Abstract
Background
Although poor-urban (inner-city) areas are thought to have high asthma prevalence and morbidity, we recently found that inner-cities do not have higher prevalent pediatric asthma. Whether asthma morbidity is higher in inner-city areas across the U.S. not known.
Objective
To examine relationships between residence in poor and urban areas, race/ethnicity, and asthma morbidity among children with asthma enrolled in Medicaid.
Methods
Children aged 5–19 enrolled in Medicaid in 2009–2010 were included. Asthma was defined by at least one outpatient or emergency department (ED) visit with a primary diagnosis code of asthma over the 2 year period. Urbanization status was defined at the county level and neighborhood poverty at the zip-code level. Among children with asthma, logistic models were created to examine the effects of urbanization, neighborhood poverty and race/ethnicity on rates of asthma outpatient visits, ED visits and hospitalizations.
Results
16,860,716 children were included (1,534,820 with asthma). Among children enrolled in Medicaid, residence in inner-city areas did not confer increased risk of prevalent asthma in either crude or adjusted analyses, but was associated with significantly more asthma-related emergency room visits and hospitalizations among those with asthma in crude analyses (RR 1.48, 95%CI:1.24–1.36 and 1.97, 95%CI:1.50–1.72, respectively) and when adjusted for race/ethnicity, age and gender (aRR 1.23, 95%CI:1.08–1.15 and 1.62, 95%CI:1.26–1.43). Residence in urban or poor areas, and non-Hispanic black race/ethnicity were all independently associated with increased risk of asthma related emergency room visits and hospitalizations.
Conclusions
Residence in poor and urban areas is an important risk factor for asthma morbidity, but not prevalence, among low-income U.S. children.
Keywords: Urbanization, poverty, inner-city, asthma
Introduction
Since at least the 1960s, researchers have identified poor-urban areas (the “inner-city”) as hotspots of high asthma prevalence and morbidity1,2. Over the past several decades, the National Institutes of Health (NIH) and other public health institutions have focused substantial resources on inner-city areas, usually defined for official purposes as census tracts in large central metro areas with at least 20% of households below the poverty line, in an effort to reduce asthma disparities. However, until recently, there was very little data on the national scale to confirm that inner-city residence is in fact associated with either a higher prevalence of asthma or, among those with asthma, greater asthma morbidity. In a recent analysis of data from the National Health Interview Survey (NHIS), we recently found that residence in inner-city areas was not actually associated with higher prevalence of asthma in children across the U.S.3.
Because the NHIS does not include rates of asthma outpatient visits, emergency room visits or hospitalizations, we were unable to determine whether living in an inner-city was associated with increased morbidity among children with asthma in our previous study. Medicaid, as a federally funded program available to low-income children across the U.S. with central collation of claims data, offers the ability to assess the effect of residence in poor and urban areas among low-income children nationally. Thus, our goal was first to determine whether living in an inner-city is indeed associated with increased morbidity, as assessed by more frequent hospitalizations or emergency department (ED) visits, among low-income children with asthma and if so, whether urbanization, neighborhood poverty or race/ethnicity were independently associated with asthma morbidity.
Methods
The study population included children aged 5–19 years enrolled in Medicaid in the U.S. between 2009 and 2010. Claims data were aggregated on the state level and then processed by the Centers for Medicare and Medicaid into the Medicaid Analytic Extract (MAX), and were obtained by the Research Data Assistance Center (University of Minnesota, Minneapolis, MN). Use of the data was approved by the Johns Hopkins School of Medicine Institutional Review Board.
Children with asthma were defined as those who had at least one outpatient or emergency visit with a primary International Classification of Disease-9 (ICD-9) diagnosis code of an asthma related condition (493.x) over the two year period of observation.
For the purposes of asthma morbidity analyses, emergency department visits were defined as outpatient visits occurring in hospital based emergency departments with a primary or secondary diagnosis code of an asthma related condition. Inpatient visits were defined as those occurring in a hospital with a primary diagnosis code of an asthma related condition. Outpatient visits for asthma, excluding hospital based emergency departments, with a primary or secondary diagnosis code of an asthma related condition were analyzed separately.
Urbanization status of each subject was classified on the county level using the National Centers for Health Statistics Urban Rural Codes 20134. This classification system divides counties into Large Central Metro (“Urban”), Large Fringe Metro (“Suburban”), Medium Metro, Small Metro, Micropolitan and Non-Core. Because there are relatively few people living in Small Metro, Micropolitan and Non-Core areas, these categories were collapsed.
Neighborhood poverty was classified at the zip-code tabulation area level by linking participant zip-codes to data from the Missouri Data Resource Center5. This dataset maps census level data from the American Community Survey 2008–2012 to Zip Code Tabulation Areas. Race/ethnicity was defined as non-Hispanic White, non-Hispanic Black, Hispanic or Latino (“Hispanic”), Asian, or “other”, which included multi-racial (non-Hispanic), American Indian or Alaskan Native, and Native Hawaiian. Residence in an inner-city was defined as living in a county defined as Urban and a zip-code with at least 20% of households below the federally defined poverty line.6
Procedures for reporting race/ethnicity varied by state, with some states mandating reporting of race/ethnicity, others not reporting race/ethnicity at all, reporting on only a portion of participants and or with improbable lack of certain racial/ethnic groups. Because race/ethnicity was unlikely to be reliable in states with high levels of missing or improbable data, and because race/ethnicity was an important covariate and predictor in our analyses, we only included states where 10% or less of participants had missing data on race/ethnicity and where all major race/ethnicity groups were represented in the data. This excluded Massachusetts, Rhode Island, Iowa, Washington, Vermont, Colorado, Arkansas, Wisconsin and New Jersey. Maine did not have clinical information available. The combined eligible population in these 10 states represents about 12% of the total MAX population. In addition, because our primary analysis was a two level analysis combining state level analyses, states without urban areas could not contribute to analyses comparing urban to non-urban areas. This requirement excluded an additional 17 states, leaving Arizona, California, Florida, Georgia, Illinois, Indiana, Louisiana, Maryland, Michigan, Minnesota, Missouri, North Carolina, New York, Ohio, Oregon, Pennsylvania, Texas and Virginia. Subjects were included for months in which they were enrolled in Medicaid with unrestricted benefits.
Statistical Methods
Because each state has different Medicaid eligibility criteria and may have other sources of heterogeneity in claims data, the analysis was conducted in two stages. At the first stage, over-dispersed log-linear Poisson regression models (logistic models for binary outcomes) were used to estimate the association between key predictors (e.g. urbanization status, race/ethnicity and neighborhood poverty) and counts of asthma outcomes (hospitalizations, ED visits, outpatient visits) for each state. At this stage, crude and adjusted models were used, where adjusted models included covariates on poverty, urbanization, sex, race, and age. At the second stage, associations (i.e. coefficients) between key predictors and outcomes in each state were combined using a two-level Normal hierarchical model7. Given the large sample sizes available in this study, each estimated coefficient was assumed to have a Normal distribution about its true value. Then, state-specific coefficients were modeled as having a Normal distribution around a national average association. The approach uses Bayesian modeling with a Normal prior distribution placed on the national average association and a uniform prior placed on the heterogeneity variance. Samples were drawn from the posterior distribution of the national average association and we report the posterior mean as our estimate. This approach accounts for the statistical uncertainty incurred in the first stage and potential unexplained variability between states at the second stage, similar to a meta-analysis. The resulting confidence intervals and p-values incorporate both sources of variability. Potential confounders were included in the state-specific regression models.
Results
Demographics
A total of 16,860,716 children enrolled in Medicaid between 2009 and 2010 were included, of whom 1,534,820 (8.8%) had at least one visit with a primary diagnosis of asthma (see Table 1 for demographic information). Among those with asthma, there were a mean of 3.7 outpatient visits, 0.30 emergency department visits and 0.02 hospital admissions per person per year (Table 2).
Table 1.
Demographic characteristics of the study population
| Number | Percent | Percent with asthma | |
|---|---|---|---|
| Total | 16,860,716 | 100% | 8.8% |
| Race/Ethnicity | |||
| White | 6,038,614 | 35.8% | 7.8% |
| Black | 4,426,019 | 26.3% | 10.4% |
| Hispanic | 4,300,740 | 25.5% | 8.7% |
| Asian | 476,225 | 2.8% | 5.9% |
| Other | 1,619,118 | 9.6% | 9.6% |
| Sex | |||
| Female | 8,492,053 | 50.4% | 7.8% |
| Male | 8,368,143 | 49.6% | 9.8% |
| Urban-rural status | |||
| Urban | 6,762,301 | 40.1% | 8.6% |
| Suburban | 3,301,121 | 19.6% | 8.9% |
| Med Metro | 3,262,218 | 19.4% | 8.8% |
| Small/micro/non-core | 3,535,076 | 21.0% | 9.2% |
| Neighborhood poverty | |||
| Non-Poor | 9,399,979 | 55.8% | 8.4% |
| Poor | 7,460,737 | 44.3% | 9.4% |
| Age category (years) | |||
| 5–7 | 4,958,178 | 29.4% | 11.6% |
| 8–10 | 3,365,368 | 20.0% | 10.0% |
| 11–13 | 3,012,862 | 17.9% | 8.3% |
| 14–16 | 2,963,396 | 17.6% | 6.9% |
| 17–20 | 2,560,912 | 15.2% | 4.9% |
| Inner-city residence | |||
| Non-inner city | 13,129,230 | 77.9% | 8.8% |
| Inner-city | 3,731,486 | 22.1% | 8.9% |
Table 2.
Rates of markers of asthma morbidity among children with asthma (per year), n=1,534,820.
| Outpatient visits | ER visits | Hospitalizations | |
|---|---|---|---|
| Overall | 3.69 | 0.30 | 0.018 |
| Race | |||
| White | 3.39 | 0.23 | 0.010 |
| Black | 3.97 | 0.38 | 0.025 |
| Hispanic | 3.68 | 0.29 | 0.011 |
| Asian | 3.42 | 0.17 | 0.013 |
| Other | 3.82 | 0.33 | 0.034 |
| Urban Rural Status | |||
| Urban | 3.78 | 0.34 | 0.026 |
| Suburban | 3.73 | 0.30 | 0.015 |
| Medium Metro | 3.70 | 0.29 | 0.012 |
| Small/micro/noncore | 3.49 | 0.23 | 0.012 |
| Neighborhood poverty | |||
| Non-poor | 3.62 | 0.28 | 0.015 |
| Poor | 3.77 | 0.33 | 0.022 |
| Inner-city residence | |||
| Non-inner city | 3.65 | 0.29 | 0.014 |
| Inner-city | 3.83 | 0.35 | 0.030 |
Asthma prevalence
In both crude and adjusted analyses, the prevalence of current asthma was not different in inner-city (poor urban) areas compared to non-inner city areas (crude OR: 0.99, 95% CI: 0.81–1.22, adjusted OR: 0.95, 95% CI: 0.81–1.12), and urban status was not a predictor of asthma prevalence in analyses adjusting for neighborhood poverty, and race/ethnicity. Black race and residence in a poor neighborhood were significant risk factors for prevalent asthma. (Table 3).
Table 3.
Associations with asthma prevalence among the overall population, odds ratios.
| Crude Analyses, OR (95% CI) | Adjusted Analyses, OR (95% CI) | |
|---|---|---|
| Race/ethnicity | ||
| White | -ref- | -ref- |
| Black | 1.27 (1.08–1.50) | 1.25 (1.17–1.34) |
| Hispanic | 1.02 (0.90–1.16) | 1.02 (0.90–1.16) |
| Asian | 0.66 (0.53–0.81) | 0.70 (0.61–0.81) |
| Metro Status | ||
| Urban | -ref- | -ref- |
| Suburban | 0.90 (0.84–0.97) | 1.00 (0.95–1.04) |
| Medium Metro | 0.99 (0.81–1.21) | 1.07 (0.88–1.31) |
| Small Metro/Rural | 1.02 (0.75–1.40) | 1.13 (0.83–1.56) |
| Neighborhood Poverty | 1.05 (0.97–1.13) | 1.04 (1.01–1.06) |
Analyses adjusted for age, sex, and the co-variates listed here.
Asthma morbidity
Inner-city areas
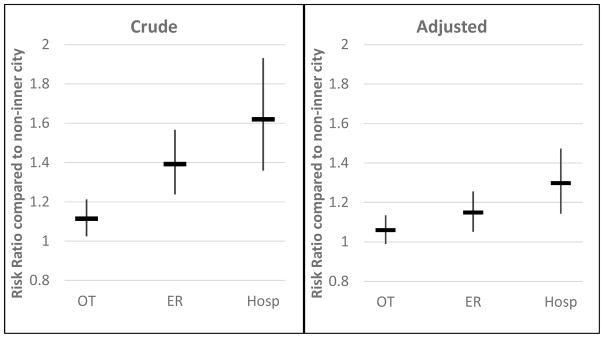
Among children with asthma, living in an inner-city (poor-urban area) was a risk factor for asthma-related emergency room visits and hospitalizations in crude analyses (RR: 1.39, 95% CI: 1.24–1.57, and 1.62, 95% CI: 1.36–1.93, respectively) and in those adjusted for race/ethnicity, age and gender, although the effect size was attenuated (RR: 1.14, 95% CI: 1.05–1.26, and 1.30, 95% CI: 1.14–1.47, for emergency room visits and hospitalizations, respectively, Figure 1).
Figure 1. Association between residence in the Inner-City and asthma morbidity and outpatient visits.
A: Risk ratio in crude analyses; B: Adjusted for race/ethnicity, age, and sex. OT: outpatient visits, ER: Emergency room visits, Hosp: Hospitalizations
Urban/rural status
Among asthmatics, there were significantly fewer emergency room visits and hospitalizations among those living in suburban, medium metro or small/micro-core areas compared to urban areas in crude and adjusted analyses. The strongest of these associations were with hospitalizations, where those living in non-urban areas had 18–28% lower risk of hospitalizations than those living in urban areas, even after accounting for race/ethnicity (Table 4).
Table 4.
Associations with asthma morbidity and outpatient visits among children with asthma.
| Outpatient Visits | ER Visits | Hospitalizations | Outpatient visits | ER visits | Hospitalizations | |
|---|---|---|---|---|---|---|
| Crude RR (95% CI) | Adjusted RR (95% CI) | |||||
| Race/ethnicity | ||||||
| White | -ref- | -ref- | ||||
| Black | 1.17 (1.08–1.25) | 1.79 (1.62–1.98) | 2.18 (1.90–2.51) | 1.12 (1.06–1.18) | 1.68 (1.55–1.82) | 1.89 (1.73–2.06) |
| Hispanic | 1.18 (1.11–1.26) | 1.14 (0.97–1.34) | 1.24 (1.06–1.45) | 1.12 (1.05–1.19) | 1.13 (0.99–1.30) | 1.06 (0.92–1.22) |
| Asian | 1.09 (1.03–1.14) | 0.72 (0.60–0.88) | 0.91 (0.74–1.13) | 1.03 (0.98–1.08) | 0.79 (0.59–0.82) | 0.77 (0.62–0.95) |
| Metro Status | ||||||
| Urban | -ref- | -ref- | ||||
| Suburban | 0.95 (0.90–0.99) | 0.82 (0.71–0.95) | 0.70 (0.60–0.81) | 0.98 (0.94–1.02) | 0.94 (0.83–1.07) | 0.82 (0.73–0.93) |
| Medium Metro | 0.92 (0.84–1.00) | 0.77 (0.67–0.88) | 0.60 (0.48–0.75) | 0.95 (0.88–1.03) | 0.90 (0.80–1.02) | 0.72 (0.58–0.89) |
| Small Metro/Rural | 0.83 (0.77–0.89) | 0.68 (0.59–0.79) | 0.55 (0.43–0.70) | 0.87 (0.82–0.93) | 0.84 (0.74–0.95) | 0.72 (0.60–0.85) |
| Neighborhood Poverty | 1.04 (1.00–1.08) | 1.21 (1.09–1.34) | 1.34 (1.19–1.52) | 1.01 (0.99–1.02) | 1.06 (1.01–1.12) | 1.10 (1.03–1.17) |
Analyses adjusted for age, sex, and the co-variates listed here.
Poverty
Among this low-income population, residence in poor neighborhoods was associated with more asthma related ED visits and hospitalizations in crude and adjusted analyses. (Table 4)
Race/ethnicity
Among asthmatics, non-Hispanic Black children and children of “other” race had significantly higher rates of ED visits and hospitalizations for asthma than non-Hispanic white children, in crude and adjusted analyses. These relationships were strongest for hospitalization, where even after adjustment, Black children had 89% and children of “other” race 61% higher risk of asthma-related hospitalizations than non-Hispanic white children. Hispanic children did not have significantly different rates of ED visits or hospitalizations in adjusted analyses compared to non-Hispanic White children. In contrast, Asian children had significantly fewer ED and hospitalizations than non-Hispanic White children in adjusted analyses. (Table 4)
Interactions between urban/rural status, race/ethnicity and poverty
Because our previous investigations had shown that relationships between poverty and asthma prevalence differed between Hispanic children and non-Hispanic children, we examined whether relationships between neighborhood poverty and asthma morbidity also differed by Hispanic status, and did not find that this was the case (data not shown). In addition, we also examined whether residence in an urban area affected asthma morbidity differently among Hispanic and non-Hispanic Children, and found that the relationship between asthma morbidity and residence in a small/micro/rural area compared to urban area was different for Hispanic compared to non-Hispanic children. Specifically, among Hispanic children, residence in a small/micro/rural area was not protective for ER visits or hospitalizations whereas it was among other racial/ethnic groups. (Table 5).
Table 5.
Adjusted associations with asthma morbidity and outpatient visits among children with asthma, stratified by Hispanic ethnicity.
| Outpatient Visits | ER Visits | Hospitalizations | Outpatient visits | ER visits | Hospitalizations | |
|---|---|---|---|---|---|---|
| Hispanic, risk ratio (95% CI) | Non-Hispanic, risk ratio (95% CI) | |||||
| Metro Status | ||||||
| Urban | -ref- | -ref- | ||||
| Suburban | 1.04 (0.98–1.10) | 0.83 (0.72–0.96) | 0.77 (0.62–0.96) | 0.95 (0.91–0.99) | 0.85 (0.74–0.98) | 0.73 (0.65–0.83) |
| Medium Metro | 0.99 (0.92–1.07) | 0.87 (0.69–1.11) | 0.75 (0.56–1.00) | 0.92 (0.85–1.01) | 0.81 (0.72–0.91) | 0.61 (0.49–0.77) |
| Small Metro/Rural | 1.10 (1.01–1.21) | 0.98 (0.79–1.21) | 0.90 (0.68–1.17) | 0.83 (0.77–0.89) | 0.68 (0.60–0.78) | 0.55 (0.46–0.67) |
Analyses adjusted for age, sex, and the co-variates listed here.
Fraction of hospitalizations attributable to race/ethnicity, poverty and urban residence
The fraction of asthma hospitalizations attributable to race/ethnicity, residence in a poor area, and residence in an urban area were calculated from the fully adjusted model. Among this Medicaid population, 19% of hospitalizations are estimated to be attributable to black race/ethnicity, 4% to residence in a poor area, and 7% to residence in an urban area. Thus, we estimate that a full 30% of asthma hospitalizations among children in Medicaid could be attributable to socioeconomic, geographic and racial/ethnic disparities.
Frequency of outpatient visits
To evaluate the possibility that differences found in emergency room visits and hospitalizations between geographic areas and racial/ethnic groups were due to differences in the propensity to use hospital based versus non-hospital based medical services, we also examined associations with rates of outpatient visits separately. We found that with the exception of Asian race/ethnicity, which was associated with more outpatient visits but fewer ED visits and hospitalizations, risk factors for emergency room visits and hospitalizations showed the same direction of association with outpatient visits, although the magnitude of the relationships were smaller, and less often statistically significant (Table 4).
Discussion
In this analysis of 1.5 million children with asthma enrolled in Medicaid from 2009–2010, we found that, among this lower income population, those living in inner-city areas had an overall 40% higher risk of asthma-related emergency room visits and 62% higher risk of asthma-related hospitalizations than those living in other kinds of neighborhoods, even though overall asthma prevalence was not increased. Although adjustment for race/ethnicity did attenuate this increased risk to a 14% and 30% higher risk of emergency room visits and hospitalizations, respectively, residence in inner-city areas remained a risk for asthma morbidity even after adjusting for race/ethnicity, age and gender. By definition, inner-city areas are both poor and urban, and we further found that both of these factors were independent risk factors for asthma morbidity. Together, these findings highlight substantial geographic and racial disparities in asthma morbidity in the U.S., and support the theory that risk factors concentrated in poor and urban areas contribute to asthma morbidity, even if they may not necessarily contribute to its development.
It is very likely that no one exposure accounts for the increased asthma morbidity associated with living in poor or urban areas. Researchers studying asthma in the inner-city have established that exposure to common household pests that are more common in poor and urban areas, such as cockroaches8 and mice9, is associated with worse asthma control. Air pollution, which may act synergistically with allergen exposures10, is another likely contributor to increased morbidity in poor and urban areas11. Both urban and poor areas tend to have higher densities of major roadways, and to be closer to stationary sources of air pollution, such as power plants and manufacturing facilities, and thus have higher levels of pollutants associated with asthma morbidity, such as particulate matter, nitric oxides and ozone. Additional environmental factors that may contribute to asthma morbidity in poor and urban areas include exposure to second hand smoke12 and other sources of indoor pollution13, prematurity14, and social stress15. Differences in health care quality, adherence to medications and care access patterns could also explain some of the neighborhood disparities found here16,17. Generally, we found that trends with outpatient visits followed those of emergency department and hospitalizations, suggesting that treatment in the non-emergency department outpatient setting was not responsible for the associations seen. More broadly, however, it is difficult within Medicaid to distinguish increased asthma morbidity due to inadequate use of preventative care from that due to environmental exposures.
In contrast to our morbidity findings, here we show that residence in urban areas, or even inner-city areas, is not associated with increased prevalence of asthma, similar to what we previously found in our analysis of the National Health Information Survey3. It is becoming increasingly clear that at least some of the factors that contribute to asthma morbidity may be distinct from those that contribute to initiation of asthma. For example, exposure to pest allergens, while strongly associated with asthma morbidity among urban children9,18, was recently shown to protect against development of wheeze and allergic sensitization among high-risk urban infants19. Other exposures strongly tied to asthma morbidity may similarly have weaker relationships with asthma inception.
Even after adjusting for neighborhood poverty and urban residence, we found that black race/ethnicity was associated with markedly increased rates of outpatient visits, emergency room visits and hospitalizations for asthma, on top of the already increased risk of current asthma. As with urban/rural status and neighborhood poverty, there are likely several reasons for racial/ethnic disparities in asthma morbidity. Genetic differences in risk of asthma development and morbidity have been proposed, and there is some evidence that genes associated with African-heritage may be related to asthma20–22. However, it can be difficult to separate ancestry from socioeconomic status, and it is possible that the crude measures of socioeconomic status used here and in other studies may underestimate the contribution of socioeconomic disparities to racial/ethnic asthma disparities23. For example, because of the historical legacy of segregation and discrimination in the U.S., there are large wealth gaps by race/ethnicity, even among families with the same income, so simply measuring income underestimates socioeconomic disparities by race/ethnicity24. Income and urban status may also poorly capture relevant neighborhood factors, such as air pollution and poor housing stock, which are more likely to be experienced by minority families25. Whatever the cause, these disparities are striking and remain a serious public health problem.
In our previous analysis of National Health Interview Survey data3, we found that among Hispanic children, poverty was protective against prevalent asthma. Here, among low-income children with asthma, we did not find that being of Hispanic race/ethnicity changed the relationship between living in a poor neighborhood and asthma morbidity. However, we did find that for Hispanic children, the relationship between urban residence and asthma morbidity differed compared to other ethnicities, with rural residence conferring no benefit to Hispanic children. We speculate that Hispanic children may be more likely to live in rural areas that have worse air pollution than the rural areas where other race/ethnicities predominate. For example, a high density of Hispanic children live in non-urban areas in the California central valley, an area with among the highest levels of air pollution in the U.S26.
There are several limitations to our analyses. Most importantly, data were collected for administrative purposes, and, as is the case for any analyses that rely on claims data, it is possible that diagnostic miscoding could affect our results. In addition, individual level income data were not available, and Medicaid data are coded only to the zip-code tabulation area, so the assignment of neighborhood poverty was by the zip-code, potentially leading to residual confounding by income. However, children enrolled in Medicaid are all low income, and we accounted for neighborhood income, so we would expect residual confounding by income to be minimal. Outpatient visits could have included follow-up visits for asthma care, and so may not fully represent asthma morbidity. However, this limitation should not apply to emergency department visits and hospitalizations. State rules for Medicaid eligibility vary by state, so there may be some heterogeneity between states, but we accounted for this in our statistical methods. We only included states with race/ethnicity data and with at least one urban area, potentially limiting the generalizability of our data. The available data did not allow us to separate our sub-groups of Hispanic children, such as Puerto-Rican and Mexican children, who have been reported to have different asthma prevalence and morbidity. Finally, while Medicaid provides an opportunity to disentangle risk factors among those that are most disadvantaged and have the highest burden of asthma, the results may not be generalizable to all socioeconomic groups.
These limitations are balanced by several important strengths. Most importantly, this is a massive database that includes data on more than 1.5 million children with asthma, allowing us to make conclusions about low-income children across the entire U.S., instead of just limiting our analysis to one city or region. In addition, our analysis strategy minimized the effect of between state differences, as we analyzed each state individually and combined the analyses for our final estimates.
In conclusion, in this comprehensive analysis of children with asthma covered by Medicaid, we found significant disparities in asthma morbidity related to race/ethnicity and residence in poor and urban neighborhoods. These findings support the theory that environmental risk factors for asthma exacerbation are concentrated in poor urban areas, but highlight the fact that despite several decades of attention to asthma in the inner city, asthma morbidity remains high in urban and poor areas.
Key messages.
Residence in an urban or poor area, and Black race/ethnicity are each significant independent risk factors for asthma emergency room visits and hospitalizations among U.S. children enrolled in Medicaid.
Acknowledgments
Sources of support: This work was supported by the National Institute of Environmental Health Sciences (P50ES018176), the Environmental Protection Agency (STAR83563901), the National Institute of Allergy and Infectious Diseases (K23AI103187, U01AI083238, K24AI114769, R01ES023447, R01ES026170 and R21AI107085). No funder had any role in the design and conduct of the study; collection, management, analysis and interpretation of data, or preparation, review or approval of the manuscript.
ABBREVIATIONS
- CI
Confidence interval
- ED
Emergency Department
- RR
Risk ratio
- OR
Odds ratio
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Corinne A. Keet, Email: ckeet1@jhmi.edu, Associate Professor, Johns Hopkins University School of Medicine, Division of Pediatric Allergy and Immunology.
Elizabeth C. Matsui, Email: ematsui@jhmi.edu, Professor, Johns Hopkins University School of Medicine, Division of Pediatric Allergy and Immunology, Baltimore, MD.
Meredith C. McCormack, Email: mmccor16@jhmi.edu, Associate Professor, Johns Hopkins University School of Medicine, Division of Pulmonary and Critical Care Medicine, Baltimore, MD.
Roger D. Peng, Email: rpeng@jhsph.edu, Professor, Johns Hopkins Bloomberg School of Public Health, Department of Biostatistics, Baltimore, MD.
References
- 1.Weiss KB, Gergen PJ, Crain EF. Inner-city asthma. The epidemiology of an emerging US public health concern. Chest. 1992;101:362S–7S. doi: 10.1378/chest.101.6.362s. [DOI] [PubMed] [Google Scholar]
- 2.Togias A, Fenton MJ, Gergen PJ, Rotrosen D, Fauci AS. Asthma in the inner city: the perspective of the National Institute of Allergy and Infectious Diseases. The Journal of allergy and clinical immunology. 2010;125:540–4. doi: 10.1016/j.jaci.2010.01.040. [DOI] [PubMed] [Google Scholar]
- 3.Keet CA, McCormack MC, Pollack CE, Peng RD, McGowan E, Matsui EC. Neighborhood poverty, urban residence, race/ethnicity, and asthma: Rethinking the inner-city asthma epidemic. The Journal of allergy and clinical immunology. 2015;135:655–62. doi: 10.1016/j.jaci.2014.11.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ingram DD, Franco SJ. 2013 NCHS Urban-Rural Classification Scheme for Counties. Vital Health Stat. 2014;2:1–73. [PubMed] [Google Scholar]
- 5.ZIP/ZCTA master dataset vintage 2014. 2014 (Accessed at http://mcdc2.missouri.edu/cgi-bin/broker?_PROGRAM=websas.dispdada.sas&_SERVICE=appdev&libname=georef&memname=zcta_master&libpath=/pub/data/georef.)
- 6.Busse WW. The National Institutes of Allergy and Infectious Diseases networks on asthma in inner-city children: an approach to improved care. The Journal of allergy and clinical immunology. 2010;125:529–37. doi: 10.1016/j.jaci.2010.01.036. quiz 38–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Everson PJ, Morris CN. Inference for multivariate normal hierarchical models. J Roy Stat Soc B. 2000;62:399–412. [Google Scholar]
- 8.Gruchalla RS, Pongracic J, Plaut M, et al. Inner City Asthma Study: relationships among sensitivity, allergen exposure, and asthma morbidity. The Journal of allergy and clinical immunology. 2005;115:478–85. doi: 10.1016/j.jaci.2004.12.006. [DOI] [PubMed] [Google Scholar]
- 9.Ahluwalia SK, Peng RD, Breysse PN, et al. Mouse allergen is the major allergen of public health relevance in Baltimore City. The Journal of allergy and clinical immunology. 2013;132:830–5. e1–2. doi: 10.1016/j.jaci.2013.05.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Brandt EB, Biagini Myers JM, Acciani TH, et al. Exposure to allergen and diesel exhaust particles potentiates secondary allergen-specific memory responses, promoting asthma susceptibility. The Journal of allergy and clinical immunology. 2015;136:295–303. e7. doi: 10.1016/j.jaci.2014.11.043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ierodiakonou D, Zanobetti A, Coull BA, et al. Ambient air pollution, lung function, and airway responsiveness in asthmatic children. The Journal of allergy and clinical immunology. 2016;137:390–9. doi: 10.1016/j.jaci.2015.05.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Been JV, Nurmatov UB, Cox B, Nawrot TS, van Schayck CP, Sheikh A. Effect of smoke-free legislation on perinatal and child health: a systematic review and meta-analysis. Eur J Paediatr Dent. 2015;16:210–1. [PubMed] [Google Scholar]
- 13.Kanchongkittiphon W, Mendell MJ, Gaffin JM, Wang G, Phipatanakul W. Indoor environmental exposures and exacerbation of asthma: an update to the 2000 review by the Institute of Medicine. Environ Health Perspect. 2015;123:6–20. doi: 10.1289/ehp.1307922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.He H, Butz A, Keet CA, et al. Preterm Birth with Childhood Asthma: The Role of Degree of Prematurity and Asthma Definitions. American journal of respiratory and critical care medicine. 2015;192:520–3. doi: 10.1164/rccm.201503-0522LE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wright RJ. Psychological stress: a social pollutant that may enhance environmental risk. American journal of respiratory and critical care medicine. 2011;184:752–4. doi: 10.1164/rccm.201106-1139ED. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gergen PJ, Togias A. Inner city asthma. Immunology and allergy clinics of North America. 2015;35:101–14. doi: 10.1016/j.iac.2014.09.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gergen PJ, Teach SJ, Togias A, Busse WW. Reducing Exacerbations in the Inner City: Lessons from the Inner-City Asthma Consortium (ICAC) The journal of allergy and clinical immunology In practice. 2016;4:22–6. doi: 10.1016/j.jaip.2015.07.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Rosenstreich DL, Eggleston P, Kattan M, et al. The role of cockroach allergy and exposure to cockroach allergen in causing morbidity among inner-city children with asthma. The New England journal of medicine. 1997;336:1356–63. doi: 10.1056/NEJM199705083361904. [DOI] [PubMed] [Google Scholar]
- 19.Lynch SV, Wood RA, Boushey H, et al. Effects of early-life exposure to allergens and bacteria on recurrent wheeze and atopy in urban children. The Journal of allergy and clinical immunology. 2014;134:593–601. e12. doi: 10.1016/j.jaci.2014.04.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Neophytou AM, White MJ, Oh SS, et al. Air Pollution and Lung Function in Minority Youth with Asthma in the GALA II & SAGE II Studies. American journal of respiratory and critical care medicine. 2016 doi: 10.1164/rccm.201508-1706OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Pino-Yanes M, Thakur N, Gignoux CR, et al. Genetic ancestry influences asthma susceptibility and lung function among Latinos. The Journal of allergy and clinical immunology. 2015;135:228–35. doi: 10.1016/j.jaci.2014.07.053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Vergara C, Murray T, Rafaels N, et al. African ancestry is a risk factor for asthma and high total IgE levels in African admixed populations. Genet Epidemiol. 2013;37:393–401. doi: 10.1002/gepi.21702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sampson RJ, Sharkey P, Raudenbush SW. Durable effects of concentrated disadvantage on verbal ability among African-American children. P Natl Acad Sci USA. 2008;105:845–52. doi: 10.1073/pnas.0710189104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Krivo LJ, Kaufman RL. Housing and wealth inequality: Racial-ethnic differences in home equity in the United States. Demography. 2004;41:585–605. doi: 10.1353/dem.2004.0023. [DOI] [PubMed] [Google Scholar]
- 25.Ard K. Trends in exposure to industrial air toxins for different racial and socioeconomic groups: A spatial and temporal examination of environmental inequality in the US from 1995 to 2004. Soc Sci Res. 2015;53:375–90. doi: 10.1016/j.ssresearch.2015.06.019. [DOI] [PubMed] [Google Scholar]
- 26. [Accessed April 13, 2016];San Joaquin Valley. 2015 at https://www.epa.gov/sanjoaquinvalley/epa-activities-cleaner-air.