Abstract
Although philosophies and practices analogous to bioethics exist in Aboriginal cultures, the terms and categorical distinctions of "ethics" and "bioethics" do not generally exist. In this article we address ethical values appropriate to Aboriginal patients, rather than a preconceived "Aboriginal bioethic." Aboriginal beliefs are rooted in the context of oral history and culture. For Aboriginal people, decision-making is best understood as a process and not as the correct interpretation of a unified code. Aboriginal cultures differ from religious and cultural groups that draw on Scripture and textual foundations for their ethical beliefs and practices. Aboriginal ethical values generally emphasize holism, pluralism, autonomy, community- or family-based decision-making, and the maintenance of quality of life rather than the exclusive pursuit of a cure. Most Aboriginal belief systems also emphasize achieving balance and wellness within the domains of human life (mental, physical, emotional and spiritual). Although these bioethical tenets are important to understand and apply, examining specific applications in detail is not as useful as developing a more generalized understanding of how to approach ethical decision-making with Aboriginal people. Aboriginal ethical decisions are often situational and highly dependent on the values of the individual within the context of his or her family and community.
Mr. F, a 70-year-old Aboriginal elder who speaks only Ojibway, is admitted to a tertiary care hospital for diagnostic investigation of possible prostate cancer. Initially, only a female interpreter is available, and she has difficulty translating the physician's references to the penis while obtaining consent for cystoscopy. When asked to tell Mr. F that the procedure would aid in cancer diagnosis, she refuses to directly translate the concept of cancer and, instead, uses the word for "growth." The patient responds that he does not fully understand the diagnostic test but trusts the interpreter and the urologist and agrees to sign the consent form. During cystoscopy both his son and a male interpreter are present to translate.
Following the biopsy and other diagnostic tests, Mr. F, his son, the male interpreter and the urologist meet. Addressing the son and the interpreter, the urologist explains that Mr. F has advanced cancer spreading to bone. When asked by the son about treatment, the urologist replies that any attempted curative treatment would probably cause more risk and discomfort than would pain relief and other palliative measures. The interpreter begins to translate the urologist's summary, but his explanation of the diagnosis is interrupted by the son, who says that he will communicate directly with his father. He states that the interpreter should not have used the Ojibway word manitoc, which denotes cancer through the cultural metaphor of "being eaten from within," and that direct reference to cancer and his father's terminal prognosis will promote fear and pain. He adds that his father has given him responsibility to interpret and to act as his proxy decision-maker.
The son further opposes the physician's attempt to communicate the prognosis directly to Mr. F, stating that direct references to death and dying may "bring death closer." The urologist argues that Mr. F needs to understand his diagnosis to give informed consent for treatment. The son replies that he will not lie to his father but that he needs time to communicate with his father through a more gradual and indirect process. The physician and son finally agree that the son will involve other family members over the next 48 hours. The physician and family arrange to meet again in 2 days and, in the meantime, to hold a "sharing circle" (see Appendix 1 for definition) in which patient, family members and caregivers will discuss palliative care and answer Mr. F.'s questions.
What is Aboriginal bioethics?
Although philosophies and practices analogous to bioethics do exist in Aboriginal cultures, the concept of "bioethics" is not generally differentiated from the ethical values and frameworks for decision-making that are applied in all dimensions of living. Accordingly, we will address ethical values that may be held by Aboriginal people rather than a formal, codified system of Aboriginal bioethics.
A recent review of the literature revealed that little has been published on the subject of Aboriginal health ethics.1 In the scope of cultural bioethics, Aboriginal systems are unique in their respect for the visions and beliefs of the individual and concomitant respect for the community.2 Aboriginal values are frequently discounted by Western colonial culture. Primarily rooted in the context of oral history and culture, Aboriginal ethics are best understood as a process and not as the correct interpretation of a unified code.1,3 In their approach to ethical decision-making, Aboriginal cultures differ from religious and cultural groups that draw on Scripture and textual foundations for their ethical beliefs and practices. Despite these challenges, common themes and the diversity within Aboriginal ethics may be highlighted. Research conducted with Aboriginal elders4 provides the basis for identifying widely held values in Aboriginal frameworks for decision-making.
Themes in approaches to communication and caregiving
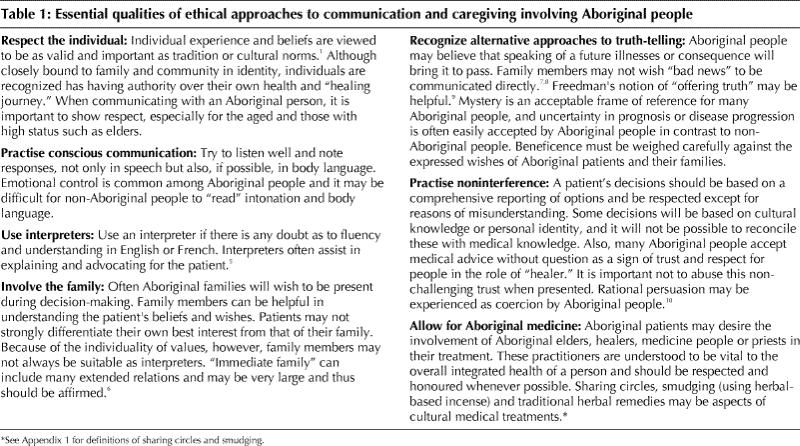
Some essential qualities of ethical approaches to communication and caregiving involving Aboriginal peoples are summarized in Table 1. Although these ethical values are important to understand and apply, examining specific applications of ethical care in detail is not as useful as developing a more generalized understanding of how to approach ethical decision-making with Aboriginal people in actual clinical settings. Aboriginal ethical decisions are often situational and highly dependent on individual values and on the context of the family and community.
Table 1
In general, Aboriginal ethical values include the concepts of holism, pluralism, autonomy, community- or family-based decision-making, and the maintenance of quality of life rather than the exclusive pursuit of a cure. Most Aboriginal belief systems also emphasize achieving balance and wellness within all domains of human life (mental, physical, emotional and spiritual).
Aboriginal North American cultures share some ethical practices, such as the need to respect the integrity of the human body after death.1,2 Spirituality and cultural understandings of death, loss and the existence of Spirit Beings often play a role in the bioethical decisions of Aboriginal patients and families.1 Acceptance is a common, deeply rooted aspect of Aboriginal relationships to death and the passage of time during illness.11,12,13,14,15,16 Maintaining quality of life is commonly seen as paramount to extending life. Simultaneously, life is to be preserved and should be pursued whenever meaningful quality can be maintained. Affirming the dignity of life is essential.10
Some Aboriginal people have a problem with advanced technology, and it is important to acknowledge this in treatment. Problems arise when a cultural heritage of nature-based medicine encounters biomedical treatment emphasizing technological interventions. Health care institutions such as urban teaching hospitals may be associated with a "culture of colonization" emphasizing technological solutions. There are diverse perspectives in Aboriginal communities regarding the use of technologically advanced and aggressive treatments such as transplantation, dialysis and mechanical ventilation. However, many Aboriginal people, particularly the young, may be open to and desirous of using the full range of medical technologies available.
Barriers
Ethical care of Aboriginal peoples may include the current emphasis in bioethics on the moral context of individual relationships in clinical interactions. However, this approach does not fully engage the broader structural context of barriers that impede access to care or interfere with healing processes. Barriers include language problems, lack of cultural competence among health care providers, problems of transportation and communication in service delivery to remote communities, and institutional discrimination.
Applications of the bioethical principles of autonomy, beneficence and justice in contemporary relationships must recognize the historical context of power relationships between Aboriginal people and providers of health and social services. The dominant emphasis on respect for individual autonomy in bioethics may need to incorporate Aboriginal values emphasizing noninterference. The Aboriginal psychiatrist, Clare Brant,10 observed:
The ethic of non-interference is a behavioural norm of North America Native tribes that promotes positive interpersonal relations by discouraging coercion of any kind, be it physical, verbal or psychological.
Approaches to guaranteeing autonomy in communication involving consent and truth-telling must accommodate this value of avoiding coercion. Direct, unmediated communication of "bad news" involving terminal prognosis or risks of impending death may violate some individual's and community's values. Cultural and spiritual traditions, including those of Navajo people in the United States and Dene people in Canada, assert that speaking explicitly about terminal illness and death may hasten death.7,8 Some families may therefore ask to be present to mediate communication of bad news and support the family. One potential way of recognizing alternative approaches to truth-telling in consent may resemble Freedman's concept of "offering truth."9 This framework avoids "imposing truth" by allowing the person to define the level and explicitness of the information they require to interpret care options.
Emphasis on guaranteeing informed consent and minimizing risks to individuals in the decision-making process may be unduly influenced by historical relationships that discount Aboriginal values, which emphasize protection of the family and the community. In making consent decisions, Aboriginal patients and their families may balance the risks and benefits to the individual with interests of the family and community. For example, a patient may defer to the wisdom of an elder or healer or elect to use a proxy decision-maker from the family in signing consent agreements or advance directives.8
In ethical decision-making, power differences may be accentuated with language barriers among patients who are monolingual speakers of Aboriginal languages or who have limited fluency in English or French. In these situations ethical communication should involve the use of trained Aboriginal health interpreters who have competence in both biomedical terminology and Aboriginal concepts of health and healing.
Diversity and pluralism
Diversity and pluralism are essential dimensions of Aboriginal ethics. Aboriginal ethics emphasize a pluralistic perspective that accepts that a wide spectrum of values and perspectives may be held by family members. In allowing for the expression of a plural spectrum of values, autonomy among individual family members is emphasized and respected. Aboriginal cultures and communities are diverse, and therefore it is difficult to develop generalizations about values or decision-making practices. Across Canada and within individual provinces and territories, there is a wide spectrum of cultural and language groups, and variations between individual Aboriginal communities and regional organizations. For example, Manitoba is home to Cree, Ojibway (Annishinabe), Métis, Inuit, Dene and Dakota people. Despite some shared beliefs, each cultural group must be treated with respect and an understanding of inherent diversity.
In considering the diversity of beliefs among Aboriginal people, one needs to recognize the impact of Christianity on Aboriginal communities. In many communities and families the introduction of Christianity increased the diversity of values influencing ethical decision-making. In some cases, the result has been division and animosity between family and community members who hold traditional Aboriginal values and those who assert Christian values.
Why are ethics for Aboriginal people important?
Population
The population of Aboriginal people who may benefit from culturally appropriate ethical decision-making is growing. There are alternative ways to define the Aboriginal population of Canada. Data from the 1996 Census indicated that about 800 000 people identified themselves with one or more Aboriginal groups (North American Indian, Métis or Inuit).17 The population includes about 41 000 who identified themselves as Inuit and about 210 000 as Métis. Approximately 44% of Aboriginal people live in urban areas.18 Of the more than 550 000 respondents who identified themselves as "North American Indian," about 60% indicated that they were a member of a First Nation or Band or had treaty status as defined by the Indian Act of Canada.17 The ongoing transfer of control over health services to individual First Nations or Bands will mean that mandates to apply Aboriginal values in ethical decision-making will be emphasized in primary and tertiary health programs.
Access to care
The importance of understanding Aboriginal perspectives on health ethics is often linked with differences in health status and utilization of health services. Lower health status and barriers to medical care access are engaged within the ethical context of distributive justice and equality. Research documenting the disproportionate burden of morbidity and mortality and high levels of health service utilization among Aboriginal people is often cited in medical literature. However, some Aboriginal health policy-makers have recently emphasized that epidemiological comparisons do not express the importance of individual and community historical relationships or contemporary experiences of racism in residential schools, social welfare programs or the health care system.19 In addition, there are many culturally distinct practices among Aboriginal people that necessitate a unique ethic of care.
Equitable access to high-quality health services is a central focus for both rural and urban Aboriginal people. Because of the centrality of family in Aboriginal people's experience of illness and treatment, and restrictions in the access of friends and family members, Aboriginal patients often feel isolated when in hospital. Aboriginal approaches to decision-making commonly involve members of the extended family, and offering opportunities for family involvement should be considered a prerequisite of providing ethical and culturally appropriate services.8
How should I approach the practice of ethics for Aboriginal people?
To understand Aboriginal health ethics in clinical practice, several fundamental dimensions need to be recognized. Health care providers must recognize the risks of applying stereotyped values and spiritual beliefs, as well as the futility of attempting to develop generalized ethical formulas for communicating with Aboriginal patients. Plural belief systems and variation among individuals preclude the direct application of knowledge in reconciling Aboriginal beliefs with biomedical and bioethical criteria.
Aboriginal bioethics can best be viewed as an interpersonal process. Immediate and clearly defined approaches should not be expected. Aboriginal bioethical positions are largely situational; adopting a case-specific approach is therefore important. Health care providers working with Aboriginal people must first try to acknowledge the importance of autonomy, the centrality of family to health and identity, the diversity in beliefs and practices among Aboriginal people, and the value of developing and maintaining personal and emotionally sincere relationships with patients. Provider ethics emphasizing the maintenance of professional distance may contravene the Aboriginal affirmation of the power of human relationships in the healing process. Trust is paramount.
Health care providers might consider adopting the role of learner, allowing Aboriginal elders and each patient to lead in the articulation of the ethical principles guiding care. Not only is the process of family consultation critical in making decisions about acute and emergency care, but it is also an important dimension of day-to-day primary care. Health care providers should recognize that biomedical values may not always be reconcilable with Aboriginal values, despite improved communication methods or increased cross-cultural awareness.
If health care providers ignore differences related to Aboriginal culture, they will not be able to understand the wide spectrum of beliefs and attitudes that Aboriginal people draw on in making ethical decisions. Thus, although certain values such as respect for dignity, noninterference, sharing and the importance of family and community are widespread, other beliefs such as those about truth-telling may differ, even among members of the same family. Health care providers cannot take Aboriginal beliefs for granted and need to explore these carefully with each person. As well as respecting beliefs, health care providers need to respect the decisions of patients and families who request involvement of Aboriginal healers, elders and medicine people in their care (Table 1).
The future of ethics and Aboriginal people
Aboriginal cultures can be identified as premodern in the sense that there is no separation between the self and the universe, between self, family and community or between mind, body and spirit. Thus, healing is not possible without spirituality, nor without relationships to family and community, and to the cosmos. Restoring these values and beliefs can balance biomedical treatments and lead to healing of the person as well as cure of disease.
Recent Western history has emphasized scientific and technological advances at the expense of, and exclusion of, spirituality. The consequences of this have been traumatic for many traditional Aboriginal people. When in need of health care, many Aboriginal people view health care institutions as dehumanizing: they experience mind-body separation and separation from family and community, and they are asked to participate in ethical decision-making guided by biomedical values.
The postmodern paradigm, which questions the existence of universal norms, scientific truth and "superior" cultures, presents an interesting challenge to modern medicine and its claims of exclusive efficacy in achieving cure. The current popularity of alternative healing methods, such as Aboriginal medicine, and the thirst for spiritual values are but a few indications of a postmodern culture that is more inclusive and holistic and thus more akin to traditional Aboriginal culture.
Aboriginal ethics is an important area of study because of its potential to make exceptional contributions to more generalized understandings of bioethical practice in increasingly diverse clinical and sociocultural environments. The emphasis in Aboriginal ethics on pluralism, diversity and the maintenance of a high level of respect for individuality challenges Western biomedical paradigms to become more responsive and dynamic in their approach to ethical decision-making. By incorporating a model of ethics that acknowledges pluralism and cultural context, medicine has the opportunity to develop models of ethics and care that are relevant to the cross-cultural treatment of the whole person.20
Considering the unique perspectives and experiences of Aboriginal people and the need for a dynamic, responsive framework for cross-cultural ethical decision-making, the Aboriginal population is clearly not the only cultural or religious group that is diverse and has a variety of beliefs and practices. By learning to respond to the nature of Aboriginal ethics, Western health care practitioners will become more responsive to the dynamics of culture in ethical decision-making for members of many ethnocultural communities.
The case
The young female interpreter, out of respect for Mr. F's age, sex and status, cannot discuss the urological procedure with him directly. However, by adhering to Ojibway beliefs, she does use a generalized term to refer to cancer and thus avoids contravening the belief that "speaking the future may bring it to pass." Although the male interpreter is able to use anatomic language without disrespect, Mr. F's son feels that explicit truth-telling about cancer is against traditional practice. In giving his son permission to be his interpreter and to be a proxy decision-maker, Mr. F is not undermining his own personal autonomy and instead is demonstrating shared family and communal responsibility in decision-making. This is in contrast to the usual Western view of autonomy as conceding supremacy to the individual rather than to anyone else in making decisions. Only recently has the importance of relationships, especially as propounded in feminist ethics, been given a place in bioethics. It is worrisome for some that a cognitively competent individual is not being involved in making decisions about his future. Mr. F has, however, delegated responsibility to his son, even though non-Aboriginal patients more commonly accord such delegation to the medical team.
Given the principle of noninterference among Aboriginal people, the father's values and beliefs may differ considerably from those of his family. An important task of the interpreter and caregivers is to determine whether such differences are present. Aboriginal language interpreters are thus necessary not just for translation but to bring cultural awareness and sensitivity to interactions between patients, family members and health care providers. If differences in values are present, the physician may need to "offer truth" to ensure that Mr. F's views are respected. For example, Mr. F might be asked, "Are you the sort of person who likes to know all available information, or are you happy for your son to make decisions for you?" In this case it is reasonable that the father is not immediately told about his prognosis, since curative treatment is not being recommended. By being given extra time and a cultural medical treatment (i.e., a sharing circle in which caregivers, family and the patient participate), Mr. F achieves "balance" between his diagnosis, the biomedical view and his spiritual beliefs in a culturally appropriate manner. Following the sharing circle and a family meeting, the son, the urologist and the interpreter meet with Mr. F, his wife and 2 of his other children.
After this process of family consultation and gradual and prolonged truth-telling by the family, Mr. F understands his diagnosis and the implications of metastatic cancer. Together with his family, he consents to palliative care, including pain control and palliative radiation.
Related Web sites .
Aboriginal healing and wellness links (Turtle Island Native Network): www.turtleisland.org
Association of American Indian Physicians: www.aaip.com
Health Canada First Nations and Inuit Health Programs: www.hc-sc.gc.ca/msb/fnihp
Indian Health Service, US Department of Health and Human Services: www.ihs.gov
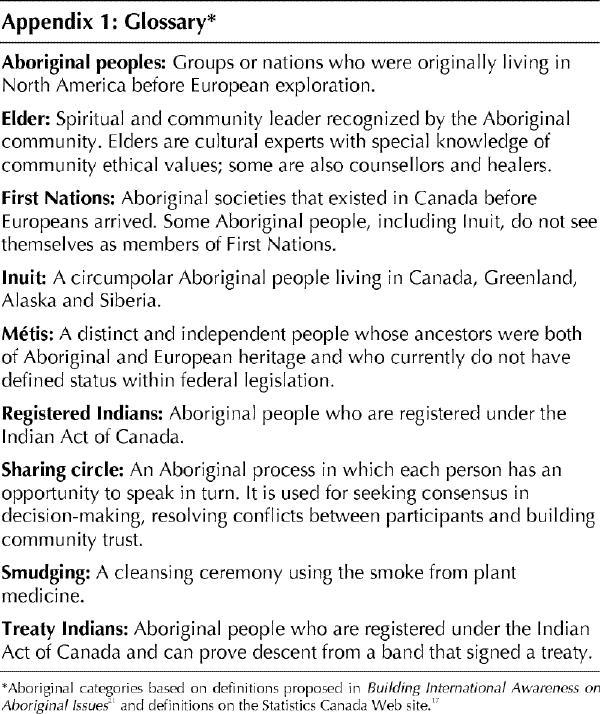
Appendix 1.
Footnotes
This series began in the July 15, 1996, issue and can be found on CMAJ's Web site (www.cma.ca/cmaj/series/bioethic.htm).
This article has been peer reviewed.
Competing interests: None declared.
Reprint requests to: Dr. Joseph M. Kaufert, Department of Community Health Sciences, Faculty of Medicine, University of Manitoba, 750 Bannatyne Ave., Winnipeg MB R3E 0W3; joseph_kaufert@umanitoba.ca
References
- 1.Gariépy GJ. End of life issues in Aboriginal North America [occasional paper]. Winnipeg: University of Manitoba; 1999.
- 2.Hultkrantz A. Native religions of North America: the power of visions and fertility. San Francisco: Harper Collins; 1987.
- 3.Ong WJ. Orality and literacy. New York: Methune; 1982. p. 57, 86, 145.
- 4.Ellerby JH. Working with Aboriginal elders: understanding Aboriginal elders and healers and the cultural conflicts involved in their work in health care agencies and institutions. Winnipeg: Earth Concepts and Biomedical Communications; 1999. p. 1-54.
- 5.Kaufert J, Koolage W. Role conflict among culture brokers: the experience of Native Canadian medical interpreters. Soc Sci Med 1984;18(3):383-6. [DOI] [PubMed]
- 6.Preston RJ, Preston S. Death and grieving among northern forest hunters: an East Cree example. In: Coping with the final tragedy: cultural variations in dying and grieving. Amittyville (NY): Baywood; 1991. p. 135-56.
- 7.Carrese JA, Rhodes LA. Western bioethics on the Navajo reservation: Benefit or harm? JAMA 1995;274:826-9. [PubMed]
- 8.Kaufert JM, Putsch RW, Lavallée M. End-of-life decision making among Aboriginal Canadians: interpretation, mediation, and discord in the communication of "bad news." J Palliat Care 1999;15:31-8. [PubMed]
- 9.Freedman B. Offering truth: one ethical approach to the uninformed cancer patient. Arch Intern Med 1993;153:572-6. [DOI] [PubMed]
- 10.Brant CC. Native ethics and rules of behaviour. Can J Psychiatry 1990;35:534-9. [DOI] [PubMed]
- 11.Deloria V. Thinking in time and space. In: God is red: a Native view of religion. Golden (CO): Fulcrum Publishing; 1993. p. 62-77.
- 12.Deloria V. Death and religion. In: God is red: a Native view of religion. Golden (CO): Fulcrum Publishing; 1993. p. 165-84.
- 13.Hultkrantz A. North American Indian religion in a circumpolar perspective. In: Houins P, editor. North American Indian studies: European contributions. Gottingen: Hovens; 1981. p. 11-28.
- 14.Hultkrantz A. Health, religion and medicine in Native North American traditions. In: Sullivan LE, editor. Healing and restoring: health and medicine in the world's religious traditions. London: Macmillan; 1989. p. 327-58.
- 15.Hultkrantz A. Shamanic healing and ritual drama: health and medicine in Native North American religious traditions. New York: Crossroad; 1992. p. 15-6.
- 16.Hultkrantz A. Shamanic healing and ritual drama: health and medicine in Native North American religious traditions. New York: Crossroad; 1992. p. 164-8.
- 17.Population by Aboriginal group. In: 1996 Census. Ottawa: Statistics Canada. Available: www.statcan.ca/english/Pgdb/People/Population/demo39a.htm (accessed 2000 Aug 29).
- 18.Royal Commission on Aboriginal Peoples. Gathering strength. Ottawa: The Commission; 1996.
- 19.O'Neil J, Reading J, Leader A. Changing the relations of surveillance: the development of a discourse of resistance in Aboriginal epidemiology. Hum Organ 1998;57(2):230-7.
- 20.Dacher E. Towards a post-modern medicine. J Altern Complement Med 1996; 2(4):531-7. [DOI] [PubMed]
- 21.Pohl A. Building international awareness on Aboriginal issues. Toronto: Citizens for Public Justice; 2000. p. 28-32.


