Abstract
Objectives:
To develop a smartphone application providing sound therapy and cognitive behavioral therapy (CBT) for treating tinnitus and performing a proof-of-concept pilot study evaluating its potential efficacy.
Methods:
An interactive smartphone application available on iOS and Android platforms was developed, which provided an 8-week tinnitus-specific CBT and personalized and frequency-matched sound therapy. Included patients presented to our tertiary clinic in 2017-2018, while those waitlisted were regarded as controls. Three surveys were administrated: Tinnitus Handicap Inventory (THI), Generalized Anxiety Disorder 7-item (GAD-7), and Perceived Stress Scale (PSS).
Results:
A total of 30 patients enrolled in this study consisting of 20 treatment and 10 control patients and mean age was 55.4±11.6 years. Treatment and control patients had similar age, sex, and pre-enrollment GAD and PSS (all P>0.05). Baseline THI scores were also similar between treatment and control cohorts (50.1±21.9 vs. 62.0±20.7; P=0.15). After 8 weeks, though changes in GAD and PSS scores were similar (P>0.05), the treatment group reported a significantly greater improvement in THI scores (17.7±15.8 vs. 5.3±10.5, P=0.04).
Conclusions:
This pilot study demonstrated potentially promising efficacy of a smartphone-based CBT and sound therapy platform for treating tinnitus and encourages future randomized controlled trials on this treatment modality.
Keywords: tinnitus, cognitive behavioral therapy, sound therapy, mobile application, iOS, Android
Introduction
Approximately 21 million adult individuals in the U.S. suffer from tinnitus,1 many of whom describe it as a daily problem causing serious consequences such as missing work, having difficulty falling asleep, and experiencing anxiety and depression.2,3 Fewer than 50% of tinnitus sufferers discuss their symptoms with a physician, where medication is the most common recommendation for treatment.1 However, Food and Drug Administration or the scientific community have not yet approved any pharmacotherapeutic agents for treating tinnitus. Despite recent updates in emerging drugs for tinnitus, there is no overwhelming evidence or consensus on a pharmaceutical treatment.4,5 Of the therapeutic options, sound therapy and tinnitus-specific cognitive behavioral therapy (CBT) have been among the most studied and possibly efficacious treatments.1,6,7
CBT management involves a variety of interventions on the basis that maladaptive cognitions contribute to the distress and behavioral issues invoked by a chronic physiopsychological problem.8 There is some evidence that tinnitus and emotional relays in the brain may share some common pathways,9,10 necessitating a multi-disciplinary approach to management.11 Furthermore, sound therapy, initially introduced in the form of white noise, is meant to reduce tinnitus perception by diminishing the contrast between tinnitus and background auditory system activity.7 Sound therapy can relieve tinnitus by masking the sound on the principle of distraction,7 whereas CBT can improve the quality of life of tinnitus-sufferers by focusing on various coping mechanisms.12,13 Sound therapy has a success rate of about 90% in the short term 14, and CBT has a success rate of about 80%.15 A comprehensive review of six prospective randomized trials on sound therapy and 553 participants failed to show strong evidence for its efficacy for improving tinnitus.7 The existing literature on CBT seems more promising, with a systematic review of 15 randomized controlled trials and 1091 patients concluding the efficacy of CBT on reducing tinnitus-related symptoms, anxiety, and depression.6 In the 2014 American Academy of Otolaryngology-Head and Neck Surgery Society clinical practice guidelines, clinicians were encouraged to incorporate a wide variety of therapies for patients suffering from chronic tinnitus, which can include counseling, CBT, sound therapy, hearing aids, dietary changes, and medications.16
Recently, internet-based CBT (i-CBT) has become an available treatment option with a potentially significant reduction in tinnitus-related distress and symptoms.17 A randomized controlled study by Hesser and colleagues reported significant improvement in Tinnitus Handicap Inventory (THI) of tinnitus patients who received i-CBT.18 Despite emerging technologic advancements and development of smartphone applications for multiple chronic conditions such as diabetes,19 obesity,20 depression,21 or social anxiety,22 there currently exist no smartphone applications providing a combination of CBT and sound therapy specifically for tinnitus patients. As such, this manuscript proposes the design, construction, and preliminary validation of a novel smartphone-based 8-week program comprised of a newly designed tinnitus-specific CBT and frequency-matched personalized sound therapy. It is hypothesized that this designed program, with the novelty of combining these two novel CBT and sound therapy versions in a smartphone platform conveniently and accessible to everyone, will improve symptoms and quality of life measures related to tinnitus.
Methods
We developed an interactive smartphone application that provides tinnitus-specific CBT and personalized and frequency-matched sound therapy for the participants. The application was written via programming languages of Swift and Java for iOS and Android platforms respectively and available for download in Apple and Android stores. Simple design layout alongside visual guides and tutorials were implemented to enhance user experience and engagement (Figure 1). The CBT course consisted of eight weekly modules, providing strategies on emotional awareness, stress coping, sleeping techniques, identification of negative feelings, as well as exercise and meditation routines (Table 1). The application also provided recalibrating personalized sound therapy based on the frequency, volume, and sidedness of the tinnitus, which can also be played in the background while listening to regular music (Figure 2). The sound therapy audio files were constructed by MATLAB as per methods previously described by the authors.23 Patient were able to calibrate the sound therapy specific to their tinnitus’ type (e.g., ringing or buzzing), frequency, sidedness, and volume, at any time.
Figure 1.
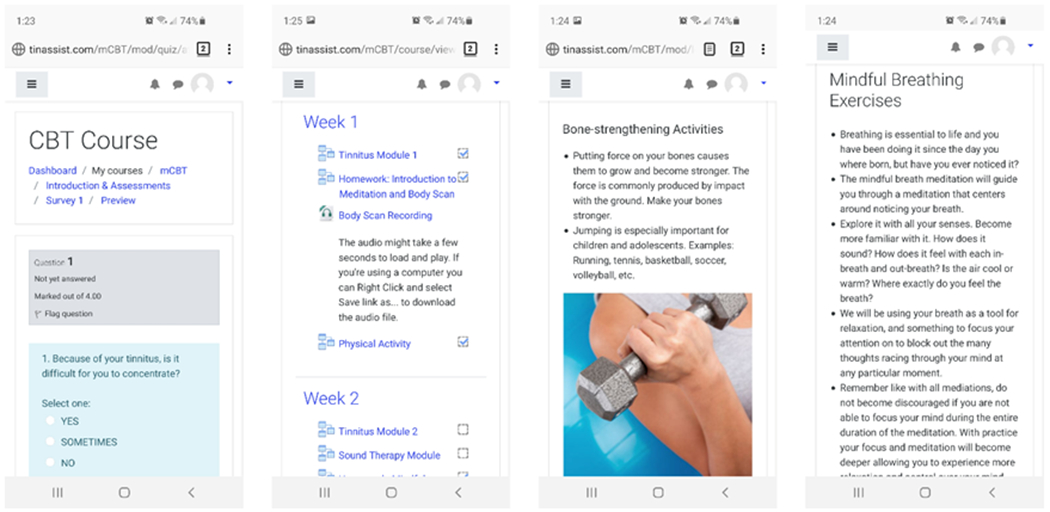
Snapshots of various CBT course modules, with easy-to-use layouts and implemented guides and tutorials to enhance user experience and engagement.
Table 1.
Modules during the 8-week course of cognitive behavioral therapy using the mobile device application.
| Week | Program Component | Explanation | Homework |
|---|---|---|---|
| 1 | Tinnitus Module 1 | Educational material on tinnitus and presentation of the general treatment rationale | None |
| Introduction to Meditation and Body Scan | Body scan mindfulness exercises through focusing on different parts of the body | Once a day, 15 min each time | |
| Physical Activity | Increase the level of physical activity to enhance well-being and to better manage stress and tinnitus | Mostly focused on increasing the everyday physical activity | |
| 2 | Customized Sound Therapy | Make tinnitus less noticeable by the use of external sounds, using customized sound therapy | Try sound therapy |
| Mindful Breathing Exercises | Meditation that centers around using the breath as a tool for relaxation | 2 times per day, 5–8 min each time | |
| 3 | Tinnitus Module 2 | Educational material on tinnitus | None |
| Sleeping Module | Brief description of general techniques for sleep problems | Follow advice regarding sleep | |
| Finding Your Breath | Relaxation through focusing on breathing | At least 5 times per day, 30 s to a few min each time in any environment | |
| 4 | Feelings Module | Learn and practice how to identify negative feelings | Follow the advice regarding negative feelings and do the exercises |
| Thoughts Module | Learn and practice how to identify distorted thoughts | Follow the advice regarding distorted thoughts and do the exercises | |
| Mindful Breathing Exercises | Meditation that centers around using the breath as a tool for relaxation | 2 times per day, 5–8 min each time | |
| 5 | Emotional Processing Module | Exploring and understanding how we process and conceptualize emotion | Follow the advice regarding emotional processing and do the exercises |
| Changing Negative Thoughts Module | Introduction to the influence and modification of negative automatic thoughts | Use the techniques and do the exercises | |
| Finding Your Breath | Relax through controlled breathing | At least 5 times per day, 30 s to a few min each time in any environment | |
| 6 | Thought Restructuring | Practice for changing negative thoughts | Use the techniques and do the exercises |
| Body Scan | Exploring and enhancing the ability to shift focus between tinnitus and some other stimuli | 2 times per day, 5–8 min each time | |
| Finding Your Breath | The use of rapid relaxation (controlled breathing and cue-controlled relaxation) in everyday situations | At least 5 times per day, 30 s to a few min each time in any environment | |
| 7 | Reduction of Worries & Stress Module | Advice regarding techniques that are helpful in reducing the amount of worries | Follow advice regarding reducing worries |
| Mindful Breathing | Expanding the use of rapid relaxation to more stressful situations and to everyday tinnitus distress | 2 times per day, 5–8 min each time | |
| 8 | Finding Your Breath | Incorporate applied relaxation in everyday life in a realistic way | At least 5 times per day, 30 s to a few min each time in any environment |
| Summary, Maintenance, and Relapse Prevention | Summarize what has been done during the treatment and how it has worked; make a plan for the future | Write personalized summary and plan |
Figure 2.
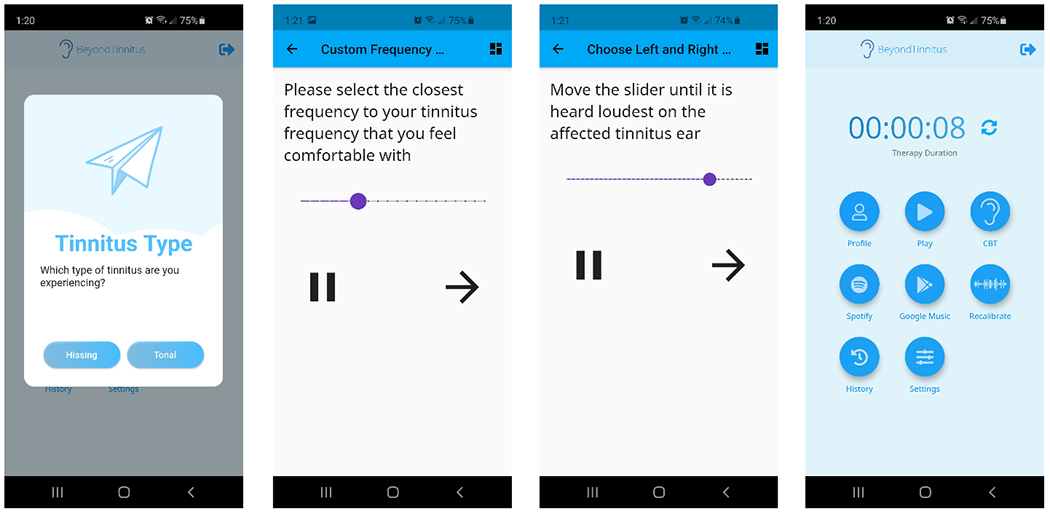
Recalibrating personalized sound therapy equipped within the application, which will take into consideration the participants’ frequency, volume, and sidedness of the tinnitus. Furthermore, the application’s sound therapy can play in the background of regular music from Google music or Spotify.
Subjects were advised to spend 2 hours daily listening to sound therapy and 2-3 hours weekly on CBT modules and implementation of the recommendations and meditations/exercises. Patients could log in to the app through a phone, tablet, or computer to complete CBT modules or to listen to sound or music therapy. The phone app did not have a notification system; however, the website version kept track of users’ progress, when they last logged in, how much time they spent in the modules, and which modules they had completed. It also kept track of who had completed the entire CBT course. We collected surveys from each patient at the conclusion of the course and kept a log of testimonials for potential improvements in the future. Patients could also provide feedback on their own at any time during their use of the app.
This pilot study of our platform consisted of patients with a chief complaint of chronic constant bilateral non-pulsatile tinnitus for at least 6 months, self-described as moderate or distressing, presenting to our outpatient tertiary clinic from February 2017 to July 2018. Patients who had self-described mild or non-constant tinnitus, pulsatile tinnitus, tinnitus due to conductive hearing loss, fluctuating hearing loss, Meniere’s disease, or vestibular schwannoma, those who had scores above 90th percentile on psychiatric questionnaires, patients with moderately severe or worse hearing loss, and patients who could not speak or read English were excluded. Sampling between treatment and controls was according to a consecutive 2:1 ratio, where the first two patients expressing interest were enrolled in the program, and the third patient was asked to wait 8 weeks (and treated as control during this time) before getting the program thereafter as a complementary service. We obtained approval from the University of California, Irvine Institutional Review Board, where HIPAA-compliance of the platform and study’s code of ethical conduct were verified.
Prior to and after participating in the program, patients completed three standardized surveys: Tinnitus Handicap Inventory (THI), Generalized Anxiety Disorder 7-item (GAD-7), and Perceived Stress Scale (PSS). The THI questionnaire was developed to quantify the impact of tinnitus on daily living using a 25-item patient-perspective questionnaire.24 The GAD-7 survey is a 7-question survey for GAD screening and its severity used commonly in research and clinical practice,25 while the PSS is a 10-item questionnaire is one of the most widely used instrument for evaluated perception of stress.26 In addition to THI, which is widely used in tinnitus research, GAD-7 and PSS surveys were also utilized in this study since tinnitus can be a source of anxiety and stress for patients,27-29 and improving these parameters are clinically significant for the overall physical and mental health of the patients. Moreover, these two parameters have been similarly utilized in previous tinnitus studies.30,31 The study design mainly consisted of evaluating changes in these parameters after each patient underwent the 8-week program and was largely compliant with the recommended engagement with sound therapy and CBT portions.
Statistical analyses were performed using PASW Statistics 18.0 software (SPSS Inc., Chicago, IL) and a P value of <0.05 was considered statistically significant. We utilized Chi-square tests of independence and Mann-Whitney U tests (due to the small sample sizes and non-normally distributed data) for comparing categorical or continuous variables, respectively.
Results
A total of 30 patients enrolled in this pilot study, 20 of which completed the 8-week smartphone-based course while 10 patients acted as controls while waiting for the program. The overall cohort had a mean age of 55.4±11.6 years and consisted of 14 (47%) females. Patients in treatment and control groups had similar age (54.2±11.9 vs. 57.8±10.9, P=0.24) and proportion of female gender (55.0% vs. 30.0%, P=0.20). The treatment and control cohorts had similar pre-enrolment GAD (7.5±5.1 vs. 7.3±7.4; P = 0.49), PSS (15.5±8.8 vs. 15.3±6.7; P=0.90), and THI scores (50.1±21.9 vs. 62.0±20.7; P=0.15). Changes in pre- and post-survey results are compared in Table 2. Though the two cohorts had similar changes in GAD-7 (P=0.07) and PSS (P=0.34) scores, the treatment group had a significantly higher improvement in THI scores (17.7±15.8 vs. 5.3±10.5, P=0.04).
Table 2.
Comparison of differences in pre- and post-survey results between the two cohorts.
| Survey/Measurement | Control Cohort’s Change in Pre – Post Survey Scores (Mean ± SD) | Treatment Cohort’s Change in Pre – Post Survey Scores (Mean ± SD) | P value |
|---|---|---|---|
| Tinnitus Handicap Inventory | 5.3±10.5 | 17.7±15.8 | 0.04* |
| Generalized Anxiety Disorder | 0.1±3.5 | 2.2±4.4 | 0.07 |
| Perceived Stress Scale Score | −0.7±3.8 | 1.6±5.5 | 0.34 |
Asterisk denotes to significant P value. SD, standard deviation.
Discussion
A variety of mobile device applications, such as white noise or meditation programs, exist that can indirectly manage tinnitus. This pilot study assessed preliminary results of the first mobile device application that incorporates CBT and customized sound therapy into a user-friendly platform. Patients were informed that the goal was not to eliminate tinnitus, but rather to reduce its impact on quality of life, perceived attention to tinnitus, and psychological disruption. A significantly larger reduction of THI score was observed in the treatment group, which supports the potentially promising efficacy of this novel platform. Even though we did not observe a significantly different change in depression or stress measures, this treatments’ improvement in tinnitus-specific quality of life measures (i.e., THI) is encouraging as proof-of-concept, warranting continued investigation smartphone-based CBT and sound therapy combination.
In our pilot study, patients receiving the program reported a decreased level of anxiety and handicap from their tinnitus based on the THI. Most importantly, our observed change in mean pre- and post-THI scores was above Zeman et al.’s concluded minimal clinically relevant change of 6-7 points.32 Previously, Henry and colleagues developed an iPhone application providing CBT for tinnitus patients, though quality of life measures such as THI were not assessed and to our knowledge the application is not available to the public.33 In a review of smart services for tinnitus self-help, Kalle et al. reported that internet-based services not only have the potential to provide therapeutic value, but they can also collect patient assessments useful for diagnostic purposes and evaluating evolution over time.17 Andersson and colleagues have reported that compared to controls, tinnitus-related distress, depression, and daily annoyance decreased significantly with i-CBT,12 which can potentially lead to time and cost saving compared to physical CBT. The results of the surveys were heterogeneous, which is commonly seen in tinnitus patients.
Although our studied patients’ GAD and PSS scores did not demonstrate significant improvement, the statistical improvement in THI, which incorporates tinnitus-induced anxiety and distress components, shows promising efficacy in some important qualities of life aspects. As such, a future large randomized controlled study with careful evaluation of multiple objective and subjective outcomes is warranted to further evaluate this type of treatment platform, which can also be significantly valuable to individuals who do not have easy access to in-person healthcare.34 The lack of significant improvement in GAD and PSS scores may be attributable to a few factors. The GAD and PSS are an assessment of general anxiety and stress from all sources in an individual’s life. The THI, on the other hand, measures tinnitus-specific anxiety, stress, and quality of life. Individuals in our cohorts may have experienced reductions in tinnitus-related adverse moods while still experiencing anxiety and stress from other sources, such as work or relationships. The relatively short time frame of this study may not have captured the entirety of the changes in life circumstances for each of our cohorts, and this may have been magnified by the smaller sample sizes.
Previously, we have administered accurate and feasible tone-matched sound therapy via a web-based software, where patients reported decreased loudness and annoyances of tinnitus.35 In a later study, we used the same web-based platform in a randomized crossover clinical trial to demonstrate the superiority of this customized sound therapy in decreasing THI scores and tinnitus loudness of patients compared to non-customized broadband noise.23 The software was capable of incorporating an individual’s tinnitus type, pitch, and loudness, and develop sound files composed of pitch-matched series of narrow-band noise peaks.23 This novel tone-matching software, now programmed in the new smartphone application, may continue to bring similar therapeutic efficacy for tinnitus sufferers through the concept of tinnitus masking.36 Though our study cannot differentiate between the specific benefit from sound therapy versus CBT, we believe the combination of the two into a novel and user-friendly smartphone platform constantly accessible to patients at their discretion makes this a unique and potentially efficacious management option for tinnitus sufferers. Our results of this pilot study add to the growing literature that CBT and sound therapy can be helpful for suppressing tinnitus symptoms and their effect on quality of life.17,18,23,37-39 Following this proof-of-concept pilot study, we will be evaluating the second version of this smartphone program in a large randomized controlled clinical trial.
To our knowledge, this is the first mobile application that combines CBT and personalized sound therapy. This online and self-managed solution can potentially address the significant barrier to treatment experienced by many tinnitus sufferers such as financial resources, insurance, means of transportation, and city or country of residence. It should be highlighted that the specific aim of this pilot study was to preliminary evaluate this novel application and propose this treatment platform as part of a new frontier for managing tinnitus. Though there are limitations with the current report, such as selection bias, small patient cohorts, and lack of extensive evaluation of quantitative or qualitative outcomes, the change in THI warrants further investigation of this platform’s potential efficacy. Besides the low sample size, this preliminary report is limited based on patient selection and the lack of randomization of the participants into the two groups. The study is also limited by the level of scaling and analysis to determine/compare tinnitus severity. Another limitation was a lack of patients’ clinical history of auditory masking, which could be important when evaluating which group of patients are more susceptible to improvement from sound therapy.40-42 This is significant because patients’ auditory masking may be the most significant predictor of the level of therapeutic efficacy that can be received from customized sound therapy. To address this, we will continue investigating this program, and implement Feldmann H masking evaluation to associate it with the sound therapy’s relative masking effect. Tinnitus and its effect on people can be uniquely individualized in other ways as well, making the proposed program more suitable for certain patients compared to the others. Due to these limitations, the findings may not be generalized to the general population until further investigations of such mobile applications with appropriate methodologies are applied. Future studies should also collect and analyze THI questionnaire’s subscale scores beyond this manuscript’s reported total score. With the positive feedback from participants and the promising results of the pilot study, this report will be followed by a proper randomized controlled clinical trial. By investigating detailed tinnitus-related and behavioral questionnaires prior to and after the program, we can evaluate specific factors associated with program responsiveness, and which patients will be most likely to improve.
Conclusion
Mobile application can potentially provide an effective and user-friendly platform for providing personal therapy and tinnitus rehabilitation. The combination of CBT and sound therapy on an easily accessible smartphone platform may be beneficial to tinnitus sufferers. Future randomized-controlled trials of larger sample sizes are warranted to assess the psychosocial efficacy of such application-delivered management for tinnitus patients.
Acknowledgement
This project was supported by an award from the UC Irvine School of Medicine Committee on Interdisciplinary Research to Hamid R. Djalilian. Mehdi Abouzari is supported by the National Center for Research Resources and the National Center for Advancing Translational Sciences, National Institutes of Health, through Grant TL1TR001415.
Footnotes
Financial Disclosure: Disclosed at the end of the manuscript.
Conflicts of Interest: Hamid R. Djalilian holds equity in MindSet Technologies and Cactus Medical LLC.
Portion of this work has been presented at the AAO-HNSF 2019 Annual Meeting & OTO Experience, September 15-18, 2019, New Orleans, LA.
References
- 1.Bhatt JM, Lin HW, Bhattacharyya N. Prevalence, Severity, Exposures, and Treatment Patterns of Tinnitus in the United States. JAMA Otolaryngol Head Neck Surg 2016; 142:959–965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bhatt JM, Bhattacharyya N, Lin HW. Relationships between tinnitus and the prevalence of anxiety and depression. Laryngoscope 2017; 127:466–469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Halford JB, Anderson SD. Anxiety and depression in tinnitus sufferers. J Psychosom Res 1991; 35:383–390. [DOI] [PubMed] [Google Scholar]
- 4.Langguth B, Elgoyhen AB, Cederroth CR. Therapeutic Approaches to the Treatment of Tinnitus. Annu Rev Pharmacol Toxicol 2019; 59:291–313. [DOI] [PubMed] [Google Scholar]
- 5.Cederroth CR, Dyhrfjeld-Johnsen J, Langguth B. An update: emerging drugs for tinnitus. Expert Opin Emerg Drugs 2018; 23:251–260. [DOI] [PubMed] [Google Scholar]
- 6.Hesser H, Weise C, Westin VZ, Andersson G. A systematic review and meta-analysis of randomized controlled trials of cognitive-behavioral therapy for tinnitus distress. Clin Psychol Rev 2011; 31:545–553. [DOI] [PubMed] [Google Scholar]
- 7.Hobson J, Chisholm E, El Refaie A. Sound therapy (masking) in the management of tinnitus in adults. Cochrane Database Syst Rev 2010:CD006371. [DOI] [PubMed] [Google Scholar]
- 8.Hofmann SG, Asnaani A, Vonk IJ, Sawyer AT, Fang A. The Efficacy of Cognitive Behavioral Therapy: A Review of Meta-analyses. Cognit Ther Res 2012; 36:427–440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Shulman A A Final Common Pathway for Tinnitus - The Medial Temporal Lobe System. Int Tinnitus J 1995; 1:115–126. [PubMed] [Google Scholar]
- 10.Shulman A Efferent auditory system pathways and tinnitus. Tinnitus diagnosis/treatment Lea & Febiger. 1991:184–210 [Google Scholar]
- 11.Shulman A, Goldstein B. Medical Significance of Tinnitus. Int Tinnitus J 1997; 3:45–50. [PubMed] [Google Scholar]
- 12.Andersson G Psychological aspects of tinnitus and the application of cognitive-behavioral therapy. Clin Psychol Rev 2002; 22:977–990. [DOI] [PubMed] [Google Scholar]
- 13.Sadlier M, Stephens SD, Kennedy V. Tinnitus rehabilitation: a mindfulness meditation cognitive behavioural therapy approach. J Laryngol Otol 2008; 122:31–37. [DOI] [PubMed] [Google Scholar]
- 14.Reavis KM, Rothholtz VS, Tang Q, Carroll JA, Djalilian H, Zeng FG. Temporary suppression of tinnitus by modulated sounds. J Assoc Res Otolaryngol 2012; 13:561–571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Heinecke K, Weise C, Rief W. [Chronic tinnitus: which kind of patients benefit from an outpatient psychotherapy?]. Psychother Psychosom Med Psychol 2010; 60:271–278. [DOI] [PubMed] [Google Scholar]
- 16.Tunkel DE, Bauer CA, Sun GH, et al. Clinical practice guideline: tinnitus. Otolaryngol Head Neck Surg 2014; 151:S1–S40. [DOI] [PubMed] [Google Scholar]
- 17.Kalle S, Schlee W, Pryss RC, et al. Review of Smart Services for Tinnitus Self-Help, Diagnostics and Treatments. Front Neurosci 2018; 12:541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hesser H, Gustafsson T, Lunden C, et al. A randomized controlled trial of Internet-delivered cognitive behavior therapy and acceptance and commitment therapy in the treatment of tinnitus. J Consult Clin Psychol 2012; 80:649–661. [DOI] [PubMed] [Google Scholar]
- 19.Chomutare T, Fernandez-Luque L, Arsand E, Hartvigsen G. Features of mobile diabetes applications: review of the literature and analysis of current applications compared against evidence-based guidelines. J Med Internet Res 2011; 13:e65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Gan KO, Allman-Farinelli M. A scientific audit of smartphone applications for the management of obesity. Aust N Z J Public Health 2011; 35:293–294. [DOI] [PubMed] [Google Scholar]
- 21.Huguet A, Rao S, McGrath PJ, et al. A Systematic Review of Cognitive Behavioral Therapy and Behavioral Activation Apps for Depression. PLoS One 2016; 11:e0154248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Miloff A, Marklund A, Carlbring P. The challenger app for social anxiety disorder: New advances in mobile psychological treatment. Internet Interventions. 2015; 2(4): 382–391. [Google Scholar]
- 23.Mahboubi H, Haidar YM, Kiumehr S, Ziai K, Djalilian HR. Customized Versus Noncustomized Sound Therapy for Treatment of Tinnitus: A Randomized Crossover Clinical Trial. Ann Otol Rhinol Laryngol 2017; 126:681–687. [DOI] [PubMed] [Google Scholar]
- 24.Newman CW, Jacobson GP, Spitzer JB. Development of the Tinnitus Handicap Inventory. Arch Otolaryngol Head Neck Surg 1996; 122:143–148. [DOI] [PubMed] [Google Scholar]
- 25.Spitzer RL, Kroenke K, Williams JB, Lowe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med 2006; 166:1092–1097. [DOI] [PubMed] [Google Scholar]
- 26.Cohen S, Kamarck T, Mermelstein R. Perceived stress scale. Measuring stress: A guide for health and social scientists. 1994;10. [Google Scholar]
- 27.Hebert S, Lupien SJ. The sound of stress: blunted cortisol reactivity to psychosocial stress in tinnitus sufferers. Neurosci Lett 2007; 411:138–142. [DOI] [PubMed] [Google Scholar]
- 28.Heinecke K, Weise C, Schwarz K, Rief W. Physiological and psychological stress reactivity in chronic tinnitus. J Behav Med 2008; 31:179–188. [DOI] [PubMed] [Google Scholar]
- 29.Pattyn T, Van Den Eede F, Vanneste S, et al. Tinnitus and anxiety disorders: A review. Hear Res 2016; 333:255–265. [DOI] [PubMed] [Google Scholar]
- 30.Bruggemann P, Szczepek AJ, Rose M, McKenna L, Olze H, Mazurek B. Impact of Multiple Factors on the Degree of Tinnitus Distress. Front Hum Neurosci 2016; 10:341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ketterer MC, Knopke S, Haussler SM, et al. Asymmetric hearing loss and the benefit of cochlear implantation regarding speech perception, tinnitus burden and psychological comorbidities: a prospective follow-up study. Eur Arch Otorhinolaryngol 2018; 275:2683–2693. [DOI] [PubMed] [Google Scholar]
- 32.Zeman F, Koller M, Figueiredo R, et al. Tinnitus handicap inventory for evaluating treatment effects: which changes are clinically relevant? Otolaryngol Head Neck Surg 2011; 145:282–287. [DOI] [PubMed] [Google Scholar]
- 33.Henry JA, Thielman E, Zaugg T, et al. Development and field testing of a smartphone “App” for tinnitus management. Int J Audiol 2017; 56:784–792. [DOI] [PubMed] [Google Scholar]
- 34.Martinez P, Rojas G, Martinez V, Lara MA, Perez JC. Internet-based interventions for the prevention and treatment of depression in people living in developing countries: A systematic review. J Affect Disord 2018; 234:193–200. [DOI] [PubMed] [Google Scholar]
- 35.Mahboubi H, Ziai K, Djalilian HR. Customized web-based sound therapy for tinnitus. Int Tinnitus J 2012; 17:26–30. [PubMed] [Google Scholar]
- 36.Feldmann H. Homolateral and contralateral masking of tinnitus by noise-bands and by pure tones. Audiology 1971; 10:138–144. [DOI] [PubMed] [Google Scholar]
- 37.Tyler RS, Perreau A, Powers T, et al. Tinnitus Sound Therapy Trial Shows Effectiveness for Those with Tinnitus. J Am Acad Audiol 2020; 31:6–16. [DOI] [PubMed] [Google Scholar]
- 38.Theodoroff SM, McMillan GP, Zaugg TL, Cheslock M, Roberts C, Henry JA. Randomized Controlled Trial of a Novel Device for Tinnitus Sound Therapy During Sleep. Am J Audiol 2017; 26:543–554. [DOI] [PubMed] [Google Scholar]
- 39.Li J, Jin J, Xi S, et al. Clinical efficacy of cognitive behavioral therapy for chronic subjective tinnitus. Am J Otolaryngol 2019; 40(2): 253–256. [DOI] [PubMed] [Google Scholar]
- 40.Henry JA, Schechter MA, Zaugg TL, et al. Outcomes of clinical trial: tinnitus masking versus tinnitus retraining therapy. J Am Acad Audiol 2006; 17(2): 104–132. [DOI] [PubMed] [Google Scholar]
- 41.Vernon JA, Meikle MB. Masking devices and alprazolam treatment for tinnitus. Otolaryngol Clin North Am 2003; 36(2): 307–320. [DOI] [PubMed] [Google Scholar]
- 42.Hazell JW, Wood SM. Tinnitus masking-a significant contribution to tinnitus management. Br J Audiol 1981; 15: 223–230. [DOI] [PubMed] [Google Scholar]


