Abstract
Introduction:
Vitamin D has been shown to play a vital role in bone mineral homeostasis by stimulating the intestinal absorption of calcium and phosphate. The critical role of Vitamin D in bone metabolism triggered the need to evaluate the effect of Vitamin D deficiency and hence replacement of the same on osseointegration of dental implants. This prospective study evaluated the crestal bone level in patients having low level of Vitamin D treated with dental implant with or without Vitamin D3 supplements.
Materials and Methods:
A prospective clinical study was conducted on 32 patients based on the inclusion and exclusion criteria. Patients were divided into two groups on the basis of Vitamin D level < 30 ng/ml (Group I: patients receiving Vitamin D3 supplements, i.e., cholecalciferol 1 g sachet 60,000 IU/month) or <30 ng/ml (Group II: not receiving Vitamin D3 supplements). The crestal bone level measurements were made with the help of Digimizer Image Analysis, MedCalc software.
Results:
All implants showed clinically acceptable crestal bone level at interval of 1 week (baseline), 3 months, and 6 months. There was a statistically nonsignificant difference seen for the values between the groups (P > 0.05) for all other values at various time intervals. However, there was a statistically significant/highly significant difference seen for the values between the groups (P < 0.01, 0.05) for 3 months distal with higher values for Group I as compared to Group II.
Conclusion:
From the study, it can be concluded that cholecalciferol has systemic effects on accelerating bone formation around titanium implant.
Keywords: Cholecalciferol, MedCalc software, osseointegration, Vitamin D
INTRODUCTION
Tooth loss is a common phenomenon and can occur because of trauma, caries, or periodontal disease. Dental implants are now a reliable solution for the functional and esthetic rehabilitation of partially and completely edentulous patients.[1,2,3]
Factors improving osseointegration consist of implant-related factors, use of adjuvant treatment methods such as bone grafting, osteogenic biological coatings, and biophysical stimulation as well as pharmacological agents.[4] Supplementation with cholecalciferol (Vitamin D3) is reported to show favorable impacts on bone mineral density.[5,6]
Vitamin D is a fat-soluble biomolecule, which is obtained through Vitamin D-rich diet or is generated in the skin on ultraviolet light exposure.[6,7,8] Vitamin D-binding protein is responsible for transporting Vitamin D from the skin or intestine to the liver, where it is metabolized and yields 25-hydroxyvitamin D, or 25(OH)2D. Next, 25(OH)2D will produce the active form of Vitamin D in the kidneys: 1,25-dihydroxyvitamin D, also known as 1,25(OH)2D or calcitriol, which is responsible for binding to Vitamin D receptor (VDR).[9] The VDR is a ligand-dependent transcription factor of the nuclear receptor superfamily. VDR belongs to the NR1I subfamily along with other nuclear receptors involved in xenobiotic metabolism, such as pregnane X receptor.[10]
Vitamin D deficiency has become increasingly common and can result from inadequate dietary intake together with insufficient exposure to sunlight.[11] Vitamin D has been shown to play a vital role in bone mineral homeostasis12 by stimulating intestinal absorption of calcium and phosphate.
Serum levels of Vitamin D in the 25(OH) D form are the most accurate way of determining Vitamin D status: A patient with <10 ng/mL is considered to be Vitamin D deficient; one with 10–30 ng/mL is considered to have low levels of Vitamin D. The optimal blood level of Vitamin D is a value >30 ng/mL.[13]
Vitamin D deficiency likewise negatively influences bone regeneration, including fracture healing[14] and also osseointegration of implants.[15] A genome-wide screening additionally suggested that Vitamin D deficiency influences the osseointegration of dental implants by regulating the circadian rhythm system and the cartilage extracellular matrix.[16] Hence, Vitamin D supplementation is an effective treatment for reduced peri-implant bone formation because it directly counteracts the catabolic mechanisms of Vitamin D deficiency.[17] Hence, the aim of our study was to evaluate the crestal bone level in patients having low Vitamin D level treated with dental implant with or without Vitamin D3 supplements.
MATERIALS AND METHODS
A prospective, randomized clinical trial was conducted involving total of 32 patients aged between 20 and 40 years. The patients were assessed based on chief complaints needing replacement of missing mandibular posterior teeth. Ethical clearance no. PGIDS/IEC/17/13 was obtained from the Institutional Ethical Committee of PGIDS, Rohtak. After explaining the proposed study criteria including alternative treatment options, potential risks, and benefits, a signed informed consent was obtained from all patients.
Inclusion criteria
Patients who consented to participate in the study and will also be available for follow-up
Patients with maintainable oral hygiene and nonsmokers
Patients having adequate quality and quantity of bone at the placement site
Patients who were having Vitamin D level <30 ng/ml.
Exclusion criteria
Patients with the presence of infection around site of implant placement
Patients with a history of bleeding disorder or on anticoagulant drugs
Patients with immunocompromised state or debilitating disease and recent history of myocardial infarction
Patients on Vitamin D3 supplements.
Grouping of subjects
A total of 32 implants were placed (16 implants in Group I and 16 implants in Group II) in patients requiring restoration of mandibular posterior teeth. Patients were divided into the following groups on the basis of Vitamin D level.
Group I: Patients having Vitamin D <30 ng/ml, treated with dental implant and received Vitamin D3 supplements (cholecalciferol sachet 60000 IU/month) for 3 months and continued for 6 months depending on level of Vitamin D
Group II: Patients having Vitamin D <30 ng/ml, treated with dental implant and not received Vitamin D3 supplements.
Pre-surgical assessment
An informed consent was obtained and history was recorded
Preoperative radiographic assessment: Intraoral periapical (IOPA) X-ray and orthopantomograph were done for the evaluation of bone
Investigations such as complete hemogram (Hb, bleeding time, and closure time) and all vitals were recorded (blood pressure, pulse, and heart rate) to evaluate patient's fitness for implant placement
Clinical photographs were taken.
Estimation of Vitamin D levels
Sample collection
Five milliliters of blood sample was collected in a sterile plain vacutainer under all aseptic conditions from all the patients at the time of diagnosis. Blood samples were processed and serum was separated by centrifugation at 2000 rpm ×10 min after clotting. Samples were stored at −20°C in separate aliquots for estimation of Vitamin D in batches subsequently. The subsequent blood samples were taken at 3-month and 6-month follow-up period from Group I patients receiving Vitamin D supplements.
Method
Serum 25OH Vitamin D was estimated by radioimmunoassay (RIA) method on fully automated RIA Analyzer SR300 by STRATEC Biomedical AG, Germany, using Beckman Coulter 25OH Vitamin D total RIA kit.
Implant surgery planning and procedure
Diagnostic records
The diagnostic impression was made and diagnostic cast was prepared and mounted on mean value articulator.
Intraoral periapical radiograph
This involved:
Fabrication of the vinyl polysiloxane putty jig
A vinyl polysiloxane putty jig was made to standardize the radiographic film holder (Rinn XCP) for each and every patient in terms of angulation and also position of the film relative to the X-ray beam. Vinyl polysiloxane putty was mixed and attached to bite plane of the film holder. The film holder was placed into the patient's mouth at a proper angulation, and the patient was instructed to bite on putty to obtain the indentation of maxillary teeth. The periapical radiographs were taken using the long-cone paralleling technique with radiographic film holders (Rinn XCP) making the use of customized putty. The occlusal jig was stored separately for each patient and used for taking radiographs at subsequent visits.
Surgical procedures
Implants were placed in a conventional manner under aseptic conditions.
Postoperative instructions were provided to the patient regarding diet, oro-dental hygiene and medications, which were prescribed.
Patients were recalled after 24 h for review and after 7 days for suture removal and radiographic and crestal bone level evaluation at baseline, 3 months, and 6 months postoperatively.
Radiographic evaluation of crestal bone level
All implants were evaluated radiographically at baseline (within 1 week after implant placement), 3 months, and 6 months after implant placement [Figures 1-6].
Figure 1.
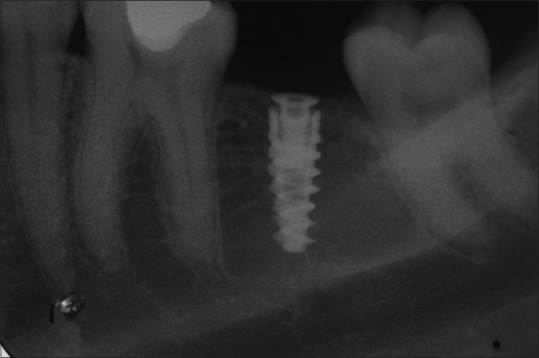
Intraoral periapical 1 week after implant placement (Group I)
Figure 6.
Intraoral periapical 6 months after implant placement (Group II)
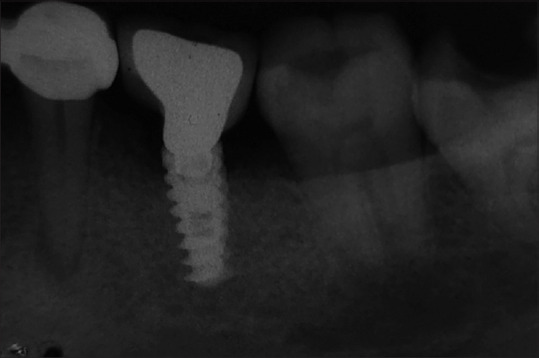
Figure 2.

Intraoral periapical 3 months after implant placement (Group I)
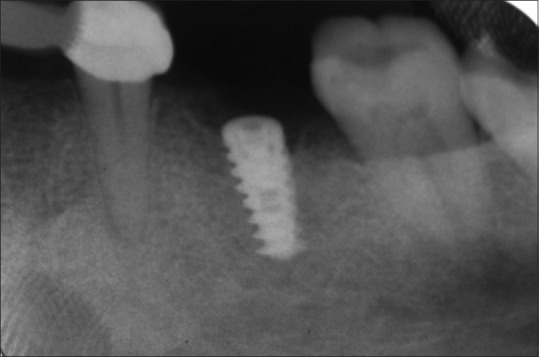
Figure 3.

Intraoral periapical 6 months after implant placement (Group I)
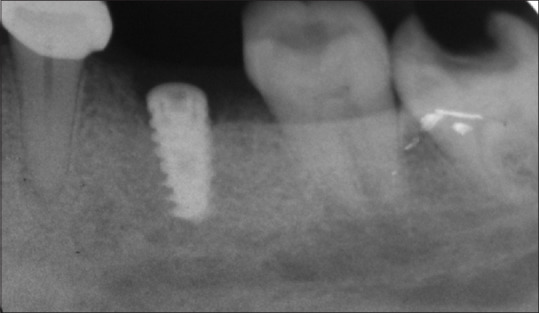
Figure 4.
Intraoral periapical 1 week after implant placement (Group II)
Figure 5.
Intraoral periapical 3 months after implant placement (Group II)
The intraoral periapical radiographs were obtained using a paralleling technique and were digitalized. The first thread of implant was taken as a reference line because it was static, permanently visible, and easy to locate on all radiographs. The point of bone-to-dental implant contact was selected as the bone level. The measurements were obtained using Digimizer Image Analysis, Medcalc software, version 4.3.5.0( Medcalc software Ltd, Ostend, Belgium). Before analysis, the images were calibrated geometrically to record the radiographic dental implant length. Measurements were made at baseline, 3 months, and 6 months at the mesial and distal aspects of implants by dropping perpendiculars from the reference line to the bone level.
Statistical procedures
Information obtained was compiled on a MS Office Excel Sheet (v 2010, Microsoft Redmond Campus, Redmond, Washington, United States).
Data went through statistical analysis utilizing the Statistical Package for the Social Sciences (SPSS v 21.0, SPSS Inc. Chicago, Illinois, U.S.A).
Descriptive statistics such as frequencies and percentage for categorical data and mean and standard deviation for numerical data have been depicted.
Normality of numerical data was checked using Kolmogorov–Smirnov and Shapiro–Wilk tests and was found that the data did not follow a normal curve; hence, nonparametric tests have been used for comparisons.
Intergroup comparison (two groups) was done using Mann–Whitney U-test
Intragroup comparison was done using Friedman's test (for >2 observations), followed by pairwise comparison using Wilcoxon signed-rank test.
For all the statistical tests, P < 0.05 was considered to be statistically significant, keeping α error at 5% and β error at 20%, thus giving a power to the study as 80%.
The results of our study showed that there was a statistically significant/highly significant difference seen for the values between the groups (P < 0.01, 0.05) for 3 months distal with higher values for group I as compared to group II [Graph 2]. While there was a statistically non-significant difference seen for the values between the groups (P > 0.05) for all other values at various time intervals [Graphs 1 and 2].
Graph 2.
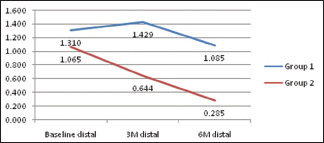
Intergroup comparison of distal bone level at various time intervals
Graph 1.
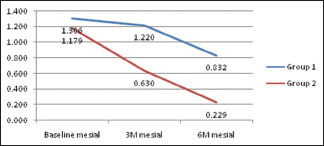
Intergroup comparison of mesial bone level at various time intervals
DISCUSSION
Dental implant has become a treatment of choice in most of the situations of missing teeth. To be specific, failure to osseointegrate and peri-implantitis are the most frequent causes of early implant failure.[3,18,19] To date, only a few clinical studies in the dental literature have investigated the effects of Vitamin D deficiency on osseointegration and on bone regeneration.[7,20,21] Most of these are experimental animal studies, and only a few of them are clinical research in humans.
Vitamin D plays a fundamental role in bone metabolism.[13,18] It regulates calcium and phosphate homeostasis in the tissues, and it is a fundamental element in the mineralization of bones and teeth.[13,18] In dental implantology, Vitamin D has actually been investigated nearly exclusively as an influencing factor of the BIC (bone-to-implant contact) and implant stability.[22] Vitamin D demonstrates several effects on bone metabolism: It upregulates the gene expression of osteocalcin, osteopontin, and 24-hydroxylase, increases extracellular matrix protein formation by osteoblasts, and stimulates osteoclast activity.[20]
The long-term survival of implants is assessed by the amount of marginal bone loss around the dental implant. The quantity of bone loss anticipated from dental implant during the 1st year must be <2 mm, apical to implant-abutment junction. After the 1st year, it is expected that bone loss will be 0.2 mm annually.[23] Hence, our study aimed to evaluate the crestal bone level in patients having low and normal levels of Vitamin D treated with dental implant with or without Vitamin D supplements. Follow-up period was of 6 months.
Table 1 shows the crestal bone level (mm) on mesial and distal sides of dental implant utilizing IOPA radiograph at baseline, at 3 months, and 6 months after implant placement in Group I. Table 2 shows the crestal bone level (mm) on mesial and distal sides of dental implant utilizing IOPA radiograph at baseline, at 3 months, and 6 months after implant placement in Group II. Table 3 shows the mean percentage difference between both the groups.
Table 1.
Measurements of crestal bone level (in mm) on mesial and distal sides of implant in Group I
| S.No. | Baseline | 3 month | 3 month | |||
|---|---|---|---|---|---|---|
| Mesial | Distal | Mesial | Distal | Mesial | Distal | |
| 1. | 1.07 | 0.623 | 1.553 | 1.339 | 1.358 | 0 |
| 2. | 1.622 | 2.189 | 1.888 | 2.579 | 1.422 | 2.064 |
| 3. | 1.569 | 1.366 | 1.222 | 0.698 | 1.814 | 1.256 |
| 4. | 1.009 | 1.021 | 0.789 | 0.868 | 1.331 | 1.409 |
| 5. | 0.953 | 1.053 | 0.789 | 1.213 | 1.724 | 1.149 |
| 6. | 0.9 | 0.876 | 1.333 | 1.63 | 1.077 | 1.928 |
| 7. | 1.495 | 1.762 | 2.138 | 2.614 | 0 | 0.215 |
| 8. | 1.197 | 0.884 | 0.892 | 0.701 | 1.015 | 0.95 |
| 9. | 3.727 | 3.408 | 3.249 | 2.999 | 2.396 | 2.675 |
| 10. | 0.481 | 0 | 1.791 | 1.271 | 0.855 | 1.006 |
| 11. | 0.725 | 1.245 | 0.894 | 1.947 | 0.95 | 1.23 |
| 12. | 2.885 | 2.885 | 1.734 | 1.8 | 1.548 | 1.481 |
| 13. | 1.047 | 0 | 1.007 | 0 | 1.05 | 0.051 |
| 14. | 1.055 | 1.055 | 0.987 | 0.88 | 1.092 | 1.058 |
| 15. | 1.147 | 1.095 | -1.108 | 1.034 | -0.475 | 0.238 |
| 16. | 0 | 1.16 | 0.849 | 1.12 | -1.679 | 0.845 |
Table 2.
Measurements of crestal bone level (in mm) on mesial and distal sides of implant in Group II
| S.No. | Baseline | 3 month | 6 month | |||
|---|---|---|---|---|---|---|
| Mesial | Distal | Mesial | Distal | Mesial | Distal | |
| 1. | 1.859 | 0.165 | 1.478 | 0 | 0 | -0.529 |
| 2. | 0 | -0.882 | 0 | 0 | 0 | 0.325 |
| 3. | 0 | -0.514 | -1.637 | -0.98 | -0.773 | -0.822 |
| 4. | 1.207 | 1.169 | 0.959 | 0.532 | -0.7 | 0.6 |
| 5. | 0.894 | 1.022 | 1.081 | 1.032 | 1.676 | 0.905 |
| 6. | 1.282 | 1.165 | 0.938 | 1.536 | -1.438 | -1.741 |
| 7. | 0.969 | 1.099 | 0.881 | 0 | 0.761 | 1.012 |
| 8. | 0 | 0.961 | 0 | 0.961 | 0 | 0.815 |
| 9. | 2.004 | 1.728 | 1.617 | 1.671 | 1.524 | 1.631 |
| 10. | 1.111 | 1.304 | 0 | 0.582 | -0.767 | 0 |
| 11. | 1.987 | 2.5 | 1.852 | 2.1 | 1.95 | 2.012 |
| 12. | 1.458 | 1.185 | 0 | -0.678 | -0.12 | -0.57 |
| 13. | 2.767 | 2.57 | 2.127 | 2.061 | 1.39 | 1.341 |
| 14. | 1.453 | 1.13 | -0.772 | -0.647 | -1.18 | -2.491 |
| 15. | 1.256 | 1.491 | 1.005 | 1.571 | 0.888 | 1.571 |
| 16. | 0.617 | 0.947 | 0.558 | 0.558 | 0.452 | 0.497 |
Table 3.
Mean percentage difference between groups
| Group I | |||
|---|---|---|---|
| B to 3M Mesial | B to 6M Mesial | 3M to 6M Mesial | |
| Mesial | 6.9230 | 36.15 | 31.40 |
| B to 3M Distal | B to 6M Distal | 3M to 6M Distal | |
| Distal | 8.45 | 16.92 | 23.94 |
| Group II | |||
| B to 3M Mesial | B to 6M Mesial | 3M to 6M Mesial | |
| Mesial | 46.15 | 81.19 | 65.07 |
| B to 3M Distal | B to 6M Distal | 3M to 6M Distal | |
| Distal | 39.33 | 73.58 | 56.25 |
Graph 1 shows a comparison of bone level on mesial aspect of implant between Groups I and II at different time intervals. Graph 2 shows a comparison of bone level on distal aspect of implant between Groups I and II at different time intervals.
In the present study, we evaluated the mesial and distal crestal bone levels in patients of both the groups. It was observed that there is definitely better osseointegration of implants in patients supplemented with Vitamin D. There was lesser bone loss in patients with low Vitamin D level who were supplemented with Vitamin D. This can be attributed to role of Vitamin D in induction of anti-inflammatory cytokines and a reduction in level of pro-inflammatory cytokines, thus decreasing the body's response to surgical intervention. Calcitriol plays a immunomodulatory role stimulating both the acquired and innate responses.[24]
There was an increase in serum Vitamin D levels (up to 45 ng/ml) in Group I patients who were supplemented with Vitamin D. The normal range of Vitamin D level is 30–100 ng/ml. The second reason is role of Vitamin D in calcium metabolism because Vitamin D supplementation may increase calcium availability, which may promote the mineralization at the rate at which new bone is mineralized.[25] Furthermore, Vitamin D is known to stimulate osteocalcin and alkaline phosphatase production in the osteoblasts which may counteract the effect of lowering turnover.[25]
The results of our study are in accordance with a study conducted by Javed et al., who concluded that Vitamin D supplementation could stimulate bone formation and, as a result, augment the contact between the surface of titanium implants and bone.[22] Similar results were reported by Zhou et al., who found an increase in osseointegration in osteoporotic rats given Vitamin D supplements,[26] and Wu et al., who demonstrated an increase in the percentage of contact between bone and implant in diabetic rats given Vitamin D supplements.[27] The results of these studies also support our study because Vitamin D activates osteoblasts and increases the production of extracellular matrix proteins by osteoblasts.
In the present study, the difference in mesial and distal crestal bone levels between various time intervals was found to be nonsignificant in Group I [Graphs 1 and 2]. This is because of Vitamin D supplementation that crestal bone loss was less. However, there was a statistically significant difference seen in Group II for values between all the time pairs (P < 0.01,0.05) except 3 months to 6 months distal where there was nonsignificant difference seen (P > 0.05) [Graphs 1 and 2]. This is attributed to the crestal bone loss which occurs during the 1st year after implant placement. There is nonsignificant difference from 3 months to 6 months because, after loading of implant, remodeling of bone occurs which maintains the crestal bone levels.
Finally, Gaber et al.[28] evaluated the effect of cholecalciferol on dental implant osseointegration in dogs. They concluded that Vitamin D3 had systemic effects on increasing bone formation around dental titanium implant. This also supports our study that Vitamin D supplementation promotes the osseointegration of implants.
Vitamin D3 has been extensively studied for its dual action of promoting bone remodeling.[27] Supplementation is an effective means of improving Vitamin D status.[29] As osseointegration of dental implants also relies on bone metabolism, there is the possibility that decreased blood levels of Vitamin D can negatively influence healing processes and new bone formation on the implant surface.[30]
Vitamin D insufficiency might similarly reduce bone remodeling activities around dental implants and potentially extend the healing time for osseointegration to occur.[31] Hence, based on the results of our study, we can conclude that the establishment of osseointegration during early periods may require Vitamin D-dependent regulatory mechanisms.
Hence, within the results of our study, we can conclude that Vitamin D supplementation is an effective approach to improve the osseointegration of dental implants.
The merits of study are:
This is a prospective study design
Only same type of Vitamin D supplement (cholecalciferol 60000 IU 1 g sachet) was given to all patients in the study group
Optimization of Vitamin D status may also have additional general health benefits
Since half-life of 25(OH)D is a month or longer, so daily dosing is not necessary
IOPA X-rays were obtained using paralleling technique to minimize distortion
A single implant system was used throughout the study
In the present study, all patients participated until the end of the study.
Limitations of our study
The limitations were small sample size and brief follow-up time period.
CONCLUSION
The connection between serum levels of Vitamin D and osseointegration of dental implants has been evaluated in very few studies, the majority of them in animals.
In the present study, it was observed that there is definitely much better osseointegration of implants in individuals supplemented with Vitamin D. In cases where a link between reduced serum levels of Vitamin D and enhanced risk of dental implant failure is shown, the clinician may provide a dose of Vitamin D in the weeks before surgery. By doing this way, the clinician might regulate the serum levels and help enhance the healing process.
Obviously, even more prospective clinical research studies as well as randomized controlled trials are needed to show a significant correlation between decreased serum levels of Vitamin D and increased risk of dental implant failure and hence prove that Vitamin D supplementation can promote the osseointegration of dental implants.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Mangano C, Iaculli F, Piattelli A, Mangano F. Fixed restorations supported by Morse-taper connection implants: A retrospective clinical study with 10-20 years of follow-up. Clin Oral Implants Res. 2015;26:1229–36. doi: 10.1111/clr.12439. [DOI] [PubMed] [Google Scholar]
- 2.Becker ST, Beck-Broichsitter BE, Rossmann CM, Behrens E, Jochens A, Wiltfang J. Long-term survival of straumann dental implants with TPS surfaces: A retrospective study with a follow-up of 12 to 23 years. Clin Implant Dent Relat Res. 2016;18:480–8. doi: 10.1111/cid.12334. [DOI] [PubMed] [Google Scholar]
- 3.Mangano F, Macchi A, Caprioglio A, Sammons RL, Piattelli A, Mangano C. Survival and complication rates of fixed restorations supported by locking-taper implants: A prospective study with 1 to 10 years of follow-up. J Prosthodont. 2014;23:434–44. doi: 10.1111/jopr.12152. [DOI] [PubMed] [Google Scholar]
- 4.Gaber M, Saleh M, Fahmy M, Elba G. The effect of cholecalciferol on titanium implant osseointegration. J Dent Alexandria. 2015;40:35–9. [Google Scholar]
- 5.Viljakainen HT, Natri AM, Kärkkäinen M, Huttunen MM, Palssa A, Jakobsen J, et al. A positive dose-response effect of vitamin D supplementation on site-specific bone mineral augmentation in adolescent girls: A double-blinded randomized placebo-controlled 1-year intervention. J Bone Miner Res. 2006;21:836–44. doi: 10.1359/jbmr.060302. [DOI] [PubMed] [Google Scholar]
- 6.Dawson-Hughes B, Harris SS, Krall EA, Dallal GE. Effect of calcium and vitamin D supplementation on bone density in men and women 65 years of age or older. N Engl J Med. 1997;337:670–6. doi: 10.1056/NEJM199709043371003. [DOI] [PubMed] [Google Scholar]
- 7.Alvim-Pereira F, Montes CC, Thomé G, Olandoski M, Trevilatto PC. Analysis of association of clinical aspects and vitamin D receptor gene polymorphism with dental implant loss. Clin Oral Implants Res. 2008;19:786–95. doi: 10.1111/j.1600-0501.2008.01532.x. [DOI] [PubMed] [Google Scholar]
- 8.Holick MF. Vitamin D deficiency. N Engl J Med. 2007;357:266–81. doi: 10.1056/NEJMra070553. [DOI] [PubMed] [Google Scholar]
- 9.Freitas RP, Nunes FP, Santos LM, Santos PL, Silveria EM, Gulinelli JL. Influence of vitamin D in bone healing. J Oral Diag. 2017;2:1–8. [Google Scholar]
- 10.Makishima M. Update on recent progress in vitamin D research.Vitamin D receptor and the nuclear receptor superfamily. Clin Calcium. 2017;27:1533–41. [PubMed] [Google Scholar]
- 11.Dvorak G, Fügl A, Watzek G, Tangl S, Pokorny P, Gruber R. Impact of dietary vitamin D on osseointegration in the ovariectomized rat. Clin Oral Implants Res. 2012;23:1308–13. doi: 10.1111/j.1600-0501.2011.02346.x. [DOI] [PubMed] [Google Scholar]
- 12.Nemere I, Garbi N, Hammerling G, Hintze KJ. Role of the 1,25D3-MARRS receptor in the 1,25(OH) 2D3-stimulated uptake of calcium and phosphate in intestinal cells. Steroids. 2012;77:897–902. doi: 10.1016/j.steroids.2012.04.002. [DOI] [PubMed] [Google Scholar]
- 13.Weaver CM, Gordon CM, Janz KF. The National Osteoporosis Foundation's position statement on peak bone mass development and lifestyle factors: A systematic review and implementation recommendations. Osteoporos Int. 2016;27:1281–386. doi: 10.1007/s00198-015-3440-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Masuyama R, Stockmans I, Torrekens S, Van Looveren R, Maes C, Carmeliet P, et al. Vitamin D receptor in chondrocytes promotes osteoclastogenesis and regulates FGF23 production in osteoblasts. J Clin Invest. 2006;116:3150–9. doi: 10.1172/JCI29463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Brinker MR, O'Connor DP, Monla YT, Earthman TP. Metabolic and endocrine abnormalities in patients with nonunions. J Orthop Trauma. 2007;21:557–70. doi: 10.1097/BOT.0b013e31814d4dc6. [DOI] [PubMed] [Google Scholar]
- 16.Liu W, Zhang S, Zhao D, Zou H, Sun N, Liang X, et al. Vitamin D supplementation enhances the fixation of titanium implants in chronic kidney disease mice. PLoS One. 2014;9:e95689. doi: 10.1371/journal.pone.0095689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lee AM, Anderson PH, Sawyer RK, Moore AJ, Forwood MR, Steck R, et al. Discordant effects of vitamin D deficiency in trabecular and cortical bone architecture and strength in growing rodents. J Steroid Biochem Mol Biol. 2010;121:284–7. doi: 10.1016/j.jsbmb.2010.04.004. [DOI] [PubMed] [Google Scholar]
- 18.Mangano F, Mortellaro C, Mangano N, Mangano C. Is low serum vitamin D associated with early dental implant failure.A retrospective evaluation on 1625 implants placed in 822 patients? Mediators inflamm. 2016;2016:1–7. doi: 10.1155/2016/5319718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Monje A, Aranda L, Diaz KT, Alarcón MA, Bagramian RA, Wang HL, et al. Impact of maintenance therapy for the prevention of peri-implant diseases: A systematic review and meta-analysis. J Dent Res. 2016;95:372–9. doi: 10.1177/0022034515622432. [DOI] [PubMed] [Google Scholar]
- 20.Bryce G, MacBeth N. Vitamin D deficiency as a suspected causative factor in the failure of an immediately placed dental implant: A case report. J R Nav Med Serv. 2014;100:328–32. [PubMed] [Google Scholar]
- 21.Schulze-Späte U, Dietrich T, Wu C, Wang K, Hasturk H, Dibart S. Systemic vitamin D supplementation and local bone formation after maxillary sinus augmentation-a randomized, double-blind, placebo-controlled clinical investigation. Clin Oral Implants Res. 2016;27:701–6. doi: 10.1111/clr.12641. [DOI] [PubMed] [Google Scholar]
- 22.Javed F, Malmstrom H, Kellesarian SV, Al-Kheraif AA, Vohra F, Romanos GE. Efficacy of Vitamin D3 Supplementation on Osseointegration of Implants. Implant Dent. 2016;25:281–7. doi: 10.1097/ID.0000000000000390. [DOI] [PubMed] [Google Scholar]
- 23.Nagarajan B, Murthy V, Livingstone D, Surendra MP, Jayaraman S. Evaluation of crestal bone loss around implants placed at equicrestal and subcrestal levels before loading: A prospective clinical study. J Clin Diagn Res. 2015;9:ZC47–50. doi: 10.7860/JCDR/2015/13911.7000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Trybek G, Magda AW, Jakub K, Olga P, Andrzej B, Andrzej S, et al. The effect of vitamin D3 on the osteointegration of dental implants. BJHPA. 2018;10:25–33. [Google Scholar]
- 25.Ooms ME, Roos JC, Bezemer PD, van der Vijgh WJ, Bouter LM, Lips P. Prevention of bone loss by vitamin D supplementation in elderly women: A randomized double-blind trial. J Clin Endocrinol Metab. 1995;80:1052–8. doi: 10.1210/jcem.80.4.7714065. [DOI] [PubMed] [Google Scholar]
- 26.Zhou C, Li Y, Wang X, Shui X, Hu J. 1,25Dihydroxy vitamin D(3) improves titanium implant osseointegration in osteoporotic rats. Oral Surg Oral Med Oral Pathol Oral Radiol. 2012;114:S174–8. doi: 10.1016/j.oooo.2011.09.030. [DOI] [PubMed] [Google Scholar]
- 27.Wu Y, Yu T, Yang X. Vitamin D3 and insulin combined treatment promotes titanium implant osseointegration in diabetes mellitus rats. J Bone. 2013;52:1–8. doi: 10.1016/j.bone.2012.09.005. [DOI] [PubMed] [Google Scholar]
- 28.Miyahara T, Simoura T, Osahune N, Uchida Y, Sakuma T, Nemoto N, et al. A highly potent 26,27-Hexafluoro-1a,25-dihydroxyvitamin D3 on calcification in SV40-transformed human fetal osteoblastic cells. Calcif Tissue Int. 2002;70:488–95. doi: 10.1007/s00223-001-1039-5. [DOI] [PubMed] [Google Scholar]
- 29.Reginster JY. The high prevalence of inadequate serum vitamin D levels and implications for bone health. Curr Med Res Opin. 2005;21:579–86. doi: 10.1185/030079905X41435. [DOI] [PubMed] [Google Scholar]
- 30.Mangano FG, Oskouei SG, Paz A, Mangano N, Mangano C. Low serum vitamin D and early dental implant failure: Is there a connection.A retrospective clinical study on 1740 implants placed in 885 patients? J Dent Res Dent Clin Dent Prospects. 2018;12:174–82. doi: 10.15171/joddd.2018.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kelly J, Lin A, Wang CJ, Park S, Nishimura I. Vitamin D and bone physiology: Demonstration of vitamin D deficiency in an implant osseointegration rat model. J Prosthodont. 2009;18:473–8. doi: 10.1111/j.1532-849X.2009.00446.x. [DOI] [PubMed] [Google Scholar]


