Abstract
Objective
There is a two-way relationship between frailty and depression, but the mechanisms by which one may influence the other are not well understood. The objective of this study was to evaluate the relationship between psychosocial factors and frailty in community-dwelling aged populations with depression.
Design
Observational cross-sectional study.
Site
5 primary care centres.
Participants
Community-dwelling subjects with depression aged ≥70 years.
Main measurements
Frailty status was established according to Fried criteria, depression and depression severity were evaluated by DSM-IV criteria and the Hamilton Depression Rating Scale, respectively, and psychosocial factors were assessed using the Gijón Social-Familial Evaluation Scale and ad hoc questionnaires.
Results
Recruited were 338 subjects (mean age 77.2 years), 82% women and 36.1% rated as frail. A dose–response relationship was observed between depression severity and frailty risk. Widowhood was a risk factor for frailty, while a higher educational level, home internet, stairs in the home, and an active social life had a protective effect. A multivariate analysis showed that age, number of drugs, and depression severity were independent risk factors for frailty, while an active social life was a protective factor. The severity of depressive symptoms showed higher association with frailty than other clinical and socio-demographic characteristics.
Conclusions
In depressed elderly subjects, frailty is associated with psychologiocal factors such as the intensity of depressive symptoms and with social factors such as education level, widowhood, loneliness, and limited social life. More research is required to better understand the modifiable psychological risk factors for frailty.
Keywords: Aged, Depression, Educational level, Frailty, Psychological factors, Social factors
Abstract
Objetivo
Existe una relación bidireccional entre la fragilidad y la depresión en la población anciana. El objetivo de este estudio fue evaluar la relación entre los factores psicosociales y la fragilidad en ancianos de la comunidad con depresión.
Diseño
Estudio observacional transversal.
Sitio
Cinco centros de atención primaria.
Participantes
Ancianos ≥ 70 años de la comunidad con depresión.
Principales mediciones
La fragilidad se estableció de acuerdo con los criterios de Fried, la depresión y la gravedad de la depresión se evaluaron mediante los criterios DSM-IV y la Escala de Hamilton, respectivamente, y los factores psicosociales se evaluaron utilizando la Escala de Evaluación Social-Familiar de Gijón y cuestionarios ad hoc.
Resultados
Se reclutaron 338 sujetos (edad media 77 años), 82% mujeres y 36,1% frágiles. Se observó una relación dosis-respuesta entre la gravedad de la depresión y el riesgo de fragilidad. La viudez era un factor de riesgo para la fragilidad, mientras que un nivel educativo más alto, internet en el hogar, escaleras en el hogar y una vida social activa tenían un efecto protector. El análisis multivariado mostró que la edad, el número de medicamentos y la gravedad de la depresión eran factores de riesgo independientes para la fragilidad, mientras que una vida social activa era un factor protector.
Conclusiones
En ancianos con depresión la fragilidad se asocia con factores psicológicos como la intensidad de los síntomas depresivos y con factores sociales como el nivel de estudios, la viudez, la soledad o la escasa vida social. Se requiere más investigación para comprender mejor los factores de riesgo psicológicos modificables de fragilidad.
Palabras clave: Anciano, Depresión, Nivel educativo, Fragilidad, Factores psicológicos, Factores sociales
Introduction
Different studies have reported a strong association between depression and frailty.1, 2, 3, 4 Approximately 35%–40% of elderly people with depression are frail and a similar percentage of frail elderly people are depressed. A recent meta-analysis concludes that there is a two-way relationship between frailty and depression in elderly populations and suggests that interventions aimed at reducing one of these two syndromes may help prevent the other.5 In addition, the coexistence of depression and frailty has been linked to particularly poor health outcomes associated with accelerated cognitive impairment and increased risk of severe disability.6 Some prospective studies show that people with depression are at a higher risk of frailty,7 but the mechanisms by which depression may contribute to frailty are not well known. It is thought that they may be related to certain clinical characteristics of depression (such as the intensity of symptoms or evolution in years); abandonment of physical exercise, good nutrition or other healthy habits; lack of socialization; depression-related anxiety or cognitive disorders in the elderly; or treatments with psychoactive drugs, especially antidepressants.8, 9 A large cohort study has shown that, even in the absence of depression symptoms, antidepressant medication is associated with an increased risk of developing frailty.10 Despite this, depression-related factors associated with frailty are not fully established and most of them need to be corroborated.
The social determinants of health, i.e., the circumstances in which people live, work and age, are related to income distribution and the social policies adopted in each community and, ultimately, explain most inequities in health.11 Some evidence exists regarding the impact of living and household conditions, educational level, loneliness, family support and income on frailty12, 13, 14, 15; however, the relative importance of those psychosocial factors in comparison to clinical factors (somatic or psychological diseases) and any possible interaction between those factors is little understood. A better understanding of the independent effects of psychosocial factors and the mechanisms by which they may favour the frailty process would enable the design of more effective interventions to prevent frailty, disability and dependence in elderly populations. The objective of this study was to evaluate the relationship between psychosocial factors and frailty in community-dwelling elderly people with depression.
Methods
Study design and population
An observational cross-sectional study was performed of community-dwelling subjects aged 70 years and older with depression, pre-selected from the database of five primary care centres in the Maresme region in the province of Barcelona (Catalonia, Spain) with the prior authorization of their physicians. The pre-selected subjects had either a diagnosis of depression or had been prescribed antidepressants according to their electronic clinical record. Pre-selected subjects were invited by telephone to an appointment so that selection criteria could be checked and, if eligible, to be informed about the study and to obtain consent. A person was considered to experience depression: (a) if they had a diagnosis of depression in their primary care clinical history and were on antidepressant treatment for more than three months, or (b) if they were experiencing a major depressive episode, recurring depressive episodes, or a major depressive episode with melancholic symptoms or had a dysthymic disorder according to DSM-IV criteria (assessed using Mini-International Neuropsychiatric Interview (MINI) modules A and B administered by trained physicians). Subjects were excluded if they had active malignancy, dementia (with GDS > 3), or life expectancy of less than six months, were in a palliative care programme or were institutionalized. Recruitment took place from February to November 2018. The Research Ethics Committee of the Maresme Healthcare Consortium (CSdM) approved the study protocol (code CEIC CSdM 64/13). The recruitment visit was carried out by a physician who also recorded the patient's socio-demographic data, co-morbidities and chronic medication. In a period of no more than two weeks, a nurse performed the baseline visit, in which questionnaires were administered and physical examination, functional and frailty assessments were performed.
Study factors and data collection
Subjects were classified, according to the five Fried criteria16 of unintentional weight loss, exhaustion, low physical activity, slow walking speed, and poor hand grip strength, as robust (0 criteria), pre-frail (1 or 2 criteria), or frail (3 or more criteria), translated into Spanish by Serra-Prat.17
The main study factors were as follows:
-
(a)
Clinical characteristics of depression: years since diagnosis, type of depression (major depression, recurrent depression, adaptive depressive reaction, anxiety-depressive adaptation reaction or dysthymia), recurrences, psychiatric admissions, family history of depression, severity of current symptoms, and predominant symptoms according to the Hamilton Depression Rating Scale (HDRS),18, 19 interpreted as follows (maximum score 52): not depressed (0–7), slightly depressed,8, 9, 10, 11, 12, 13 moderately depressed,14, 15, 16, 17, 18 severely depressed,19, 20, 21, 22 and very severely depressed (>23).
-
(b)
Pharmacological treatment of depression: regular treatment with antidepressants, anxiolytics, antiepileptics, acetylcholinesterase inhibitors, and/or antipsychotics.
-
(c)
Presence of anxiety symptoms, as assessed by the HDRS.
-
(d)
Presence of cognitive disorders, as assessed by the Mini Mental State Exam (MMSE).20, 21
-
(e)
Social factors, as assessed by a questionnaire addressing educational level, income, housing conditions and facilities, living circumstances (alone or accompanied), recent widowhood, social relations and networks, out-of-home activities, and social risk according to the Gijón Social-Familial Evaluation Scale (SFES).22
Other study variables included sociodemographic data, co-morbidities, nutritional status, as assessed by the Mini Nutritional Assessment Short-Form questionnaire (MNA-SF),23 physical activity, as assessed by the International Physical Activity Questionnaire (IPAQ),24, 25 and functional capacity assessed by Barthel score.26
Statistical analysis
Accepting an alpha risk of 0.05 and a beta risk of 0.2 in a two-sided test, 103 subjects were necessary in the frail group and 206 in the non-frail group (a 33% prevalence of frailty was assumed in the study population) to find as statistically significant a minimum difference in the prevalence of study factors, expected to be 25% in the frail group and 12% in the non-frail group.
All data were coded and recorded in an electronic database for scrubbing and analysis. Continuous variables were described using means and standard deviations and categorical variables were described using percentages. To assess risk factors for frailty, the robust and pre-frail groups were pooled together in a non-frail group so that frail versus non-frail subjects could be compared. Comparisons between frail and non-frail groups were made using the Chi-square test or Fisher's exact test for categorical variables, and the t-test or Mann–Whitney U test for numerical variables. Odds ratios (OR) and their 95% confidence intervals (CI), estimated using logistic regression, were used as a measure of association between risk factors and frailty. All variables first underwent bivariate analysis and only those significantly associated with frailty (for p < 0.05) were used to fit multivariate models. Statistical significance was established at p < 0.05.
Results
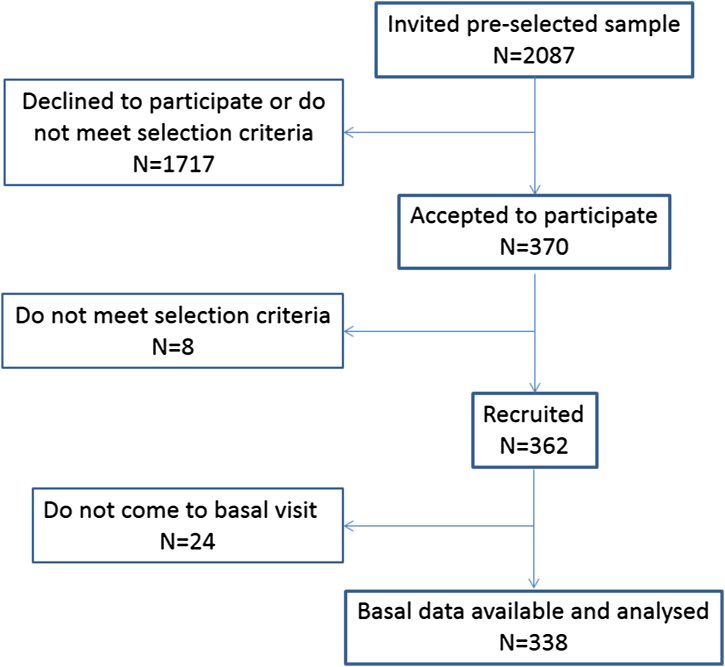
Fig. 1 shows the study flow chart. Recruited were 338 subjects, mean age 77.2 (5.0) years, 277 (82%) women. Nutritional status was generally good (78.2% well nourished) and functional capacity was optimal (97.01 (4.5) mean Barthel score). A third (36.1%, n = 122) were considered frail. Frailty was related with age (76.5 years for non-frail vs 78.2 years for frail subjects; p = 0.002) and with being female (91.8% of women in the frail group vs 76.4% of women in the non-frail group; p < 0.001; OR = 3.46; 95% CI: 1.69–7.10).
Figure 1.
Study flow chart.
Table 1, Table 2 summarize details on the relationship between frailty and different co-morbidities and clinical characteristics and the relationship between frailty and different depression traits, respectively. Highlighted is a dose–response relationship between depression severity (according to the HDRS) and frailty risk. Overall, 67.9% of participants were considered good compliant with prescribed medication and no association was observed between therapeutic compliance and frailty.
Table 1.
Co-morbidities and clinical characteristics associated with frailty.
| Non-frail (n = 216) | Frail (n = 122) | p | OR (95% CI) | |
|---|---|---|---|---|
| Arthritis | 136 (63.8%) | 100 (82.6%) | <0.001 | 2.70 (1.56–4.66) |
| Ischaemic heart disease | 23 (10.8%) | 18 (14.9%) | 0.275 | 1.44 (0.74–2.80) |
| Peripheral vasculopathy | 18 (8.5%) | 23 (19.3%) | 0.004 | 2.59 (1.33–5.04) |
| Stroke | 14 (6.6%) | 12 (10.0%) | 0.274 | 1.563 (0.698–3.5) |
| Parkinson disease | 5 (2.4%) | 4 (3.3%) | 0.599 | 1.43 (0.38–5.42) |
| Chronic bronchitis | 26 (12.2%) | 12 (10.0%) | 0.543 | 0.80 (0.39–1.65) |
| Asthma | 21 (9.9%) | 22 (18.3%) | 0.028 | 2.04 (1.07–3.89) |
| Diabetes | 35 (16.4%) | 36 (29.8%) | 0.004 | 2.15 (1.26–3.67) |
| Chronic renal failure | 28 (13.1%) | 13 (10.7%) | 0.520 | 0.79 (0.39–1.60) |
| Arterial hypertension | 152 (71.4%) | 91 (75.2%) | 0.448 | 1.22 (0.73–2.02) |
| Dyslipidaemia | 114 (53.8%) | 85 (70.2%) | 0.003 | 2.03 (1.26–3.26) |
| Pain (VAS) | 5.57 (3.17) | 7.33 (2.42) | <0.001 | 1.25 (1.14–1.37) |
| Falls last 3 months (n) | 1.66 (1.02) | 2.07 (1.39) | 0.157 | 1.36 (0.89–2.04) |
| ADL (Barthel score) | 98.10 (3.10) | 95.04 (5.80) | <0.001 | 0.84 (0.79–0.89) |
| Medications (n) | 6.34 (3.09) | 9.01 (3.76) | <0.001 | 1.26 (1.17–1.36) |
ADL, activities of daily living; VAS, visual analogue scale.
Table 2.
Clinical features of depression associated with frailty.
| Non-frail (n = 216) | Frail (n = 122) | p | OR (95% CI) | |
|---|---|---|---|---|
| Major depression | 70 (32.9%) | 55 (45.1%) | 0.026 | 1.68 (1.062–2.649) |
| Dysthymia | 47 (22.3%) | 28 (23.1%) | 0.856 | 1.05 (0.617–1.789) |
| Suicide risk | ||||
| None | 154 (73.7%) | 75 (65.2%) | 1 | |
| Low | 48 (23.0%) | 29 (25.2%) | 0.063 | 1.24 (0.725–2.123) |
| Moderate | 5 (2.4%) | 5 (4.3%) | 2.05 (0.577–7.311) | |
| High | 2 (1.0%) | 6 (5.2%) | 6.16 (1.214–31.249) | |
| Family history of depression | 69 (34.2%) | 34 (31.2%) | 0.596 | 0.87 (0.531–1.439) |
| Psychiatric admission | 15 (7.7%) | 12 (11.5%) | 0.269 | 1.56 (0.704–3.482) |
| Cognitive impairment (MMSE) | ||||
| None | 53 (57.6%) | 37 (51.4%) | 1 | |
| Possible | 11 (12.0%) | 14 (19.4%) | 0.408 | 1.823 (0.745–4.459) |
| Mild or moderate | 28 (30.4%) | 21 (29.2%) | 1.074 (0.531–2.173) | |
| Anxiety | 44 (30.1%) | 15 (34.1%) | 0.619 | 1.20 (0.59–2.46) |
| Depression symptoms(HDRS) | ||||
| None (0–7) | 90 (45.5%) | 27 (22.9%) | 1 | |
| Mild (8–13) | 73 (36.9%) | 39 (33.1%) | 1.78 (0.997–3.180) | |
| Moderate (14–18) | 26 (13.1%) | 32 (27.1%) | <0.001 | 4.10 (2.093–8.040) |
| Severe (19–22) | 7 (3.5%) | 12 (10.2%) | 5.71 (2.047–15.951) | |
| Very severe (>23) | 2 (1.0%) | 8 (6.8%) | 13.33 (2.670–66.575) | |
| Years since diagnosisa | 10 (5.0–20.0) | 15 (7.8–23.0) | 0.021 | 1.01 (0.99–1.03) |
| Use of any psychiatric drug | 197 (95.2%) | 118 (98.3%) | 0.142 | 2.995 (0.64–) |
| Use of antidepressants | 169 (82.4%) | 111 (92.5%) | 0.011 | 2.627 (1.218–5.667) |
| Use of anxiolytics | 92 (51.1%) | 64 (59.8%) | 0.152 | 1.424 (0.877–2.311 |
| Use of antiepileptics | 14 (9.0%) | 3 (3.7%) | 0.130 | 0.385 (0.107–1.381) |
| Use of AchEIs | 2 (1.3%) | 1 (1.2%) | 0.963 | 0.944 (0.84–10.574) |
Median and interquartile range.
AchEI, acetylcholinesterase inhibitor; HDRS, Hamilton Depression Rating Scale; MMSE, Mini Mental State Exam.
Table 3 summarizes data on the relationship between social factors and frailty, indicating that widowhood is a risk factor for frailty, while a higher educational level, using the internet, having stairs in the home, and an active social life had a protective effect. The results of the multivariate analysis, presented in Table 4, indicate that age, number of drugs, and depression severity are independent risk factors for frailty, while an active social life exercises an independent protective effect.
Table 3.
Psychosocial factors associated with frailty.
| Non-frail (n = 216) | Frail (n = 122) | p (<0.05) | OR (95% CI) | |
|---|---|---|---|---|
| Living alone | 59 (27.3%) | 39 (32.0%) | 0.365 | 1.250 (0.771–2.029) |
| Marital status | ||||
| Single | 3 (1.4%) | 0 (0%) | ||
| Partnered | 133 (61.6%) | 66 (54.1%) | ||
| Divorced | 16 (7.4%) | 7 (5.7%) | 0.148 | |
| Widowed | 64 (29.6%) | 49 (40.2%) | ||
| Widowhood | 64 (29.6%) | 49 (40.2%) | 0.049 | 1.594 (1.001–2.538) |
| Education | ||||
| No studies | 74 (34.3%) | 66 (54.1%) | 1 | |
| Primary | 95 (44.0%) | 46 (37.7%) | <0.001 | 0.543 (0.335–0.881) |
| Secondary | 27 (12.5%) | 9 (7.4%) | 0.374 (0.164–0.852) | |
| University | 20 (9.3%) | 1 (0.8%) | 0.056 (0.007–0.429) | |
| Income (euros) | ||||
| <12,000 | 47 (22.9%) | 31 (28.2%) | 1 | |
| 12,000–24,000 | 99 (48.3%) | 56 (50.9%) | 0.154 | 0.86 (0.49–1.50) |
| 24,000–50,000 | 52 (25.4%) | 23 (20.9%) | 0.67 (0.34–1.31) | |
| >50,000 | 7 (3.4%) | 0 (0.0%) | 0.00 (0.00–) | |
| Housing | ||||
| Flat | 143 (66.2%) | 94 (77.0%) | 0.036 | 0.584 (0.351–0.969) |
| House | 73 (33.8%) | 28 (23.0%) | ||
| Home elevator | 80 (41.0%) | 61 (52.1%) | 0.056 | 1.566 (0.987–2.484) |
| Home stairs | 66 (30.7%) | 21 (17.6%) | 0.009 | 0.484 (0.278–0.841) |
| Home heating | 162 (75.0%) | 85 (70.2%) | 0.344 | 0.787 (0.479–1.293) |
| Home internet | 114 (53.0%) | 44 (36.4%) | 0.003 | 0.506 (0.321–0.800) |
| Outdooractivities | 79 (36.7%) | 26 (21.3%) | 0.003 | 0.466 (0.279–0.780) |
| Volunteering | 14 (6.5%) | 2 (1.6%) | 0.043 | 0.239 (0.053–1.071) |
| Religious activities | 17 (7.9%) | 9 (7.4%) | 0.861 | 0.928 (0.400–2.150) |
| Social centre attendance | 34 (15.8%) | 15 (12.3%) | 0.378 | 0.746 (0.388–1.434) |
| Choir/theatre/dancing | 13 (6.1%) | 3 (2.5%) | 0.138 | 0.393 (0.110–1.408) |
| Meeting friends | 70 (32.4%) | 13 (10.7%) | <0.001 | 0.249 (0.131–0.473) |
| Other out-of-home activities | 23 (10.8%) | 6 (5.0%) | 0.070 | 0.432 (0.171–1.094) |
| Active social lifea | 135 (65.2%) | 45 (37.8%) | <0.001 | 0.324 (0.203–0.518) |
| Gijón SFES score | ||||
| Good/acceptable (5–9) | 127 (59.3%) | 52 (42.6%) | 1 | |
| Atsome risk (9–14) | 82 (38.3%) | 66 (54.1%) | 0.013 | 1.966 (1.244–3.106) |
| At great risk (>15) | 5 (2.3%) | 4 (3.3%) | 1.954 (0.505–7.566) | |
Any of the above-mentioned activities.
SFES, Social-Familial Evaluation Scale.
Table 4.
Multivariate analysis of independent psychosocial risk factors for frailty in elderly people with depression.
| Multivariate | OR | 95% CI |
|---|---|---|
| Age (years) | 1.071 | 1.010–1.135 |
| Female | 2.945 | 1.164–7.449 |
| Number of drugs | 1.246 | 1.142–1.359 |
| Depression symptoms (HDRS) | ||
| None (0–7) | 1 | 1 |
| Mild (8–13) | 1.701 | 0.835–3.467 |
| Moderate (14–18) | 3.747 | 1.677–8.373 |
| Severe (19–22) | 5.137 | 1.500–17.588 |
| Very severe (>23) | 8.782 | 1.429–53.959 |
| Active social life | 0.361 | 0.202–0.646 |
| Home internet | 0.555 | 0.307–1.003 |
HDRS, Hamilton Depression Rating Scale.
STEPWISE method. Introduced variables: age, gender, number of drugs, major depression, education, HDRS, active social life, home stairs, home internet, widowhood, housing.
Discussion
In community-dwelling elderly subjects with depression, and independently of age, sex and co-morbidity load, we observed that the prevalence of frailty increased as depression severity increases, and decreased with an active social life. No independent relationship was observed between frailty and anxiety, mild cognitive impairment, or the use of psychoactive drugs.
Regarding the clinical characteristics of depression, most (major depression, suicide risk, years since diagnosis, and depression severity) seem to indicate that the greater the exposure to depression, the greater the risk of developing frailty. Our findings agree with those reported by other authors5, 12, 13 but do not resolve the doubt as to whether depression leads to frailty or vice versa – which must of necessity be studied with longitudinal and prospective studies. Although it may seem that both syndromes influence each other mutually and that frailty may worsen depression, three facts support the argument that it is depression which aggravates frailty, namely: (a) the longer the time since diagnosis of depression (i.e., the greater the exposure to depression), the greater the prevalence of frailty; (b) depression usually appears at an earlier age than frailty, and (c) a dose–response relationship exists between depression severity and frailty prevalence. In addition, it is well known that a depressed mood is associated with social isolation, apathy, and abandonment of healthy hygienic-dietary habits, which may, in turn, contribute to decreased physical activity, a poorer nutritional status, muscle weakness and frailty. In community-dwelling elderly people with depression, the intensity of depressive symptoms seems to be the independent factor most strongly associated with frailty, so that the effect of very severe depressive symptoms on frailty is equivalent to the effect of 8 years of age more. These results highlight the importance of psychological management in this population.
On the other hand, frailty in our study was not related to concomitant anxiety or cognitive symptoms, a family history of depression, psychiatric admission, or the use of psychoactive drugs other than antidepressants. Concomitant symptoms and family history of depression do not necessarily have mean greater exposure to depression. The effect of antidepressants disappeared when an adjustment was made for depression severity, suggesting a confounding effect, while eliminating any effect of antidepressants on frailty. Finally, although psychiatric admission could be an indicator of depression severity, the small number of admissions associated with the subjects in our study meant that the statistical power to detect an association with frailty was insufficient. The above data suggest that frailty could be influenced by the intrinsic characteristics of depression and not by any accompanying collateral symptoms or antidepressant treatment.
The causes of depression in aged populations are not yet well understood. Depression has been related to negative life events, deficiencies in certain neurotransmitters, and certain chronic organic conditions, some of which have also been related to frailty, suggesting that depression and fragility may share some risk factors. Cardiovascular diseases,27 diabetes,28, 29 chronic metabolic disorders such as vitamin B12 deficiency, autoimmune diseases such as rheumatoid arthritis and certain cancers, for instance, have been shown to be risk factors for both depression and frailty.30 Depression has also been linked to hormonal changes, most especially in hormones that modulate neuroreceptors in the dopaminergic and serotonergic systems. The main hormonal alterations related to both depression and frailty are low testosterone levels,12, 31 low growth hormone levels,32 and variability in the hypothalamic-pituitary-adrenal axis response to elevated cortisol levels.12, 33 In addition, it has been reported that depression risk, like frailty risk, increases with the number of chronic clinical conditions.17, 30 Health professionals should bear in mind those possible organic and/or co-morbid causes of depression and frailty in their therapeutic approach. Moreover, higher drug use is associated with a higher prevalence of frailty, probably because it indicates a higher load of co-morbidity. Despite this, this study has not been able to deepen into the effect of different medications and their possible side effects on frailty due to lack of statistical power.
As for social factors related with frailty, notable is the fact that an active social life (physical activities, voluntary activities, meeting friends, etc) are strongly, negatively and independently associated with frailty. Although our finding (because of the cross-sectional design of the study) does not answer the question as to whether an inactive social life is a cause or consequence of frailty, it does corroborate previously reported findings that indicate that an outdoor life, visiting friends, feeling helpful to friends or family, and talking with someone every day, all have a strong impact on the risk of future disability among community-dwelling older people.13 We also observed that educational level has a protective effect on frailty. This again corroborates findings reported elsewhere, specifically, that low levels of cultural realization are significantly associated with frailty (independently of functional impairment and low physical activity), and that subjects with higher educational levels run a significantly lower risk of pre-frailty or frailty than subjects with lower educational levels.14, 34 Other studies, however, have reported no significant association.35, 36 Living in a flat instead of in a house was also related with frailty, probably because it indicates a lower socioeconomic level. Having internet in the home had an independent protective effect that can be attributed to both a higher educational level and a more active virtual social life. Other studies have reported that loneliness is a risk factor for frailty, explained by the lack of help and emotional support in daily life.12 Widowhood, strongly associated with frailty in our study, can lead to a more depressed state correlating with greater frailty. As seen in the results of this study, frailty in depressed elderly subjects is related with psychological and social factors, reinforcing the idea that frailty should be managed by a multidisciplinary team involving family physicians, geriatricians, psychiatrists, psychologists, and social workers.
The main limitation of this study is its cross-sectional design, which can only establish associations but not causal relationships, so further longitudinal studies are required to corroborate our findings. Other study limitations include a gender imbalance (a very high proportion of females, probably explained by the higher incidence of depression among women), the frailty assessment using Fried criteria (which only measures physical but not psychological frailty), and a relatively small sample size with limited statistical power.
In summary, this study shows that frailty is a complex process determined by several factors. In addition to age and sex and different organic co-morbidities (diabetes, arthritis, pain), frailty is also associated with psychological factors such as the intensity of depressive symptoms and social factors (education, widowhood, loneliness, limited social life). It seems that depression's influence on frailty results from intrinsic characteristics and clinical manifestations of the former, rather than from its treatment or related factors such as anxiety. The greater the intensity of depressive symptoms, the greater the risk of frailty. Our findings reinforce the idea that frailty must be managed by a multidisciplinary team involving family physicians, geriatricians, psychiatrists, psychologists, nurses, and social workers. Meanwhile, however, more research is required to better understand modifiable psychological risk factors for frailty.
Ethics
The Research Ethics Committee of the Maresme Healthcare Consortium (CSdM) approved the study protocol (code CEIC CSdM 64/13). All participants signed the informed consent form.
What was known?
-
•
There is a strong association between depression and frailty.
-
•
The mechanisms by which depression may contribute to frailty are not well known.
-
•
Educational level, loneliness, family support and income may also influence frailty.
What the study brings?
-
•
The greater the intensity of depressive symptoms, the greater the prevalence of frailty.
-
•
The severity of depressive symptoms shows stronger association with frailty than other clinical and socio-demographic characteristics.
-
•
Frailty is associated with intrinsic characteristics of depression and not with any accompanying collateral symptoms or antidepressant treatment.
Funding
This research was supported by a grant from the Catalan Ministry of Health (PERIS 2017, SLT006/17/56).
Conflict of interest
The authors declare that they have no conflict of interest in relation to this study.
References
- 1.Lohman M., Dumenci L., Mezuk B. Depression and frailty in late life: evidence for a common vulnerability. J Gerontol B Psychol Sci Soc Sci. 2016;71:630–640. doi: 10.1093/geronb/gbu180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Buigues C., Padilla-Sánchez C., Garrido J.F., Navarro-Martínez R., Ruiz-Ros V., Cauli O. The relationship between depression and frailty syndrome: a systematic review. Aging Ment Health. 2015;19:762–772. doi: 10.1080/13607863.2014.967174. [DOI] [PubMed] [Google Scholar]
- 3.De Rui M., Veronese N., Trevisan C., Carraro S., Berton L., Maggi S. Changes in frailty status and risk of depression: results from the progetto veneto anziani longitudinal study. Am J Geriatr Psychiatry. 2017;25:190–197. doi: 10.1016/j.jagp.2016.11.003. [DOI] [PubMed] [Google Scholar]
- 4.Mezuk B., Edwards L., Lohman M., Choi M., Lapane K. Depression and frailty in later life: a synthetic review. Int J Geriatr Psychiatry. 2012;27:879–892. doi: 10.1002/gps.2807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Soysal P., Veronese N., Thompson T., Kahl K.G., Fernandes B.S., Prina A.M. Relationship between depression and frailty in older adults: a systematic review and meta-analysis. Ageing Res Rev. 2017;36:78–87. doi: 10.1016/j.arr.2017.03.005. [DOI] [PubMed] [Google Scholar]
- 6.Fougère B., Daumas M., Lilamand M., Sourdet S., Delrieu J., Vellas B. Association between frailty and cognitive impairment: cross-sectional data from Toulouse frailty day hospital. J Am Med Dir Assoc. 2017;18 doi: 10.1016/j.jamda.2017.06.024. 990.e1–990.e5. [DOI] [PubMed] [Google Scholar]
- 7.Vaughan L., Corbin A.L., Goveas J.S. Depression and frailty in later life: a systematic review. Clin Interv Aging. 2015;10:1947–1958. doi: 10.2147/CIA.S69632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Dent E., Hoogendijk E.O. Psychosocial factors modify the association of frailty with adverse outcomes: a prospective study of hospitalised older people. BMC Geriatr. 2014;14:108. doi: 10.1186/1471-2318-14-108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gale C.R., Westbury L., Cooper C. Social isolation and loneliness as risk factors for the progression offrailty: the English Longitudinal Study of Ageing. Age Ageing. 2018;47:392–397. doi: 10.1093/ageing/afx188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lakey S.L., La Croix A.Z., Gray S.L., Borson S., Williams C.D., Calhoun D. Antidepressant use, depressive symptoms, and incident frailty in women aged 65 and older from the Women's Health Initiative Observational Study. J Am Geriatr Soc. 2012;60:854–861. doi: 10.1111/j.1532-5415.2012.03940.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Braveman P., Gottlieb L. The social determinants of health: it's time to consider the causes of the causes. Public Health Rep. 2014;Suppl. 2:19–31. doi: 10.1177/00333549141291S206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Feng Z., Lugtenberg M., Franse C., Fang X., Hu S., Jin C. Risk factors and protective factors associated with incident or increase of frailty among community-dwelling older adults: a systematic review of longitudinal studies. PLoS One. 2017;12:e0178383. doi: 10.1371/journal.pone.0178383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Makizako H., Shimada H., Tsutsumimoto K., Lee S., Doi T., Nakakubo S. Social frailty in community-dwelling older adults as a risk factor for disability. J Am Med Dir Assoc. 2015;16 doi: 10.1016/j.jamda.2015.08.023. 1003.e7–11. [DOI] [PubMed] [Google Scholar]
- 14.Poli S., Cella A., Puntoni M., Musacchio C., Pomata M., Torriglia D. Frailty is associated with socioeconomic and lifestyle factors in community-dwelling older subjects. Aging Clin Exp Res. 2017;29:721–728. doi: 10.1007/s40520-016-0623-5. [DOI] [PubMed] [Google Scholar]
- 15.Chamberlain A.M., St Sauver J.L., Jacobson D.J., Manemann S.M., Fan C., Roger V.L. Social and behavioural factors associated with frailty trajectories in a population-based cohort of older adults. BMJ Open. 2016;6:e011410. doi: 10.1136/bmjopen-2016-011410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Fried L.P., Tangen C.M., Walston J., Newman A.B., Hirsch C., Gottdiener J. Cardiovascular Health Study Collaborative Research Group. Frailty in older adults: evidence for a phenotype. J Gerontol A Biol Sci Med Sci. 2001;56:M146–M156. doi: 10.1093/gerona/56.3.m146. [DOI] [PubMed] [Google Scholar]
- 17.Serra-Prat M., Papiol M., Vico J., Palomera E., Sist X., Cabré M. Factors associated with frailty in community-dwelling elderly population. A cross-sectional study. Eur Ger Med. 2016;7:531–537. [Google Scholar]
- 18.Hamilton M. A rating scale for depression. J Neurol Neurosurg Psychiatry. 1960;23:56–62. doi: 10.1136/jnnp.23.1.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bobes J., Bulbena A., Luque A., Dal-Ré R., Ballesteros J., Ibarra N.AT Evaluación psicométrica comparativa de las versiones en español de 6, 17 y 21 ítems de la Escala de valoración de Hamilton para la evaluación de la depresión. Med Clin. 2003;120:693–770. doi: 10.1016/s0025-7753(03)73814-7. [DOI] [PubMed] [Google Scholar]
- 20.Folstein M.F., Folstein S.E., McHugh P.R. Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12:189–198. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- 21.Escribano-Aparicio M.V., Pérez-Dively M., García-García F.J., Pérez-Martín A., Romero L., Ferrer G. Validación del MMSE de Folstein en una población española de bajo nivel educativo. Rev Españ Geriatr Gerontol. 1999;34:319–326. [Google Scholar]
- 22.Díaz Palacios M.E., Domínguez Puente O., Toyos-García G. Resultados de la aplicación de una escala de valoración socio familiar en atención primaria. Trab Soc Salud. 1993;16:137–156. [Google Scholar]
- 23.Rubenstein L.Z., Harker J.O., Salva A. Screening for undernutrition in geriatric practice: developing the short-form mini-nutritional assessment (MNA-SF) J Gerontol A Biol Sci Med Sci. 2001;56:M366–M372. doi: 10.1093/gerona/56.6.m366. [DOI] [PubMed] [Google Scholar]
- 24.Craig C.L., Marshall A.L., Sjöström M., Bauman A.E., Booth M.L., Ainsworth B.E. International physical activity questionnaire: 12-country reliability and validity. Med Sci Sports Exerc. 2003;35:1381–1395. doi: 10.1249/01.MSS.0000078924.61453.FB. [DOI] [PubMed] [Google Scholar]
- 25.Rubio Castañeda F.J., Tomás Aznar C., Muro Baquero C. Medición de la actividad física en personas mayores de 65 años mediante el IPAQ-e: validez de contenido, fiabilidad y factores asociados. Rev Españ Sal Públ. 2017;91:1–12. [PubMed] [Google Scholar]
- 26.Bernaola-Sagardui I. Validación del índice de Barthel en la población española. Enferm Clín. 2018;28:210–211. doi: 10.1016/j.enfcli.2017.12.001. [DOI] [PubMed] [Google Scholar]
- 27.Grippo A.J., Johnson A.K. Stress, depression and cardiovascular dysregulation: a review of neurobiological mechanisms and the integration of research from preclinical disease models. Stress. 2009;12:1–21. doi: 10.1080/10253890802046281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Naranjo D.M., Fisher L., Areán P.A., Hessler D., Mullan J. Patients with type 2 diabetes at risk for major depressive disorder over time. Ann Fam Med. 2011;9:115–120. doi: 10.1370/afm.1212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Nouwen A., Winkley K., Twisk J., Lloyd C.E., Peyrot M., Ismail K. European Depression in Diabetes (EDID) Research Consortium. Type 2 diabetes mellitus as a risk factor for the onset of depression: a systematic review and meta-analysis. Diabetologia. 2010;53:2480–2486. doi: 10.1007/s00125-010-1874-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Gunn J.M., Ayton D.R., Densley K., Pallant J.F., Chondros P., Herrman H.E. The association between chronic illness, multimorbidity and depressive symptoms in an Australian primary care cohort. Soc Psychiatry Psychiatr Epidemiol. 2012;47:175–184. doi: 10.1007/s00127-010-0330-z. [DOI] [PubMed] [Google Scholar]
- 31.Seidman S.N., Orr G., Raviv G., Levi R., Roose S.P., Kravitz E. Effects of testosterone replacement in middle-aged men with dysthymia: a randomized, placebo-controlled clinical trial. J Clin Psycho pharmacol. 2009;29:216–221. doi: 10.1097/JCP.0b013e3181a39137. [DOI] [PubMed] [Google Scholar]
- 32.Chihara K., Kato Y., Kohno H., Takano K., Tanaka T., Teramoto A. Safety and efficacy of growth hormone (GH) during extended treatment of adult Japanese patients with GH deficiency (GHD) Growth Horm IGF Res. 2008;18:307–317. doi: 10.1016/j.ghir.2007.12.001. [DOI] [PubMed] [Google Scholar]
- 33.Nandam L.S., Brazel M., Zhou M., Jhaveri D.J. Cortisol and major depressive disorder-translating findings from humans to animal models and back. Front Psychiatry. 2020;10:974. doi: 10.3389/fpsyt.2019.00974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Rodríguez López S., Montero P., Carmenate M. Educational inequalities and frailty in Spain: what is the role of obesity? J Frailty Aging. 2014;3:120–125. doi: 10.14283/jfa.2014.12. [DOI] [PubMed] [Google Scholar]
- 35.Hoogendijk E.O., van Hout H.P., Heymans M.W., van der Horst H.E., Frijters D.H., Broese van Groenou M.I. Explaining the association between educational level and frailty in older adults: results from a 13- year longitudinal study in the Netherlands. Ann Epidemiol. 2014;24:538–544. doi: 10.1016/j.annepidem.2014.05.002. e2. [DOI] [PubMed] [Google Scholar]
- 36.Aranda M.P., Ray L.A., Snih S.A., Ottenbacher K.J., Markides K.S. The protective effect of neighborhood composition on increasing frailty among older Mexican Americans: a barrio advantage? J Aging Health. 2011;23:1189–1217. doi: 10.1177/0898264311421961. [DOI] [PMC free article] [PubMed] [Google Scholar]