Abstract
Introduction
Organizations and systems that deliver health care may better adapt to rapid change in their environments by acting as learning organizations and learning health systems (LHSs). Despite widespread recognition that multilevel forces shape capacity for learning within care delivery organizations, there is no agreed‐on, comprehensive, multilevel framework to inform LHS research and practice.
Methods
We develop such a framework, which can enhance both research on LHSs and practical steps toward their development. We draw on existing frameworks and research within organization and implementation science and synthesize contributions from three influential frameworks: the Consolidated Framework for Implementation Research, the social‐ecological framework, and the organizational change framework. These frameworks come, respectively, from the fields of implementation science, public health, and organization science.
Results
Our proposed integrative framework includes both intraorganizational levels (individual, team, mid‐management, organization) and the operating and general environments in which delivery organizations operate. We stress the importance of examining interactions among influential factors both within and across system levels and focus on the effects of leadership, incentives, and culture. Additionally, we indicate that organizational learning depends substantially on internal and cross‐level alignment of these factors. We illustrate the contribution of our multilevel perspective by applying it to the analysis of three diverse implementation initiatives that aimed at specific care improvements and enduring system learning.
Conclusions
The framework and perspective developed here can help investigators and practitioners broadly scan and then investigate forces influencing improvement and learning and may point to otherwise unnoticed interactions among influential factors. The framework can also be used as a planning tool by managers and practitioners.
Keywords: implementation science, learning health system, organizational learning
1. INTRODUCTION
Health care organizations in the United States and other industrialized nations face pressures to contain costs, improve quality, reduce health inequalities, and care for an aging population. 1 , 2 , 3 They also must adapt to major changes in payments and budgets; treatments and technologies; and patterns of ownership, organization, and delivery of care. 2 , 4 , 5 , 6 , 7 , 8
A growing group of health care leaders and researchers anticipate that delivery systems can adapt to these challenges by engaging in rapid learning; innovation; exploitation of emerging digital technologies; and development of enhanced capabilities in system redesign and quality improvement. This vision is captured in discussions of the learning health system (LHS) 9 , 10 , 11 , 12 , 13 and learning organizations. 14 , 15 , 16 , 17 , 18 , 19 The National Academy of Medicine (NAM) 1 defines the “Continuously Learning Health Care System” as “one in which science and informatics, patient‐clinician partnerships, incentives, and culture are aligned to promote and enable continuous and real‐time improvement in both the effectiveness and efficiency of care”( 13 , p. 17).
In this article, we seek to strengthen the emerging understanding of organizational and system learning in health care as resulting from interactions among diverse factors, which operate at multiple levels within and beyond individual care delivery organizations. In the view of the NAM and others, 15 , 16 LHS care organizations gain knowledge and improvement capacity as their members scan the environment for knowledge and innovations; select, try, and test them; learn from internal data and experience; and compare their findings with those of other care organizations. In the NAM's formulation, learning systems have the following characteristics:
Real‐time access to evidence; digital capture of the care experience, strong partnerships with patients, families, and other care givers; incentives aligned to promote continuous improvement and provision of high‐value care; full transparency; a leadership‐instilled culture of learning, and supportive processes such as team training and skill building, systems analysis, and feedback for continuous learning and system improvement. (Source 13 , p. 18, table S2)
Like many treatments of learning organizations, the NAM's LHS model characterizes learning in terms of observable, behavioral changes, rather than primarily cognitive ones. 20 This behavioral view defines organizational learning as “the process of improving actions through better knowledge and understanding,” ( 21 , p. 803). The LHS framework can be applied to individual health care organizations, delivery systems, organizational networks, 22 and national and international health systems. 23 In this article, we apply it to care organizations.
Research has examined how organizational learning and improvement are affected by internal organizational factors, such as individual training and learning to improve work while doing it 24 : teamwork, leadership, information technology, knowledge management, and culture. 18 , 25 , 26 , 27 , 28 , 29 , 30 , 31 , 32 , 33 , 34 Studies also identify influences on learning within an organization's operating environment, including collaboration among care organizations 35 ; partnerships with external researchers 36 ; funding for research, innovation, and other activities supporting learning 29 ; and payment for high value care and other forms of care improvement. 25 , 29
2. QUESTIONS OF INTEREST
It is widely recognized that the factors influencing organizational learning in health care and in other industries operate at multiple levels within and outside of care organizations. 28 , 30 , 37 , 38 It is particularly important to examine multiple levels of learning in health care because of the organizational complexity of care organizations and delivery systems and their dependencies on external agencies and conditions. Only a multilevel approach can adequately take account of the occupational diversity and interdependence of the work; interactions within professional hierarchies and between professionals and administrators; and the wide range of external influences and constraints on how work is accomplished. 39 A multilevel perspective thus holds promise for advancing research that will provide actionable knowledge for health care organizations seeking to become learning healthcare systems.
Currently, there is no agreed‐on, comprehensive, multilevel framework for examining factors and processes shaping organization and system learning in health care. To address this limitation, we draw on organization and implementation science to develop a framework that can be used to advance the study of organizational learning in the healthcare sector.
3. METHODS
We first review three helpful multilevel frameworks from related fields. We then synthesize contributions from these frameworks and from research into an integrated framework showing factors influencing learning at different system levels. We illustrate the contribution of the multilevel perspective by applying it to the development of three initiatives that aimed at specific care improvements and enduring system learning. Next, we highlight the influence and dynamics of incentives, culture, and leadership, three fertile areas for research on cross‐level relations among factors affecting learning. We conclude by discussing some research and practice implications of our framework and the underlying multilevel perspective.
4. RESULTS
4.1. Three multilevel frameworks
A variety of studies and frameworks on dissemination, implementation, organizational change, and public health identify system levels at which influential factors operate. 40 , 41 , 42 , 43 , 44 These levels range from the individual and work‐team to the environment of the focal organization or delivery system. Multilevel approaches often include lists of influential factors and acknowledge possible cross‐level relationships among them. Although the frameworks reviewed here were originally developed to address issues other than organizational learning in health care, they can contribute to LHS research.
4.1.1. The Consolidated Framework for Implementation Research
The Consolidated Framework for Implementation Research (CFIR) is one of the most widely cited frameworks in Implementation Science. 40 , 45 It synthesizes findings from empirical studies and from 19 earlier conceptualizations and frameworks on knowledge transfer, implementation of evidence‐based practice, dissemination, and organizational change. The CFIR's research utility is growing, thanks to a community of researchers who are actively developing standard, validated measures for many of its constructs. 46 The CFIR defines constructs for five domains: Intervention Characteristics; the Outer Setting (environment) of the organization in which implementation occurs; the Inner (organizational) Setting; involved Individuals; and the Implementation Process. Within the Inner Setting, the CFIR calls attention to the team, unit, and service levels, along with the organization as a whole.
The CFIR was developed for research on implementation of evidence‐based practices, but its multilevel perspective and many of its constructs have also been applied to research on collective learning and broad improvement programs. For example, The Veterans Health Administration uses the CFIR to guide and evaluate their efforts to become an effective learning health care system. 47 The CFIR facilitates research on learning by including a construct for learning climate, defined as one in which leaders actively seek team members' inputs; team members feel that they are essential partners in the change process and feel psychologically safe to try new methods; and members have enough time and space for reflective thinking and evaluation. Additional contributions of the CFIR include its emphasis on interaction among the five domains and its distinction between formally appointed, internal implementation leaders and informal champions and opinion leaders.
Despite its contributions, there are limitations to applying the CFIR to LHS research and practice. The framework was developed and has mainly been used for studies of implementation of discrete evidence‐based practices, rather than broad organizational changes of the sort required for LHS development. The main constructs within the Outer Setting domain do not include market forces, knowledge, technology, social norms, and values, all of which may impact organizational learning. Nor do the Inner Setting domains cover some important organizational factors delineated by the NAM and other models of organizational learning, 18 , 25 including digital capture of the care experience, partnerships with patients, and supportive processes like systems engineering. The CFIR only cites information technology as an intervention characteristic and as a factor affecting access to knowledge about interventions. Additionally, the framework does not clearly distinguish the roles in change programs played by leaders at each organizational level.
4.1.2. The social‐ecological framework
The social‐ecological perspective, which is widely used in practice and research on health behavior and public health, 44 , 48 , 49 identifies multilevel determinants of health behavior. Based on this perspective, Tabak et al 43 provide a socio‐ecological framework that distinguishes between the levels of the individual, organization (including hospitals, service organizations, and places of employment), community (local government, neighborhood), and system (eg, hospital system and government/policy).
Advantages of extending this framework to LHS research include its explicit assumptions that influential factors interact with one another within and across levels 44 , 49 and that some external “community” factors exercise immediate influences on care practice, while other external factors (at the “system” level) have less immediate and more general effects. Some community factors that affect care, such as the services available in a community and the needs and capacities of its members (eg, for self‐management and interaction with health providers), may also affect organizational learning. 19
Although helpful, the socio‐ecological framework concentrates on programs and factors affecting individual health behavior and hence is less readily adaptable to investigations of learning and LHS operations than the CFIR. Additionally, the promising distinction between the community and system levels does not adequately fit the full range of factors affecting organizational learning. For example, care delivery organizations in a learning collaborative may directly influence one another's learning. However, these organizations are not necessarily located in the immediate, surrounding “community.”
Instead of trying to fit the socio‐ecological terminology to learning, it seems more helpful to follow the organizational literature, which distinguishes conditions that directly impact operations (sometimes called the “task” or “close” environment 50 ) from a set of “general” environmental conditions, that have less immediate effects. The immediate, operating environment includes interorganizational cooperation and competition, regulations, and sources of payment and revenue. The more distant, general environment incudes scientific and technological developments, socio‐economic, and political conditions.
4.1.3. Organizational change framework
Adding a third framework, 51 which is derived from research on organizational change in health care, can help overcome some of the gaps that emerge when we try to apply the previous two frameworks to organizational and system‐wide learning in health care. Ferlie and Shortell originally applied their framework to initiatives to improve care quality across entire care organizations or delivery systems. The authors identify four main levels affecting such major organizational changes: the individual, group or team, overall organization, and larger system or environment. The system/environment level includes the political economy and markets for health care, along with institutional forces, such as regulatory and payment bodies and shared information about organizational practices and performance. At each level, “core properties” of leadership, culture, team development, and information technology influence organizational change and are influenced by it. When these properties are aligned and supportive of organization‐level learning and improvement, they closely resemble the LHS characteristics articulated by the NAM 13 and others. Similarly, the core properties of this model capture features of many of the intraorganizational “building blocks” for organizational learning identified in the research‐based model of learning developed by Singer et al. 18
The organizational change framework contains important implications for research on organization‐level learning. Individual learning must be communicated and managed for it to contribute to learning by other staff members, teams, or the entire organization. Similarly, teams can provide input into higher level learning when they implement evidence‐based practices 52 or engage in quality improvement. 37 Organization‐level learning synthesizes learning at these lower levels and applies the resulting knowledge to achieving strategic priorities and organizational goals.
Another contribution of the organizational change framework is its focus on effects of the extra‐organizational environment, including external incentives and other organizations. The authors' distinction between competitive and cooperative interorganizational relations contains important implications for learning. Competition may discourage innovative organizations from sharing knowledge and beneficial practices with one another. A further contribution of this framework is its recognition that entire organizations undergo changes, as well as serving as contexts for internal learning and for targeted implementation and improvement. Just as planned change can shape LHS capacities, so may unintended organizational changes, such as those flowing from leadership transitions, internal power struggles, external mandates, adaptation to external developments, and environmental selection. 53
The organizational change framework underlines the importance of information technology, which plays a major role in the NAM model 13 and in many other recent treatments of organizational and system learning. 12 , 23 Information technology creates new opportunities for rapidly gathering and synthesizing knowledge, assessing current performance, and providing feedback to managers and practitioners about effects of their actions.
The framework's distinction between leadership and culture contrasts with the NAM concept of “leadership instilled culture” ( 13 , p. 18). Separating culture from leadership helps remind researchers to examine a broad range of factors besides leadership that may shape learning culture. Moreover, treating culture as a focal area for investigation may encourage assessment of ways that learning is affected by internal differentiation and fragmentation in beliefs, assumptions, and work routines. 54 , 55 The organizational change framework's focus on alignment among influential factors also contributes to understanding effects of external forces on organizational learning. For instance, payment incentives for care value, rather than for volume, 56 may reinforce efforts of delivery organizations to learn how to deliver patient‐centered care and work with community services to promote population health. External incentives and policies will be more likely to foster organizational learning if they align with the care organizations' own strategies and goals for improving care.
Despite its utility, the organizational change framework also has limitations. One is insufficient attention to the impact of immediate operating conditions, as opposed to effects of broader forces in the political economy. Moreover, like the other two frameworks, the organizational change framework does not formally distinguish the roles of mid‐level management from those of executives and team leaders. Yet, middle managers often play critical roles in organizational learning 28 , 57 and change. 58 , 59
4.2. Multilevel framework of factors influencing organizational learning
Figure 1 presents an integrative framework showing factors at multiple system levels that affect organizational learning. The framework incorporates many of the levels and factors identified in the above three frameworks and in research on organizational learning in health care (Figure 1, insert). Table 1 shows how the multilevel framework builds on and differs from the preceding frameworks (Table 1). The table lists some of the most relevant factors within the CFIR (“constructs) and the organizational change framework (“properties”). For brevity, the table omits relevant psychosocial factors in the socio‐ecological framework.
FIGURE 1.
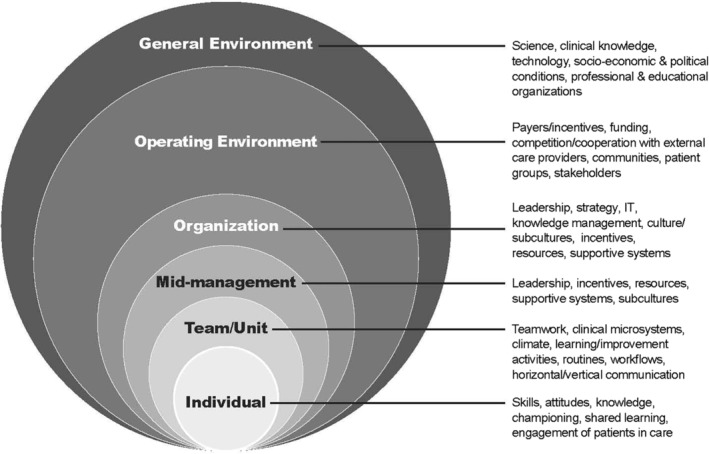
Factors influencing organizational learning
TABLE 1.
Constructing the multilevel framework
| Frameworks and relevant domains a | ||||
|---|---|---|---|---|
| Multilevel framework | CFIR | Socio‐ecological | Organizational change | Rationale for including level and/or domains in multilevel framework |
| General environment | Outer Setting (external policies and incentives; patient needs/resources) | System | Environment (political economy, markets, institutional forces) | Examine influences of slower‐to‐change, more distant environmental conditions (eg, policies, institutional norms, patient expectations). |
| Operating environment | Outer Setting (links to other organizations; peer pressure for implementation) | Community | Environment (incentives, relations to other organizations) | Distinguish immediate, more dynamic influences (eg, payment incentives, competitors, cooperating and allied organizations). |
| Organization | Inner Setting—service, unit, team levels. (structural characteristics, culture; learning climate; leadership engagement; resources; knowledge/information) | Organization | Overall organization (core properties: leadership, culture, team development, information technology) | Adopt widely used term; focus on total organization; emphasize alignment among core properties likely to have major effects on learning; distinguish leadership from culture. |
| Mid‐management | Not distinguished as separate level. Implementation Processes (planning, engaging; executing; reflecting and evaluating; actions of formal implementation leaders) | Not distinguished as level | Not included as separate level. (Core properties apply. | Focus on shared learning processes (vs change implementation); highlight strong influence of mid‐level managers. |
| Team/u | Inner Setting (variation across teams); (Implementation) Process (opinion leaders, formal leaders; champions, reflecting and evaluating) | Not included | Group/team (core properties) | Note how team processes affect organizational, as well as individual learning. |
| Individual | Involved Individuals (attributes; knowledge and beliefs about intervention; identification with organization; behavior) | Individual | Individual skills, motivation, behavior (eg, teamwork, technology use) | Indicate that individual learning may contribute to group learning; individuals can act as champions of organizational learning, engage patients in process/results of organizational learning. |
Abbreviation: CFIR, Consolidated Framework for Implementation Research.
CFIR domains are capitalized. CFIR constructs and organization change framework properties are in parentheses.
The multilevel framework, like its predecessors, anticipates interactions among influential factors within and across levels. Moreover, this new framework specially emphasizes impacts of alignment or misalignment among these factors. For example, the framework could lead researchers to ask whether influential factors, such as external and intraorganizational incentives, complement one another in encouraging LHS practices, or work at cross purposes. Similarly, the framework suggests that leaders seeking to foster learning systems consider whether their performance assessment and reward processes lead staff just to try to meet narrow performance standards or encourage questioning current practices, which can contribute to fundamental learning. 60
The general environment in Figure 1 and Table 1 includes actors and conditions which may indirectly influence learning, including private and public decision makers and their policies and regulations; developers of scientific, clinical, and technical knowledge and innovations; social, economic, and political conditions; and activities of professional and educational organizations. The operating environment includes actors and conditions that can immediately and directly affect an organization's internal operations, including learning. Members of the operating environment include payers, external care providers, patients and community groups, suppliers, consulting organizations, entities directly overseeing care (eg, boards), and competitors. The organizational level includes a focal organization's goals, strategies, resources, and operational support for learning and care improvement; knowledge management and information technology capacities; culture; and performance assessment and reward system. In keeping with the importance of mid‐level leaders in system learning, Figure 1 includes a mid‐management level, which is not formally represented in the three frameworks just reviewed. The team/unit level draws attention to the many subgroups within health care organizations that may engage in group learning, such as those in nursing units, support departments, and primary care teams. The Individual level captures capacities and behavior of care providers and other staff that may affect shared learning.
The nesting of lower levels within higher ones in Figure 1 portrays the assumption that organizational learning like that envisioned in the NAM's LHS model 13 will be more likely when characteristics fostering learning, such as supportive leadership, operate across multiple levels and align with one another. As suggested by the NAM, to ensure organizational learning based on scientific knowledge, care delivery organizations must develop their own internal mechanisms for gathering, managing, and implementing this external knowledge. Additionally, they need to develop technologies and processes that capture and use internal care experience to generate clinical knowledge. If, as advocated by the NAM, care delivery organizations are to learn from and with engaged patients, these organizations need to develop ties to the communities and patient groups they serve. The organizations will also benefit from developing clinical microsystems that place individual patients at the center of the care process and ensure shared decision‐making about care. 19 , 52 Furthermore, care delivery organizations will need to develop processes for translating learning from patients into internal knowledge and guidance for care givers. Additional factors, some of which are discussed later, must also be aligned across levels.
4.3. Multilevel analysis of learning
The value of this multilevel perspective on care organization learning can be illustrated by applying it to three, documented, improvement initiatives. The first of these began as a quality‐improvement intervention to help hospital intensive care units (ICUs) adhere to evidence‐based procedures for reducing catheter‐related infections. 61 As the researchers observed the implementation process, they recognized the importance of factors beyond the boundaries of the participating ICUs, particularly organization‐level support from senior hospital managers for unit‐level implementation efforts. The research team gradually broadened their goals to encompass reshaping safety culture at the organization and mid‐management levels. They also developed hospital improvement collaboratives, thereby adding forces from the hospitals' operating environments to the repertoire of implementation strategies. These changes in program targets, goals, and implementation strategies reflected the researchers' developing, multilevel view of hospital learning to reduce preventable health‐acquired harms. 62 , 63 The researchers further extended their multilevel perspective in their “post hoc” examination of a successful, statewide infection‐control improvement collaborative in Michigan. 62 They concluded that evidence‐based changes in team‐level practices were enhanced by peer pressure on infection control specialists from colleagues in other hospitals and by the examples that hospitals in the collaborative set for one another. These normative pressures, which originated in the hospitals' operating environment, encouraged hospital staff to share their performance data with other hospitals across the state and to strive to achieve the collaborative's agreed‐upon safety targets. 62
The second initiative aimed to help four Australian hospitals adopt an ambitious quality program. 64 The program, which embodied many principles of LHSs, sought to embed achievement of high quality care into leadership goals, operations, and hospital culture. During a 3‐year trial, one implementation hospital dropped out, while implementation in the other targeted hospitals proceeded more slowly and with less consistency than anticipated. Improvement in the implementing hospitals only occurred on one of eight quality metrics. 65
The authors did not provide a multilevel analysis of their findings, but adopting this approach helped us identify and classify the main forces limiting the program's success. The most influential forces in the hospitals' operating environment were strict state standards for safety training and for reporting on clinical quality and safety. Hospital quality managers concentrated on compliance with these standards, thereby diverting their time and attention from the hospital quality improvement initiative. 66 Shifts in other influential government policies diverted attention from the quality program, as did an accreditation review in one hospital. At the organization level, the hospitals' senior and mid‐level leaders reported additional challenges and priorities, which distracted them from dedication to the quality program. Furthermore, senior hospital leaders' concentration on compliance with state and federal regulations led them to underestimate the time and resources needed to plan and mobilize support for fundamental change in staff attitudes and behavior. At the unit and individual levels, clinicians reported insufficient support from immediate and higher level managers for far‐reaching behavioral and cultural change. A cross‐level interaction also created an implementation barrier: there was limited alignment between front‐line staff and managers about how to assure quality.
The third initiative involved development of a rheumatoid arthritis registry in Sweden, which was reported in a 15‐year retrospective study. 31 As envisioned in the LHS model, care delivery organizations adopted new information technologies that became available in their general and operating environments. These technologies gradually supported use of the registry for clinical learning about medication effects. Within the delivery organizations, health information technology also enabled patient‐centered care—a learning system value. This approach to care benefitted from development of computerized procedures for patient entry of symptoms before visits; rapid calculation of a health status score; longitudinal plotting of symptoms and past treatments; and use of the data by individual practitioners and their patients in shared decision‐making about treatment options.
To provide a full multilevel account of the registry's contribution to system learning, it is necessary to locate the registry's development within the broader context of Sweden's electronic health records system. 67 The registry's progress and learning contributions were substantially aided by alignment of supportive forces at the level of the nation, the regions (represented by County Councils), care organizations (hospitals and affiliated clinics), physicians, and patients. Sweden's Ministry of Health and Federation of County Councils created institutional foundations for collaborative information exchange across hospitals and physicians and paid for registry development and maintenance. Data collection and aggregation were aided by a national patient identifier and emerging foundations for national, interoperable data exchange. Individual hospitals shared data and bore data entry costs. Physicians specified data elements during the registry's development; recognized the contribution of registry data to clinical treatment; and demonstrated receptiveness to shared decision‐making. Patients, in turn, seem to have valued the richer and more consultative communication with their physicians, which was made possible by the electronic registry. Had physicians or patients approached registry use with different values and attitudes, the foundation for shared decision‐making might have been weaker. Had the registry lacked strong institutional support at the regional and national level, its developers would have had to follow a very different course. For example, in the United States, care systems and developers of new health information technologies face a more fragmented technical, financial, and regulatory environment. As a result, multiple, competing arthritis registries have emerged, each drawing on diverse sources of support and development, including professional associations, governmental and private funding agencies, industry, and hospitals. 68
In summary, these three cases illustrate the analytic and practical value of applying a multilevel perspective to organizational learning. The infection control researchers gradually developed this type of perspective on their initiative and uncovered previously unreported ways in which professional peers and norms outside the hospitals affected internal learning at the team and organization levels. The papers that provided the basis for the other two examples did not apply a multilevel approach. Our reexamination of the findings in those papers points to the benefits of doing so. Multilevel framing can direct attention to potentially generalizable influences on system learning, such as the overemphasis in the Australian hospital quality initiative on meeting strict external standards for training and reporting. 65 The reanalysis further suggests that system learning depends substantially on supportive interactions and alignments of influential factors within and across system levels.
4.4. Relations within and across levels
As these case studies suggest, to add precision to multilevel analysis, investigators should examine cross‐level relations among influential factors. Here we consider potential relations in three areas that organizational and implementation researchers have found to be particularly important for shared learning and improvement. Table 2 suggests research questions for each area. (Table 2). Similar questions could be developed for other types of influential factors.
TABLE 2.
Research questions on leadership, incentives, and culture
| Thematic area | Research questions |
|---|---|
| Incentives |
|
| Culture |
|
| Leadership |
|
4.4.1. Incentives
External performance incentives in a delivery system's operating environment and their alignment with intraorganizational incentives, structures, and processes can substantially affect whether and how delivery systems learn to improve care quality and efficiency. For example, the growing wave of value‐based payment initiatives 7 , 8 , 69 may encourage learning about care redesign. However, the potential and documented effects of these initiatives on organizational performance are not well established, 56 and their effects on other forms of individual and organizational behavior are widely debated. Appropriate incentives may foster system learning by supporting activities such as research, professional education, care coordination, and provision of high value care. 29 However, some analysts doubt whether current payment programs will foster better care outcomes or only produce undesired and unintended consequences, such as neglect of unmeasured or unrewarded practices; reduced intrinsic motivation 70 ; and short cutting or cheating. 69 Performance incentives may also reduce learning opportunities by discouraging collaboration within or between organizations 69 and intensifying attention to short‐term results, thereby discouraging experimentation, innovation, and systematic evaluation of improvement programs. 71 To investigate alignment among incentives and their impact on learning, researchers can pose questions like those in Table 2. For instance, they might investigate how external incentives are translated into internal sanctions and rewards and how these internal arrangements, in turn, affect individual, team, and organization‐level learning.
4.4.2. Culture
Cultural influences on LHS processes and outcomes occur both within and outside of delivery organizations and systems. Gradual shifts in societal norms, values, and beliefs can create pressures and opportunities for delivery organizations to undertake learning and develop characteristics supporting learning. For example, growing recognition of the social determinants of health has led payers and delivery systems to seek ways to foster population health. 72 , 73 As they move in this direction, care providers and their leaders must engage in fundamental forms of organizational learning 60 —rethinking basic assumptions about their goals and modes of operation. Similarly, increasing expectations for transparency and public disclosure in healthcare encourage care delivery organizations to develop more outward facing organizational cultures. 74 These cultures may encourage interorganizational collaboration and learning, rather than primarily seeking to satisfy internal stakeholders, such as boards and their professional leaders.
Many discussions of culture's intraorganizational influences on learning adopt a holistic, organization‐wide approach that concentrates on shared values, norms, beliefs, and assumptions that support learning and overcome learning barriers. For example, development of a culture of teamwork and standardized care promotes shared learning, 29 as does the establishment of a culture promoting openness to new ideas, appreciation of differences, and psychological safety, which fosters transparency and sharing of insights and concerns. 18 , 75 , 76 The holistic approach thus suggests research questions such as whether prevailing norms, values, and beliefs support or undermine share learning (see Table 2).
Besides examining effects of shared culture, analysts may gain insight by investigating divergence among cultural elements within care delivery systems or organizations. 54 There may be cultural differences among organizations within a delivery system, along with differences within a particular organization across ranks, occupations (nurses vs physicians), divisions (eg, inpatient vs outpatient), clinical specialties, and operating units. Senior leaders, for example, may hold different beliefs about the value of experimentation and innovation than do department heads or front line staff.
Finally, investigators should closely examine implicit assumptions and behavior in practice. These can be distinguished from an organization's cultural symbols (eg, official slogans buzzwords and reward ceremonies) and its espoused norms and values (eg, vision statements). 77 To explore culture in practice and effects of cultural divergence, researchers can pose questions like those shown in Table 2. For example, what implicit assumptions and norms about learning are expressed in leaders' behavior? How is learning affected by subcultural differences and prevailing ways of dealing with these differences?
4.4.3. Leadership
Leaders help bridge between the organization and its general and operating environments. 30 , 39 In doing so, they can guide and support internal system learning. 13 , 18 , 29 The multilevel framework encourages analysts to consider how governing boards and executives in care systems interpret and act on powerful forces in their general environment, such as the growing emphasis on wellness and the availability of personal digital technology. Similarly, it is important to examine how these leaders view and respond to key influences in the operating environment, such as consolidation among care delivery organizations. Then investigators can analyze how formulations of the system's vision, mission, and strategies may impact learning. 13 , 14 , 25 , 77 Within organizations, leaders at several organizational levels play a role in learning, as they put strategies into practice and influence implementation of new care practices 78 and quality improvement. 37 Leaders may synthesize and diffuse information and knowledge; help set mutually shared goals; establish and mediate strategic priorities; provide resources and training; empower front line staff by providing learning opportunities, listening to their inputs, and providing feedback; integrate stakeholders; champion and support innovation; and address external environmental challenges and opportunities. 18 , 59 , 79 , 80 , 81 Hence, as suggested in Table 2, it is important for researchers to examine the practices and values that leaders at all levels attend to, reward, and support. Then researchers can assess the degree to which leaders' actions foster learning, align with one another, and align with other influential factors, such as incentives. Researchers may discern a wide range of processes through which mid‐level managers mediate senior leadership change strategies and sometimes fundamentally alter them. 80 For example, the study of the Australian hospital quality program 65 found that quality managers and other mid‐level managers reinterpreted program objectives articulated by hospital executives and by the state government. By doing so, they undermined opportunities to develop a culture of quality.
5. DISCUSSION
The multilevel perspective developed here and the framework in Figure 1 can serve as a guide for researchers as they examine learning within complex health care organizations; its diffusion throughout organizations; and its role in helping organizations achieve their immediate goals and meet long‐term challenges posed by external change. Wide variations in care quality and substantial waste in delivery of health care services, 82 suggest the limits of relying on “one‐off,” first‐order solutions to pressing problems 75 and underline the need for deep learning. Deep learning addresses the root causes of problems and questions underlying assumptions. 60 It requires alignment and collaboration across multiple levels of organization and complex multilevel thinking.
The framework in Figure 1 may help investigators and practitioners broadly scan forces influencing improvement and learning and may point to otherwise unnoticed interactions among influential factors. Key factors and relations among them can be assessed for likely impact, theoretical importance, and amenability to change. After preliminary consideration of influential levels and key elements within them, researchers can select a subset of levels and factors for systematic data gathering and rigorous analysis. The multilevel framework can also be applied to the reporting of research findings. By specifying the levels, factors, and relations investigated in their studies, researchers can contribute to development of empirically grounded hypotheses for further testing and can facilitate synthesis of findings across studies.
Managers and practitioners may use the framework as a planning tool. For each level, they can consider requisite resources, incentives, training, skill mix, team structure, and time allocations that may be needed to promote and support learning. They can assess the cost and availability of these factors, how well they support one another, and how best to align them across organizational levels.
The NAM and other advocates of LHSs and learning organizations have articulated a set of complex and ambitious targets for transforming care delivery organizations and entire delivery systems. Research is needed that reveals the most critical paths toward developing and supporting the kind of learning envisioned by the LHS model. To that end, it would be valuable for researchers to unpack the complex multilevel, interactions of factors influencing learning within entire organizations and delivery systems.
CONFLICT OF INTEREST
The authors affirm that they have no conflicts of interest associated with this article.
ACKNOWLEDGMENTS
The following individuals provided helpful comments on earlier versions of this paper: Arlene Bierman, Sarah Birken, Cindy Brach, Alaina Fournier, Michael Furukawa, and Hector Rodriguez. Thanks also to: Cathy Baldwin and Erica Breslau for sharing their working paper and allowing us to report on some as yet unpublished findings; Caryn McManus for help in conducting literature searches; and Elise Berliner for information about arthritis registries in the United States. The views expressed in this paper are the authors and do not represent those of any U.S. government agency or any institution with which the authors are affiliated.
Endnote
In 2015, the Institute of Medicine was renamed the National Academy of Medicine. We use the new name throughout this paper, even though the Institute of Medicine's foundational LHS reports appeared before the name change.
REFERENCES
- 1. Cylus J, Roubal T, Ong P, Barber S. Sustainable Health Financing with an Ageing Population. Copenhagen, Denmark: World Health Organization European Office; 2019. http://www.euro.who.int/en/about-us/partners/observatory/activities/research-studies-and-projects/economics-of-healthy-and-active-ageing/sustainable-health-financing-with-an-ageing-population-will-population-ageing-lead-to-uncontrolled-health-expenditure-growth-2019 Accessed September 13, 2019. [Google Scholar]
- 2. Alderwick H, Dixon J. The NHS long term plan. BMJ. 2019;364:184. 10.1136/bmj.l84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Helderman JK. The crisis as catalyst for reframing health care policies in the European Union. Health Econ Policy Law. 2015;10(1):45‐59. 10.1017/S1744133114000231. [DOI] [PubMed] [Google Scholar]
- 4. Cutler DM, Scott MF. Hospitals, market share, and consolidation. JAMA. 2013;310(18):1964‐1970. 10.1001/jama.2013.281675. [DOI] [PubMed] [Google Scholar]
- 5. Doran T, Kontopantelis E, Valderas JM, et al. Effect of financial incentives on incentivised and non‐incentivised clinical activities: longitudinal analysis of data from the UK quality and outcomes framework. BMJ. 2011;342:d3590. 10.1136/bmj.d3590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Schmidt H, Stock S, Doran T. Moving forward with wellness incentives under the affordable care act: lessons from Germany. Issue Brief (Commonw Fund). 2012;13:1‐12. https://www.ncbi.nlm.nih.gov/pubmed/22666898. [PubMed] [Google Scholar]
- 7. Muhlestein D, Saunders RS, Richards R, McClellan MB. Recent progress in the value journey: growth of ACOs and value‐based payment models in 2018. Health Affairs Blog. 2018. 10.1377/hblog20180810.481968. [DOI] [Google Scholar]
- 8. Counte MA, Howard SW, Chang L, Aaronson W. Global advances in value‐based payment and their implications for global health management education, development, and practice. Front Public Health. 2018;6:379. 10.3389/fpubh.2018.00379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. National Academy of Medicine . The Learning Health System Series. Washington, DC: National Academies Press; 2018. https://nam.edu/programs/value-science-driven-health-care/learning-health-system-series. Accessed September 12, 2019. [Google Scholar]
- 10.Learning Healthcare Project Institute of Health and Society, Newcastle University; 2019. Available from: http://www.learninghealthcareproject.org/index.php. Accessed September 9, 2019
- 11. Swiss Learning Health Systems : Department of Health Sciences and Health Policy, University of Lucerne; 2018. http://www.slhs.ch/en/. Accessed September 11, 2019
- 12. Ovretveit J, Bjork C. Sweden: the learning health system. In: Braithwaite J, Mannion R, Matsuyama Y, Shekelle PG, Whittaker S, Al‐Adawi S, eds. Healthcare Systems: Future Predictions for Global Care. Boca Raton, FL: CRC Press; 2018:243‐247. [Google Scholar]
- 13. Institute of Medicine (IOM) . Best Care at Lower Cost: the Path to Continuously Learning Health Care in America. Washington, DC: Institute of Medicine; 2013. [PubMed] [Google Scholar]
- 14. Schilling L, Dearing JW, Staley P, Harvey P, Fahey L, Kuruppu F. Kaiser Permanente's performance improvement system, part 4: creating a learning organization. Jt Comm J Qual Patient Saf. 2011;37(12):532‐543. https://www.ncbi.nlm.nih.gov/pubmed/22235538. [DOI] [PubMed] [Google Scholar]
- 15. Garvin D, Edmondson AC, Gino F. Is yours a learning organization? Harv Bus Rev. 2008;86:109‐116. [PubMed] [Google Scholar]
- 16. Senge PM. The Fifth Discipline: the Art and Practice of the Learning Organization. New York, NY: Random House; 1990. [Google Scholar]
- 17. Akhnif E, Macq J, Idrissi Fakhreddine MO, Meessen B. Scoping literature review on the learning organisation concept as applied to the health system. Health Res Policy Syst. 2017;15(1):16. 10.1186/s12961-017-0176-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Singer SJ, Moore SC, Meterko M, Williams S. Development of a short‐form learning organization survey: the LOS‐27. Med Care Res Rev. 2012;69(4):432‐459. 10.1177/1077558712448135. [DOI] [PubMed] [Google Scholar]
- 19. Montori VM, Hargraves I, McNellis RJ, et al. The care and learn model: a practice and research model for improving healthcare quality and outcomes. J Gen Intern Med. 2018;34: 154‐158. 10.1007/s11606-018-4737-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Tsang EWK. Organizational learning and the learning organization: a dichotomy between descriptive and prescriptive research. Hum Relat. 2000;50:73‐89. [Google Scholar]
- 21. Fiol CM, Lyles MA. Organizational learning. Acad Manage Rev. 1985;10(4):803‐814. [Google Scholar]
- 22. Forrest CB, Margolis PA, Seid M, Colletti RB. PEDSnet: how a prototype pediatric learning health system is being expanded into a national network. Health Aff. 2014;33:1171‐1177. 10.1377/hlthaff.2014.0127. [DOI] [PubMed] [Google Scholar]
- 23. Friedman C, Rubin J, Brown J, et al. Toward a science of learning systems: a research agenda for the high‐functioning Learning health system. J Am Med Inform Assoc. 2015;22(1):43‐50. 10.1136/amiajnl-2014-002977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Nembhard IM, Tucker AL. Applying organizational learning research to accountable care organizations. Med Care Res Rev. 2016;73(6):673‐684. 10.1177/1077558716640415. [DOI] [PubMed] [Google Scholar]
- 25. Singer SJ, Benzer J, Hamdan SU. Improving health care quality and safety: the role of collective learning. J Healthc Leadersh. 2015;7:91‐107. 10.2147/JHL.S70115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Lapre MA, Nembhard IM. Inside the organizational learning curve: understanding the organizational learning process. Found Trends Technol Inform Operat Manage. 2010;4(1):1‐103. 10.1561/0200000023. [DOI] [Google Scholar]
- 27. Oliver BJ, Nelson EC, Kerrigan CL. Turning feed‐forward and feedback processes on patient‐reported data into intelligent action and informed decision‐making: case studies and principles. Med Care. 2019;57 suppl 5:S31‐S7 doi: 10.1097/MLR.0000000000001088 [DOI] [PubMed] [Google Scholar]
- 28. Berson Y, Nemanich LA, Waldman D, Galvin BM, Keller RT. Leadership and organizational learning: a multiple levels perspective. Leadersh Quart. 2006;17(6):577‐594. [Google Scholar]
- 29. Morain SR, Kass NE, Grossmann C. What allows a health care system to become a learning health care system: results from interviews with health system leaders. Learn Health Syst. 2017;1(1):e10015. 10.1002/lrh2.10015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Vera D, Crossan M. Strategic leadership and organizational learning. Acad Manage Rev. 2004;29:222‐240. [Google Scholar]
- 31. Ovretveit J, Keller C, Hvitfeldt Forsberg H, Essen A, Lindblad S, Brommels M. Continuous innovation: developing and using a clinical database with new technology for patient‐centred care—the case of the Swedish quality register for arthritis. Int J Qual Health Care. 2013;25(2):118‐124. 10.1093/intqhc/mzt002. [DOI] [PubMed] [Google Scholar]
- 32. Liberati EG, Ruggiero F, Galuppo L, et al. What hinders the uptake of computerized decision support systems in hospitals? A qualitative study and framework for implementation. Implement Sci. 2017;12(1):113. 10.1186/s13012-017-0644-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Britto MT, Fuller SC, Kaplan HC, et al. Using a network organisational architecture to support the development of Learning healthcare systems. BMJ Qual Saf. 2018;27:937‐946. 10.1136/bmjqs-2017-007219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Sibbald SL, Wathen CN, Kothari A. An empirically based model for knowledge management in health care organizations. Health Care Manage Rev. 2016;41(1):64‐74. 10.1097/HMR.0000000000000046. [DOI] [PubMed] [Google Scholar]
- 35. Leroy L, Rittner JL, Johnson KE, Gerteis J, Miller T. Facilitative components of collaborative learning: a review of nine health research networks. Healthc Policy. 2017;12(3):19‐33. https://www.ncbi.nlm.nih.gov/pubmed/28277202. [PMC free article] [PubMed] [Google Scholar]
- 36. Kislov R, Wilson PM, Knowles S, Boaden R. Learning from the emergence of NIHR collaborations for leadership in applied Health Research and care (CLAHRCs): a systematic review of evaluations. Implement Sci. 2018;13(1):111. 10.1186/s13012-018-0805-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Kaplan HC, Provost LP, Froehle CM, Margolis PA. The model for understanding success in quality (MUSIQ): building a theory of context in healthcare quality improvement. BMJ Qual Saf. 2011;21:13‐20. 10.1136/bmjqs-2011-000010. [DOI] [PubMed] [Google Scholar]
- 38. Antonacopoulou EP. The relationship between individual and organizational learning: new evidence from managerial learning practices. Manage Learn. 2006;37(4):45‐473. [Google Scholar]
- 39. Burns L, Bradley E, Weiner B. Shortell and Kaluzny's Health Care Management: Organization Design and Behavior. 6th ed. Delmar: Clifton Park, NY; 2012. [Google Scholar]
- 40. Damschroder LJ, Aron DC, Keith RE, Kirsh SR, Alexander JA, Lowery JC. Fostering implementation of health services research findings into practice: a consolidated framework for advancing implementation science. Implement Sci. 2009;4:50 http://www.implementationscience.com/content/4/1/50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Flottorp SA, Oxman AD, Krause J, et al. A checklist for identifying determinants of practice: a systematic review and synthesis of frameworks and taxonomies of factors that prevent or enable improvements in healthcare professional practice. Implement Sci. 2013;8:35. 10.1186/1748-5908-8-35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Poole MD, Van de Ven AH, eds. Handbook of Organizational Change and Innovation. New York, NY: Oxford University Press; 2004. [Google Scholar]
- 43. Tabak RG, Khoong EC, Chambers DA, Brownson RC. Bridging research and practice: models for dissemination and implementation research. Am J Prev Med. 2012;43(3):337‐350. 10.1016/j.amepre.2012.05.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Green L, Kreuter M. Health Program Planning: an Educational and Ecological Approach. 4th ed. New York, NY: McGraw Hill; 2005. [Google Scholar]
- 45. Kirk MA, Kelley C, Yankey N, Birken SA, Abadie B, Damschroder L. A systematic review of the use of the consolidated framework for implementation research. Implement Sci. 2016;11(1):72. 10.1186/s13012-016-0437-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. SIRC . The SIRC Instrument Review Project (IRP): Society for Implementation Research Colaboration (SIRC); 2019. https://societyforimplementationresearchcollaboration.org/sirc-instrument-project/. Accessed September 9, 2019
- 47. Jackson GL, Cutrona SL, Vega RJ, Bhatanagar S, Damschroder LJ. New initiative seeks to understand factors that influence innovation. Summer. 2018;4‐5. https://www.hsrd.research.va.gov/publications/forum/summer18/. [Google Scholar]
- 48. Sorensen G, Emmons K, Hunt MK, et al. Model for incorporating social context in health behavior interventions: applications for cancer prevention for working‐class, multiethnic populations. Prev Med. 2003;37(3):188‐197. https://www.ncbi.nlm.nih.gov/pubmed/12914824. [DOI] [PubMed] [Google Scholar]
- 49. Weiner BJ, Lewis MA, Clauser SB, Stitzenberg KB. In search of synergy: strategies for combining interventions at multiple levels. J Natl Cancer Inst Monogr. 2012;2012(44):34‐41. 10.1093/jncimonographs/lgs001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Dess GG, Beard DW. Dimensions of organizational task environments. Administr Sci Quart. 1984;29(1):52‐73. [Google Scholar]
- 51. Ferlie EB, Shortell SM. Improving the quality of health care in the United Kingdom and the United States: a framework for change. Milbank Q. 2001;79(2):281‐315. http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=11439467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Nelson EC, Batalden P, Godfrey M, Laza JS. Value by Design: Developing Clincial Microsystems to Achieve Organizational Excellence. San Francisco, CA: Jossey Bass; 2011. [Google Scholar]
- 53. Van de Ven AH, Poole MS. Explaining development and change in organizations. Acad Manage Rev. 1995;20:510‐540. [Google Scholar]
- 54. Martin J. Organizational Culture:Mapping the Terrain. Thousand Oaks: Sage; 2002. [Google Scholar]
- 55. Wiig S, Aase K, von Plessen C, et al. Talking about quality: exploring how 'quality’ is conceptualized in European hospitals and healthcare systems. BMC Health Serv Res. 2014;14:478. 10.1186/1472-6963-14-478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Scott A, Liu M, Yong J. Financial incentives to encourage value‐based health care. Med Care Res Rev. 2016;75(1):3‐32. 10.1177/1077558716676594. [DOI] [PubMed] [Google Scholar]
- 57. Crossan M, Lane HW, White RE. An organizational learning framework: from intuition to institution. Acad Manage Rev. 2009;24:522‐537. [Google Scholar]
- 58. Gutberg J, Berta W. Understanding middle managers' influence in implementing patient safety culture. BMC Health Serv Res. 2017;17(1):582. 10.1186/s12913-017-2533-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Kerrissey M, Satterstrom P, Leydon N, Schiff G, Singer S. Integrating: a managerial practice that enables implementation in fragmented health care environments. Health Care Manage Rev. 2017;42(3):213‐225. 10.1097/HMR.0000000000000114. [DOI] [PubMed] [Google Scholar]
- 60. Argyris C, Schon D. Organizational Learning II: Theory, Method, and Practice. Reading, MA: Addison‐Wesley; 1996. [Google Scholar]
- 61. Berenholtz SM, Pronovost PJ, Lipsett PA, et al. Eliminating catheter‐related bloodstream infections in the intensive care unit. Crit Care Med. 2004;32(10):2014‐2020. https://www.ncbi.nlm.nih.gov/pubmed/15483409. [DOI] [PubMed] [Google Scholar]
- 62. Dixon‐Woods M, Bosk CL, Aveling EL, Goeschel CA, Pronovost PJ. Explaining Michigan: developing an ex post theory of a quality improvement program. The Milbank Quart. 2011;89(2):167‐205. 10.1111/j.1468-0009.2011.00625.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Sutcliffe KM, Paine L, Pronovost PJ. Re‐examining high reliability: actively organising for safety. BMJ Qual Saf. 2017;26(3):248‐251. 10.1136/bmjqs-2015-004698. [DOI] [PubMed] [Google Scholar]
- 64. Balding C. Create a Great Quality System in Six Months. Cathy Balding: Melbourne, Australia; 2013. [Google Scholar]
- 65. Balding C, Leggat S. The impact of quality management as a hospital strategy: findings from a mixed methods longitudinal study in Australian hospitals. La Trobe University Health Management Working Paper 2019; 2019.
- 66. Leggat SG, Balding C. A qualitative study on the implementation of quality systems in Australian hospitals. Health Serv Manage Res. 2017;30(3):179‐186. 10.1177/0951484817715594. [DOI] [PubMed] [Google Scholar]
- 67. Sellberg N, Eltes J. The Swedish patient portal and its relation to the national reference architecture and the overall ehealth infrastructure. In: GM AM, Hanseth O, Vassilakopoulou P, eds. Information Infrastructures within European Health Care. Health Informatics. Cham, Switzerland: Springer; 2017:225‐244. 10.1007/978-3-319-51020-0_14. [DOI] [PubMed] [Google Scholar]
- 68. Big data: what every Rheumatologist should know. Healio Rheumatol 2017. p. https://www.healio.com/rheumatology/rheumatoid-arthritis/news/print/healio-rheumatology/%7B5694936d-f54c-4db9-8bae-715b01bbeedf%7D/big-data-what-every-rheumatologist-should-know Accessed August 8, 2019 [Google Scholar]
- 69. Doran T, Maurer KA, Ryan AM. Impact of provider incentives on quality and value of health care. Annu Rev Public Health. 2017;38:449‐465. 10.1146/annurev-publhealth-032315-021457. [DOI] [PubMed] [Google Scholar]
- 70. Phipps‐Taylor M, Shortell SM. More than money: motivating physician behavior change in accountable care organizations. Milbank Q. 2016;94(4):832‐861. 10.1111/1468-0009.12230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. Berenson R, Pronovost P, Krumhloz H. Achieving the potential of health care performance measures. Robert Wood Johnson; 2013. https://www.rwjf.org/en/library/research/2013/05/achieving-the-potential-of-health-care-performance-measures.html Accessed March 3, 2018.
- 72. Peterson TA, Bernstein SJ, Spahlinger DA. Population health: a new paradigm for medicine. Am J Med Sci. 2016;351(1):26‐32. 10.1016/j.amjms.2015.10.011. [DOI] [PubMed] [Google Scholar]
- 73. Chen M, Unruh M, Pesko M, et al. Hospitals' engagement in population health: moving past the medicine and into the community. Health Aff. 2016; https://www.healthaffairs.org/do/10.1377/hblog20160405.054312/full/ Accessed December 27, 2017. [Google Scholar]
- 74. Quinn R, Rohrbaugh J. A competing values approach to organizational effectiveness. Public Prod Rev. 1981;122–40:5. [Google Scholar]
- 75. Tucker AE. Amy. Why hospitals don't learn from failures: psychological dynamics that inhibit system change. Calif Manage Rev. 2003;45(2):55‐72. [Google Scholar]
- 76. Tucker AL, Nembhard IM, Edmondson AC. Implementing new practices: an empirical study of organizational learning in hospital intensive care units. Manage Sci. 2007;53:894‐907. [Google Scholar]
- 77. Schein E. Organizational Culture and Leadership. San Francisco, CA: Jossey Bass; 1985. [Google Scholar]
- 78. Aarons GA, Fettes DL, Hurlburt MS, et al. Collaboration, negotiation, and coalescence for interagency‐collaborative teams to scale‐up evidence‐based practice. J Clin Child Adolesc Psychol. 2014;43: 915‐928. 10.1080/15374416.2013.876642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79. Birken S, Clary A, Tabriz AA, et al. Middle managers' role in implementing evidence‐based practices in healthcare: a systematic review. Implementat Sci. 2018;13(1):149. 10.1186/s13012-018-0843-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80. Birken SA, Lee S‐YD, Weiner BJ. Uncovering middle managers' role in healthcare innovation implementation. Implement Sci. 2012;7(1):28. 10.1186/1748-5908-7-28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81. Balogun J. From blaming the middle to harnessing its potential: creating change intermediaries. British J Manage. 2003;14(1):69‐83. 10.1111/1467-8551.00266. [DOI] [Google Scholar]
- 82. National Academy of Engineering (US) and Institute of Medicine (US) Committee on Engineering and the Health Care System . Building a Better Delivery System: A New Engineering/Health Care Partnership. Washington, DC: National Academies Press; 2005. [Google Scholar]


