Abstract
Objectives:
To evaluate the condyle-fossa relationship in adolescents with various skeletal patterns using cone-beam computed tomography (CBCT).
Materials and Methods:
CBCT images obtained in 120 adolescent patients were used for this study. The patients were divided into 3 groups according to 3 criteria: (1) age (early, middle, and late adolescence); (2) facial height ratio or Jarabak quotient (hyperdivergent, normodivergent, and hypodivergent); and (3) ANB classification (Class I, Class II, and Class III). Temporomandibular joint space (TMJS: AS, anterior space; SS, superior space; PS, posterior space; MS, medial space; LS, lateral space), width and depth of the condyle (MLT, mediolateral thickness; APT, anteroposterior thickness), articular slope (ArS) and vertical height of the fossa (VHF) were measured and compared using CBCT.
Results:
Differences in condyle-fossa relationships were not significantly different between male and female adolescents, but were significantly different (P < .05) between left and right sides. The mean values showed no statistical differences according to age and skeletal pattern. Most measurements in the sagittal view showed that SS was the greatest, and the mean ratio of AS to SS to PS was 1.00 to 1.27 to 1.19, respectively. The mean values of coronal MS and LS were not significantly different.
Conclusions:
There were almost no statistical differences in the TMJS in adolescents across various factors except between left and right sides.
Keywords: Condyle-fossa relationship, TMJS, Skeletal patterns, CBCT
INTRODUCTION
Skeletal patterns are analyzed and classified by vertical disproportions (hyperdivergent, normovergent, and hypodivergent) and by anteroposterior disproportions (skeletal Class I, II, and III) for orthodontic diagnosis.1–3 Condyle-fossa relationship varies according to sagittal and vertical facial morphology. Therefore, the relationship between condylar position and skeletal patterns should be considered when planning and executing a proper treatment plan for temporomandibular anomalies during orthodontic treatment.4,5
The optimal position of the condyle in the glenoid fossa is a fundamental question in dentistry. Controversy persists over the clinical significance of condylar position in the temporomandibular joint (TMJ).6,7 The condylar position is an end product of many dynamic changes, such as growth, remodeling, responses to functional changes and occlusal alterations.6,8 Concentric condylar position is considered a normal relationship between the condyle and fossa and is usually found in asymptomatic participants.9–11 Nonconcentric condyle-fossa relationships have been associated with abnormal TMJ function.10,12–18 However, in other studies,4,5,13,19–22 the presence or absence of temporomandibular disorder (TMD) did not correlate with the condyle position in the TMJ.
Centric relation (CR) is defined as a musculoskeletal stable maxillomandibular relationship, with the condyles in the anterosuperior position against the slope of the articular eminence, centered transversely and with the articular disc properly interposed, while centric occlusion (CO) or maximum intercuspal position is a dentally determined position.23–25 There can be a significant difference in the occlusion when it is dictated by the teeth versus when it is dictated by the condyles. In diagnosis and treatment planning for orthodontic patients CO-CR discrepancies are of clinical significance.26 There may be a direct correlation between CO-CR discrepancies and the probability that a patient will develop TMD.23–25
The influence of occlusion on the condyle-fossa relationship is still controversial. Some research has noted the influence of occlusion in the condylar process–mandibular fossa relationship,4,5,10,13–15,27–33 while others have not.4,5,13,19–22 Studies have found that the condyles were positioned more anteriorly,4,5,10,13–15,27,28 posteriorly,27,29,30 intermediately,27 superiorly27,28,31,32 and inferiorly33 in various occlusal, skeletal, and facial relationships. In addition to condylar position, occlusion might be related to the articular eminence angle or slope13,14,28 and articular eminence height,14,16,17 or the vertical height of the fossa13,19,28,31 and anteroposterior and mediolateral thickness of the condylar head.17,19,31
The condyle-fossa relationship might also be related to sex,13,34–36 age,1,3,27,29,36 and side (left and right),13,15–17,20,35 but few studies have focused on adolescent patients using cone-beam computed tomography (CBCT) images. CBCT allows examination of the TMJ anatomy without superimposition and distortion to facilitate analysis of bone morphology, joint space, and dynamic function in all 3 dimensions by overcoming the limitation of other imaging modalities, such as panoramic radiography and computed tomography.37,38 The aim of this study was to use CBCT to measure and compare the condyle-fossa relationship in adolescents with various skeletal patterns.
MATERIALS AND METHODS
Sample-Size Calculation
A power analysis using G*Power (version 3.19.2; Franz Faul, Christian-Albrechts-Universitat, Kiel, Germany) was performed to estimate the sample size required for this study. In order to detect a difference using analysis of variance (ANOVA) between group means, effect size f = 0.45, 108 participants were required to achieve a power exceeding 0.90, P = .05.
Participants, Eligibility Criteria, and CBCT
Adolescent patients (10 to <20 years old) who had initial CBCT images taken in C-mode at the Department of Orthodontics, Wonkwang University Daejeon Hospital, were selected as participants. Images were taken by the same radiographer using 3 guidance pins to align the patients' head when sitting in an upright position to obtain the Frankfort horizontal (FH) plane, which was parallel to the floor, and with the patients instructed to bite in CO. Exclusion criteria included previous orthodontic treatment, CO-CR discrepancy, history of trauma to the dentofacial region, skeletal asymmetry, TMJ disorders, and general diseases that could influence bone tissue metabolism.
The study was conducted with 120 adolescent patients, 56 males and 64 females. They were classified into 3 groups according to age: early adolescence (10 to <14 years), middle adolescence (14 to <17 years), and late adolescence (17 to <20 years).24 The participants were divided into vertical skeletal groups based on facial height ratio (FHR) or the Jarabak quotient, a ratio of posterior facial height (PFH, S-Go) to anterior facial height (AFH, N-Me).3,25 These 3 groups were hypodivergent (FHR > 65%), normodivergent (FHR 62% to ≤65%), and hyperdivergent (FHR < 62%). Patients were also categorized into 1 of 3 horizontal skeletal groups based on ANB angle: Class I (ANB 1° to ≤4°), Class II (ANB > 4°), and Class III (ANB < 1°) (Table 1).
Table 1.
Sample Distribution (No.)a
| Variables |
Sex |
Age, y |
FHR |
ANB |
||||||||
| Male |
Female |
Early |
Middle |
Late |
Hyperdivergent |
Normovergent |
Hypodivergent |
Class III |
Class I |
Class II |
||
| 10 to <14 |
14 to <17 |
17 to <20 |
FHR <62% |
62% ≤ FHR ≤ 65% |
FHR > 65% |
ANB < 1° |
1° ≤ ANB ≤ 4° |
ANB > 4° |
||||
| Sex | Male | 56 | 16 | 20 | 20 | 12 | 19 | 25 | 19 | 19 | 18 | |
| Female | 64 | 24 | 20 | 20 | 27 | 16 | 21 | 12 | 18 | 34 | ||
| Age | Early | 16 | 24 | 19 | 16 | 5 | 7 | 11 | 22 | |||
| Middle | 20 | 20 | 10 | 10 | 20 | 7 | 14 | 19 | ||||
| Late | 20 | 20 | 10 | 9 | 21 | 17 | 12 | 11 | ||||
| FHR | Hyperdivergent | 12 | 27 | 19 | 10 | 10 | 5 | 8 | 26 | |||
| Normovergent | 19 | 16 | 16 | 10 | 9 | 10 | 11 | 14 | ||||
| Hypodivergent | 25 | 21 | 5 | 20 | 21 | 16 | 18 | 12 | ||||
| ANB | Class III | 19 | 12 | 7 | 7 | 17 | 5 | 10 | 16 | |||
| Class I | 19 | 18 | 11 | 14 | 12 | 8 | 11 | 18 | ||||
| Class II | 18 | 34 | 22 | 19 | 11 | 26 | 14 | 12 | ||||
| Total (each) | 120 | 40 | 40 | 40 | 39 | 35 | 46 | 31 | 37 | 52 | ||
FHR indicates facial height ratio (%): posterior facial height (S-Go) / anterior facial height (N-Me).
The CBCT (PSR 9000N; Asahi Alphard Vega, Kyoto, Japan) images were taken in C-mode (scan size, 200 × 179 mm; voxel size, 0.39 mm; field of view, 19.97 cm). The radiologic parameters used were 80 kVp, 60 mAs, and 17-second scan time. The CBCT data were saved in digital imaging and communications in medicine (DICOM) files, and Simplant Pro 2011 pack software (version 13; Materialise, Leuven, Belgium) was used to analyze the DICOM data to generate the quantitative measurements.
Institutional review board approval was granted by Wonkwang University Dental Hospital (No. WKD IRB W1804/002-001) in Daejeon, Korea, to conduct this study.
Study Design
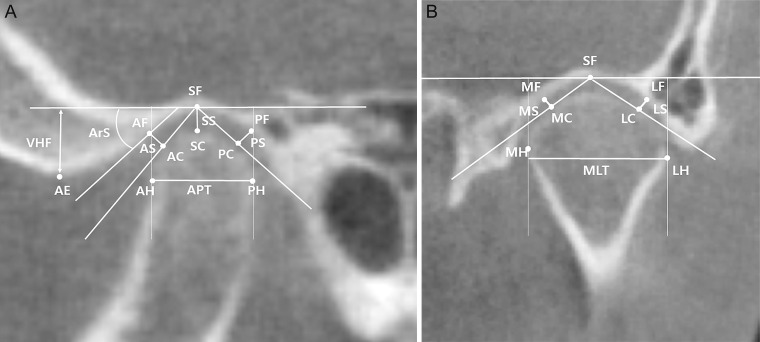
Condyle-fossa relationship was investigated by one investigator (Dr Mizutani) who was blinded to the patient groups. The constructed images were oriented with the FH plane aligned horizontally, where the FH plane was constructed by orbitale on the right side and porion on both sides (Figure 1). The TMJs on the left and right sides were evaluated separately. For TMJ evaluation, the slices that showed the greatest anteroposterior and mediolateral dimension of the condylar head were selected on the sagittal and coronal views, respectively. The landmarks were digitized using Dolphin®11.9 software (Dolphin Imaging and Management Solutions, Chatsworth, Calif), and linear and angular measurements were made. The landmarks and linear and angular measurements used for analysis are illustrated in Figure 2A, B: TMJ space (TMJS: AS, anterior space; SS, superior space; PS, posterior space; MS, medial space; LS, lateral space), width and depth of the condyle (MLT, mediolateral thickness; APT, anteroposterior thickness), articular slope (ArS), and vertical height of the fossa (VHF). TMJSs were measured as the shortest distance between 2 points: AS, anterior fossa (AF), and anterior condyle (AC); SS, superior fossa (SF), and superior condyle (SC); PS, posterior fossa (PF), and posterior condyle (PC); MS, medial fossa (MF), and medial condyle (MC); LS, lateral fossa (LF), and lateral condyle (LC). MLT was the distance between the medial head (MH) and lateral head (LH) lines perpendicular to the FH plane. APT was the distance between the anterior head (AH) and posterior head (PH) lines perpendicular to the FH plane. ArS was the angle between the FH plane and a line tangent to the anterior slope of the fossa, and VHF was the perpendicular distance from the FH plane to the articular eminence (AE).
Figure 1.
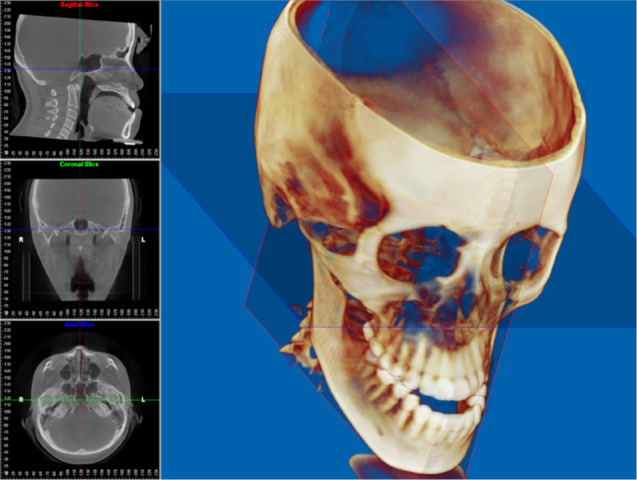
Cone-beam computed tomography orientation: Ba indicates basion; CG, Crista Galli; FH-plane, Frankfurt horizontal plane; MS-plane, midsagittal plane; Or, orbitale; Po, porion.
Figure 2.
Landmarks and measurements. (A) Sagittal view with the greatest condylar head. (B) Coronal view with the greatest condylar head. AC indicates anterior condyle; AE, articular eminence; AF, anterior fossa; AH, anterior head; APT, anteroposterior thickness; ArS, articular slope; AS, anterior space; LC, lateral condyle; LF, lateral fossa; LH, lateral head; LS, lateral space; MC, medial condyle; MF, medial fossa; MH, medial head; MLT, mediolateral thickness; MS, medial space; PC, posterior condyle; PF, posterior fossa; PH, posterior head; PS, posterior space; SC, superior condyle; SF, superior fossa; SS, superior space; VHF, vertical height of fossa..
Statistical Analysis
One investigator (Dr Mizutani) performed all the measurements on 120 participants. To test the reliability of the measurements, 30 CBCT images were randomly selected for remeasurement 3 weeks after the initial measurement. The intraclass correlation coefficient (ICC) showed excellent test-retest reliability (ICC = 0.96–1.00).
SPSS software (version 24.0 for Windows; SPSS Corp, Chicago, Ill) was used for statistical analyses. A Shapiro-Wilk normality test was performed, and a nonparametric test was performed when normality was not satisfied.
Independent sample t-test, analysis of variance. and paired t-test were used to compare the patients' condyle-fossa relationships according to sex, age, side of condyle, and skeletal patterns (Tables 2 and 3). ANOVA was used to compare the mean values of joint spaces according to vertical and horizontal skeletal pattern (FHR and ANB) (Table 4). The results of the Kruskal-Wallis test were presented when the variance analysis did not satisfy normality and homogeneity of variance test results. When the ANOVA was significant, a Scheffe's post-test was conducted. ANOVA was performed to compare the joint spaces (sagittal AS, SS, and PS) and an independent sample t-test was performed to compare the joint spaces (coronal MS and LS) (Tables 2 through 4). Significance was established at P < .05.
Table 2.
Mean Values of Joint Spaces According to Sex, Age, and Side of Condylea
| Mean |
|||||||||
| Total (n = 120) |
Ratio |
SD |
Male (n = 56) |
SD |
Female (n = .64) |
SD |
P Value |
||
| Sagittal view | AS (mm) | 2.33a | 1.00 | 0.46 | 2.29a | 0.41 | 2.36a | 0.51 | .466 |
| SS (mm) | 2.96b | 1.27 | 0.68 | 2.97c | 0.66 | 2.96b | 0.70 | .953 | |
| PS (mm) | 2.78b | 1.19 | 0.71 | 2.68b | 0.62 | 2.87b | 0.78 | .155 | |
| P value | .000*** (.000***) | .000*** (.000***) | .000*** (.000***) | ||||||
| ArS (°) | 48.78 | 8.04 | 50.17 | 7.00 | 47.56 | 8.73 | .076 | ||
| VHF (mm) | 6.43 | 1.37 | 6.79 | 1.36 | 6.12 | 1.32 | .008** | ||
| APT (mm) | 8.62 | 1.20 | 8.63 | 1.07 | 8.60 | 1.31 | .890 | ||
| Coronal view | MS (mm) | 2.65 | 1.00 | 0.57 | 2.67 | 0.57 | 2.63 | 0.58 | .690 |
| LS (mm) | 2.78 | 1.05 | 0.80 | 2.78 | 0.78 | 2.79 | 0.81 | .955 | |
| P value | .134 (.393) | .406 (.745) | .208 | ||||||
| MLT (mm) | 17.16 | 2.35 | 17.22 | 2.48 | 17.11 | 2.25 | .816 | ||
Same letters mean no statistical differences; a, b, c. The Shapiro-Wilk normality test was performed and the nonparametric test results are presented in parentheses when normality is not satisfied. APT indicates anteroposterior thickness; AS, anterior space; ArS, articular slope; LS, lateral space; MLT, mediolateral thickness; MS, medial space; PS, posterior space; SD, standard deviation; SS, superior space; VHF, vertical height of fossa;. * P < .05, ** P < .01, *** P < .001.
Table 2.
Extended
| Mean | |||||||||||
| Early 10 to <14 y (n = 40) |
SD |
Middle 14 to <17 y (n = 40) |
SD |
Late 17 to <20 y (n = 40) |
SD |
P Value |
Right (n = .20) |
SD |
Left (n = 120) |
SD |
P Value |
| 2.29a | 0.48 | 2.34a | 0.38 | 2.35a | 0.52 | .811 | 2.30a | 0.62 | 2.36a | 0.61 | .405 |
| 2.93b | 0.65 | 2.99b | 0.67 | 2.98b | 0.72 | .906 | 2.87b | 0.76 | 3.06b | 0.81 | .011* |
| 2.77b | 0.73 | 2.82b | 0.61 | 2.75b | 0.80 | .880 | 2.69b | 0.78 | 2.87b | 0.92 | .038* |
| .000*** (.000***) | .000*** (.000***) | .000*** (.001***) | .000*** (.000***) | .000*** (.000***) | |||||||
| 49.01 | 7.38 | 47.64 | 8.58 | 49.68 | 8.19 | .516 | 47.73 | 10.22 | 49.82 | 9.04 | .034* |
| 6.35 | 1.27 | 6.17 | 1.29 | 6.77 | 1.51 | .135 | 6.43 | 1.50 | 6.44 | 1.43 | .862 |
| 8.74 | 1.33 | 8.54 | 0.94 | 8.57 | 1.32 | .712 | 8.78 | 1.25 | 8.45 | 1.46 | .005** |
| 2.63 | 0.47 | 2.66 | 0.59 | 2.66 | 0.66 | .982 | 2.49 | 0.71 | 2.81 | 0.73 | .000*** |
| 2.74 | 0.64 | 2.89 | 0.71 | 2.73 | 1.00 | .606 | 2.69 | 0.71 | 2.87 | 1.23 | 0.109 |
| .418 | .116 | .710 | .031* (.007) | .595 (.413) | |||||||
| 17.08 | 2.09 | 16.93 | 2.43 | 17.47 | 2.54 | .579 | 17.23 | 2.52 | 17.09 | 2.56 | .425 |
Table 3.
Mean Values of Joint Spaces According to Vertical and Horizontal Skeletal Patterns (FHR and ANB)
| Mean |
||||||||||
| Total (n = 120) |
SD |
Hyperdivergent FHR < 62% (n = 39) |
SD |
Normovergent 62% ≤ FHR≤ 65% (n = 35) |
SD |
Hypodivergent FHR > 65% (n = 46) |
SD |
P Value |
||
| Sagittal view | AS (mm) | 2.33a | 0.46 | 2.29a | 0.52 | 2.32a | 0.48 | 2.36a | 0.41 | .753 |
| SS (mm) | 2.96b | 0.68 | 2.81b | 0.74 | 3.02b | 0.63 | 3.06b | 0.64 | .197 | |
| PS (mm) | 2.78b | 0.71 | 2.72b | 0.82 | 2.69b | 0.68 | 2.90b | 0.64 | .344 | |
| P value | .000*** (.000***) | .003** | .000*** | .000*** (.000***) | ||||||
| ArS (°) | 48.78 | 8.04 | 48.78 | 8.97 | 48.77 | 7.15 | 48.78 | 8.03 | 1.000 | |
| VHF (mm) | 6.43 | 1.37 | 6.54 | 1.46 | 6.38 | 1.36 | 6.38 | 1.33 | .832 | |
| APT (mm) | 8.62 | 1.20 | 8.47 | 0.91 | 8.90 | 1.18 | 8.52 | 1.40 | .240 | |
| Coronal view | MS (mm) | 2.65 | 0.57 | 2.63 | 0.55 | 2.76 | 0.54 | 2.58 | 0.62 | .372 |
| LS (mm) | 2.78 | 0.80 | 2.68 | 0.73 | 2.87 | 0.73 | 2.81 | 0.90 | .569 | |
| P value | .134 (.393) | .749 | .487 | .155 (.314) | ||||||
| MLT (mm) | 17.16 | 2.35 | 16.72 | 2.44 | 17.49 | 2.45 | 17.29 | 2.19 | .332 | |
Same letters mean no statistical differences; a, b. The Shapiro-Wilk normality test was performed and the nonparametric test results are presented in parentheses when normality is not satisfied, APT indicates anteroposterior thickness; AS, anterior space; ArS, articular slope; LS, lateral space; MLT, mediolateral thickness; MS, medial space; PS, posterior space; SD, standard deviation; SS, superior space; VHF, vertical height of fossa. * P < .05, ** P < .01, *** P < .001.
Table 3.
Extended
| Mean | ||||||
| Class III ANB < 1° (n = 31) |
SD |
Class I 1°≤ ANB ≤ 4° (n = 37) |
SD |
Class II ANB > 4° (n = 52) |
SD |
P Value |
| 2.35a | 0.51 | 2.27a | 0.44 | 2.36a | 0.45 | .651 |
| 2.89b | 0.65 | 3.02b | 0.61 | 2.97b | 0.74 | .720 |
| 2.63a,b | 0.65 | 2.78b | 0.72 | 2.87b | 0.74 | .331 |
| .003** | .000*** (.000***) | .000*** (.000***) | ||||
| 47.13 | 6.65 | 49.50 | 8.88 | 49.25 | 8.18 | .414 |
| 6.31 | 1.25 | 6.48 | 1.47 | 6.48 | 1.39 | .838 |
| 8.27 | 1.15 | 8.93 | 1.46 | 8.60 | 0.97 | .077 |
| 2.60 | 0.51 | 2.63 | 0.61 | 2.69 | 0.59 | .744 |
| 2.60 | 0.69 | 2.94 | 0.78 | 2.78 | 0.86 | .221 |
| 0.969 | .062 | .546 (.969) | ||||
| 17.59 | 2.09 | 17.25 | 2.57 | 16.84 | 2.33 | .362 |
Table 4.
Mean Values of j\Joint Spaces According to Vertical and Horizontal Skeletal Patterns (FHR and ANB) a
| Mean |
||||||||
| Class III ANB < 1° (n = 31) | ||||||||
| Hyperdivergent FHR < 62% (n = 5) |
SD |
Normovergent 62% ≤ FHR ≤ 65% (n = 10) |
SD |
Hypodivergent FHR > 65% (n = 16) |
SD |
P Value |
||
| Sagittal view | AS (mm) | 2.43 | 0.69 | 2.39 | 0.60 | 2.30a | 0.42 | .861 |
| SS (mm) | 2.89 | 0.62 | 2.91 | 0.83 | 2.87b | 0.57 | .986 (.973) | |
| PS (mm) | 2.79 | 0.51 | 2.30 | 0.51 | 2.79a,b | 0.71 | .140 | |
| P value | .470 (.228) | .097 (.119) | .016* (.031*) | |||||
| ArS (°) | 44.72 | 5.47 | 47.15 | 8.58 | 47.86 | 5.80 | .669 | |
| VHF (mm) | 5.84 | 0.81 | 6.52 | 1.18 | 6.32 | 1.42 | .627 (.624) | |
| APT (mm) | 8.22 | 1.41 | 8.53 | 1.42 | 8.13 | 0.91 | .707 | |
| Coronal view | MS (mm) | 2.68 | 0.26 | 2.59 | 0.61 | 2.57 | 0.53 | .919 |
| LS (mm) | 2.78 | 0.90 | 2.68 | 0.89 | 2.50 | 0.47 | .687 | |
| P value | .827 | .808 | .695 | |||||
| MLT (mm) | 16.62 | 1.97 | 18.14 | 2.30 | 17.56 | 2.01 | .429 | |
Same letters mean no statistical differences; a, b. Kruskal-Wallis test results are presented in parentheses when the homogeneity of variance and the normality are not satisfied. APT indicates anteroposterior thickness; AS, anterior space; ArS, articular slope; LS, lateral space; MLT, mediolateral thickness; MS, medial space; PS, posterior space; SD, standard deviation; SS, superior space; VHF, vertical height of fossa. * P < .05, ** P < .01, *** P < .001.
Table 4.
Extended
| Mean | ||||||
| Class I 1° ≤ ANB ≤ 4° (n = 37) | ||||||
| Hyperdivergent FHR < 62% (n = 8) |
SD |
Normovergent 62% ≤ FHR≤ 65% (n = 11) |
SD |
Hypodivergent FHR > 65% (n = 8) |
SD |
P Value |
| 2.17 | 0.53 | 2.25a | 0.54 | 2.32a | 0.35 | .718 |
| 2.86 | 0.73 | 3.06b | 0.70 | 3.07b | 0.52 | .715 |
| 2.42 | 0.92 | 2.83a,b | 0.69 | 2.91b | 0.62 | .269 |
| .196 | .018* | .000*** (.001**) | ||||
| 54.58 | 6.36 | 48.80 | 7.95 | 47.66 | 9.86 | .180 (.462) |
| 6.97 | 1.60 | 6.23 | 1.76 | 6.41 | 1.25 | .554 |
| 8.60 | 0.82 | 9.05 | 1.22 | 9.01 | 1.82 | .777 |
| 2.82 | 0.65 | 2.61 | 0.47 | 2.56 | 0.68 | .609 |
| 3.10 | 0.66 | 2.93 | 0.73 | 2.88 | 0.89 | .800 |
| .404 | .241 | .237 | ||||
| 17.82 | 2.11 | 16.74 | 3.03 | 17.31 | 2.55 | .675 |
Table 4.
Extended
| Mean |
|||||||
| Class II ANB > 4° (n = 52) |
|||||||
| Hyperdivergent FHR < 62% (n = 26) |
SD |
Normovergent 62% ≤ FHR ≤ 65% (n = 14) |
SD |
Hypodivergent FHR > 65% (n = 46) |
SD |
P Value |
P Value |
| 2.30a | 0.50 | 2.34a | 0.34 | 2.51a | 0.47 | .412 | .897 |
| 2.77a,b | 0.79 | 3.07b | 0.42 | 3.29b | 0.85 | .112 | .597 |
| 2.80b | 0.84 | 2.85b | 0.70 | 3.04b | 0.59 | .653 (.324) | .334 |
| .023* (.033*) | .002** (.002**) | .019* | |||||
| 47.78 | 9.54 | 49.90 | 5.53 | 51.68 | 7.43 | .378 | .379 |
| 6.55 | 1.51 | 6.40 | 1.20 | 6.42 | 1.44 | .935 | .954 |
| 8.48 | 0.86 | 9.06 | 0.99 | 8.32 | 1.05 | .096 (.146) | .298 |
| 2.56 | 0.56 | 3.00 | 0.48 | 2.63 | 0.67 | .072 | .507 |
| 2.53 | 0.70 | 2.95 | 0.61 | 3.13 | 1.24 | .085 (.0780) | .287 |
| .847 | .837 | .229 | |||||
| 16.40 | 2.58 | 17.62 | 2.05 | 16.90 | 1.95 | .290 | .558 |
RESULTS
There were no statistical differences in condyle-fossa relationships between male and female participants except for VHF (P = .008). While the mean values of sagittal SS (P = .011), PS (P = .038), ArS (P = .034), and MS (P < .001) were greater on the left than right sides, the mean value of APT (P = .005) was greater on the right than left sides (Table 2). The mean values showed no statistical differences according to age and vertical and horizontal skeletal patterns (Tables 2 and 3). While the mean values of sagittal AS, SS, and PS were significantly different, the mean values of coronal MS and LS were not significantly different except on the right side (P = .031). Most measurements in the sagittal view showed that SS was the greatest and AS was statistically smaller than SS and PS (P < .05). The mean ratio of AS to SS to PS was 1.00 to 1.27 to 1.19, respectively (Tables 2 through 4).
DISCUSSION
The condyle-fossa relationship has varied according to sagittal and vertical skeletal patterns in several studies.1–5 This study demonstrated that there were only some differences in condylar position inside the glenoid fossa. The condyle was positioned more inferiorly in hypodivergent than hyperdivergent Class II skeletal patterns (Table 4), which was similar to findings of previous studies.27,28,31,39 Burke et al.39 believed that reduced sagittal SS in hyperdivergent tendency reflected reduced condylar tissue and predicted decreased condylar growth potential that would eventually result in increased AFH during growth and development. This might be used to predict the growth patterns and/or growth potential of the mandible in future studies.
Previous studies demonstrated that the condyles were positioned more anteriorly in Class II patients whether they had horizontal4,10,14,27 or vertical5 skeletal patterns. In this study, PS increased in the Class II skeletal pattern, but this relationship was not statistically significant. Anteroposterior condylar position might be related with TMD. In a previous study,27 the condyle was positioned more posteriorly in Class II, division 2 patients, and this might cause severe TMD by more physical loading. Adequate TMJS would be necessary to avoid excessive compression of the disc.40 Therefore, TMJS should be investigated for orthodontic patients to prevent TMD. A limitation of this study, however, was that it did not involve Class II, division 2 patients due to their small sample size.
The mean value of VHF was greater in male than in female participants, which was consistent with a previous study,13 but other values were not statistically different between sexes.35 On the basis of age, there were no significant differences in the growing children, which might suggest that a constant condyle-fossa relationship is maintained during growth.13 However, other studies have showed significant differences associated with radiographic abnormalities between sexes and between females of varying ages, and the condyles were positioned more posteriorly in adults than in adolescents.13,36 However, the current study was limited to adolescents, so further research including adults might be recommended.
This study demonstrated significant differences in condylar position between the right and left sides, which was consistent with the results of previous studies.13,15–17 However, other studies have shown no differences in joint spaces and ratios between sides.20,35 Therefore, controversy exists regarding condyle-fossa relationships. This may be due to inconsistencies in research methods.
Concentric condylar position in the glenoid fossa is usually considered optimal, but this remains controversial.6,41 The optimal condylar position can be determined by the TMJS. The TMJS is a radiographic term referring to the space between the condyle and glenoid fossa. Ikeda and Kawamura41 obtained norms of TMJS from optimal joints using limited CBCT. The mean AS, SS, and PS values were 1.3 mm, 2.5 mm, and 2.1 mm, respectively, and the ratio of AS to SS to PS was 1.0 to1.9 to 1.6, respectively. These results were different from those in the current study, but the tendencies of TMJS were similar to the results of this study: AS (2.33 mm), SS (2.96 mm), PS (2.78 mm), AS to SS to PS (1.00 to 1.27 to 1.19). The difference might have been due to the use of different equipment and different samples. A future study might be needed to obtain more definitive norm values for TMJS.
CONCLUSIONS
In this study, the condyle-fossa relationship was evaluated in adolescents of various skeletal patterns using CBCT.
There were almost no statistical differences in condyle-fossa relationships according to sex, age, and skeletal patterns except between the left and right sides.
The condyle was positioned more inferiorly in hypodivergent than hyperdivergent Class II patients.
Sagittal AS, SS, and PS were significantly different, but the coronal MS and LS were not significantly different.
In the sagittal view, SS was the greatest and AS was significantly smaller than SS and PS (P < .001), and the mean ratio of AS to SS to PS was 1.00 to 1.27 to 1.19, respectively.
ACKNOWLEDGMENT
This paper was supported by Wonkwang University in 2020.
REFERENCES
- 1.Schudy FF. Vertical growth versus anteroposterior growth as related to function and treatment. Angle Orthod. 1964;34:75–93. [Google Scholar]
- 2.Sassouni V. A classification of skeletal facial types. Am J Orthod. 1969;55:109–123. doi: 10.1016/0002-9416(69)90122-5. [DOI] [PubMed] [Google Scholar]
- 3.Siriwat PP, Jarabak JR. Malocclusion and facial morphology is there a relationship? An epidemiologic study. Angle Orthod. 1985;55:127–138. doi: 10.1043/0003-3219(1985)055<0127:MAFMIT>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 4.Paknahad M, Shahidi S, Abbaszade H. Correlation between condylar position and different sagittal skeletal facial types. J Orofac Orthop. 2016;77:350–356. doi: 10.1007/s00056-016-0039-z. [DOI] [PubMed] [Google Scholar]
- 5.Paknahad M, Shahidi S. Association between condylar position and vertical skeletal craniofacial morphology: a cone beam computed tomography study. Int Orthod. 2017;15:740–751. doi: 10.1016/j.ortho.2017.09.007. [DOI] [PubMed] [Google Scholar]
- 6.Abdel-Fattah RA. Optimum temporomandibular joint (TMJ) condylar position. Todays FDA. 1989;1:1C–3C. [PubMed] [Google Scholar]
- 7.Okur A, Ozkiris M, Kapusuz Z, Karaçavus S, Saydam L. Characteristics of articular fossa and condyle in patients with temporomandibular joint complaint. Eur Rev Med Pharmacol Sci. 2012;16:2131–2135. [PubMed] [Google Scholar]
- 8.Goldstein BH. Temporomandibular disorders: a review of current understanding. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1999;88:379–385. doi: 10.1016/s1079-2104(99)70048-x. [DOI] [PubMed] [Google Scholar]
- 9.Pullinger AG, Hollender L, Solberg WK, Petersson A. A tomographic study of mandibular condyle position in an asymptomatic population. J Prosthet Dent. 1985;53:706–713. doi: 10.1016/0022-3913(85)90029-0. [DOI] [PubMed] [Google Scholar]
- 10.Pullinger AG, Solberg WK, Hollender L, Petersson A. Relationship of mandibular condylar position to dental occlusion factors in an asymptomatic population. Am J Orthod Dentofacial Orthop. 1987;91:200–206. doi: 10.1016/0889-5406(87)90447-1. [DOI] [PubMed] [Google Scholar]
- 11.Seren E, Akan H, Toller MO, Akyar S. An evaluation of the condylar position of the temporomandibular joint by computerized tomography in Class III malocclusions: a preliminary study. Am J Orthod Dentofacial Orthop. 1994;105:483–488. doi: 10.1016/S0889-5406(94)70009-5. [DOI] [PubMed] [Google Scholar]
- 12.Pullinger AG, Solberg WK, Hollender L, Guichet D. Tomographic analysis of mandibular condyle position in diagnostic subgroups of temporomandibular disorders. J Prosthet Dent. 1986;55:723–729. doi: 10.1016/0022-3913(86)90450-6. [DOI] [PubMed] [Google Scholar]
- 13.Cohlmia JT, Ghosh J, Sinha PK, Nanda RS, Currier GF. Tomographic assessment of temporomandibular joints in patients with malocclusion. Angle Orthod. 1996;66:27–35. doi: 10.1043/0003-3219(1996)066<0027:TAOTJI>2.3.CO;2. [DOI] [PubMed] [Google Scholar]
- 14.Vitral RW, Telles Cde S, Fraga MR, de Oliveira RS, Tanaka OM. Computed tomography evaluation of temporomandibular joint alterations in patients with class II division 1 subdivision malocclusions: condyle-fossa relationship. Am J Orthod Dentofacial Orthop. 2004;126:48–52. doi: 10.1016/j.ajodo.2003.06.012. [DOI] [PubMed] [Google Scholar]
- 15.Rodrigues AF, Fraga MR, Vitral RW. Computed tomography evaluation of the temporomandibular joint in Class I malocclusion patients: condylar symmetry and condyle-fossa relationship. Am J Orthod Dentofacial Orthop. 2009;136:192–198. doi: 10.1016/j.ajodo.2007.07.032. [DOI] [PubMed] [Google Scholar]
- 16.Rodrigues AF, Fraga MR, Vitral RW. Computed tomography evaluation of the temporomandibular joint in Class II Division 1 and Class III malocclusion patients: condylar symmetry and condyle-fossa relationship. Am J Orthod Dentofacial Orthop. 2009;136:199–206. doi: 10.1016/j.ajodo.2007.07.033. [DOI] [PubMed] [Google Scholar]
- 17.Vitral RW, da Silva Campos MJ, Rodrigues AF, Fraga MR. Temporomandibular joint and normal occlusion: is there anything singular about it? A computed tomographic evaluation. Am J Orthod Dentofacial Orthop. 2011;140:18–24. doi: 10.1016/j.ajodo.2009.07.030. [DOI] [PubMed] [Google Scholar]
- 18.Kim HO, Lee W, Kook YA, Kim Y. Comparison of the condyle-fossa relationship between skeletal class III malocclusion patients with and without asymmetry: a retrospective 3-dimensional cone-beam computed tomography study. Korean J Orthod. 2013;43:209–217. doi: 10.4041/kjod.2013.43.5.209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Okur A, Ozkiris M, Kapusuz Z, Karaçavus S, Saydam L. Characteristics of articular fossa and condyle in patients with temporomandibular joint complaint. Eur Rev Med Pharmacol Sci. 2012;16:2131–2135. [PubMed] [Google Scholar]
- 20.Manjula WS, Tajir F, Murali RV, Kumar SK, Nizam M. Assessment of optimal condylar position with cone-beam computed tomography in south Indian female population. J Pharm Bioallied Sci. 2015;7(suppl 1):S121–S124. doi: 10.4103/0975-7406.155855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lelis ÉR, Guimarães Henriques JC, Tavares M, de Mendonça MR, Fernandes Neto AJ, Almeida Gde A. Cone-beam tomography assessment of the condylar position in asymptomatic and symptomatic young individuals. J Prosthet Dent. 2015;114:420–425. doi: 10.1016/j.prosdent.2015.04.006. [DOI] [PubMed] [Google Scholar]
- 22.Paknahad M, Shahidi S, Iranpour S, Mirhadi S, Paknahad M. Cone-beam computed tomographic assessment of mandibular condylar position in patients with temporomandibular joint dysfunction and in healthy subjects. Int J Dent. 2015;2015:301796. doi: 10.1155/2015/301796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Cordray FE. Three-dimensional analysis of models articulated in the seated condylar position from a deprogrammed asymptomatic population: a prospective study. Part 1. Am J Orthod Dentofacial Orthop. 2006;129:619–630. doi: 10.1016/j.ajodo.2004.10.015. [DOI] [PubMed] [Google Scholar]
- 24.Galeković NH, Fugošić V, Braut V, Ćelić R. Influence of the hinge axis transfer modality on the three-dimensional condylar shift between the centric relation and the maximum intercuspation positions. Acta Stomatol Croat. 2015;49:36–44. doi: 10.15644/asc49/1/5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Costea CM, Badea ME, Vasilache S, Mesaroş M. Effects of CO-CR discrepancy in daily orthodontic treatment planning. Clujul Med. 2016;89:279–286. doi: 10.15386/cjmed-538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Utt TW, Meyers CE, Jr, Wierzba TF, Hondrum SO. A three-dimensional comparison of condylar position changes between centric relation and centric occlusion using the mandibular position indicator. Am J Orthod Dentofacial Orthop. 1995;107:298–308. doi: 10.1016/s0889-5406(95)70146-x. [DOI] [PubMed] [Google Scholar]
- 27.Katsavrias EG, Halazonetis DJ. Condyle and fossa shape in Class II and Class III skeletal patterns: a morphometric tomographic study. Am J Orthod Dentofacial Orthop. 2005;128:337–346. doi: 10.1016/j.ajodo.2004.05.024. [DOI] [PubMed] [Google Scholar]
- 28.Arieta-Miranda JM, Silva-Valencia M, Flores-Mir C, Paredes-Sampen NA, Arriola-Guillen LE. Spatial analysis of condyle position according to sagittal skeletal relationship, assessed by cone beam computed tomography. Prog Orthod. 2013;14:36. doi: 10.1186/2196-1042-14-36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Arici S, Akan H, Yakubov K, Arici N. Effects of fixed functional appliance treatment on the temporomandibular joint. Am J Orthod Dentofacial Orthop. 2008;133:809–814. doi: 10.1016/j.ajodo.2006.07.035. [DOI] [PubMed] [Google Scholar]
- 30.Du L, Zhao Q, Tian M, Heng C, Cui X, Li Q. Comparative study of the condylar positions in different sagittal skeletal facial types with cone-beam computed tomography. Hua Xi Kou Qiang Yi Xue Za Zhi. 2014;32:382–385. doi: 10.7518/hxkq.2014.04.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Park IY, Kim JH, Park YH. Three-dimensional cone-beam computed tomography based comparison of condylar position and morphology according to the vertical skeletal pattern. Korean J Orthod. 2015;45:66–73. doi: 10.4041/kjod.2015.45.2.66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Čimić S, Žaja M, Kraljević S, Šimunković M, Kopić A. Ćatić. Influence of occlusal interference on the mandibular condylar position. Acta Stomatol Croat. 2016;50:116–121. doi: 10.1564/asc50/2/3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Gu YJ, Lu SN, Gao MQ, Gu XY, Shi H, Ma JQ. Comparison of condylar position between Angle Class I and Class II malocclusion in teenagers. Shanghai Kou Qiang Yi Xue. 2016;25:694–696. [PubMed] [Google Scholar]
- 34.Kimos P, Nebbe B, Heo G, Packota G, Major PW. Changes in temporomandibular joint sagittal disc position over time in adolescents: a longitudinal retrospective study. Am J Orthod Dentofacial Orthop. 2009;136:185–191. doi: 10.1016/j.ajodo.2008.12.016. [DOI] [PubMed] [Google Scholar]
- 35.Dalili Z, Khaki N, Kia SJ, Salamat F. Assessing joint space and condylar position in the people with normal function of temporomandibular joint with cone-beam computed tomography. Dent Res J (Isfahan) 2012;9:607–612. doi: 10.4103/1735-3327.104881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Petrikowski CG, Grace MG. Age and gender differences in temporomandibular joint radiographic findings before orthodontic treatment in adolescents. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1999;87:380–385. doi: 10.1016/s1079-2104(99)70228-3. [DOI] [PubMed] [Google Scholar]
- 37.Barghan S, Tetradis S, Mallya S. Application of cone beam computed tomography for assessment of the temporomandibular joints. Aust Dent J. 2012;57(suppl 1):109–118. doi: 10.1111/j.1834-7819.2011.01663.x. [DOI] [PubMed] [Google Scholar]
- 38.Zhang ZL, Cheng JG, Li G, Zhang JZ, Zhang ZY, Ma XC. Measurement accuracy of temporomandibular joint space in Promax 3-dimensional cone-beam computerized tomography images. Oral Surg Oral Med Oral Pathol Oral Radiol. 2012;114:112–117. doi: 10.1016/j.oooo.2011.11.020. [DOI] [PubMed] [Google Scholar]
- 39.Burke G, Major P, Glover K, Prasad N. Correlations between condylar characteristics and facial morphology in Class II preadolescent patients. Am J Orthod Dentofacial Orthop. 1998;114:328–336. doi: 10.1016/s0889-5406(98)70216-1. [DOI] [PubMed] [Google Scholar]
- 40.Paknahad M, Shahidi S. Association between mandibular condylar position and clinical dysfunction index. J Craniomaxillofac Surg. 2015;43:432–436. doi: 10.1016/j.jcms.2015.01.005. [DOI] [PubMed] [Google Scholar]
- 41.Ikeda K, Kawamura A. Assessment of optimal condylar position with limited cone-beam computed tomography. Am J Orthod Dentofacial Orthop. 2009;135:495–501. doi: 10.1016/j.ajodo.2007.05.021. [DOI] [PubMed] [Google Scholar]