels in lower-dose subgroups (P < .0001, repeated measures ANOVA). GM-WM CNR increased from 1.48 ± 0.04 in the reduced-dose subgroup with 0% ASIR to 3.42 ± 0.10 at 100% ASIR. Mean CNR between GM and WM for routine higher-dose head CT studies was 1.61 ± 0.05, which was not significantly different from the values in the reduced-dose CT subgroups with ASIR levels of 0% and 20%, but it was significantly lower in comparison with the reduced-dose subgroups with ASIR levels of ≥40% (all P < .0001) (Fig 3).
Qualitative Assessment.
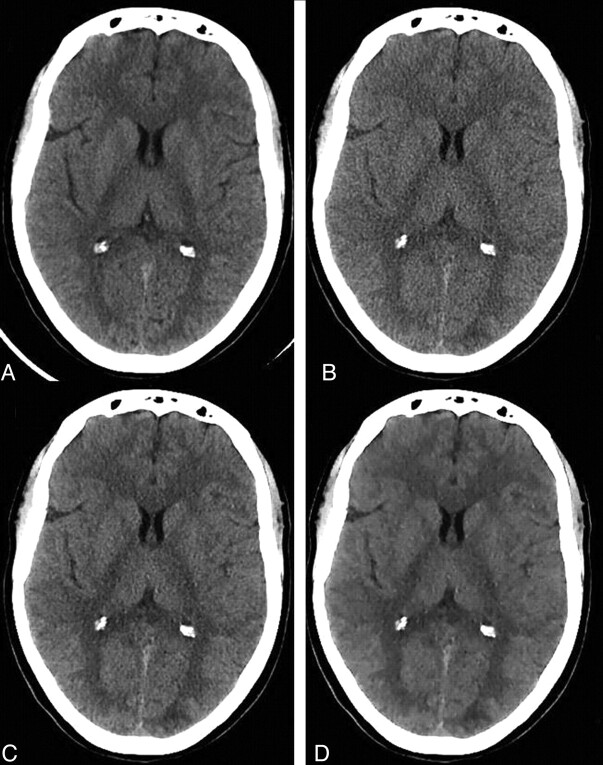
There was a significant decrease in image noise and scatter-related artifacts when applying 60% and 100% ASIR in the lower-dose group in comparison with the regular- and lower-dose groups without ASIR (P < .0001). A statistically significant increase in GM-WM differentiation was noted when using ASIR levels of 60% and 100% in the lower-dose group in comparison with the regular dose and lower-dose groups without ASIR (P < .0001) (Fig 4). The image-quality indices in the routine higher-dose group (175 mAs) were not significantly different from similar indices from scans acquired at 140 mAs (reduced-dose group) with an ASIR level of 30%.
Fig 4.
Examples of nonenhanced head CT images of an adult patient obtained at a regular dose without ASIR (A), a lower dose without ASIR (B), and a lower dose with 60% (C) and 100% (D) of ASIR.
Regarding the visibility of small anatomic structures and image sharpness, there was no statistically significant difference between the lower- (independent of ASIR level) and regular-dose groups (Table 5).
Table 5:
Qualitative assessment of regular-dose and reduced-dose clinical CT datasets with variable ASIR blending using the 5-point grading system
| Radiation Dose | Reconstruction Technique | Noise | Scatter-Related Artifacts | GM-WM Differentiation | Visibility of Small Structures | Image Sharpness |
|---|---|---|---|---|---|---|
| Regular dose (175 mAs) | 100% FBP | 2.80 ± 0.09 | 2.70 ± 0.10 | 2.82 ± 0.12a | 2.85 ± 0.08 | 3.00 ± 0.26 |
| Lower dose (140 mAs) | 100% FBP | 2.10 ± 0.06a | 2.85 ± 0.10 | 2.09 ± 0.11 | 2.82 ± 0.09 | 3.09 ± 0.25 |
| 30% ASIR + 70% FBP | 2.90 ± 0.10 | 3.00 ± 0.07 | 2.90 ± 0.11 | 3.00 ± 0.00 | 3.19 ± 0.24 | |
| 60% ASIR + 40% FBP | 3.70 ± 0.12a | 3.55 ± 0.11a | 3.61 ± 0.12a | 3.05 ± 0.05 | 3.28 ± 0.30 | |
| 100% ASIR | 4.25 ± 0.12a | 3.70 ± 0.14a | 4.00 ± 0.15a | 3.00 ± 0.12 | 3.00 ± 0.39 |
Qualitative assessment: mean scores ± standard error.
Discussion
Iterative methods for reconstruction of CT data are not new, and algebraic iterative-reconstruction algorithms were actually used in the first CT scanners.3,9,10 Mainly due to high computational requirements (approximately 100-1000 times in comparison with FBP algorithms),3 the iterative-reconstruction algorithms were displaced after a few years by the now widely available FBP methods. However, iterative-reconstruction algorithms are very accurate and perform better than the FBP methods in many cases,11–14 particularly when dealing with a small number of projections or noisy datasets.12,15 Iterative reconstruction algorithms have been used more commonly in SPECT and PET imaging.3
Recently, iterative-reconstruction algorithms have become increasingly used in CT imaging due to continuous improvements in computer hardware and software. The use of iterative-reconstruction methods appears to result in significant improvements in overall image quality and noise reduction.4,9,12–19 Our results demonstrate that the use of ASIR improves measurements of SNR and CNR of GM and WM brain structures in reduced-dose head CT scans for adult patients. This effect appears to be related to the noise reduction produced by this type of iterative-reconstruction algorithm.9,12–19 These results were obtained with a commercially available CT scanner with acquisition and postprocessing times similar to those of routine FBP reconstructions on comparable multisection scanners.
The progressive decrease of quantum noise with CT images acquired at progressively higher levels of ASIR blends results in a more uniform appearance.12,15 Consequently, radiologists may perceive these images as overly smooth or “painted,” with concern that critical findings or fine anatomic features may be obscured.4 These perceptions make the switch from FBP to ASIR processing more difficult to accept. Based on our study of adult clinical CT and phantom datasets, there was no apparent compromise of high- and low-contrast resolution with increasing ASIR levels by using a lower-dose technique in comparison with regular-dose datasets (Fig 2).
Additional studies will be helpful for evaluation of the potential effect of this type of iterative-reconstruction algorithm on diagnostic performance, particularly at very high ASIR levels, and for definition of an “optimal” level of ASIR effect, particularly with different section thicknesses. Our findings demonstrate that the use of ASIR levels of 20%–40% on reduced-dose scans (26.2% of dose reduction) by using 5-mm thick images results in quantitative and qualitative indices of image quality comparable with regular-dose scans, and ASIR levels of >40% on reduced-dose scans with similar section thickness result in significant improvement of image-quality indices and noise reduction in comparison with regular-dose scans reconstructed with FBP algorithms.9,12–19 CT images with moderate ASIR levels (eg, 60%) will show the expected benefits of decreased image noise and increased contrast resolution while allowing a lower radiation dose without experiencing the more pronounced smoothing effect seen with higher ASIR levels. Recent studies by using iterative-reconstruction methods (including ASIR) in different anatomic locations have shown similar results with noise reduction and improved image quality at lower radiation levels without compromising diagnostic accuracy.3,9,12–19
One of the limitations of this study is that the reduced-dose and higher routine-dose clinical CT scans were not obtained at the same scanning session due to the fact that these studies were for diagnostic purposes. However, the scans were acquired by using very similar techniques (with the exception of the radiation dose). Another limitation was evident during the qualitative assessment: The readers reviewing the imaging datasets were blinded to the radiation dose and degree of ASIR blending of the CT datasets. However, high ASIR levels have an expected smoothing effect on the appearance of CT images, limiting the blinded status of the readers.
Conclusions
ASIR can produce significant improvements in different qualitative and quantitative aspects of image quality in adult head CT studies, while, at the same time, allowing a significant reduction in radiation exposure.
ABBREVIATIONS:
- ACR
American College of Radiology
- ASIR
Adaptive Statistical Iterative Reconstruction
- CNR
contrast-to-noise ratio
- CTDIvol
volume CT dose index
- DLP
dose-length product
- ED
effective dose
- FBP
filtered back-projection
- GM
gray matter
- HU
Hounsfield unit
- lp
line pair
Footnotes
Disclosures: Joshi Mukta—UNRELATED: Employment: GE Healthcare. Dushyant Sahani—RELATED: Grant: GE Healthcare;* UNRELATED: Payment for Manuscript Preparation: Bracco Diagnostics; Royalties: Elsevier. Michael Lev—RELATED: GE Healthcare,* Comments: research support (software, hardware), Research Assistant support; Consulting Fee or Honorarium: GE Healthcare, Millennium Pharmaceuticals, CoAxia, Comments: consultant. Stuart Pomerantz—RELATED: Grant: GE Healthcare,* Comments: for research assistant support. *Money paid to institution.
References
- 1. Brenner DJ, Hall EJ. Computed tomography: an increasing source of radiation exposure. N Engl J Med 2007;357:2277–84 [DOI] [PubMed] [Google Scholar]
- 2. Boland GW, Guimaraes AS, Mueller PR. The radiologist's conundrum: benefits and costs of increasing CT capacity and utilization. Eur Radiol 2009;19:9–11, discussion 12 [DOI] [PubMed] [Google Scholar]
- 3. Xu J, Mahesh M, Tsui BM. Is iterative reconstruction ready for MDCT? J Am Coll Radiol 2009;6:274–76 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Silva AC, Lawder HJ, Hara A, et al. Innovations in CT dose reduction strategy: application of the adaptive statistical iterative reconstruction algorithm. AJR Am J Roentgenol 2010;194:191–99 [DOI] [PubMed] [Google Scholar]
- 5. McCollough C, Cody D, Edyvean S, et al. The Measurement, Reporting, and Management of Radiation Dose in CT: AAPM Report No. 96. College Park, Maryland: American Association of Physicists in Medicine; 2008. [Google Scholar]
- 6. McCollough CH, Bruesewitz MR, McNitt-Gray MF, et al. The phantom portion of the American College of Radiology (ACR) computed tomography (CT) accreditation program: practical tips, artifact examples, and pitfalls to avoid. Med Phys 2004;31:2423–42 [DOI] [PubMed] [Google Scholar]
- 7. ACR. CT Accreditation Phantom Instruction. 2011. http://www.acr.org/accreditation/computed/qc_forms/Phantom_Testing_Instruction_Final.aspx. 10-10-11 version. Accessed 10 October 2011
- 8. Mullins ME, Lev MH, Bove P, et al. Comparison of image quality between conventional and low-dose nonenhanced head CT. AJNR Am J Neuroradiol 2004;25:533–38 [PMC free article] [PubMed] [Google Scholar]
- 9. Wang G, Yu H, De Man B. An outlook on x-ray CT research and development. Med Phys 2008;35:1051–64 [DOI] [PubMed] [Google Scholar]
- 10. Gordon R, Bender R, Herman GT. Algebraic reconstruction techniques (ART) for three-dimensional electron microscopy and x-ray photography. J Theor Biol 1970;29:471–81 [DOI] [PubMed] [Google Scholar]
- 11. Rogalla P, Kloeters C, Hein PA. CT technology overview: 64-slice and beyond. Radiol Clin North Am 2009;47:1–11 [DOI] [PubMed] [Google Scholar]
- 12. Wang G, Snyder DL, O'Sullivan JA, et al. Iterative deblurring for CT metal artifact reduction. IEEE Trans Med Imaging 1996;15:657–64 [DOI] [PubMed] [Google Scholar]
- 13. Nuyts J, De Man B, Dupont P, et al. Iterative reconstruction for helical CT: a simulation study. Phys Med Biol 1998;43:729–37 [DOI] [PubMed] [Google Scholar]
- 14. Ziegler A, Kohler T, Proksa R. Noise and resolution in images reconstructed with FBP and OSC algorithms for CT. Med Phys 2007;34:585–98 [DOI] [PubMed] [Google Scholar]
- 15. McCollough CH, Primak AN, Braun N, et al. Strategies for reducing radiation dose in CT. Radiol Clin North Am 2009;47:27–40 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Prakash P, Kalra MK, Kambadakone AK, et al. Reducing abdominal CT radiation dose with adaptive statistical iterative reconstruction technique. Invest Radiol 2010;45:202–10 [DOI] [PubMed] [Google Scholar]
- 17. Prakash P, Kalra MK, Digumarthy SR, et al. Radiation dose reduction with chest computed tomography using adaptive statistical iterative reconstruction technique: initial experience. J Comput Assist Tomogr 2010;34:40–45 [DOI] [PubMed] [Google Scholar]
- 18. Marin D, Nelson RC, Schindera ST, et al. Low-tube-voltage, high-tube-current multidetector abdominal CT: improved image quality and decreased radiation dose with adaptive statistical iterative reconstruction algorithm—initial clinical experience. Radiology 2010;254:145–53 [DOI] [PubMed] [Google Scholar]
- 19. Singh S, Kalra MK, Gilman MD, et al. Adaptive statistical iterative reconstruction technique for radiation dose reduction in chest CT: a pilot study. Radiology 2010;259:565–73 [DOI] [PubMed] [Google Scholar]
- 20. ACR. ACR Practice Guideline For Diagnostic Reference Levels in Medical X-Ray Imaging. 2008. http://www.acr.org/SecondaryMainMenuCategories/quality_safety/RadSafety/RadiationSafety/guideline-diagnostic-reference.aspx. Accessed October 1, 2008