Abstract
Background and Aims
Naloxone access laws (NALs) have been suggested to be an important strategy to reduce opioid-related harm. We describe the evolution of NALs across states and over time and review existing evidence of their overall association with naloxone distribution and opioid overdose as well as the potential effects of specific NAL components.
Methods
Descriptive analysis of temporal variation in US regional adoption of NAL components, accompanied by a systematic search of 13 databases for studies (published between 2005 and 20 December 2019) assessing the effects of NALs on naloxone distribution or opioid-related health outcomes. Eleven studies, all published since 2018, met inclusion criteria. Study time-frames spanned 1999–2017. Opioid-related overdose mortality, emergency department episodes and naloxone distribution were correlated with the presence of a NAL and, where data were available, NAL components.
Results
Existing evidence suggests mixed, but generally beneficial, effects for NALs. Nearly all studies show that NALs, particularly those that permit naloxone distribution without patient-specific prescriptions, are associated with increased naloxone access [incidence rate ratios (IRR) range from 1.40, 95% confidence interval (CI) = 1.15–1.66 to 7.75, 95% CI = 1.22–49.35] and increased opioid-related emergency department visits (IRR range from 1.14, 95% CI = 1.07–1.20 to 1.15, 95% CI = 1.02–1.29). Most studies show NALs are associated with reduced overdose mortality, although findings vary depending on the specific NAL components and time-period analyzed (IRR range from 0.66, 95% CI = 0.42–0.90 to 1.27, 95% CI = 1.27–1.27). Few studies account for the variation in opioid environments (i.e. illicit versus prescription) or other policy dimensions that may be correlated with outcomes.
Conclusions
The existing literature on naloxone access laws in the United States supports beneficial effects for increased naloxone distribution, but provides inconclusive evidence for reduced fatal opioid overdose. Mixed findings may reflect variation in the laws’ design and implementation, confounding effects of concurrent policy adoption, or differential effectiveness in light of changing opioid environments.
Keywords: Harm reduction, mortality, naloxone, opioids, overdose, pharmacy
INTRODUCTION
The growing global burden of opioid-related morbidity and mortality necessitates expanded overdose prevention and reversal efforts. Escalating rates of opioid overdose deaths have been particularly dramatic in North America, and the United States is currently experiencing the worst opioid overdose crisis in its history. In 2018, there were more than 47000 opioid-involved overdose deaths in the United States [1], and it is likely that this number would have been higher if it were not for expanded access to naloxone, an opioid antagonist effective for reversing the overdose-producing effects of opioids [2]. Naloxone is an essential tool employed by uniformed first responders, family, friends and those who use drugs to save lives and reduce other opioid-related harm.
Naloxone has been traditionally available in the outpatient setting only to patients who had been directly prescribed it by a medical provider, although international efforts during the last 20 years aimed to expand access through take-home models [3]. As of 2018, all US states and Washington DC have enacted some form of naloxone access laws (NAL) to encourage providers to prescribe and dispense naloxone, to remove the requirement that the person at risk of overdose has an in-person consultation with a prescriber and, in some cases, to permit the medication to be provided in non-medical settings [4]. These laws vary in the specifics of their design both across states and over time. The various components that comprise NALs underscore that naloxone availability and use may be influenced at different points from prescription to dispensation to administration—some of which may be more directly impacted by legal change than others.
Given that research into other legal and policy interventions, such as prescription drug monitoring programs (PDMPs), has shown that the specific components of these interventions may have differential impacts on opioid-related public health outcomes [5–8], it is likely that research evaluating the effectiveness of specific NAL components may produce more useful results than studies that evaluate NALs as a binary construct. Furthermore, some NAL components may have a differential impact depending on the environment in which they exist. For example, some NAL provisions, such as those that mandate that naloxone be prescribed to patients at increased risk of opioid overdose, may be better suited to addressing overdose risk from those prescribed opioid analgesics than others who use heroin or fentanyl.
In this study, we examine variation in NAL design across states and over time and synthesize findings from the existing literature regarding the effectiveness of these laws and the various components that comprise them. This review of the literature sheds some light into NAL variation and documents the evidence of NAL components on relevant outcomes, including fatal and non-fatal overdoses and changes in naloxone distribution.
METHODS
First, we examined the composition of NALs across states and over time utilizing legal data coded by the Prescription Drug Abuse Policy System (PDAPS) for all states and the District of Columbia from 2001 to 1 July 2017 [9]. Components codified by PDAPS and their definitions are detailed in Table 1. We then visualize several of these elements to show which are most frequently adopted by states and when.
Table 1.
Various naloxone access law components.
| NAL component | Definition |
|---|---|
| Policies targeting prescriber/prescription | |
| Prescriber immunity | Prescribers (e.g. physicians) are granted criminal or civil immunity for prescribing, dispensing or distributing naloxone to a layperson |
| Third-party prescribing | Naloxone prescriptions can be written for third parties—individuals who have not been examined by the prescriber |
| Prescribing requirements | Law recommends or requires prescribing of naloxone to patients potentially at risk of overdose |
| Policies targeting dispenser/distribution | |
| Dispenser immunity | Dispensers (e.g. pharmacists) are granted criminal or civil immunity for prescribing, dispensing or distributing naloxone to a layperson |
| Non-patient-specific dispensing model | Naloxone can be dispensed or distributed without patient-specific prescriptions, such as via standing-order |
| Lay dispensing permitted | Law permits laypeople to dispense naloxone |
| Policies targeting individual obtaining or using naloxone | |
| Protections to layperson for administering naloxone | Laypeople are immune from criminal or civil liability when administering naloxone |
| Permits naloxone possession without prescription | Removes criminal penalties for possession of naloxone without prescription |
NAL = naloxone access law.
To further understanding of the association that certain NAL components have with outcomes of interest, we conducted a systematic review of the NAL literature. This synthesis of the NAL literature draws from a broader scoping review of opioid policy evaluation studies, details of which are described in Schuler et al. [10], updated to include articles published to December 2019. Briefly, the broader review searched for articles published in English within 13 medicine, social science, economic and legal databases using a defined set of search terms (details provided in the Supporting information). Articles were included if they contained at least one search term from each of three categories: (1) policy terms (e.g. ‘naloxone access’, ‘state policy*’, ‘Good Samaritan’), (2) opioid terms (e.g. opioid, heroin, oxycodone) and (3) opioid-related outcome terms (e.g. overdos*, ‘doctor shopping’, ‘inappropriate presci*’). The search time-frame covered 1 January 2005 to 20 December 2019. As the review was not pre-registered, these analyses should be considered exploratory.
Inclusion criteria
Studies were first screened on title and abstract and selected for full review if they evaluated at least one US opioid-related law and included as a dependent variable at least one opioid- or naloxone-related outcome. For the purposes of this study, we applied additional inclusion criteria to restrict to empirical studies that assessed the effects of NALs on naloxone distribution or opioid-related health outcomes. We excluded descriptive studies, commentaries and dissertations.
Data extraction
Information from each included study was extracted into a database with predesignated fields, including metadata (e.g. title, authors), study features (e.g. study period, data sources, population), statistical methods (e.g. model type, analytical unit, covariates) and results (e.g. coefficient point estimates, standard errors); see Supporting information, Table S2. One reviewer extracted data from each study and entered them into the standardized form. A second reviewer checked all fields for accuracy and completeness; discrepancies were resolved by consensus.
Quality assessment
We assessed methodological quality by whether authors adjusted for potential confounders, accounted for potential collinearity in policy adoption and used models well-suited for causal inference (i.e. inclusion of pre–post policy data, control/comparison groups and number of treated units). Methodological concerns for studies are described narratively in the Results.
Effect size estimates
Studies reported effects in various ways. To facilitate comparisons of the magnitude of effect sizes across studies, we calculated and presented incidence rate ratios (IRRs). Studies reporting the results from a negative binomial or Poisson regression model are directly reported as IRRs with their associated confidence intervals (CIs). For low probability outcomes, odds ratios (ORs) were interpreted and reported as IRRs with their associated CIs. For studies that used linear models with a log-transformed outcome, we used the exponentiated coefficient estimate as its IRR.
For studies that estimated linear regression models, an average base rate (generally taken from the article) of the outcome of interest was determined and used to transform the regression coefficient estimate, β, to an IRR using the following formula:
| (1) |
CIs for the IRRs derived from the linear regression models were transformed in a similar fashion based on standard error estimates provided in the study.
Due to the heterogeneity of the studies included, a meta-analysis was not performed. Furthermore, because most studies used identical or highly overlapping outcome data sets, the estimates are not independent of each other, and thus cannot be combined as a single estimate.
Search results
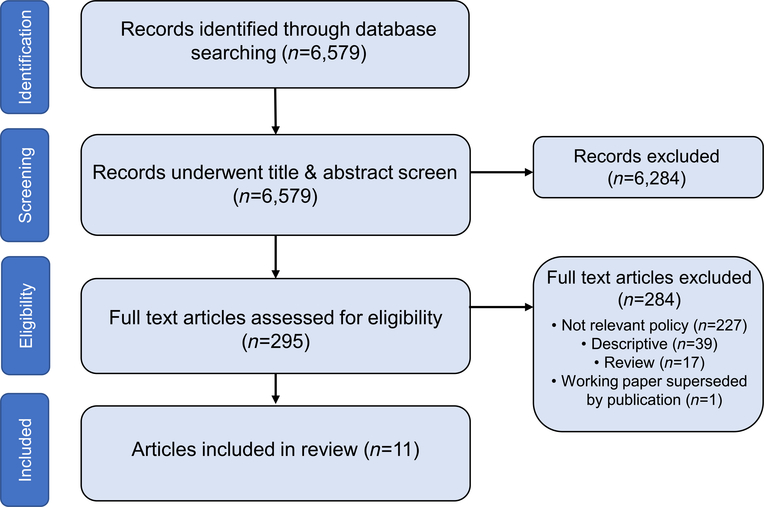
Our search yielded 6579 papers for review (Fig. 1). Following title and abstract screening, 295 articles were considered for full text review, of which 11 met our inclusion criteria and underwent data extraction.
FIGURE 1.
Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) flow diagram.
RESULTS
Policy landscape
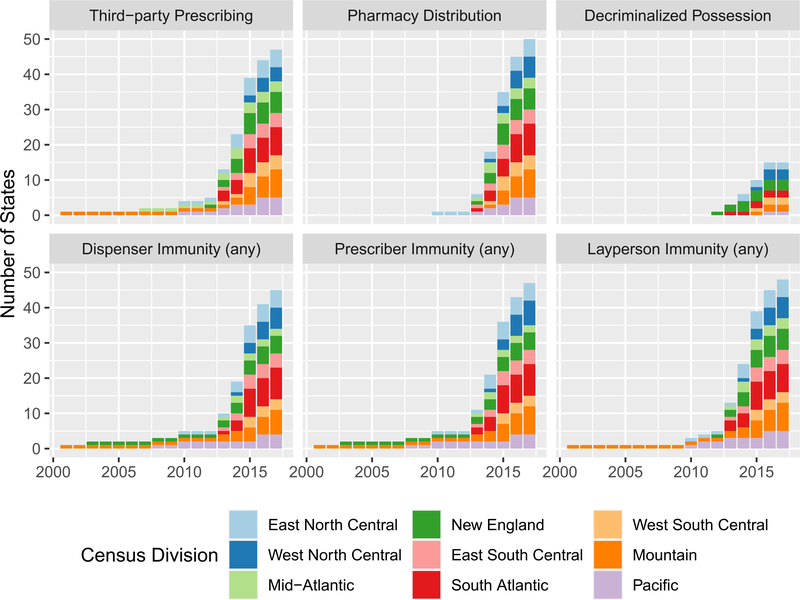
Only four states had some form of a NAL prior to 2010. From 2010 to 2017, states increasingly adopted NALs with various components designed to encourage the prescription, distribution and use of naloxone (see Table 1).
Figure 2 shows the number of states with NAL components from 2001 to July 2017, color-coded by census division (see Supporting information, Table S3 for dates of NAL component adoption by state). There appears to be some regional variation in NAL adoption, with the mid-Atlantic and northeastern regions tending to adopt laws earlier than others. The number of components increased over time, as states adopted more comprehensive NALs that extended beyond immunities from civil and/or criminal penalties for naloxone prescribers and dispensers, to include other components, including those permitting third-party prescribing and pharmacy distribution without patient-specific prescriptions. By 2015 most states had some form of NAL. With the exception of components that decriminalize possession of naloxone without a prescription, most NAL components are highly correlated, with correlation coefficients ranging from 0.73 to 0.97 (see Supporting information, Figs S1 and S2).
FIGURE 2.
Number of states with naloxone access laws (NAL) components 2001–17, by Census Division. Data are to 1 July 2017 from the Prescription Drug Abuse Policy System. US Census Divisions are as follows: East North Central (Wisconsin, Michigan, Illinois, Indiana and Ohio), West North Central (North Dakota, South Dakota, Nebraska, Kansas, Minnesota, Iowa and Missouri), mid-Atlantic (New York, Pennsylvania and New Jersey), New England (Maine, New Hampshire, Vermont, Massachusetts, Connecticut and Rhode Island), East South Central (Kentucky, Tennessee, Mississippi and Alabama), South Atlantic (West Virginia, Maryland, Delaware, Washington DC, Virginia, North Carolina, South Carolina, Georgia and Florida), West South Central (Texas, Oklahoma, Arkansas and Louisiana), Mountain (Montana, Idaho, Wyoming, Utah, Nevada, Colorado, Arizona and New Mexico) and Pacific (Alaska, Washington, Oregon, California and Hawaii).
Evidence for effects of NALs
Of the 11 articles that met our inclusion criteria, nine employed a quasi-experimental design with pre–post data alongside a comparison group, and two examined variations in outcomes using cross-sectional analyses. Table 2 shows characteristics of each study.
Table 2.
Characteristics of studies that met inclusion criteria.
| Study | Period | NAL components examined | Outcome and cases | Outcome data source | Method | Controls for possible confounders | Opioid-specific outcomes | Collinearity |
|---|---|---|---|---|---|---|---|---|
| Blanchard [11] 2018 | April 2013–June 2015 | Standing-order | Opioid-related hospital re-admissions in 12 states (individual-level) | HCUP | Cross-sectional | Good Samaritan laws, edicaid MAT coverage | No | NA |
| Doleac & Mukherjee [12] 2018 | ED = 2006–15; OD = 2010–15 | Third-party prescribing Standing-order |
Opioid-related ED visits; opioid-related mortality (jurisdiction-level) | CDC mortality data; HCUP | Controlled pre–post | Good Samaritan laws, PDMPs, doctor-shopping restrictions, pain clinic regulations, physician and pharmacy regulations, tamper-resistant formulations | Prescription and illegal | Collapsed two policy components into one intervention |
| McClellan [13] 2018 | 2000–14 | Naloxone possession without prescription Prescriber immunity Dispenser immunity Third-party prescribing Standing-order |
Overdose deaths (state-level) | CDC mortality data | Controlled pre–post | Good Samaritan laws | No | Not discussed |
| Gertner [14] 2018 | 2007–16 | Prescriber immunity Third-party prescribing Standing-order Lay dispensation |
Quarterly prescriptions for naloxone (state-level) | CMS Medicaid data | Controlled pre–post | Medicaid expansion and expenditures | No | Not discussed |
| Xu [15] 2018 | 2007–16 | Third-party prescribing Standing-order |
Monthly prescriptions for naloxone (state-level) | Symphony health data | Controlled pre–post | Buprenorphine prescriptions | No | Ran separate models for each policy component |
| Lambdin [16] 2018 | 2014 | Naloxone possession without prescription Prescriber immunity Dispenser immunity Third-party prescribing Standing-order Lay dispensation |
Implementation of overdose education and naloxone distribution (OEND) programs (county-level) | Harm reduction coalition’s OEND database | Cross-sectional | PDMPs | No | Ran separate models for each policy component |
| Sohn [17] 2019 | 2011–17 | Third-party prescribing Standing-order Prescribing requirements |
Naloxone prescriptions (state-level) | IQVIA | Controlled pre–post | Retail prescription opioid distribution | No | Collapsed two policy components into one intervention |
| Abouk [18] 2019 | 2005–16 | Standing-order Direct dispensing by pharmacists authorized |
Overdose deaths; ED episodes; Medicaid naloxone prescriptions (state-level) | CDC mortality data; HCUP data | Controlled pre–post | Medicaid expansion, PDMP, must access PDMP, Good Samaritan laws, medical cannabis access | Prescription and illegal | Collapsed several policy components into three categories of interventions |
| Atkins [19] 2019 | 1999–2016 | Dichotomous Naloxone access law | Overdose deaths (state-level) | CDC mortality data | Controlled pre–post | Good Samaritan laws, PDMPs, pain clinic laws, medical cannabis access | Prescription and illegal | NA |
| Erfanian [20] 2019 | 1999–2016 | Naloxone possession without prescription Prescriber immunity Dispenser immunity Third-party prescribing Standing-order Protections to layperson for administering naloxone |
Overdose deaths (state-level) | CDC mortality data | Controlled pre–post; spatial autoregressive model | Medical cannabis laws; per-capita prescription analgesics dispensed; drug arrests | No | Group policy components into five categories |
| Rees [21] 2019 | 1999–2014 | Naloxone possession without prescription Prescriber immunity Third-party prescribing Standing-order |
Overdose deaths (state-level) | CDC mortality data | Controlled pre–post | Good Samaritan laws, PDMP, medical cannabis laws | Prescription and illegal | Acknowledged but not addressed in analyses |
NAL = naloxone access law; ED = emergency department; OD = overdose; NA = not applicable; MAT = medication-assisted treatment; OEND = overdose education and naloxone distribution; PDMP = prescription drug monitoring program; HCUP = health-care cost and utilization program; CDC = Centers for Disease Control and Prevention; IQVIA = formerly Quintiles and IMS Health, Inc.
Seven of the 11 articles examined outcomes of opioid-related overdoses, such as the count or rate of fatal overdoses and the number or rate of opioid-involved emergency department (ED) visits in a state. Four studies examined changes in the number of naloxone prescriptions dispensed, and one examined the implementation of overdose education and naloxone distribution (OEND) programs. All studies but one were published in peer-reviewed journals (Doleac & Mukherjee [12] was published as a working paper).
Seven studies examined NALs dichotomously, and only one [19] did not also account for specific NAL components. Six studies dealt with potential issues of multicollinearity by collapsing components or running individual models for each component. In three cases [12,15,17], third-party prescribing and standing-order laws were combined into one policy intervention due to the substantial correlation in their enactment. One study [18] combined NAL components into a three-tiered categorical measure based on the degree of dispensing authority granted to pharmacists (direct dispensing authority, indirect dispensing authority, other ‘weak’ form of NAL). One study [20] combined prescriber and dispenser immunity provisions into a single intervention.
The most commonly evaluated components were non-patient-specific prescription pharmacy distribution models (e.g. standing-orders; n = 10), followed by third-party prescribing (n = 8). Less commonly assessed were provisions related to prescriber immunity (n = 5), decriminalization of possession of naloxone without a prescription (n = 4), dispenser immunity (n = 3) and immunity for lay dispensing (n = 2). Only one study each examined NAL components granting liability protections to lay administrators of naloxone, pharmacist direct dispensing authority or NALs. See Table 3 for details of study results and components evaluated.
Table 3.
Effect sizes of NALs and NAL components on overdose mortality, emergency department visits or naloxone prescriptions.
| Dichotomous naloxone access law | Naloxone possession without prescription | Prescriber immunity | Dispenser immunity | Third-party prescribing | Standing-order | Direct dispensing by pharmacists authorized | Protections to layperson for administering naloxone | Lay dispensing permitted | Prescribing requirements | |
|---|---|---|---|---|---|---|---|---|---|---|
| Naloxone prescriptions and distribution | ||||||||||
| Gertner [14] 2018a | 1.40*** (1.15, 1.66) | 1.62** (1.12, 2.12) | 0.41** (0.00, 0.96) | 1.84*** (1.33, 2.35) | 0.73 (0.00, 1.57) | |||||
| About [18] 2019a | 0.82 (0.00, 1.85) 3 years post-intervention | 1.95 (0.00, 4.91) 3 years post-intervention | 1.95 (0.30, 3.59) 3 years post-intervention | |||||||
| Xu [15] 2018 | 1.70** (1.13, 1.73) | 1.43** (1.28, 2.12) | ||||||||
| Lambdin [16] 2018 | 28.98*** (5.26, 159.61) times likely to have OEND | 45.97*** (7.91, 267.29) OEND | 5.19*** (1.57, 17.11) OEND | 3.50*** (1.15, 10.70) OEND | 12.86*** (3.01, 54.97) OEND | 11.45***(2.94, 44.94) OEND | 12.91*** (3.07, 54.26) OEND | |||
| Sohn [17] 2019 | 1.37*** (1.05, 1.78) | 7.75** (1.22, 49.35) | ||||||||
| Opioid-related overdose mortality | ||||||||||
| Doleac and Mukherjee [12] 2018a | All opioids: 1.01 (0.92, 1.10) Synthetic opioids: 0.96 (0.23, 1.70) |
|||||||||
| McClellan (20)2018b | 0.86** (0.78, 0.99) | 0.94(0.83, 1.03) | 0.77*** (0.68, 0.86) | 0.94 (0.71, 1.20) | 0.87 (0.72, 1.03) | 0.93 (0.79, 1.04) | ||||
| About [18] 2019a | 1.12 (0.95, 1.29) 3 years post-intervention | 1.12 (0.99, 1.25) 3 years post-intervention | 0.66*** (0.42, 0.90) 3 years post-intervention | |||||||
| Atkins [19] 2019 | All: 1.10 (0.94, 1.29) Rx: 1.16 (0.96, 1.40) Illicit: 1.14 (0.96, 1.36) | |||||||||
| Erfanian [20] 2019a,c | 1.03 (0.89, 1.18) | 1.05 (0.91, 1.19) | 0.97 (0.78, 1.16) | 0.93 (0.82, 1.03) | 0.97 (0.78, 1.16) | 1.27**(1.27, 1.27) | ||||
| Rees [21] 2019 | All: 0.91* (0.84, 0.98) Heroin: 0.95 (0.75, 1.21) | All: 0.84** (0.75, 0.95) Heroin: 0.88 (0.70, 1.09) | All: 0.95 (0.87, 1.05) Heroin: 0.68** (0.57, 0.80) | All: 1.15 (0.91, 1.44) Heroin: 1.38* (1.07, 1.78) | All: 0.94 (0.75, 1.19) Heroin: 0.91 (0.65, 1.29) | |||||
| Opioid-related emergency department visits | ||||||||||
| Blanchard [11] 2018 | 1.14*** (1.07, 1.20) | |||||||||
| Doleac and Mukherjee [12] 2018a | 1.15** (1.02, 1.29) | |||||||||
| About [18] 2019a | 1.03 (0.97, 1.08) 3 years post-intervention | 0.95 (0.84, 1.06) 3 years post-intervention | 1.15** (1.01, 1.29) 3 years post-intervention | |||||||
| Total | 7 | 4 | 5 | 3 | 8 | 9 | 1 | 1 | 2 | 1 |
P < 0.1
P < 0.05
P < 0.01.
Missing cells indicate component not examined. Studies shaded in grey consider naloxone policy components simultaneously instead of separately or as part of a composite measure. NAL = naloxone access law; NA = not applicable; OEND = overdose education and naloxone distribution.
Studies reported estimates as level changes. Incidence rate ratios (IRRs) and 95% confidence intervals (CIs) were approximated based on baseline mean information provided in the text or through communication with study authors
authors did not report coefficient estimates for all components in study. For McClellan et al. [13], incidence rate ratios (IRRs) and 95% confidence intervals (CIs) were approximated based on study figures
IRRs and 95% CIs are presented for estimates of own-state effects provided by the authors to maintain comparability with other studies. See text for discussion of estimated cross-border effects from this study.
Most studies controlled for other laws and policies that could be correlated with opioid control or overdose, most commonly PDMPs, overdose Good Samaritan laws, medical cannabis laws or access through dispensaries or Medicaid expansion. Only four studies considered the differential impacts that NALs may have on outcomes by opioid type (e.g. prescription or illicit). One considered regional variation in mortality, which may be related to local opioid environments, by estimating the effects of NALs across four census regions in the United States [12], and one considered differential effects for early (e.g. states that adopted NALs before 2011) versus late adopters [21].
Naloxone availability or distribution
Five studies evaluated whether NALs or various NAL components were related to changes in naloxone access [14–18]. Two examined naloxone prescriptions reimbursed by Medicaid specifically [14,18]. Gertner et al. [14] reported that a NAL, specified dichotomously, was associated with an increase of 18 naloxone prescriptions per state-quarter. Examining specific NAL components, the authors found generally beneficial associations with naloxone prescriptions except for third-party prescribing, which was associated with a reduction of approximately 21 prescriptions per state-quarter. However, given the high degree of correlation between third-party prescribing and standing-order policies, joint estimation of these two policy component effects within the same model threatens validity of their estimates and confidence intervals. In contrast to Gertner et al. [14], Abouk et al. [18] found no significant relationship of NALs (as specified by the authors) with naloxone prescriptions paid for by Medicaid between 2010 and 2016, but noted suggestive evidence of increased naloxone prescriptions among Medicaid enrollees.
Two studies evaluated the impact of NALs on naloxone prescriptions dispensed in retail pharmacies without restricting on payer. Both found significant increases in naloxone dispensing associated with third-party or standing-order provisions [15,17]. Additionally, Sohn and colleagues found that naloxone prescribing mandates are associated with almost eightfold increases in naloxone dispensing. However, at the time, only two states had adopted such a law; with less than 1 year of post-implementation data for both states, the extent to which these effects are generalizable is unclear.
Lastly, Lambdin et al. [16] evaluated whether NALs affected the presence of community-based OEND programs. They found that counties were almost 29 times more likely to have an OEND if their state had any form of a NAL. All NAL components were significantly associated with greater odds of a county having an OEND, with the largest effects for decriminalization of naloxone possession without a prescription, lay dispensing and third-party prescribing.
Overdose mortality
Six studies examined the association of NALs or NAL components with opioid overdose mortality (Table 3). Two studies using data to 2014 reported that NALs, specified as a dichotomous variable, were associated with a significant decrease in opioid overdose mortality [13,21]. However, when examining which specific NAL components drove these effects, findings were less consistent. McClellan et al. [13] reported a significant 23% reduction in overdoses related to prescriber immunity provisions; they found no significant relationship among four other NAL components, although all point estimates were negative. Covering the same time-frame, using the same source of outcome data and examining largely the same components, Rees et al. [21] instead found that removal of criminal liability for possession of naloxone without a prescription was significantly associated with 16%reductionsinopioidoverdosemortality,whileprescriber immunity provisions had limited effect.
However, three studies that extended the study time-frame to 2015 or 2016, just as the most recent fentanyl outbreak was unfolding in parts of the country, reported a null effect overall for NALs and overdose deaths [12,18,19], and one found an increase in overdose deaths following NAL adoption [20]. Using data from 1999 to 2016, Atkins et al. [19] found a statistically insignificant relationship between NAL passage and state-level opioid overdose mortality; based on a shorter time-frame (2010–15) and county-level data, Doleac & Mukherjee [12] also found small and insignificant effects of NALs that included third-party or standing-order provisions. Using a different categorization, Abouk et al. [18] similarly found insignificant effects for NALs other than those that provide pharmacists with direct authority to dispense naloxone, which were associated with a 34% decline in opioid mortality at 3 or more years post-implementation.
One study employed a spatial panel approach to model the effects of NALs with consideration of potential spillover effects on neighboring states [20]. For the state in which the NAL was passed, the authors estimated generally small and statistically insignificant effects on opioid overdose rates, with the exception of protections for lay administration of naloxone which were estimated to be associated with a significant increase in overdose deaths. In contrast, they found that almost all NAL components resulted in large increases in opioid overdose mortality in neighboring states, with the size of estimated effects on neighboring states exceeding within-state effects by an order of magnitude. While these findings indicate substantial cross-state externalities, the size of these estimated effects—particularly when considered relative to their estimates of the within-state effects of NALs—and precision of their estimates suggests potential model overparameterization or misspecification of the spatial model’s weight matrix.
Four studies [12,18,19,21] examined the relationship of NAL components with fatal overdoses involving different types of opioids. Two studies that considered NALs as a dichotomous variable found no statistical association between NALs and illicit opioid related mortality [19,21]. Rees and colleagues [21] found that prescriber immunity was associated with significant 32% declines in heroin-involved deaths and that third-party prescribing—while not significantly associated with changes in all opioid overdoses—was associated with a 38% increase in heroin-involved deaths. Evaluating synthetic opioid mortality specifically, Doleac & Mukherjee [12] found a null association nationally, but that synthetic opioid-related mortality increased by 84% in the Midwest and declined by 34% in the West. The reduced opioid overdose mortality associated with direct authority NALs as found in Abouk et al. [18] was primarily driven by reduced deaths involving opioid analgesics and synthetic opioids; it is worth noting that the direct authority states contributing to their identifying variation were located predominantly in the West (California, New Mexico, Oregon), which is consistent with findings by Doleac & Mukherjee [12] despite different operationalization of NAL policies.
Emergency department (ED) events
Three studies examined the association of NALs or NAL components with opioid-related ED visits, finding that NALs were associated with increases in ED episodes or re-admissions for opioid overdose. Blanchard et al. [11] reported that individuals who experienced an opioid-related ED visit in states with standing naloxone order laws had 14% higher odds of an opioid-related re-admission relative to individuals in states without such policies. Because their study design had potential limitations for causal inference, findings may reflect confounding differences between jurisdictions that chose to implement NALs versus those that did not, rather than causal effects of the policies of interest.
However, two other studies that examined NAL components and attempted to more clearly address confounders reported largely similar findings. Doleac & Mukherjee [12] reported a 15% increase in monthly opioid-related ED visits for NALs that allow third-party prescribing or had a standing-order policy in effect. Abouk and colleagues reported that NALs providing pharmacists with direct authority to prescribe naloxone were associated with a 15% increase in quarterly opioid-related ED visits, although other types of NALs showed null effects [18]. While the magnitudes of these findings were consistent they are somewhat puzzling, given that the two studies reported different results for the same or similar measures. Specifically, Abouk et al. [18] found that NALs granting indirect dispensing authority to pharmacists, which seems most closely related to the policy construct Doleac & Mukherjee [12] found to be associated with an increase in ED visits, had a negative but statistically insignificant relationship with those visits.
DISCUSSION
Overall, the evidence on NALs is more mixed than certain, although most studies report that NALs are associated with favorable outcomes, including increased distribution of naloxone and reductions in overdose fatalities. In part, this may be because studies examined different outcomes across different time-periods, sometimes using different sources of data. Additionally, there is a high degree of variation in the types of specific NAL components that authors chose to analyze and how they operationalized these components in their analyses.
Of the studies that evaluate the relationship between NALs and ED events involving opioid overdose, all report a positive association. We note that positive associations between NAL and overdose-related ED events may be entirely consistent with positive associations with naloxone distribution and negative associations with overdose mortality, as increased naloxone access may increase the probability that an individual survives an overdose and is seen in the ED.
In terms of NAL components, prescriber immunity appears to be significantly associated with decreases in overdose deaths, including heroin overdose deaths, and increases in naloxone dispensing. As nearly all state NALs include prescriber immunity provisions within their initial legislation, it is unclear whether these findings reflect an overall NAL effect or effects specific to granting prescribers protections from civil or criminal penalties. While third-party prescribing and non-patient-specific pharmacy distribution laws showed relatively consistent evidence of increasing pharmacy naloxone distribution and opioid-related ED episodes, their effects on overdose mortality were generally small and uncertain. Decriminalization of possessing naloxone without a prescription showed mixed effects on opioid overdose deaths and positive associations with presence of OEND programs.
Given the variation in NALs across states and over time, greater effort is needed to understand how the laws’ components contribute to their efficacy. This is challenging empirically, because components that make up NALs are highly correlated. While several studies attempted to address issues of collinearity by collapsing some policy components into a combined measure or estimated separate models for each characteristic, doing so limits the ability to tease out correlations specific to each. The development of a composite naloxone policy index measure, as performed in other contexts to evaluate diverse policy responses to the opioid crisis [5,7,22], could potentially facilitate a more parsimonious operationalization and evaluation of diverse NALs. However, these composite measures may have inherent trade-offs between allowing for potentially more robust empirical evaluations of the causal impacts of NALs versus providing policymakers with actionable information on which components of the policies impact their effectiveness.
Further, the current literature is limited in informing the extent to which the opioid environment within a state impacts the effectiveness of its NAL. In recent years, illicit opioids such as heroin and illicitly manufactured fentanyl have accounted for the vast majority of opioid overdose fatalities [1]. The same is probably true for non-fatal overdoses. Fentanyl’s exposure across states remains geographically concentrated [23], yet only a few studies account for the dominant source of harm associated with opioids in a given place and time by examining deaths involving heroin or fentanyl compared to all opioid-involved overdoses. Furthermore, few studies evaluate potential geographic variability in the effectiveness of NALs. Given marked regional variation in the severity of the opioid crisis, as well as regional differences in pharmacy and prescriber access, this may represent a promising area for future research.
Certain NAL components may be better targeted at different sources of opioid overdoses. For example, naloxone co-prescribing mandates may enhance access to those receiving prescribed opioid analgesics, but do little for people who use illicit opioids, while provisions that permit laypeople to distribute naloxone may preferentially improve access among people who use illicit drugs. Additionally, variations in the implementation of naloxone laws that are not captured in statute (e.g. out-of-pocket costs, available formulations and the types and locations of pharmacies that actually stock naloxone [24–26]) may moderate the effectiveness of NALs and opioid overdose-related outcomes.
We note that, even though the amount of naloxone available to laypeople has increased over time, it is still at a relatively low level compared to the number of individuals who are potentially at risk of opioid overdose [27]. With the exception of those that mandate naloxone prescription, all NALs to date passively modify the policy environment regarding naloxone access; they do not allocate funds for naloxone purchase or require that the medication be prescribed or distributed. It is possible that more proactive state NALs change at the federal level to make naloxone available over-the-counter, or policies that make naloxone available at no or minimal cost to patients, their family and the general public would lead to greater changes in measures of naloxone access and opioid-related harm.
Many of the studies in this review use pharmacy naloxone distribution as the outcome measure. However, there are several other important distribution channels, most notably community-based harm reduction programs, which distributed more than 1 million naloxone doses in 2019 [28], nearly double the number of naloxone prescriptions dispensed through retail pharmacies in 2018 [27]. Additionally, all studies reviewed here examine laws that were mainly designed to increase access to naloxone among laypeople. Concurrent with the expansion in these NALs, there has also been a significant increase in laws and policies authorizing lower levels of emergency medical services (EMS) personnel and other first responders (e.g. law enforcement) to carry and administer naloxone [29–31].
We identified no studies of the effects of NALs on opioid-related overdose outcomes that accounted for this potential increase in naloxone administration via these mechanisms. Failure to account for these channels of increased naloxone access may misattribute effects of NALs on mortality or overdose through these alternative channels to pharmacy distribution. More comprehensive and systematic collection of naloxone distribution data through OEND programs as well as administration via EMS and other first responders can offer further insights into the role they may play in the context of broader naloxone policy and programmatic efforts.
Overall, the weight of the evidence suggests that NALs increase naloxone distribution, but that this increase may be insufficient to overcome barriers in access and to consistently and significantly reduce opioid overdose mortality at the population level, particularly now that highly potent synthetic opioids are increasingly penetrating the illicit opioid supply. This suggests that while NALs may be necessary to significantly increase access to naloxone, current NALs may not be sufficient to significantly reduce opioid-related harm. Beyond reducing barriers, including costs, greater efforts to more clearly understand which NAL provisions, policies and naloxone formulations are best suited to those at highest risk are needed.
Supplementary Material
Table S1 Full Scopus Search String.
Table S2 List of Item Fields in Data Extraction Form.
Figure S1 Correlation plot of naloxone policy components, specified in levels.
Figure S2 Correlation plot of naloxone policy components, specified in first-differences.
Table S3 Dates of Adoption for Naloxone Access Laws and Naloxone Access Law Components.
Acknowledgements
This research was supported by the following grants from the National Institutes of Health: R21 DA045950 (R.S., Principal Investigator) and P50 DA046351 (B.D. Stein, Principal Investigator). We thank Megan S. Schuler, Sara E. Heins, Beth Ann Griffin, David Powell, Sierra Smucker, Rosalie Liccardo Pacula and Anita Szafran for their assistance with search strategy design and article identification. We also thank Lynn Polite for research assistance.
Footnotes
Declaration of interests
None.
Supporting Information
Additional supporting information may be found online in the Supporting Information section at the end of the article.
References
- 1.Scholl L, Seth P, Kariisa M, Wilson N, Baldwin G Drug and opioid-involved overdose deaths - United States, 2013–2017. Morb Mortal Wkly Rep 2018; 67: 1419–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Boyer EW Management of opioid analgesic overdose. N Engl J Med 2012; 367: 146–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.McDonald R, Campbell ND, Strang J Twenty years of take-home naloxone for the prevention of overdose deaths from heroin and other opioids—conception and maturation. Drug Alcohol Depend 2017; 178: 176–87. [DOI] [PubMed] [Google Scholar]
- 4.Davis CS, Carr D Legal changes to increase access to naloxone for opioid overdose reversal in the United States. Drug Alcohol Depend 2015; 157: 112–20. [DOI] [PubMed] [Google Scholar]
- 5.Haffajee RL, Mello MM, Zhang F, Zaslavsky AM, Larochelle MR, Wharam JF Four states with robust prescription drug monitoring programs reduced opioid dosages. Health Aff 2018; 37: 964–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mauri AI, Townsend TN, Haffajee RL The association of state opioid misuse prevention policies with patient- and provider-related outcomes: a scoping review. Milbank Q 2020; 98: 57–105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Pardo B Do more robust prescription drug monitoring programs reduce prescription opioid overdose? Addiction 2017; 112: 1773–83. [DOI] [PubMed] [Google Scholar]
- 8.Cerdá M, Ponicki WR, Smith N, Rivera-Aguirre A, Davis CS, Marshall BDL et al. Measuring relationships between proactive reporting state-level prescription drug monitoring programs and county-level fatal prescription opioid overdoses. Epidemiology 2020; 31: 32–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Prescription Drug Abuse Policy System (PDAPS) [internet]. 2018. Available at: http://www.pdaps.org/ (accessed 18 November 2019).
- 10.Schuler M, Heins S, Smart R, Pardo B, Powell D, Smucker S et al. The State of the Science in Opioid Policy Research. Drug and Alcohol Dependence; in press; 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Blanchard J, Weiss AJ, Barrett ML, McDermott KW, Heslin KC State variation in opioid treatment policies and opioid-related hospital readmissions. BMC Health Serv Res 2018; 18: 971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Doleac JL, Mukherjee A. The moral hazard of lifesaving innovations: naloxone access, opioid abuse, and crime. IA discussion Papers 11489. Bonn, Germany: Zukunft der Arbeit GmbH (Institute of Labor Economics) (IZA); 2018. [Google Scholar]
- 13.McClellan C, Lambdin BH, Ali MM, Mutter R, Davis CS, Wheeler E et al. Opioid-overdose laws association with opioid use and overdose mortality. Addict Behav 2018; 86: 90–5. [DOI] [PubMed] [Google Scholar]
- 14.Gertner AK, Domino ME, Davis CS Do naloxone access laws increase outpatient naloxone prescriptions? Evidence from Medicaid. Drug Alcohol Depend 2018; 190: 37–41. [DOI] [PubMed] [Google Scholar]
- 15.Xu J, Davis CS, Cruz M, Lurie P State naloxone access laws are associated with an increase in the number of naloxone prescriptions dispensed in retail pharmacies. Drug Alcohol Depend 2018; 189: 37–41. [DOI] [PubMed] [Google Scholar]
- 16.Lambdin BH, Davis CS, Wheeler E, Tueller S, Kral AH Naloxone laws facilitate the establishment of overdose education and naloxone distribution programs in the United States. Drug Alcohol Depend 2018; 188: 370–6. [DOI] [PubMed] [Google Scholar]
- 17.Sohn M, Talbert JC, Huang Z, Lofwall MR, Freeman PR Association of naloxone coprescription laws with naloxone prescription dispensing in the United States. JAMA Netw Open 2019; 2: e196215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Abouk R, Pacula RL, Powell D Association between state laws facilitating pharmacy distribution of naloxone and risk of fatal overdose. JAMA Intern Med 2019; 179: 805–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Atkins DN, Durrance CP, Kim Y Good Samaritan harm reduction policy and drug overdose deaths. Health Serv Res 2019; 54: 407–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Erfanian E, Grossman D, Collins AR The impact of naloxone access laws on opioid overdose deaths in the US. Rev Reg Stud 2019; 49: 45–72. [Google Scholar]
- 21.Rees DI, Sabia JJ, Argys LM, Dave D, Latshaw J With a little help from my friends: the effects of good Samaritan and naloxone access laws on opioid-related deaths. J Law Econ 2019; 62: 1–27. [Google Scholar]
- 22.Martins SS, Ponicki W, Smith N, Rivera-Aguirre A, Davis CS, Fink DS et al. Prescription drug monitoring programs operational characteristics and fatal heroin poisoning. Int J Drug Policy 2019; 74: 174–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Pardo B, Taylor J, Caulkins JP, Kilmer B, Reuter P, Stein BD. The Future of Fentanyl and Other Synthetic Opioids [internet]. 2019. Available at: https://www.rand.org/pubs/research_reports/RR3117.html. (accessed 10 February 2020).
- 24.Dietze P, Jauncey M, Salmon A, Mohebbi M, Latimer J, van Beek I et al. Effect of intranasal vs intramuscular naloxone on opioid overdose: a randomized clinical trial. JAMA Netw Open 2019; 2: e1914977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Wu C, Brown T, Moreno JL. Access to naloxone at community pharmacies under the Massachusetts statewide standing order. J Am Pharm Assoc [internet]. 2019. Available at: http://www.sciencedirect.com/science/article/pii/S1544319119305151. (accessed 10 February 2020). [DOI] [PubMed]
- 26.Guadamuz JS, Alexander GC, Chaudhri T, Trotzky-Sirr R,Qato DM Availability and cost of naloxone nasal spray at pharmacies in Philadelphia, Pennsylvania, 2017. JAMA Netw Open 2019. June 5; 2: e195388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Guy GP, Haegerich T, Evans M, Losby J, Young R, Jones C. Vital Signs: Pharmacy-Based Naloxone Dispensing—United States, 2012–2018. Morb Mortal Wkly Rep [internet]. 2019; 68. Available at: https://www.cdc.gov/mmwr/volumes/68/wr/mm6831e1.htm. (accessed 13 December 2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Wheeler E, Doe-Simkins M. Harm reduction programs distribute one million doses of naloxone in 2019 [internet]. Medium. 2020. Available at: https://medium.com/@ejwharmreduction/harm-reduction-programs-distribute-one-million-doses-of-naloxone-in-2019-4884d3535256. (accessed 4 January 2020). [Google Scholar]
- 29.Davis CS, Carr D, Southwell JK, Beletsky L Engaging law enforcement in overdose reversal initiatives: authorization and liability for naloxone administration. Am J Public Health 2015; 105: 1530–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Geiger C, Smart R, Stein BD Who receives naloxone from emergency medical services? Characteristics of calls and recent trends. Subst Abuse 20191–8; 10.1080/08897077.2019.1640832 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kinsman JM, Robinson K National systematic legal review of state policies on emergency medical services licensure levels’ authority to administer opioid antagonists. Prehosp Emerg Care 2018; 22: 650–4. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1 Full Scopus Search String.
Table S2 List of Item Fields in Data Extraction Form.
Figure S1 Correlation plot of naloxone policy components, specified in levels.
Figure S2 Correlation plot of naloxone policy components, specified in first-differences.
Table S3 Dates of Adoption for Naloxone Access Laws and Naloxone Access Law Components.