Abstract
Purpose:
Platelet-rich fibrin (PRF) is a new platelet concentrate concept consisting of an autologous fibrin gel having accumulation of platelets and the released cytokines in a fibrin clot. The study aims to evaluate the efficacy of autologous PRF in accelerating bone regeneration and repair in fresh third molar extraction sockets. The investigators hypothesized the cicatricial properties and accumulation of growth factors in a single clot which will improve bone density and quality.
Materials and Methods:
PRF results from a natural and progressive polymerization occurring during centrifugation. Two groups were made with bilaterally impacted third molar patients. PRF was obtained and surgical extraction was carried out under aseptic conditions. Quantitative data are presented as mean. Statistical significance was inferred at P < 0.05.
Results:
Results obtained were evaluated statistically and found a significant difference between the groups in improvement in alveolar bone density of regenerate measured radiographically. The study demonstrates a faster bone formation in the extracted sockets with PRF as compared to control.
Conclusion:
PRF proved to be an autologous biomaterial with useful features that allowed efficient postextraction bone defect filling and faster bone regeneration.
Keywords: Fibrin, growth factors, platelet, platelet-rich fibrin
INTRODUCTION
Platelet-rich fibrin (PRF) is a fibrin gel made from autologous blood. It is a newly developed platelet concentrate concept. The protocol of its production attempts to accumulate platelets and the released cytokines in a fibrin clot. PRF results from a natural and progressive polymerization of the blood during centrifugation. A particularly homogeneous fibrin network thus formed presents a three-dimensional organization, even more highly coherent than natural fibrin clots.[1,2,3,4]
There are numerous functions of platelets than simple hemostasis. Platelets contain very important growth factors, for example, platelet-derived growth factors (PDGFaa, PDGFbb, and PDGFab), two isomers of transforming growth factor-beta (TGFβ1 and TGFβ2), vascular endothelial growth factor, and epithelial growth factor.[1]
The growth factors are responsible for increasing mitosis of the cell, accumulating other cells responsible for recovery to the site of injury, initiating the process of vascular growth, increasing the collagen production, and inducing cell differentiation. Wound healing these very crucial steps. Further, the increase of concentration of platelets at the site of wound is proved to promote more rapid and better healing. The same is true about osteoinduction and bone healing.[5]
PRF structurally consists of a single fibrin membrane with platelet concentrate as a major constituent which is favorable for healing and immunity. Platelets along with leukocytes and cytokines are responsible for the biology of PRF, but the matrix structure supporting them certainly plays a determining role to increase the real therapeutic potential of PRF.[3,4,6,7,8]
A natural blood clot contains mainly red blood cells (95%), approximately 5% platelets, and <1% white blood cells.[9] PRF clot contains around 97% of the platelets and >50% of the leukocytes. Platelets and leukocytes were concentrated in the PRF fibrin clot. When PRF clot is given in wound, then alteration of the cellular ratios in the wound blood clot occurs, hence leading to replacement of blood cells with platelets which stimulates all phases of healing and explains its ability to enhance healing.[10]
The purpose of this study was to evaluate PRF as a biomaterial for bone regeneration and wound healing. The investigators hypothesized the cicatricial properties and accumulation of growth factors in a single clot which will improve bone density and quality. The specific aims of the study were to compare the efficacy of PRF in terms of bone regeneration and wound healing.
MATERIALS AND METHODS
A prospective, controlled, single-blind split-mouth study composed of all patients presenting for evaluation and management of bilaterally mesioangular impacted third molars. Patients had to undergo a medical blood examination for hemoglobin, leukocyte count, platelet count, blood sugar, and serum creatinine so as to rule out any blood-related disorder. Patients with a good general health according to the American Society of Anesthesiologists classification (ASA-I and ASA-II) without any contraindication for minor oral and maxillofacial surgery and/or local or general anesthesia were included in the study. Patients diagnosed with medically compromised conditions, noncooperative patients, alcoholics, patients on anticoagulants or immunosuppressant drugs, patients with bleeding disorders, and patients with connective tissue disorders were excluded.
Ethics
This study was approved by the Institution Review Board and Institution Ethics Committee of the University vide Project no. IEC – 01, and all participants signed an informed consent agreement.
Procedure for obtaining platelet-rich fibrin
An autologous blood sample was obtained without anticoagulant in 10 ml sterilized test tubes. Blood sample was immediately centrifuged at a speed of 3000 rpm (approximately 400 g) for 10 min (Remi Model C-854/6). A fibrin clot thus formed was in three layers, i.e., the red corpuscles at the bottom, PRF in the middle of the test tube, and acellular plasma at the top [Figure 1]. The top layer of acellular plasma was removed by micropipette. The PRF clot was removed with 1 mm layer of red corpuscles with a tweezer.
Figure 1.

Platelet-rich fibrin
Surgical procedure
The mandibular third molar was extracted in a single sitting. Proper surgical protocol was followed. After extraction, in Group I, extraction socket was packed with PRF [Figure 2] after obtaining hemostasis. A regular clot was allowed to form in Group II, i.e., control group. The socket was primarily closed with 3–0 silk sutures.
Figure 2.

Empty socket with platelet-rich fibrin
Evaluation
In this study, we believe that the predictor variable is treatment group. Radiological evaluation of alveolar bone height and alveolar bone density of regenerate were considered as primary outcome variables.
The secondary clinical variables measured were pain on the Visual Analog Scale (VAS) of 0–10, presence or absence of swelling, periodontal pocket depth (PPD) by Williams' periodontal probe, presence or absence of infection, and attachment and approximation of wound margins. All the parameters were evaluated preoperatively, 1 week, 1 month, and 2 months postoperatively.
Radiological evaluation was done on a specific and fixed area, i.e., just distal to the second molar so as to remove bias associated with different types of impaction.
Radiological evaluation included alveolar bone height on the distal aspect of the second molar from the cementoenamel junction (CEJ) of the 2nd molar to the alveolar crest using digital radiography machine Orthophos XG5 (Sirona, Germany) with Sidexis Next Gen. 2.4 (Germany) Software and alveolar bone density of regenerate measured using ImageJ Software, NIH, USA, on digital orthopantomogram. All the parameters were evaluated immediately postoperatively, 1 month, 2 months, and 4 months postoperatively. A total of 4-month postoperative follow-up was done.
Statistical evaluation
The results were appropriately tabulated and analyzed statistically. The Mann–Whitney test was performed to evaluate the significance of mean values of both the groups, and the Wilcoxon signed-rank test was performed to evaluate the change in pain and PPD with time.
Statistical t-test was done to evaluate the significance in the mean values for alveolar bone depth and alveolar bone density of regenerate measured radiographically. One-way ANOVA test was done between all time intervals between each group, and post hoc Bonferroni test was done for analysis of change in alveolar bone depth and density with time.
RESULTS
The sample was composed of fifty patients having 100 third molars reported during the study period and were grouped as follows: PRF (n = 50), control (n = 50). Random selection of patients reporting to the outpatient department with age range from 20 to 35 years were included in the study. The incidence of impaction and pericoronitis was evaluated on the demographic variables more in female patients (41.18%) than male patients (58.82%). The mean age of male and female patients was 22.9 and 24.6 years, respectively.
Pain
Postoperative mean pain score in the PRF group was 2.87 ± 0.21, 0.40 ± 0.02, and 0.06 ± 0.01 evaluated at an interval of 1 week, 1 month and 2 months postoperatively. Postoperative mean pain score in the control group was 3.27 ± 0.27, 0.47 ± 0.12, and 0.0 ± 0.0 evaluated at an interval of 1 week, 1 month, and 2 months postoperatively. The pain scores in participants of both the groups marginally reduced in 1 week postoperatively (P > 0.05), as represented in Table 1.
Table 1.
Mean pain score (Visual Analog Scale) with Mann-Whitney statistical analysis
| Group | Number of sites | Day of reporting | 1 week | 1 month | 2 months |
|---|---|---|---|---|---|
| I (PRF) | 50 | 3.20 | 2.87 | 0.40 | 0.06 |
| II (control) | 50 | 3.47 | 3.27 | 0.47 | 0.00 |
| Statistical analysis | P | 0.699 | 0.303 | 0.715 | 0.317 |
| Mann-Whitney test | Inference (P) | Not significant (>0.05) | Not significant (>0.05) | Not significant (>0.05) | Not significant (>0.05) |
PRF: Platelet-rich fibrin
Swelling
Extra-oral obvious swelling was not present preoperatively in any of the sites. In the PRF group, 1 week postoperatively, 20% sites had extra-oral obvious swelling. In the control group, 1 week postoperatively, 26.6% sites had extra-oral obvious swelling. Swelling was absent after 1 and 2 months in all the patients. Difference was not statistically significant (P > 0.05) at all time intervals.
Periodontal pocket depth
Mean preoperative PPD in the PRF group was 3.67 ± 0.12 mm and in the control group were 3.73 ± 0.11 mm. After 1 week, PPD in the PRF group was 3.40 ± 0.15 mm and in the control group was 4.07 ± 0.22 mm. After 1 month, PPD in the PRF group was 2.40 ± 0.21 mm and in the control group was 2.93 ± 0.19 mm. After 2 months, PPD in the PRF group was 2.00 ± 0.22 mm and in the control group was 2.13 ± 0.19 mm [Figure 3].
Figure 3.

Alveolar bone height after 4 months
Difference between the PPD (distal to second molar) in both the groups at all time intervals was not statistically significant at all time intervals (P > 0.05). The PPD in both the groups marginally reduced after 1 week (P > 0.05) and reduced significantly after 1 month (P < 0.05) in Group I when compared to Group II, as represented in Table 2.
Table 2.
Mean periodontal pocket depth distal to second molar (mm)
| Group | Number of sites | Preoperative | 1 week | 1 month | 2 months |
|---|---|---|---|---|---|
| I (PRF) | 50 | 3.67 | 3.40 | 2.40 | 2.00 |
| II (control) | 50 | 3.73 | 4.07 | 2.93 | 2.13 |
| Statistical analysis | P | 0.906 | 0.182 | 0.118 | 0.550 |
| Mann-Whitney test | Inference (P) | Not significant (>0.05) | Not significant (>0.05) | Not significant (>0.05) | Not significant (>0.05) |
PRF: Platelet-rich fibrin
Wound health
All sites were healthy for both the groups on the 1st and 2nd months postoperatively. No significant difference of wound margins was seen between both the groups. After 1 week, the approximation was proper.
Alveolar bone height
Mean alveolar bone height immediately postoperatively in the PRF group was 4.34 ± 0.31 mm and in the control group was 4.58 ± 0.29 mm [Figure 4]. Mean of 1-month postoperative alveolar bone depth in the PRF group was 2.84 ± 0.18 mm and in the control group was 3.79 ± 0.19 mm. Two-month postoperative alveolar bone height in the PRF group was 2.15 ± 0.15 mm and in the control group was 2.72 ± 0.16 mm. After 4 months, mean alveolar bone height in the PRF group was 1.30 ± 0.11 mm and in the control group was 1.89 ± 0.12 mm [Figure 5]. Difference between both the groups was statistically significant at the 1st, 2nd, and 4th months postoperatively (P < 0.05), as represented in [Table 3a].
Figure 4.
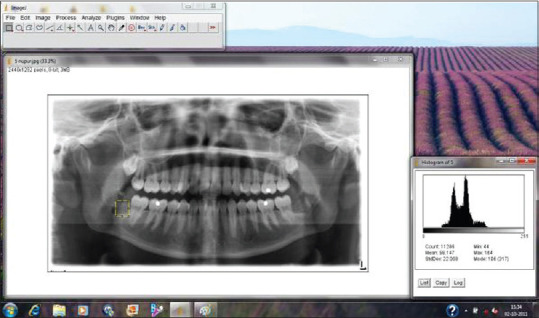
Immediate postoperative alveolar bone density
Figure 5.
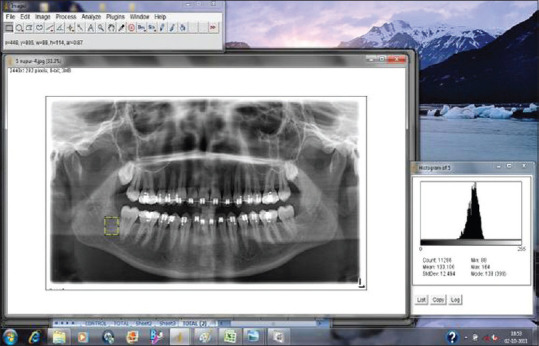
Alveolar bone density after 4 months
Table 3a.
Alveolar bone height just distal to second molar radiographically (mm)
| Group | Number of sites | Immediate postoperative | 1 month | 2 months | 4 months |
|---|---|---|---|---|---|
| I (PRF) | 50 | 4.34 | 2.84 | 2.15 | 1.30 |
| II (control) | 50 | 4.58 | 3.79 | 2.72 | 1.89 |
| Statistical analysis | P | 0.613 | 0.042 | 0.049 | 0.041 |
| T-test | Inference (P) | Not significant (>0.05) | Significant (<0.05) | Significant (<0.05) | Significant (<0.05) |
PRF: Platelet-rich fibrin
Statistical analysis of change in alveolar height with time was done by one way ANOVA test [Table 3b] and was found to be very highly significant (P < 0.001). Post hoc test was done within the group for both the groups after 1 month. The PRF group had statistically highly significant (P < 0.01) whereas the control group had statistically not significant (P > 0.05) difference when compared with the immediate postoperative alveolar bone height. Post hoc test for both the groups after the 2nd month was statistically highly significant (P < 0.01), but after the 4th month, the PRF group was statistically very highly significant (P < 0.001), whereas the control group was statistically highly significant (P < 0.01) as compared with immediate postoperative distance.
Table 3b.
Statistical analysis of change in alveolar height with time (post hoc tests)
| Group | Time | P | Inference (P) |
|---|---|---|---|
| I (PRF) | After 1 month | 0.002 | Highly significant (<0.01) |
| After 2 months | 0.01 | Highly significant (<0.01) | |
| After 4 months | <0.001 | Very highly significant (<0.001) | |
| II (control) | After 1 month | 0.266 | Not significant (>0.05) |
| After 2 months | 0.01 | Highly significant (<0.01) | |
| After 4 months | 0.01 | Highly significant (<0.01) |
PRF: Platelet-rich fibrin
Alveolar bone density of regenerate
Mean alveolar bone density measured immediately postoperatively in the PRF group was 107.40 ± 0.28 and in the control group was 107.55 ± 0.27. After 1 month, mean in the PRF group was 114.01 ± 0.21 and in the control group was 108.21 ± 0.23. After 2 months, mean in the PRF group was 124.13 ± 0.21 and in the control group was 115.59 ± 0.19. After 4 months, mean in the PRF group was 135.15 ± 0.20 and in the control group was 124.26 ± 0.21 [Table 4a]. Difference between both the groups was not statistically significant immediately postoperatively (P > 0.05) but was statistically significant at the 1st month postoperatively and was statistically very highly significant at the 2nd and 4th months postoperatively (P < 0.001).
Table 4a.
Mean alveolar bone density of regenerate in pixels radiographically
| Group | n | Immediate postoperative | 1 month | 2 months | 4 months |
|---|---|---|---|---|---|
| I (PRF) | 50 | 107.40 | 114.01 | 124.13 | 135.15 |
| II (control) | 50 | 107.55 | 108.21 | 115.59 | 124.26 |
| Statistical analysis t-test | P | 0.972 | 0.048 | 0.001 | <0.001 |
| Inference (P) | Not significant (>0.05) | Significant (<0.05) | Very highly significant (<0.001) | Very highly significant (<0.001) |
ImageJ Software, NIH, USA. PRF: Platelet-rich fibrin
Oneway ANOVA test was done for change in alveolar bone density with time [Table 4b] and was found to be highly significant (P < 0.001). After 1month, Post hoc test within the groups were found to be statistically not significant (P < 0.05). After 2 months, Statistical analysis of change in alveolar density with time in PRF Group was found to be very highly significant (P < 0.001) whereas in control group it was found to be statistically not significant (P > 0.05). Post hoc test for both the groups after the 4th month was statistically very highly significant (P < 0.001) as compared with the immediate postoperative alveolar bone density.
Table 4b.
Statistical analysis of change in alveolar bone density with time (post hoc tests)
| Group | Time | P | Inference (P) |
|---|---|---|---|
| I (PRF) | After 1 month | 0.126 | Not significant (>0.05) |
| After 2 months | <0.001 | Very highly significant (<0.001) | |
| After 4 months | <0.001 | Very highly significant (<0.001) | |
| II (control) | After 1 month | 0.101 | Not significant (>0.05) |
| After 2 months | 0.140 | Not significant (>0.05) | |
| After 4 months | <0.001 | Very highly significant (<0.001) |
PRF: Platelet-rich fibrin
DISCUSSION
The purpose of this study was to evaluate PRF as a biomaterial for bone regeneration and wound healing. The investigators hypothesized the cicatricial properties and accumulation of growth factors in a single clot which will improve bone density and quality. The specific aims of the study were to compare the efficacy of PRF in terms of bone regeneration and wound healing.
In this study, comparative evaluation of PRF was done when given in extraction socket in respect to pain, swelling, wound margins, PPD, wound health, alveolar bone height, and alveolar bone density of the regenerate. Dohan Ehrenfest et al.,[11] while investigating clinical effects of PRF on healing of tissues, conducted clinical trials to confirm the properties of PRF as a healing biomaterial. PRF consists of all the necessary parameters required for healing. A fibrin matrix polymerized in a tetramolecular structure, consisting of platelets, leukocyte, cytokines, and circulating stem cells. The cytokines trapped in matrix are released gradually and are responsible to accelerate the cellular phenomenon.[12,13]
The primary outcome variables of alveolar bone height when augmented with the clinical variables show a better outcome in relation to pain, swelling, and alveolar bone height on the PRF sites as compared to the control side.
Pain was evaluated and recorded on the VAS of 0–10. The patients in Group I exhibited less pain than those in Group II postoperatively in general. However, the difference in pain at 1 week, 1 month, and 2 months in both the groups evaluated was statistically not significant (P > 0.05). Alissa et al.[14] did a study for pain evaluation using VAS and was found to be significantly higher pain in the control group than the test group on the first 3 postoperative days. No differences were observed on the 4th, 5th, 6th, and 7th postoperative days. Marco Mozzati et al.[15] reported lower pain for autologous plasma rich in growth factors (PRGF) site than for control sites at all times examined, even if the difference was significant.
The patients in the PRF group had less incidence of swelling postoperatively as compared to the control group. There were no statistically significant differences between the swelling evaluated in both the groups (P > 0.05).
According to Alissa et al.,[14] complications encountered in their study consisted of dry sockets and acute inflammation of alveolus in the control group patients. The complications determined a statistically significant difference in favor of the test group, i.e., Periodontal Pocket Depth PPD group (P = 0.06). The PPD (distal to second molar) improved significantly after 1 month in participants of Group I as compared to participants of Group II. However, the difference in improvement of the PPD between the groups at all time intervals was not statistically significant. Krausz et al.[16] studied longterm clinical changes in the health of periodontium and height of alveolar bone present at the distal aspect of the adjacent second molar but found no statistically significant difference (P > 0.05) in clinical attachment level.
Alveolar bone height just distal to second molar was measured radiographically by Sidexis software (Sirona). There was a statistically significant difference between both the groups in distance between CEJ to the highest point of alveolar bone just distal to second molar measured radiographically on 1 month, 2 months, and 4 months postoperatively. Within Group I, the improvement in alveolar bone height after 1 month was statistically highly significant, whereas in Group II, it was statistically not significant. After the 4th month also, the improvement was statistically very highly significant in Group I, whereas it was statistically highly significant in Group II patients.
The primary outcome variable, i.e., alveolar bone density of regenerate was measured in pixels radiographically by ImageJ Software, NIH, USA. A statistically significant difference was observed between the groups in improvement in alveolar bone density of regenerate measured radiographically after 1 month, 2 months, and 4 months postoperatively. Within Group I, the improvement in alveolar bone density after 2 months was statistically very highly significant, whereas in Group II, it was statistically not significant. Hence, We concluded that there was faster bone formation in the extracted sockets with PRF as compared to controls. In studies conducted by Sammartino et al.[17] and Choukroun et al.[18] who performed histological evaluation of the test sites after an interval of 3 months found the presence of bone tissue newly formed with a high density of osteoblast. Our study had a prime focus on the alveolar bone density which was measured on the specific and most crucial area, i.e., distal to the second molar in any type of impaction. Our study measured a fixed area similar on all radiographs which reduced the study bias and hence an edge over other conducted studies.
CONCLUSION
The results of the study show that applying PRF is an emerging technique/graft material for treating alveolar defects after third molar impaction as it has been stated that Choukroun's PRF is a quickly and easily preparable second-generation platelet concentrate. It is an autologous product with cicatricial properties and is the latest development in bioactive surgical additives. After the surgical extraction of impacted third molar, complications more prevalent are periodontal pocket formation on the distal aspect of the second molar tooth. The use of PRF is found to be a useful tool in countering periodontal problems distal to second molar and bone regeneration because of the high content of growth factors.[19] In this study, we evaluated PRF as a biomaterial for its bone regeneration properties following extraction of impacted third molars and compared with control or normal healing. Patients with PRF demonstrated better periodontal healing distal to the second molar showing improvement in PPD clinically and level of bone formation distal to second molar radiographically leading to significant reduction in incidence of periodontal complications after third molar removal than the patients of the control group.[20,21] In essence, the PRF proved to be an autologous biomaterial with useful features that allowed efficient postextraction bone defect filling and faster bone regeneration.[22,23] In conclusion, the present study shows that PRF can be of paramount importance in accelerating bone healing following the extraction of impacted lower third molar and appears to accelerate physiologic tissue healing.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
The authors deny any conflicts of interest or involvement with any commercial organization with direct financial interest in the subject or materials discussed in this manuscript.
REFERENCES
- 1.Marx RE, Carlson ER, Eichstaedt RM, Schimmele SR, Strauss JE, Georgeff KR. Platelet-rich plasma: Growth factor enhancement for bone grafts. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1998;85:638–46. doi: 10.1016/s1079-2104(98)90029-4. [DOI] [PubMed] [Google Scholar]
- 2.Soffer E, Ouhayoun JP, Anagnostou F. Fibrin sealants and platelet preparations in bone and periodontal healing. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2003;95:521–8. doi: 10.1067/moe.2003.152. [DOI] [PubMed] [Google Scholar]
- 3.Dohan DM, Choukroun J, Diss A, Dohan SL, Dohan AJ, Mouhyi J, et al. Platelet-rich fibrin (PRF): A second-generation platelet concentrate.Part I: Technological concepts and evolution. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2006;101:e37–44. doi: 10.1016/j.tripleo.2005.07.008. [DOI] [PubMed] [Google Scholar]
- 4.Dohan DM, Choukroun J, Diss A, Dohan SL, Dohan AJ, Mouhyi J, et al. Platelet-rich fibrin (PRF): A second-generation platelet concentrate.Part II: Platelet-related biologic features. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2006;101:e45–50. doi: 10.1016/j.tripleo.2005.07.009. [DOI] [PubMed] [Google Scholar]
- 5.Banks RE, Forbes MA, Kinsey SE, Stanley A, Ingham E, Walters C, et al. Release of the angiogenic cytokine vascular endothelial growth factor (VEGF) from platelets: Significance for VEGF measurements and cancer biology. Br J Cancer. 1998;77:956–64. doi: 10.1038/bjc.1998.158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Choukroun J, Adda F, Schoeffler C, Vervelle A. Une opportuniteen paro-implantologie: Le PRF. Implantodontie. 2001;42:55–62. [Google Scholar]
- 7.Gaultier F, Navarro G, Donsimoni JM, Dohan D. Platelet concentrates.Part 3: Clinical applications. Implantodontie. 2004;13:3–11. [Google Scholar]
- 8.Simonpieri A, Choukroun J, Girard MO, Ouaknine T, Dohan D. Immediate post-extraction implantation: interest of the PRF. Implantodontie. 2004;13:177–89. [Google Scholar]
- 9.Carlson NE, Roach RB., Jr Platelet-rich plasma: Clinical applications in dentistry. J Am Dent Assoc. 2002;133:1383–6. doi: 10.14219/jada.archive.2002.0054. [DOI] [PubMed] [Google Scholar]
- 10.Dohan DM, Choukroun J, Diss A, Dohan SL, Dohan AJ, Mouhyi J, et al. Platelet-rich fibrin (PRF): A second-generation platelet concentrate.Part III: Leucocyte activation: A new feature for platelet concentrates? Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2006;101:e51–5. doi: 10.1016/j.tripleo.2005.07.010. [DOI] [PubMed] [Google Scholar]
- 11.Dohan Ehrenfest DM, Diss A, Odin G, Doglioli P, Hippolyte MP, Charrier JB, et al. In vitro effects of Choukroun's PRF (platelet-rich fibrin) on human gingival fibroblasts, dermal prekeratinocytes, preadipocytes, and maxillofacial osteoblasts in primary cultures. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2009;108:341–52. doi: 10.1016/j.tripleo.2009.04.020. [DOI] [PubMed] [Google Scholar]
- 12.Choukroun J, Diss A, Simonpieri A, Girard MO, Schoeffler C, Dohan SL, et al. Platelet-rich fibrin (PRF): A second-generation platelet concentrate.Part IV: Clinical effects on tissue healing. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2006;101:e56–60. doi: 10.1016/j.tripleo.2005.07.011. [DOI] [PubMed] [Google Scholar]
- 13.Prakash S, Thakur A. Platelet concentrates: Past, present and future. J Maxillofac Oral Surg. 2011;10:45–9. doi: 10.1007/s12663-011-0182-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Alissa R, Esposito M, Horner K, Oliver R. The influence of platelet-rich plasma on the healing of extraction sockets: An explorative randomised clinical trial. Eur J Oral Implantol. 2010;3:121–34. [PubMed] [Google Scholar]
- 15.Mozzati M, Gallesio G, Arata V, Pol R, Scoletta M. Platelet-rich therapies in the treatment of intravenous bisphosphonate-related osteonecrosis of the jaw: A report of 32 cases. Oral Oncol. 2012;48:469–74. doi: 10.1016/j.oraloncology.2011.12.004. [DOI] [PubMed] [Google Scholar]
- 16.Krausz AA, Machtei EE, Peled M. Effects of lower third molar extraction on attachment level and alveolar bone height of the adjacent second molar. Int J Oral Maxillofac Surg. 2005;34:756–60. doi: 10.1016/j.ijom.2005.02.006. [DOI] [PubMed] [Google Scholar]
- 17.Sammartino G, Tia M, Marenzi G, di Lauro AE, D'Agostino E, Claudio PP. Use of autologous platelet-rich plasma (PRP) in periodontal defect treatment after extraction of impacted mandibular third molars. J Oral Maxillofac Surg. 2005;63:766–70. doi: 10.1016/j.joms.2005.02.010. [DOI] [PubMed] [Google Scholar]
- 18.Choukroun J, Diss A, Simonpieri A, Girard MO, Schoeffler C, Dohan SL, et al. Platelet-rich fibrin (PRF): A second-generation platelet concentrate.Part V: Histologic evaluations of PRF effects on bone allograft maturation in sinus lift. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2006;101:299–303. doi: 10.1016/j.tripleo.2005.07.012. [DOI] [PubMed] [Google Scholar]
- 19.Del Fabbro M, Bortolin M, Taschieri S. Is autologous platelet concentrate beneficial for post-extraction socket healing.A systematic review? Int J Oral Maxillofac Surg. 2011;40:891–900. doi: 10.1016/j.ijom.2011.04.009. [DOI] [PubMed] [Google Scholar]
- 20.Zhao JH, Tsai CH, Chang YC. Clinical and histologic evaluations of healing in an extraction socket filled with platelet-rich fibrin. J Dent Sci. 2011;6:116–22. [Google Scholar]
- 21.Hoaglin DR, Lines GK. Prevention of localized osteitis in mandibular third-molar sites using platelet-rich fibrin. Int J Dent. 2013;2013:875380. doi: 10.1155/2013/875380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Uyanık LO, Bilginaylar K, Etikan İ. Effects of platelet-rich fibrin and piezosurgery on impacted mandibular third molar surgery outcomes. Head Face Med. 2015;11:25. doi: 10.1186/s13005-015-0081-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kumar YR, Mohanty S, Verma M, Kaur RR, Bhatia P, Kumar VR, et al. Platelet-rich fibrin: The benefits. Br J Oral Maxillofac Surg. 2016;54:57–61. doi: 10.1016/j.bjoms.2015.10.015. [DOI] [PubMed] [Google Scholar]


