Abstract
Purpose:
Mantle cell lymphoma (MCL) is characterized by the t(11;14)(q13;q32) translocation leading to cyclin D1 overexpression. Cyclin D1 is a major cell cycle regulator and also regulates transcription, but the impact of cyclin D1-mediated transcriptional dysregulation on MCL pathogenesis remains poorly understood. The aim of this study was to define a cyclin D1-dependent gene expression program and analyze its prognostic value.
Experimental design:
We integrated genome-wide expression analysis of cyclin D1-silenced and overexpressing cells with cyclin D1 chromatin binding profiles to identify a cyclin D1-dependent transcriptional program in MCL cells. We analyzed this gene program in two MCL series of peripheral blood samples (n=53) and lymphoid tissues (n=106) to determine its biological and clinical relevance. We then obtained a simplified signature of this program and evaluated a third series of peripheral blood MCL samples (n=81) by NanoString gene expression profiling to validate our findings.
Results:
We identified a cyclin D1-dependent transcriptional program composed of 295 genes that were mainly involved in cell cycle control. The cyclin D1-dependent gene program was overexpressed in MCL tumors directly proportional to cyclin D1 levels. High expression of this program conferred an adverse prognosis with significant shorter overall survival of the patients. These observations were validated in an independent cohort of patients using a simplified 37-gene cyclin D1 signature. The cyclin D1-dependent transcriptional program was also present in multiple myeloma and breast tumors with cyclin D1 overexpression.
Conclusion:
We identified a cyclin D1-dependent transcriptional program that is overexpressed in MCL and predicts clinical outcome.
Keywords: Mantle cell lymphoma, Cyclin D1, Gene expression profiling
Introduction
Mantle cell lymphoma (MCL) is a mature B-cell lymphoid neoplasm with a heterogeneous clinical behavior that varies from aggressive evolution in most patients, requiring immediate treatment, to indolent course that may be managed with conservative measures. The initial oncogenic event of MCL is the translocation t(11;14)(q13;q32) leading to cyclin D1 overexpression (1–3). Additionally, MCL usually carries a high number of secondary genetic and molecular alterations that target mainly genes involved in cell cycle, DNA damage, and cell survival (1). Dysregulation of cell cycle is considered one of the main hallmarks of MCL, and proliferation levels measured either by the Ki67 immunohistochemical index or a proliferation gene expression signature predict the outcome of the patients (4–7). Two molecular subtypes of MCL have been recently identified with different biological and clinical characteristics. Conventional MCL (cMCL) is usually very aggressive and the patients present with disseminated, predominantly nodal, disease, whereas the less frequent leukemic nonnodal MCL (nnMCL) subtype often has an indolent clinical evolution with isolated leukemic presentation, although eventually some tumors progress to more aggressive behavior (7–9). Prognostic biomarkers suitable for both subtypes are needed since the MCL proliferation gene signature, which is a robust prognostic parameter when measured in nodal samples, has a lower performance in blood samples (4,5,8).
MCL represents a paradigm of a neoplasia with cyclin D1-related oncogenesis. In fact, MCL cells frequently select additional mechanisms besides the t(11;14) translocation to further increase cyclin D1 levels, such as amplification of the translocated allele or mutations and rearrangements involving the cyclin D1 N-terminal fragment or the 3’ untranslated region (3’UTR) (5,10–13). These secondary genetic events have been associated with increased aggressiveness of the tumors (14). Besides MCL, cyclin D1 is frequently upregulated in other cancers by different genetic alterations. Among them, a subset of multiple myeloma carries the t(11;14) translocation, cyclin D1 amplifications are common in breast, head and neck, lung, pancreatic and colorectal cancer, and activating point mutations are present in esophageal and endometrial carcinomas (15).
The classical view of cyclin D1-mediated tumorigenesis considers that its oncogenic effect is based on its role in the G1/S phase transition through the CDK4-mediated phosphorylation of pRB (1). However, emerging data have shown that cyclin D1 has additional functions, such as transcriptional regulation through the interaction with several transcription factors and chromatin modifiers (16,17). Cyclin D1 seems to have a role both as a transcriptional activator and repressor depending on the molecular and cellular context (18,19). We recently reported that cyclin D1 shows widespread binding to promoters of active genes in malignant lymphoid cells and induces a global transcriptional down-modulation through the interaction with the transcriptional machinery (20). Nevertheless, we also observed that some cyclin D1 target genes were not affected by this global down-modulation and showed a paradoxical upregulation.
Whether cyclin D1-dependent transcriptional dysregulation has an impact on MCL pathogenesis remains poorly understood. In this study, we identified and characterized a transcriptional program activated by cyclin D1 in MCL, whose high overexpression conferred an adverse clinical outcome.
Materials and Methods
Cell lines
We used two well characterized MCL cell lines (13), JeKo-1 (ATCC, CRL-3006, RRID:CVCL_1865) and Granta-519 (DSMZ, ACC-342, RRID:CVCL_1818), the lymphoblastoid leukemic cell line JVM13 (ATCC, CRL-3003, RRID:CVCL_1318), and HEK293T (ATCC, CRL-3216, RRID:CVCL_0063). Cell lines were cultured at 37°C and 5% CO2; JeKo-1 and JVM13 in RPMI (Gibco) and Granta-519 and HEK293T in DMEM (Gibco), both supplemented with 10% FBS and penicillin-streptomycin (Gibco). Cell line authentication was performed by qCell Identity (qGenomics) when appropriate. Cells were tested for Mycoplasma on a regular basis. We obtained cyclin D1 knocked-down MCL cell lines by lentiviral infection using the shRNA plasmids TRCN0000295873 and TRCN0000295874 (Sigma-Aldrich) as described before (20,21). Cyclin D1 inducible overexpression models in JVM13, with wild type (CycD1wt) or a highly stable form of the protein with the T286A mutation (CycD1T286A), were generated previously (20). Cell infections and gene expression analyses were performed with low-passage cells.
Primary MCL samples
We studied two MCL series of 53 cases from peripheral blood samples and 106 from lymphoid tissues (lymph node and spleen) with gene expression microarray data previously reported (4,22). Additionally, we performed NanoString expression analysis in a third series of peripheral blood samples from 81 MCL patients, including sequential samples in five of them. All cases had cyclin D1 overexpression and samples were collected before treatment. Cases in the three cohorts were classified as cMCL or nnMCL based on gene expression signatures analyzed by expression microarrays or NanoString and/or SOX11 immunohistochemistry, depending on the available material, as reported before (23). Tumor cell purification (from peripheral blood samples) and RNA extraction was performed as previously described (24). Molecular characterization was performed as described before (4,8,23,25,26). To assess the status of cyclin D1 RNA (full length or truncated 3’UTR) a ratio of 1.5 between the two cyclin D1 probes was used as threshold, both in microarray and NanoString analyses. This study was approved by the institutional review board of the Hospital Clinic of Barcelona, patients provided written informed consent, and the investigation was conducted according to the Declaration of Helsinki.
RNA-sequencing and gene expression microarrays
RNA from cell lines was extracted with the RNeasy Plus Mini Kit (Qiagen). RNA-sequencing (RNA-seq) was performed in cyclin D1-silenced and control MCL cell lines (JeKo-1 and Granta-519) shortly after infection and selection. One μg of total RNA was used to prepare the RNA libraries, which were processed for 50bp single-end sequencing on Illumina HiSeq 2500 (supplementary Methods). Affymetrix Human Genome U219 microarrays were used to analyze cyclin D1-overexpressing and control JVM13 cells. Cyclin D1 was induced by doxycycline as described before (20). 150 ng of each RNA sample were processed according to the standard Affymetrix protocol (supplementary Methods). Data were deposited in GEO under accession numbers GSE144106 and GSE144095, respectively.
We also revisited several gene expression microarray data sets previously obtained by us and others using Affymetrix Human Genome U133 Plus 2.0 microarrays, and deposited under the following GEO accession numbers: GSE79196 for leukemic MCL samples (n=53) (22); GSE93291 for lymphoid tissue MCL samples (n=106) (4); GSE12453 and GSE3526 for normal naïve and memory B-cells (n=10) and normal lymphoid tissues (lymph node and spleen, n=11), respectively (27,28); GSE79196 for leukemic B-cell chronic lymphoid neoplasms (n=101; 54 chronic lymphocytic leukemia, 12 follicular lymphoma, 4 hairy cell leukemia variant, 4 lymphoplasmacytic lymphoma, 23 splenic marginal zone lymphoma, and 4 splenic diffuse red pulp lymphomas) (22); GSE70910 for paired leukemic and nodal MCL samples (29); and GSE19784 for multiple myeloma patients (30). Microarray data from breast cancer patients were available online (http://kmplot.com/) (31). Raw microarray data were normalized using the frozen robust multiarray analysis (fRMA) method (32), and differentially expressed genes were identified using Limma (33).
NanoString gene expression profiling
Gene expression of the simplified cyclin D1 signature generated in this study was evaluated on the NanoString platform (NanoString Technologies) together with 6 housekeeping genes and two cyclin D1 probes (exonic and 3’UTR) described before (4). 100 ng of total RNA from MCL peripheral blood samples were used. Data analysis was performed with nSolver v2.6 software; normalization was done using the geometric mean of both the internal positive controls and the six housekeeping genes. Normalized data were log2 transformed. Further details are described in supplementary Methods.
Statistical analysis
Analyses were performed using R software v3.5.0. The end point of the survival analyses was overall survival (OS). Univariate and multivariate Cox regression models were used to test the association of variables with survival. Martingale residuals of Cox regression models were used to assess the functional form of continuous covariates in relation to survival. The log-rank test was used to compare Kaplan–Meier curves. Unless otherwise specified, survival was calculated from the time of diagnosis. Associations between variables were measured with Student’s t-test, Fisher’s test or Pearson’s r as appropriate; statistical tests are indicated in the figure legends.
Results
Identification of a cyclin D1-dependent transcriptional program in MCL cells
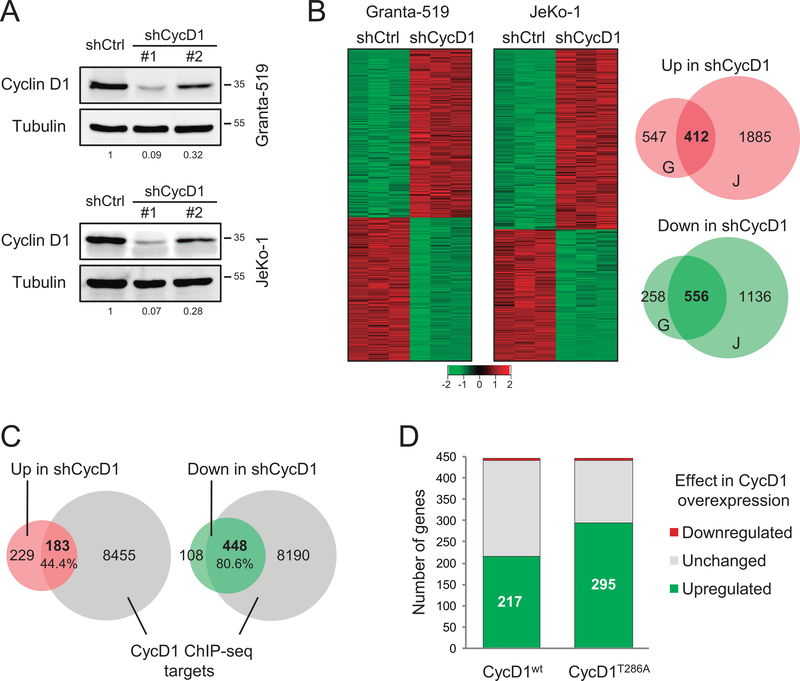
To study the transcriptional dysregulation associated with cyclin D1 overexpression in MCL, we initially silenced cyclin D1 using two shRNA constructs in Granta-519 and JeKo-1 MCL cells (Figure 1A and supplementary Figure S1A). As expected, analysis of EdU incorporation showed a noticeable decrease in cell proliferation in cyclin D1-depleted cells (supplementary Figure S1B). We then performed RNA-seq experiments using the most efficient shRNA to characterize the transcriptional profile related to cyclin D1 silencing. We identified 556 downregulated and 412 upregulated genes shared by the two cell lines, with a higher overlap in those genes downregulated upon cyclin D1 depletion (Figure 1B). Since we previously identified that cyclin D1 interacts with active promoters in MCL cells (20), we integrated the RNA-seq results with our previous cyclin D1 ChIP-sequencing (ChIP-seq) analysis, in which we identified 8,638 cyclin D1 target genes in four MCL cell lines. Interestingly, 448 (81%, p<2.2×10−16) of the genes downregulated upon cyclin D1 silencing had a cyclin D1 peak in their promoters, while only 183 (44%, p=0.574) of the genes upregulated following cyclin D1 depletion had a cyclin D1 peak (Figure 1C). These results suggest that cyclin D1 may participate in the activation of a specific set of genes.
Figure 1. Identification of a cyclin D1-dependent transcriptional program in MCL cells.
(A) Western blot analysis of cyclin D1 in control (shCtrl) and cyclin D1-silenced (shCycD1 #1 and #2) MCL cell lines. Tubulin was used as loading control. Cyclin D1 quantification normalized by tubulin and relative to shCtrl cells is shown. Molecular weights (in kDa) are indicated. (B) RNA-seq experiment in shCtrl and shCycD1 #1 MCL cells. Left, heatmaps showing significantly upregulated (red) and downregulated (green) genes in the three biological replicates. Right, Venn diagrams showing the overlap between differentially expressed genes in Granta-519 (G) and JeKo-1 (J) cells (in bold), which were selected for further analysis. (C) Venn diagrams showing the overlap between either upregulated (red) or downregulated (green) genes in shCycD1 MCL cells and cyclin D1 (CycD1) target genes by ChIP-seq in four MCL cell lines (n = 8,638). Statistical significance was assessed by one-tailed Fisher’s test. (D) Differential expression analysis of the cyclin D1-activated genes identified in MCL cells (n = 448) in CycD1wt or CycD1T286 overexpressing versus control JVM13 cells.
We then analyzed the transcriptional profile associated with cyclin D1 overexpression using cellular models established in the cyclin D1-negative lymphoblastoid cell line JVM13. We overexpressed either CycD1wt or CycD1T286A (supplementary Figure S2A), a mutant that reaches expression levels closer to the high amounts observed in MCL (20). We identified 739 upregulated and 841 downregulated genes common in both models. Concordantly with the cyclin D1 silencing experiments, we observed that the proportion of genes with a cyclin D1 peak in their promoters was markedly higher in the genes upregulated upon cyclin D1 overexpression (63%, p<2.2×10−16) than in the downregulated ones (37%, p=0.994), confirming the contribution of cyclin D1 in transcriptional activation of a specific gene set (supplementary Figure S2B).
We then combined the cyclin D1 silencing and overexpression results to define a robust gene expression program associated with cyclin D1 dysregulation. Remarkably, we observed that 295 (66%) of the 448 genes that were downregulated by cyclin D1 depletion in MCL cells and had a cyclin D1 peak in their promoters were upregulated by CycD1T286A overexpression in JVM13 cells (Figure 1D and supplementary Figure S2C). This tendency was also observed in the CycD1wt cells, although the proportion of genes upregulated was slightly lower concordantly with the lower cyclin D1 expression in these cells. Taken together, these results strongly suggest that cyclin D1 promotes the transcriptional activation of a specific subset of its target genes in MCL cell lines. We identified a cyclin D1-dependent transcriptional program of 295 genes that were downregulated upon cyclin D1 silencing, upregulated upon cyclin D1 overexpression, and had a cyclin D1 peak in their promoters (supplementary Figure S3 and supplementary Table S1).
Cyclin D1 promotes the activation of a cell cycle transcriptional program
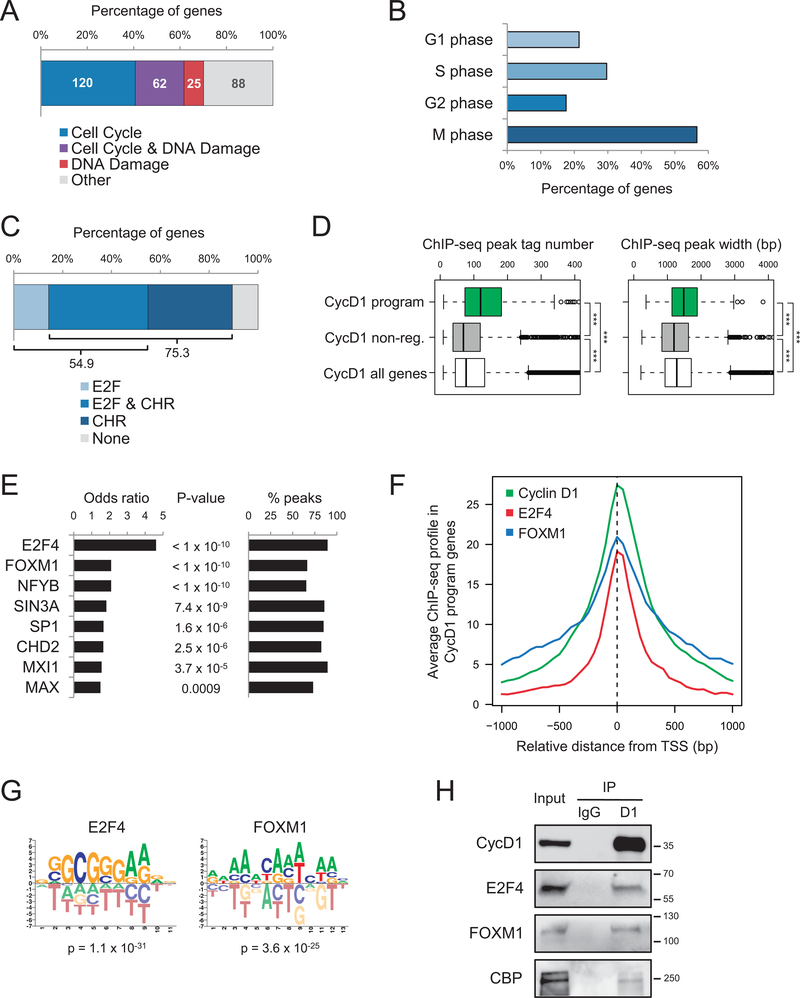
Gene Ontology (GO) analysis of the 295 genes activated by cyclin D1 showed a high enrichment of cell cycle and DNA damage, with 182 (62%) of them involved in the four phases of the cell cycle (Figure 2A–B and supplementary Table S2). Transcriptional control during cell cycle is based on two major waves of transcription: one occurring during G1/S phases, whose genes are characterized by E2F motifs in their promoters, and the other during G2/M, with genes displaying CHR elements (34). Both E2F and CHR motifs were highly enriched in the cyclin D1 peaks present in the promoters of cyclin D1-activated genes, reinforcing the idea that cyclin D1 regulates the expression of genes that control the entire cell cycle (Figure 2C). These results are consistent with the reduced proliferation following cyclin D1 silencing in MCL cells described above.
Figure 2. Cyclin D1 promotes the activation of a cell cycle transcriptional program.
(A) GO analysis of cyclin D1-dependent gene expression program (n = 295) showing the number and the percentage of genes involved in cell cycle (p = 3.4 × 10−116), DNA damage response (p = 2.4 × 10−47), or both. (B) Percentage of cell cycle genes from the cyclin D1-dependent transcriptional program (n = 182) corresponding to the four cell cycle phases according to GO categories. G1 corresponds to “cell cycle G1/S phase transition” (p = 1.4 × 10−26), S to “DNA replication” (p = 1.3 × 10−64), G2 to “cell cycle G2/M phase transition” (p = 5.9 × 10−22), and M to “cell division” (p = 6.7 × 10−61) and “chromosome segregation” (p = 6.4 × 10−56). Genes belonging to more than one category were included in all of them. (C) Analysis of DNA motifs related to cell cycle transcriptional control in the cyclin D1 peaks present in the promoters of cyclin D1-activated genes. Statistical assessment by Fisher’s test in comparison to all gene promoters resulted in p < 2.2 × 10−16 for E2F and p = 0.003 for CHR sites. (D) Boxplots of cyclin D1 ChIP-seq peak tag number and width, corresponding to the cyclin D1-activated genes (n = 295), cyclin D1 non-regulated genes (n = 2,752), and all cyclin D1 target genes (n = 8,638). Statistical significance was assessed by two-tailed Student’s t-test, ***: p < 0.0001. (E) Colocalization analysis between cyclin D1 peaks and transcriptional regulators from the ENCODE database (GM12878 cells) in the cyclin D1-activated genes. Statistical significance was assessed by Fisher’s test in comparison with cyclin D1 non-regulated genes. Percentages of cyclin D1-activated genes containing a peak of the corresponding transcription factor overlapping with the cyclin D1 peak are indicated; only the transcription factors present in more than 50% of genes were selected. (F) ChIP-seq profiles of cyclin D1 (in JeKo-1 cells) and E2F4 and FOXM1 (in GM12878 cells) around the transcription start site (TSS) from the cyclin D1-dependent program genes. (G) Enrichment of E2F4 and FOXM1 motifs in cyclin D1 peaks present in cyclin D1-activated gene promoters. (H) Co-IP experiments of endogenous cyclin D1 with E2F4, FOXM1, and CBP in JeKo-1 cells. IgG was used as a control. Molecular weights (in kDa) are indicated.
We next explored the specific features of the cyclin D1 peaks present in the promoters of the 295 genes activated by cyclin D1. For that, we compared the morphology of these cyclin D1 peaks with either the peaks present in all cyclin D1 target genes or with the peaks from a subset of cyclin D1 target genes whose expression remained stable upon cyclin D1 silencing (cyclin D1 non-regulated genes). Cyclin D1 peaks present in cyclin D1-activated genes were significantly larger, with higher tag number and width, suggesting that they represent a specific subgroup among all cyclin D1 peaks (Figure 2D). We next analyzed whether cyclin D1 peaks overlapped with specific transcription factors in cyclin D1-activated gene promoters compared to cyclin D1 non-regulated genes. We used ChIP-seq data corresponding to multiple transcription factors from the ENCODE project obtained in normal B-cells (GM12878) (35). Interestingly, we found a significant overlap between cyclin D1 peaks and several factors involved in transcriptional regulation during cell cycle (34), such as E2F4 and FOXM1 (Figure 2E and supplementary Table S3). These results are concordant with the previous observation that most cyclin D1-activated genes are cell cycle-related. Accordingly, we observed a clear colocalization of cyclin D1 with both E2F4 and FOXM1 around the transcription start site of cyclin D1-activated genes (Figure 2F). Motif enrichment analysis showed that E2F4 and FOXM1 binding sites were significantly enriched in the cyclin D1 peaks present in cyclin D1-activated gene promoters (Figure 2G and supplementary Table S4). Of note, FOXM1 was one of the genes included in the cyclin D1-dependent transcriptional program. Interestingly, cyclin D1 was previously described to interact with both transcription factors in other cell types (36–40). Co-immunoprecipitation (co-IP) experiments in JeKo-1 cells confirmed that cyclin D1 physically interacted with both E2F4 and FOXM1 (Figure 2H). In other cellular contexts, cyclin D1 has been shown to activate transcription through the recruitment of the coactivator CBP (41). Co-IP experiments also confirmed the interaction between these two proteins in MCL cells (Figure 2H). Together, these results show that cyclin D1 promotes the activation of an expression program of genes mainly involved in cell cycle control through a mechanism that may include in part the interaction of cyclin D1 with key cell cycle transcriptional regulators such as E2F4 and FOXM1, and with CBP.
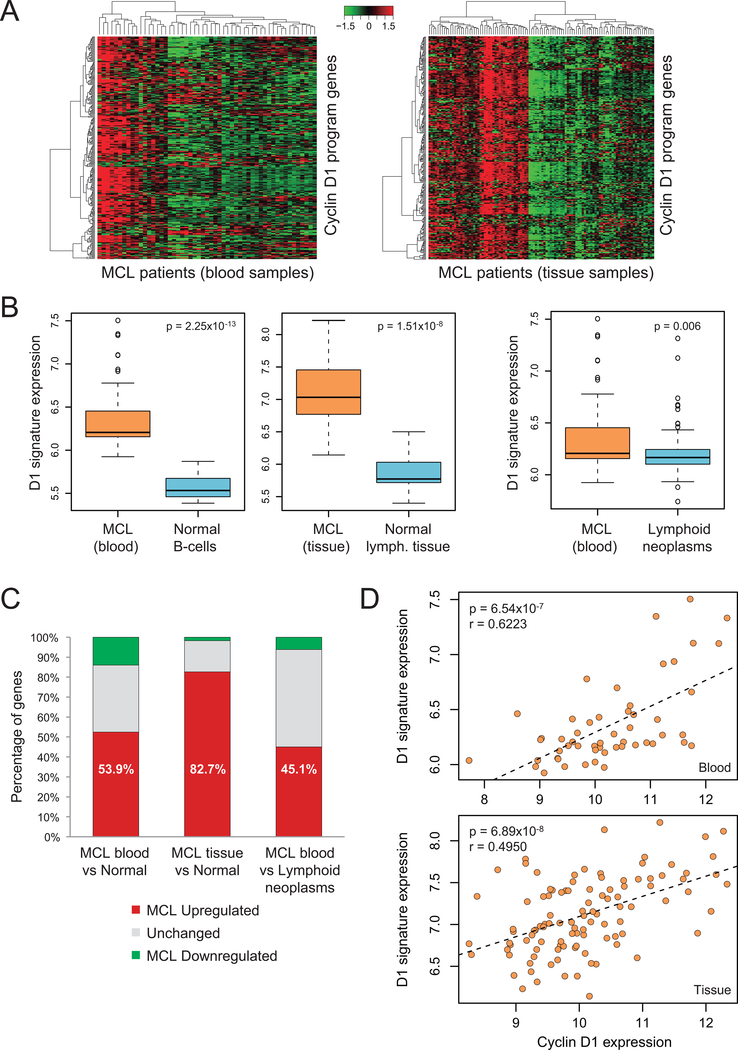
Cyclin D1-dependent transcriptional program is upregulated in primary MCL
To determine whether the cyclin D1-dependent transcriptional program identified in MCL cell lines was also modulated in primary MCL tumors, we studied the microarray expression data in two independent MCL cohorts of 53 cases from peripheral blood samples (55% cMCL, 45% nnMCL) and 106 from lymphoid tissues (96% cMCL, 4% nnMCL). Hierarchical clustering analysis of the 295 cyclin D1-activated genes in both blood and tissue samples resulted in the distribution of MCL patients in groups with different expression levels (Figure 3A). Since cyclin D1-activated genes had a homogeneous expression pattern within each patient, we summarized the cyclin D1-dependent program by defining a cyclin D1 signature score based on the mean expression of all genes (supplementary Figure S4).
Figure 3: Cyclin D1-dependent transcriptional program is upregulated in primary MCL.
(A) Heatmap and hierarchical clustering analysis of cyclin D1-dependent gene program in MCL primary cases from both peripheral blood (n = 53, left) and lymphoid tissue (n = 106, right) samples. (B) Boxplots displaying the 295-gene cyclin D1 signature expression score. Left, MCL primary cases from peripheral blood versus normal naïve and memory B-cells (n = 10), and MCL lymphoid tissue samples versus normal lymphoid tissues (n = 11). Right, MCL primary cases from peripheral blood versus leukemic cyclin D1-negative lymphoid neoplasms (n = 101). Statistical significance was assessed by two-tailed Student’s t-test. (C) Differential gene expression analysis of cyclin D1-dependent program genes (n = 295) in MCL primary cases versus either normal samples or other lymphoid neoplasms; percentages of upregulated genes in MCL are indicated. (D) Correlation between cyclin D1 expression and the 295-gene cyclin D1 signature score in MCL primary cases, from both peripheral blood and lymphoid tissue samples. Correlation was assessed by Pearson’s r.
Given that cyclin D1 is specifically overexpressed in MCL, we analyzed whether the cyclin D1 signature was upregulated in primary MCL. We used gene expression microarray data from normal B-cell and lymphoid tissue samples to compare them with blood and tissue MCL samples, respectively (27,28). Interestingly, we found that the cyclin D1-dependent transcriptional program was highly overexpressed in MCL (Figure 3B). Additionally, by analyzing expression microarrays from a large series of different leukemic cyclin D1-negative B-cell lymphoid neoplasms (22), we found that the cyclin D1 signature was significantly overexpressed in leukemic MCL compared to other lymphoid malignancies (Figure 3B). Concordantly, a high proportion of the 295 cyclin D1-activated genes were upregulated in MCL compared to the normal lymphoid samples or other lymphoid neoplasms (Figure 3C and supplementary Figure S5A). Furthermore, we found a strong positive correlation between cyclin D1 signature expression and cyclin D1 levels in primary MCL, in both blood and tissue samples (Figure 3D). Accordingly, the vast majority of cyclin D1-activated genes showed a significant positive correlation with cyclin D1 (supplementary Figure S5B). Additionally, the expression analysis of two gene sets composed by FOXM1 or E2F4 targets obtained in GM12878 cells (35) displayed a significant correlation with cyclin D1 levels in primary MCL cases, further supporting the functional interplay of cyclin D1 with these two transcription factors (supplementary Figure S6). Taken together, these results suggest that cyclin D1 overexpression in primary MCL contributes to the upregulation of the cyclin D1-dependent transcriptional program identified in cell lines.
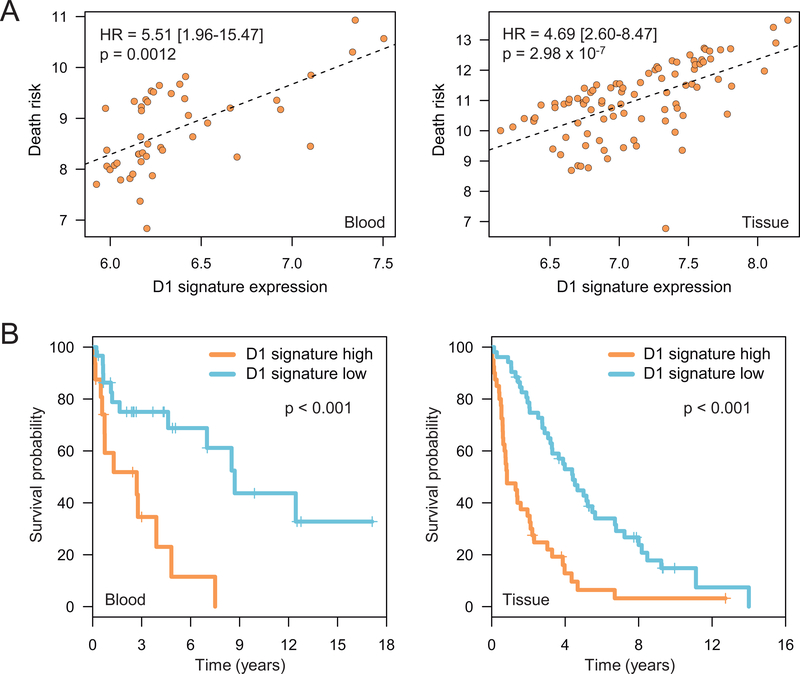
Expression levels of cyclin D1-dependent transcriptional program correlate with survival in MCL patients
We next investigated whether the cyclin D1-dependent transcriptional program was associated with clinicopathological features. We observed a significant association between high levels of cyclin D1 signature and common genetic alterations in MCL such as 17p/TP53 alteration, truncated 3’UTR cyclin D1, and high number of copy number alterations (CNA) (supplementary Figures S4 and S7). Interestingly, analysis of the cyclin D1 signature score as a continuous variable using Cox regression showed a very strong direct correlation between cyclin D1 signature expression levels and the death risk, in both leukemic (HR = 5.51[1.96–15.47]; p=0.0012) and tissue (HR = 4.69[2.60–8.47]; p=2.98×10−7) MCL cohorts (Figure 4A). Accordingly, a high proportion of the 295 cyclin D1-activated genes had a positive correlation with death risk (supplementary Figure S8A). Moreover, the division of MCL patients in two subgroups based on the cyclin D1 signature score distribution (supplementary Figure S8B) showed that patients with high score had a significant shorter OS than patients with low score, in both leukemic (median survival 2.7 vs. 8.7 years; p<0.001) and tissue (median survival 0.8 vs. 4.4 years; p<0.001) samples (Figure 4B). Together, these results demonstrate that increasing expression levels of cyclin D1-dependent program are associated with more aggressive features and shorter survival in MCL patients.
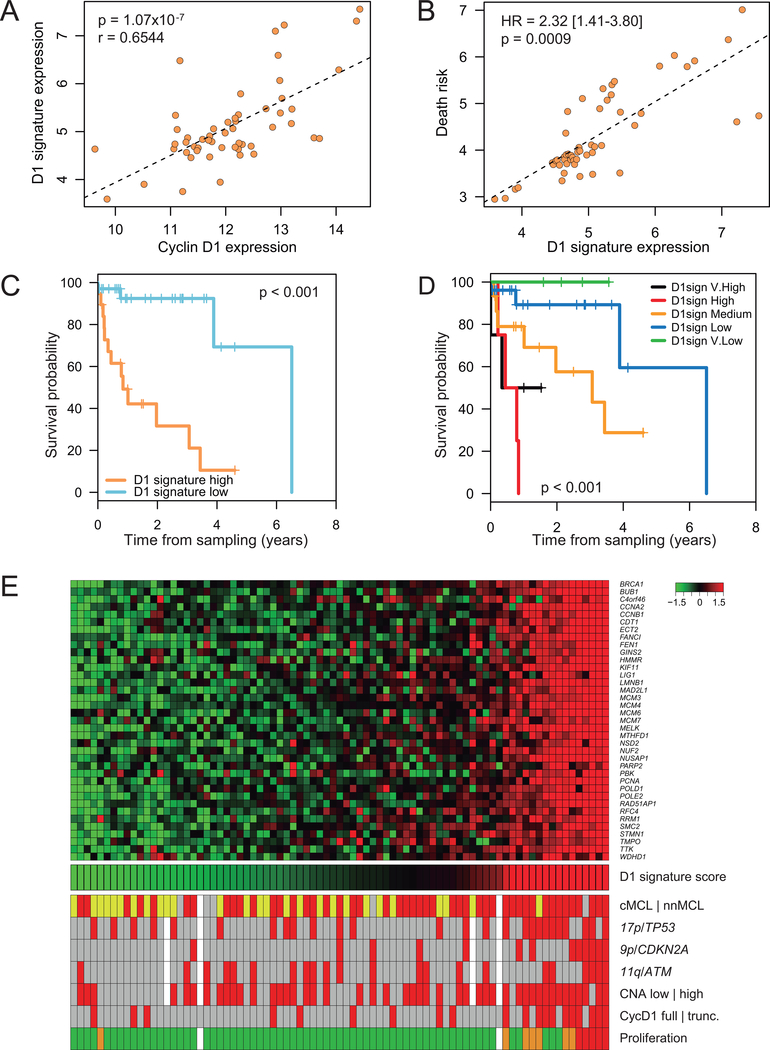
Figure 4: Expression levels of cyclin D1-dependent program correlate with survival in MCL patients.
(A) Association between the 295-gene cyclin D1 signature score and the death risk in MCL primary cases, from both peripheral blood and lymphoid tissue samples. The death risk (y-axis) corresponds to the sum of the martingale residuals and the linear predictors of the fitted OS Cox model; hazard ratios (HR) with 95% confidence interval and p-values are shown. (B) Kaplan-Meier curves of OS from diagnosis date corresponding to 295-gene cyclin D1 signature high and low MCL groups, in peripheral blood (high n = 16; low n = 30) and lymphoid tissue (high n = 40; low n = 52) samples.
Validation of a simplified cyclin D1-dependent gene expression signature
We next wanted to validate the association of the cyclin D1-dependent transcriptional program with clinical outcome using an approach more adaptable to the clinical practice, such as digital gene expression profiling by NanoString technology. We initially applied several filters to reduce the full cyclin D1 program to a 37-gene signature (supplementary Figure S9 and supplementary Methods). For the validation, we focused on MCL blood samples, so that the assay could be applied to all leukemic MCL patients, either with cMCL and nnMCL. We first analyzed the simplified 37-gene signature by NanoString in 28 cases previously evaluated by microarray and we found that it showed a very high correlation with the 295-gene signature (r = 0.9525) (supplementary Figure S10A), confirming the adequacy of this approach. To validate the clinical impact of this simplified cyclin D1 signature, we studied an independent cohort of 53 MCL patients (validation series) together with sequential samples from five patients. The analysis of the sequential samples showed that the cyclin D1 signature levels changed over time (supplementary Figure S10B), and therefore we evaluated the OS from the sampling time. In this validation series we could confirm the previous findings observed with the full cyclin D1-dependent gene program, including the clustering of MCL patients in different expression groups, the positive correlation of this simplified signature with cyclin D1 expression levels, and the association of increasing cyclin D1 signature with adverse prognosis (Figure 5A–C and supplementary Figure S11). Moreover, by dividing the MCL patients into five groups of increasing cyclin D1 signature expression by equal width binning, we found a significantly shorter OS as cyclin D1 signature levels increased (Figure 5D).
Figure 5: Validation of a simplified cyclin D1-dependent gene expression signature.
(A) Correlation between cyclin D1 expression and the 37-gene cyclin D1 signature score in peripheral blood samples from the MCL validation series (n = 53). Statistical significance was assessed by Pearson’s r. (B) Association between the 37-gene cyclin D1 signature score and the death risk in the validation series. The death risk (y-axis) corresponds to the sum of the martingale residuals and the linear predictors of the fitted OS Cox model; HR with 95% confidence interval and p-value are shown. Survival data were calculated from sampling time. (C-D) Kaplan-Meier curves of the OS from sampling time in the validation series. Patients were divided into two groups based on the 37-gene cyclin D1 signature score distribution, leading to cyclin D1 signature high (n = 19) and low (n = 34) groups (C), or in five groups of increasing signature score (D1sign) by equal width binning: very low ([3–4], n = 4); low ([4–5], n = 26); medium ([5–6], n = 15); high ([6–7], n = 4); very high ([7–8], n = 4) (D). (E) Heatmap of the simplified 37-gene cyclin D1 signature in the full set of primary leukemic MCL analyzed by NanoString (n = 81), ordered by cyclin D1 signature score (top panel). MCL patients are shown in columns. Molecular features are shown at the bottom. Patients were classified in cMCL (red), nnMCL (yellow), and undefined (grey) based on the L-MCL16 gene expression signature. 17p/TP53, 9p/CDKN2A, and 11q/ATM genetic alterations are represented in red. Patients with high number (≥5) of CNA are shown in red. Patients with full length and truncated 3’UTR cyclin D1 RNA are represented in grey and red, respectively. MCL proliferation signature classification in low (green), standard (orange), and high (red) is shown. White: data not available.
We further studied the biological and clinical features associated with the cyclin D1 signature in the full set of 81 leukemic MCL analyzed by NanoString (Figure 5E). We found that cMCL had higher expression of cyclin D1 than nnMCL and, concordantly, cyclin D1 signature levels were also higher in cMCL (supplementary Figure S12A). Interestingly, cyclin D1 signature correlated with cyclin D1 expression and with survival in both MCL subtypes independently (supplementary Figure S13). Furthermore, higher levels of both cyclin D1 and cyclin D1 signature were significantly associated with some of the most common genetic alterations in MCL such as aberrations in 17p/TP53 and 9p/CDKN2A, presence of truncated 3’UTR cyclin D1 and high number of CNA (supplementary Figure S12B–F), in line with the observations in the previous MCL microarray series. Finally, patients classified as “high” and “standard” proliferation according to the MCL35 proliferation signature assay defined in tissue samples (4,8), showed higher cyclin D1 signature expression than those classified as “low” proliferation, although only 15% of patients were classified in “high” or “standard” groups (supplementary Figure S14A). Multiple two-variable Cox regression models in the 53 cases from the validation series showed that cyclin D1 signature was a better predictor of survival compared not only with the MCL proliferation signature but also with most of the molecular factors analyzed previously (supplementary Table S5). This analysis also showed that cyclin D1 signature had prognostic value for OS independently of TP53, CDKN2A, and total number of CNA.
To understand the prognostic difference between the cyclin D1 signature and the previously defined MCL proliferation signature (4) in this leukemic MCL cohort, we analyzed the genes from both signatures. While most genes in the proliferation signature belonged to G2/M, the cyclin D1 signature contained a similar proportion of G1/S and G2/M genes (supplementary Figure S14B). Additionally, by evaluating both cyclin D1 and MCL proliferation signatures in a set of blood and tissue samples from the same patients (29), we found that the genes from both signatures were expressed at similar levels in tissue, but the ones from the proliferation signature displayed significantly lower expression than those of the cyclin D1 signature in blood samples (supplementary Figure S14C).
Cyclin D1-dependent transcriptional program in other cyclin D1-overexpressing tumors
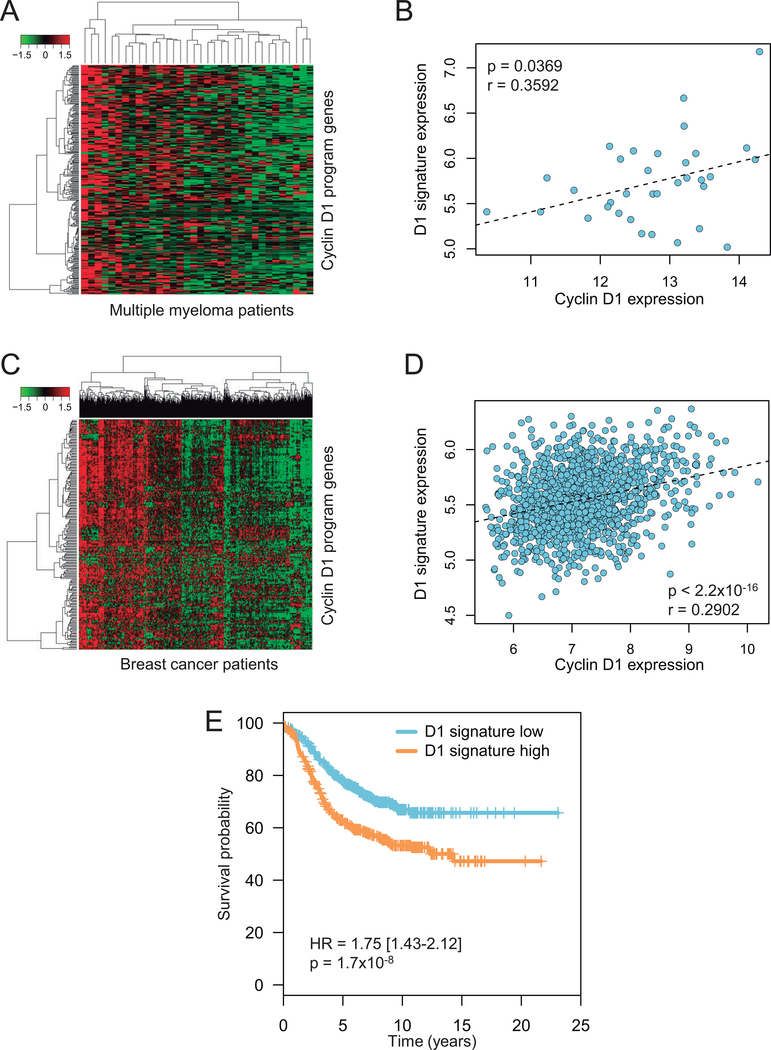
We investigated whether the cyclin D1-dependent transcriptional program identified in MCL could be present in other cyclin D1-overexpressing cancers. We analyzed the gene expression profiling of a multiple myeloma series previously reported (30), focusing on a subgroup characterized by cyclin D1 overexpression. Hierarchical clustering analysis led to the distribution of multiple myeloma patients in groups with different expression levels of the cyclin D1-dependent program (Figure 6A). More importantly, we found a significant positive correlation between cyclin D1 levels and those of the cyclin D1 signature (Figure 6B). We next analyzed a large series of breast cancer patients previously published (31). Since cyclin D1 was shown to play different roles in estrogen receptor (ER)-positive versus ER-negative breast cancers and to be overexpressed mainly in the first (42–44), we analyzed the two groups independently. Hierarchical clustering analysis of the cyclin D1-dependent program in ER-positive breast cancer showed distinct groups characterized by different expression levels (Figure 6C). Remarkably, cyclin D1 signature expression showed a significant positive correlation to cyclin D1 levels in ER-positive but not in ER-negative breast cancer (Figure 6D and supplementary Figure S15A). Concordantly, when splitting the patients by the median cyclin D1 signature level, we found that high expression of cyclin D1 signature was associated with poorer survival in ER-positive but not in ER-negative breast cancer (Figure 6E and supplementary Figure S15B). Together, these data suggest that cyclin D1 overexpression in a subset of multiple myeloma and breast cancer patients may contribute to the upregulation of the specific cyclin D1-dependent transcriptional program identified in MCL.
Figure 6: Cyclin D1-dependent transcriptional program in other cyclin D1-overexpressing tumors.
(A) Heatmap and hierarchical clustering analysis of cyclin D1-dependent gene program in multiple myeloma; only patients from the CD-2 molecular subclass, characterized by a high prevalence of t(11;14) translocation, were selected (n = 34). (B) Correlation between cyclin D1 expression and the 295-gene cyclin D1 signature score in multiple myeloma. Correlation was assessed by Pearson’s r. (C) Heatmap and hierarchical clustering analysis of cyclin D1-dependent gene program in ER-positive breast cancer patients (n = 1399). (D) Correlation between cyclin D1 expression and the 295-gene cyclin D1 signature score in ER-positive breast cancer. Correlation was assessed by Pearson’s r. (E) Kaplan-Meier curves of the progression free survival in ER-positive breast cancer patients splitted in “high” and “low” groups based on the median value of the 37-gene cyclin D1 signature.
Discussion
In this study, we have identified a cyclin D1-dependent transcriptional program in MCL cells composed of 295 genes mainly related to cell cycle regulation. Cyclin D1-dependent program was overexpressed in primary MCL directly proportional to cyclin D1 levels and increased expression of this program was associated with poorer survival. This transcriptional program was also present in multiple myeloma and breast cancer with cyclin D1 overexpression. Our data suggest that transcriptional dysregulation mediated by cyclin D1 overexpression might play an important role in MCL pathogenesis thus impacting on clinical outcome.
The relevance of cyclin D1 overexpression in MCL is stressed by the finding that tumors with higher cyclin D1 levels have increased proliferation and aggressiveness (14,45,46). These observations are concordant with our finding that the cyclin D1-dependent transcriptional program is highly enriched in cell cycle-related genes and high levels of this program are associated with shorter survival of the patients. Interestingly, half of the genes from the previously defined MCL proliferation signature are included in the cyclin D1-dependent program. Therefore, gene activation by cyclin D1 may be, in addition to other common MCL genetic alterations, one of the underlying mechanisms dysregulating MCL proliferation. The association between the cyclin D1 signature and the presence of TP53 and CDKN2A alterations could be the result of a selective pressure to inactivate cell cycle regulatory pathways in cases with high cyclin D1.
Our results suggest that cyclin D1 may facilitate transcriptional activation of cell cycle genes through the binding to their promoters in MCL cells. We cannot rule out that the induction of these genes may also reflect in part the activation of the CDK4/6-pRB pathway mediated by cyclin D1 overexpression that triggers the G1/S phase transition. However, previous genome-wide studies in mouse embryonic fibroblasts and in breast cancer models showed that cyclin D1 binds to the promoter of genes that regulate cell division and activates their expression independent of CDK4, stressing the importance of the transcriptional role of cyclin D1 (36,47). Moreover, the complete inactivation of RB1 by mutations and deletions in some MCLs (48), would support the idea that cyclin D1 may play additional oncogenic roles besides its classical cell cycle function. Similarly to other cellular models (16–18), in MCL cells cyclin D1 might facilitate transcriptional activation through the interaction with transcription factors, including E2F4 and FOXM1. Remarkably, cyclin D1 was previously described to interact with E2F4 and stimulate the expression of E2F motif-containing genes (36–38), and cyclin D1-CDK4 complex was reported to activate FOXM1 thus inducing the expression of cell cycle genes (39,40), in different murine and human models. These two proteins are important regulators of the two transcriptional waves occurring during cell cycle: E2F4 mainly regulates G1/S genes while FOXM1 mostly works in G2/M phase (34). This is consistent with our observation that the cyclin D1-dependent transcriptional program contains genes that belong to the different cell cycle phases. Moreover, we found that cyclin D1 interacted with the coactivator CBP in MCL cells as previously reported in other cellular models (41), reinforcing the idea that cyclin D1 would play a role in transcriptional activation in MCL cells. Overall, our results suggest that cyclin D1-mediated cell cycle activation in MCL would rely not only on its function as a regulator of the G1/S phase transition through CDK4 binding but also in its role facilitating transcriptional activation of G1/S and G2/M cell cycle genes.
The transcriptional role of cyclin D1 in MCL was not addressed until recently when we described that cyclin D1 shows widespread binding to promoters of active genes in MCL cells, inducing a global transcriptional downmodulation (20). However, we also observed that some cyclin D1 target genes were not affected by this effect. Here, we have found that, in parallel to the large-scale transcriptional downregulation, cyclin D1 also promotes the activation of a specific subset of its many targets. We observed that cyclin D1-activated genes had larger cyclin D1 peaks and presented specific DNA motifs compared to other cyclin D1 targets, suggesting that these genes may represent a distinct functional subgroup. This behavior of cyclin D1 is similar to that reported for the oncogene MYC, which works as a global transcriptional amplifier and in parallel activates or represses specific gene sets (49–51). Further studies should clarify in more detail the mechanisms of cyclin D1-mediated transcriptional regulation, not only in lymphomagenesis but also in other cancers.
The fact that a subset of MCL patients, particularly with nnMCL, have only leukemic manifestation of the disease, jeopardize the use of prognostic biomarkers such as the MCL proliferation signature, that is a robust prognostic parameter when measured in nodal samples but has a lower performance in leukemic samples (8). In contrast, the cyclin D1-dependent transcriptional program described here is consistently associated with the survival of the patients in both tissue and leukemic MCL samples. Moreover, our 37-gene cyclin D1 signature assay uses a gene expression platform compatible with clinical setting. The different performance between the proliferation and the cyclin D1 signatures could be due to the fact that the former was developed through the identification of genes associated with survival in MCL nodal samples (4,5), and we have seen here that the expression of these genes is significantly lower in MCL blood samples. Since cyclin D1 signature is highly expressed in both blood and tissue tumor cells, it is likely that it may represent an intrinsic biological feature of MCL cells, independent of microenvironment interactions. Moreover, since it contains genes from both G1/S and G2/M phases it might better capture the proliferation state in both tumor compartments. In any case, the fact that measurement of the cyclin D1-dependent transcriptional program, including the simplified 37-gene signature, could be applied to predict the clinical outcome in both MCL subtypes is relevant and it may help to identify nnMCL patients with adverse clinical outcome similar to cMCL.
The cyclin D1-dependent transcriptional program identified in MCL cells was also observed in specific molecular subsets of multiple myeloma and breast cancer with cyclin D1 overexpression. The moderate correlation observed between the cyclin D1 signature and cyclin D1 levels may reflect that dysregulation of the proliferation genes that belong to the signature could also occur by different oncogenic mechanisms active in these tumors. Concerning multiple myeloma, although cases with cyclin D1 overexpression generally show a more favorable prognosis (52), increased cyclin D1 signature might confer shorter survival in this particular subset of patients as we have observed in MCL. Regarding breast cancer, high cyclin D1 signature was associated with decreased survival in ER-positive but not ER-negative tumors. Accordingly, cyclin D1 overexpression was previously associated with high proliferation and increased risk of mortality exclusively in ER-positive breast cancers (42–44). Further research should clarify to which extent cyclin D1-mediated transcriptional dysregulation contributes to oncogenesis in these and other cyclin D1-overexpressing tumors.
In conclusion, our results suggest that cyclin D1 oncogenic effect in MCL, and possibly in other cancers, is based not only on its canonical cell cycle function but also on its role in transcriptional regulation. We have identified a cyclin D1-dependent transcriptional program that is overexpressed in MCL and can be applied to predict clinical outcome in both MCL subtypes.
Supplementary Material
Translational relevance.
Mantle cell lymphoma (MCL) is a B-cell neoplasm characterized by cyclin D1 overexpression that has two major molecular subtypes. Conventional MCL (cMCL) usually has an aggressive course with patients showing disseminated, predominantly nodal, disease, whereas leukemic nonnodal MCL (nnMCL) subtype often presents indolent clinical evolution with isolated leukemic presentation. Although prognostic factors have been established for cMCL, new biomarkers suitable for both subtypes are needed. In this study, we identified and characterized a cyclin D1-dependent transcriptional program that predicts clinical outcome of MCL patients. We validated a simplified cyclin D1 signature of the program with leukemic samples and a digital gene expression platform adaptable to the clinical practice. The prognostic value of the cyclin D1 signature in blood samples is relevant because it can be applied to both MCL subtypes, and it may be helpful to identify nnMCL patients with adverse prognosis similar to cMCL.
Acknowledgments
This study was supported by Fondo de Investigaciones Sanitarias-Instituto de Salud Carlos III (Grant PI14/00355 and Grant PI19/01838 to P.J.); National Institutes of Health “Molecular Diagnosis, Prognosis, and Therapeutic Targets in Mantle Cell Lymphoma” (Grant P01CA229100 to E.C.); the Spanish Ministerio de Ciencia, Innovación y Universidades (Grant RTI2018-094274-B-I00 to E.C.); Generalitat de Catalunya Suport Grups de Recerca AGAUR (Grant 2017-SGR-1142 to E.C.); FEDER: European Regional Development Fund “Una manera de hacer Europa”; CERCA Programme / Generalitat de Catalunya. S.D. was supported by a Juan de la Cierva fellowship (Spanish Ministerio de Economía y Competitividad). R.A. was supported by a grant of the Leukemia and Lymphoma society. E.C. is an academia researcher of the Institució Catalana de Recerca i Estudis Avançats (ICREA) of the Generalitat de Catalunya. This work was mainly developed at the Centre Esther Koplowitz (CEK), Barcelona, Spain. The authors thank the Hematopathology Collection registered at the Biobank of Hospital Clínic – IDIBAPS for sample procurement. We are indebted to the Genomics core facility of the IDIBAPS and the Genomics Unit of the CRG for technical help. We are grateful to Dr. N. Agell for providing reagents and N. Garcia and S. Ruiz for their technical and logistic assistance.
Financial support: This study was supported by Fondo de Investigaciones Sanitarias-Instituto de Salud Carlos III (Grant PI14/00355 and Grant PI19/01838 to P.J.); National Institutes of Health “Molecular Diagnosis, Prognosis, and Therapeutic Targets in Mantle Cell Lymphoma” (Grant P01CA229100 to E.C.); the Spanish Ministerio de Ciencia, Innovación y Universidades (Grant RTI2018-094274-B-I00 to E.C.); Generalitat de Catalunya Suport Grups de Recerca AGAUR (Grant 2017-SGR-1142 to E.C.); FEDER: European Regional Development Fund “Una manera de hacer Europa”; CERCA Programme / Generalitat de Catalunya.
Disclosure of Potential Conflicts of Interest: E.C., E.S.J, G.O., L.M.S., A.R., D.W.S., and L.M.R. are named inventors on 2 patents filed by the National Cancer Institute: “Methods for selecting and treating lymphoma types” licensed to NanoString Technologies and “Evaluation of mantle cell lymphoma and methods related thereof.” D.W.S has received research support from NanoString Technologies. The remaining authors declare no potential conflicts of interest.
References
- 1.Jares P, Colomer D, Campo E. Molecular pathogenesis of mantle cell lymphoma. J Clin Invest. 2012;122:3416–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bosch F, Jares P, Campo E, Lopez-Guillermo A, Piris MA, Villamor N, et al. PRAD-1/cyclin D1 gene overexpression in chronic lymphoproliferative disorders: a highly specific marker of mantle cell lymphoma. Blood. 1994;84:2726–32. [PubMed] [Google Scholar]
- 3.Seto M, Yamamoto K, Iida S, Akao Y, Utsumi KR, Kubonishi I, et al. Gene rearrangement and overexpression of PRAD1 in lymphoid malignancy with t(11;14)(q13;q32) translocation. Oncogene. 1992;7:1401–6. [PubMed] [Google Scholar]
- 4.Scott DW, Abrisqueta P, Wright GW, Slack GW, Mottok A, Villa D, et al. New Molecular Assay for the Proliferation Signature in Mantle Cell Lymphoma Applicable to Formalin-Fixed Paraffin-Embedded Biopsies. J Clin Oncol. 2017;35:1668–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rosenwald A, Wright G, Wiestner A, Chan WC, Connors JM, Campo E, et al. The proliferation gene expression signature is a quantitative integrator of oncogenic events that predicts survival in mantle cell lymphoma. Cancer Cell. 2003;3:185–97. [DOI] [PubMed] [Google Scholar]
- 6.Katzenberger T, Petzoldt C, Höller S, Mäder U, Kalla J, Adam P, et al. Mantle Cell Lymphoma: A Clinicopathologic Study of 80 Cases. Blood. 2006;89:2067–78. [PubMed] [Google Scholar]
- 7.Swerdlow SH, Campo E, Pileri SA, Harris NL, Stein H, Siebert R, et al. The 2016 revision of the World Health Organization classification of lymphoid neoplasms. Blood. 2016;127:2375–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Clot G, Jares P, Giné E, Navarro A, Royo C, Pinyol M, et al. A gene signature that distinguishes conventional and leukemic nonnodal mantle cell lymphoma helps predict outcome. Blood. 2018;132:413–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Fernàndez V, Salamero O, Espinet B, Solé F, Royo C, Navarro A, et al. Genomic and gene expression profiling defines indolent forms of mantle cell lymphoma. Cancer Res. 2010;70:1408–18. [DOI] [PubMed] [Google Scholar]
- 10.Beà S, Salaverria I, Armengol L, Pinyol M, Fernández V, Hartmann EM, et al. Uniparental disomies, homozygous deletions, amplifications, and target genes in mantle cell lymphoma revealed by integrative high-resolution whole-genome profiling. Blood. 2009;113:3059–69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gruszka-Westwood AM, Atkinson S, Summersgill BM, Shipley J, Elnenaei MO, Jain P, et al. Unusual case of leukemic mantle cell lymphoma with amplified CCND1/IGH fusion gene. Genes, Chromosom Cancer. 2002;33:206–12. [DOI] [PubMed] [Google Scholar]
- 12.Mohanty A, Sandoval N, Das M, Pillai R, Chen L, Chen RW, et al. CCND1 mutations increase protein stability and promote ibrutinib resistance in mantle cell lymphoma. Oncotarget. 2016;7:73558–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Beà S, Valdés-Mas R, Navarro A, Salaverria I, Martín-Garcia D, Jares P, et al. Landscape of somatic mutations and clonal evolution in mantle cell lymphoma. Proc Natl Acad Sci U S A. 2013;110:18250–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wiestner A, Tehrani M, Chiorazzi M, Wright G, Gibellini F, Nakayama K, et al. Point mutations and genomic deletions in CCND1 create stable truncated cyclin D1 mRNAs that are associated with increased proliferation rate and shorter survival. Blood. 2007;109:4599–606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Musgrove EA, Caldon CE, Barraclough J, Stone A, Sutherland RL. Cyclin D as a therapeutic target in cancer. Nat Rev Cancer. 2011;11:558–72. [DOI] [PubMed] [Google Scholar]
- 16.Pestell RG. New roles of cyclin D1. Am J Pathol. 2013;183:3–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Coqueret O Linking cyclins to transcriptional control. Gene. 2002;299:35–55. [DOI] [PubMed] [Google Scholar]
- 18.Zwijsen RML, Wientjens E, Klompmaker R, Van der Sman J, Bernards R, Michalides RJAM. CDK-independent activation of estrogen receptor by cyclin D1. Cell. 1997;88:405–15. [DOI] [PubMed] [Google Scholar]
- 19.Reutens AT, Fu M, Wang C, Albanese C, McPhaul MJ, Sun Z, et al. Cyclin D1 Binds the Androgen Receptor and Regulates Hormone-Dependent Signaling in a p300/CBP-Associated Factor (P/CAF)-Dependent Manner. Mol Endocrinol. 2014;15:797–811. [DOI] [PubMed] [Google Scholar]
- 20.Albero R, Enjuanes A, Demajo S, Castellano G, Pinyol M, García N, et al. Cyclin D1 overexpression induces global transcriptional downregulation in lymphoid neoplasms. J Clin Invest. 2018;128:4132–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Demajo S, Uribesalgo I, Gutiérrez A, Ballaré C, Capdevila S, Roth M, et al. ZRF1 controls the retinoic acid pathway and regulates leukemogenic potential in acute myeloid leukemia. Oncogene. 2014;33:5501–10. [DOI] [PubMed] [Google Scholar]
- 22.Navarro A, Clot G, Martínez-Trillos A, Pinyol M, Jares P, González-Farré B, et al. Improved classification of leukemic B-cell lymphoproliferative disorders using a transcriptional and genetic classifier. Haematologica. 2017;102:e360–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Nadeu F, Martin-Garcia D, Clot G, Díaz-Navarro A, Duran-Ferrer M, Navarro A, et al. Genomic and epigenomic insights into the origin, pathogenesis, and clinical behavior of mantle cell lymphoma subtypes. Blood. 2020;136:1419–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Navarro A, Clot G, Royo C, Jares P, Hadzidimitriou A, Agathangelidis A, et al. Molecular subsets of mantle cell lymphoma defined by the IGHV mutational status and SOX11 expression have distinct biologic and clinical features. Cancer Res. 2012;72:5307–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Greiner TC, Dasgupta C, Ho VV, Weisenburger DD, Smith LM, Lynch JC, et al. Mutation and genomic deletion status of ataxia telangiectasia mutated (ATM) and p53 confer specific gene expression profiles in mantle cell lymphoma. Proc Natl Acad Sci U S A. 2006;103:2352–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hartmann EM, Campo E, Wright G, Lenz G, Salaverria I, Jares P, et al. Pathway discovery in mantle cell lymphoma by integrated analysis of high-resolution gene expression and copy number profiling. Blood. 2010;116:953–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Brune V, Tiacci E, Pfeil I, Döring C, Eckerle S, van Noesel CJM, et al. Origin and pathogenesis of nodular lymphocyte–predominant Hodgkin lymphoma as revealed by global gene expression analysis. J Exp Med. 2008;205:2251–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Roth RB, Hevezi P, Lee J, Willhite D, Lechner SM, Foster AC, et al. Gene expression analyses reveal molecular relationships among 20 regions of the human CNS. Neurogenetics. 2006;7:67–80. [DOI] [PubMed] [Google Scholar]
- 29.Saba NS, Liu D, Herman SEM, Underbayev C, Tian X, Behrend D, et al. Pathogenic role of B-cell receptor signaling and canonical NF-κB activation in mantle cell lymphoma. Blood. 2016;128:82–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Broyl A, Hose D, Lokhorst H, de Knegt Y, Peeters J, Jauch A, et al. Gene expression profiling for molecular classification of multiple myeloma in newly diagnosed patients. Blood. 2010;116:2543–53. [DOI] [PubMed] [Google Scholar]
- 31.Györffy B, Lanczky A, Eklund AC, Denkert C, Budczies J, Li Q, et al. An online survival analysis tool to rapidly assess the effect of 22,277 genes on breast cancer prognosis using microarray data of 1,809 patients. Breast Cancer Res Treat. 2010;123:725–31. [DOI] [PubMed] [Google Scholar]
- 32.McCall MN, Bolstad BM, Irizarry RA. Frozen robust multiarray analysis (fRMA). Biostatistics. 2010;11:242–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Smyth GK. Linear Models and Empirical Bayes Methods for Assessing Differential Expression in Microarray Experiments. Stat Appl Genet Mol Biol. 2004;3:1–25. [DOI] [PubMed] [Google Scholar]
- 34.Fischer M, Müller GA. Cell cycle transcription control: DREAM/MuvB and RB-E2F complexes. Crit Rev Biochem Mol Biol. 2017;52:638–62. [DOI] [PubMed] [Google Scholar]
- 35.Dunham I, Kundaje A, Aldred SF, Collins PJ, Davis CA, Doyle F, et al. An integrated encyclopedia of DNA elements in the human genome. Nature. 2012;489:57–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Casimiro MC, Crosariol M, Loro E, Ertel A, Yu Z, Dampier W, et al. ChIP sequencing of cyclin D1 reveals a transcriptional role in chromosomal instability in mice. J Clin Invest. 2012;122:833–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Pauklin S, Madrigal P, Bertero A, Vallier L. Initiation of stem cell differentiation involves cell cycle-dependent regulation of developmental genes by Cyclin D. Genes Dev. 2016;30:421–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Scimè A, Li L, Ciavarra G, Whyte P. Cyclin D1/cdk4 can interact with E2F4/DP1 and disrupts its DNA-binding capacity. J Cell Physiol. 2008;214:568–81. [DOI] [PubMed] [Google Scholar]
- 39.Anders L, Ke N, Hydbring P, Choi YJ, Widlund HR, Chick JM, et al. A systematic screen for CDK4/6 substrates links FOXM1 phosphorylation to senescence suppression in cancer cells. Cancer Cell. 2011;20:620–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Wierstra I, Alves J. Transcription factor FOXM1c is repressed by RB and activated by cyclin D1/Cdk4. Biol Chem. 2006;387:949–62. [DOI] [PubMed] [Google Scholar]
- 41.Bienvenu F, Jirawatnotai S, Elias JE, Meyer CA, Mizeracka K, Marson A, et al. Transcriptional role of cyclin D1 in development revealed by a genetic-proteomic screen. Nature. 2010;463:374–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Arnold A, Papanikolaou A. Cyclin D1 in breast cancer pathogenesis. J Clin Oncol. 2005;23:4215–24. [DOI] [PubMed] [Google Scholar]
- 43.Lamb R, Lehn S, Rogerson L, Clarke RB, Landberg G. Cell cycle regulators cyclin D1 and CDK4/6 have estrogen receptor-dependent divergent functions in breast cancer migration and stem cell-like activity. Cell Cycle. 2013;12:2384–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Ahlin C, Lundgren C, Embretsén-Varro E, Jirström K, Blomqvist C, Fjällskog ML. High expression of cyclin D1 is associated to high proliferation rate and increased risk of mortality in women with ER-positive but not in ER-negative breast cancers. Breast Cancer Res Treat. 2017;164:667–78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Kimura Y, Sato K, Arakawa F, Karube K, Nomura Y, Shimizu K, et al. Mantle cell lymphoma shows three morphological evolutions of classical, intermediate, and aggressive forms, which occur in parallel with increased labeling index of cyclin D1 and Ki-67. Cancer Sci. 2010;101:806–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Shakir R, Ngo N, Naresh KN. Correlation of cyclin D1 transcript levels, transcript type and protein expression with proliferation and histology among mantle cell lymphoma. J Clin Pathol. 2008;61:920–7. [DOI] [PubMed] [Google Scholar]
- 47.Casimiro MC, Di Sante G, Crosariol M, Loro E, Dampier W, Ertel A, et al. Kinase-independent role of cyclin D1 in chromosomal instability and mammary tumorigenesis. Oncotarget. 2015;6:8525–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Pinyol M, Bea S, Plà L, Ribrag V, Bosq J, Rosenwald A, et al. Inactivation of RB1 in mantle-cell lymphoma detected by nonsense-mediated mRNA decay pathway inhibition and microarray analysis. Blood. 2007;109:5422–9. [DOI] [PubMed] [Google Scholar]
- 49.Nie Z, Hu G, Wei G, Cui K, Yamane A, Resch W, et al. c-Myc is a universal amplifier of expressed genes in lymphocytes and embryonic stem cells. Cell. 2012;151:68–79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Lin CY, Lovén J, Rahl PB, Paranal RM, Burge CB, Bradner JE, et al. Transcriptional amplification in tumor cells with elevated c-Myc. Cell. 2012;151:56–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Sabò A, Kress TR, Pelizzola M, de Pretis S, Gorski MM, Tesi A, et al. Selective transcriptional regulation by Myc in cellular growth control and lymphomagenesis. Nature. 2014;511:488–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Bergsagel PL, Kuehl WM. Molecular pathogenesis and a consequent classification of multiple myeloma. J Clin Oncol. 2005;23:6333–8. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.