Abstract
Introduction:
University of Utah Health is an academic health care system that serves residents in Utah and beyond. Clinical pharmacists with the health care system’s pharmacy primary care services (PPCS) team provide medication education, population-based care, and medication management through collaborative practice agreements. With the expansion of clinical pharmacist and technician positions and services, the need to measure and assess the impact of pharmacy services and create a value proposition for internal and external stakeholders became an important goal, and the decision was made to better align practices across all PPCS sites. This paper highlights University of Utah Health’s approach to implement comprehensive medication management (CMM) across all primary care clinics with embedded clinical pharmacy staff and subsequent evaluation of implementation fidelity.
Methods:
Implementation of CMM was assisted by participation in the National A3 Collaborative and by using selected principles from the Active Implementation Framework. Stages of implementation included exploration, instillation, and initiating improvement cycles. An implementation team consisting of PPCS employees was created to help with standardization, developing implementation plans, and creating a dissemination strategy for all PPCS team members. The CMM care process was subsequently presented and implemented by clinical pharmacists in primary care clinics. Following implementation, fidelity measures were collected including identification and resolution of medication therapy problems (MTPs) and responses from a questionnaire distributed to the clinical pharmacists to self-report understanding and implementation of CMM key elements. The number and type of MTPs identified were tracked over 18 months.
Results:
Within the measurement window, clinical pharmacists identified 17,953 MTPs. Of the total number of MTPs identified, 21% were related to indication, 53% to efficacy, 15% to safety and 11% to adherence. The questionnaire was distributed to clinical pharmacists 9 months after CMM implementation, with a 71% response rate. Pharmacists reported “always” or “often” performing each step in the patient care process as follows: indication (93%), effectiveness (93%), safety (87%), and adherence (93%). Reported barriers to implementation of the CMM include lack of time to complete all aspects of the process efficiently, lack of a standardized format for documentation, and changing practice habits.
Conclusion:
Implementation of a CMM process within University of Utah Health’s PPCS services with the help of a national collaborative and implementation framework yielded identification of 17,953 MTPs over 18 months and foundational fidelity to core principles.
Keywords: comprehensive medication management, clinical pharmacy, implementation science, fidelity
Introduction
University of Utah Health is an academic health care system located in Utah that serves residents in the state and beyond via 14 community clinics, 4 hospitals, and more than 5,000 health care professionals. As a part of University of Utah Health, Pharmacy Primary Care Services (PPCS) consists of 17 clinical pharmacists, 4 primary care pharmacy residents, and 7 clinical pharmacy technicians embedded into 16 primary care practices. These professionals contribute to the primary care team by providing patients and health care providers with medication education, transitions of care support, population-based care, and medication management using collaborative practice agreements. Clinical technicians support pharmacist practitioners with administrative and patient care duties including managing referrals, assisting with medication affordability, and contacting patients for follow up regarding disease state management.
In 2017, after considerable expansion of pharmacists, technicians and location of practices, driven largely by internal recognition of pharmacist impact, PPCS leaders and practitioners noted that variation existed between primary care practice sites resulting in inconsistent services, unreliable outcomes, and limited efficiency. For example, some practitioners focused their time more on single disease management services while others had developed more comprehensive practices as they established stronger relationships with primary care providers and patients. Other concerns included location of services provided and varying degrees of integration into the medical practice to provide team-based care. Finally, following the expansion of the number of pharmacist and technician positions, the focus on tracking solely activities performed, time spent, and patient outcomes was shifted to the need to measure and assess value of pharmacy services for internal and external stakeholders. Recognizing that, if unaddressed, these barriers could potentially limit future growth and sustainability of the provision of patient care services by PPCS pharmacists, the decision was made to better align practices across all PPCS practice sites.
As a solution, the PPCS team began the process of implementing comprehensive medication management (CMM) based on the principles of the Active Implementation Frameworks (AIFs).1 CMM is defined as a patient-centered standard delivered by a clinical pharmacist in partnership with a team of health care professionals; practitioners delivering CMM ensure each medication taken by a given patient has an appropriate indication, is effective for the medical condition, is safe for that specific patient, and is adhered to by the patient. Medications are deliberately reviewed in this order to assist the pharmacist in ensuring each medication is optimized for an individual patient. The CMM patient care process also involves developing patient medication therapy care plans based on goals of therapy.2,3 To help with implementation of CMM, PPCS leaders specifically selected principles from the AIFs, which was created through a review and analysis of implementation science literature, because it had been highlighted as a model by previous CMM research teams.1,4 The five AIFs are evidence-based frameworks that include a usable innovation, implementation drivers, implementation stages, improvement cycles, and implementation teams.1 PPCS leaders adopted CMM as the “usable innovation” to standardize practice and align with national efforts encouraging its uptake in primary care settings.2–3 Additionally, CMM was selected as an evidence-based approach which has demonstrated positive outcome in previous research in the hope that CMM implementation with high fidelity would create similar positive results in a new setting.5–8 Implementation of CMM included aspects of all three essential CMM components: shared philosophy of practice, patient care process, and practice management system.3 This paper highlights the approach of University of Utah Health’s CMM primary care implementation and evaluation of implementation fidelity.
Methods
Implementation of CMM was assisted by participation in the National A3 Collaborative, a learning collaborative to support health care organizations implementing CMM services in value-based payment models, offered by the Alliance for Integrated Medication Management, Apexus, and the American Society of Health-System Pharmacists.9 PPCS pharmacists engaged in the collaborative over the course of two years through in-person meetings at national pharmacy conferences, monthly coaching calls and tools designed to measure progress and institutional change. As previously discussed, selected principles from the AIFs were used to help with CMM implementation, including the usable innovation (described above), framing via implementation stages, determining drivers and cycles of CMM adoption and description of the implementation team. This CMM implementation project was determined to be exempt from institutional review board review due to the quality improvement nature of the project.
Stage 1: Exploration
After the gap in standardization and consistency of practice noted was identified, the PPCS clinical manager created a CMM implementation team comprised of eight PPCS pharmacists in March 2017. Additional team members included fourth year pharmacy students, clinical technicians and pharmacy residents as needed based on the current stages of implementation and participant interest. The implementation team met twice monthly to develop implementation plans, divide tasks and consider a dissemination strategy for all PPCS team members. Implementation occurred intentionally within key CMM domains including creating a shared philosophy of practice, utilization of a consistent patient care process and developing similar practice management systems.3 The implementation team considered essential CMM implementation drivers (described below), accumulated current best practices in the institution’s primary care clinics, and considered how to motivate primary care pharmacists towards a more complete and comprehensive view of the patient and their medications. The workgroup also discussed how to organize CMM within the clinics to maximize outcomes and identify, track and document interventions. As mentioned, participation in the National A3 Collaborative facilitated the workgroup’s implementation of CMM by providing coaching and sharing of successful practices from assigned collaborative coaches working in outside institutions and bi-annual live team sessions with other organizations implementing CMM. See Figure 1 for project implementation timeline.
Figure 1.
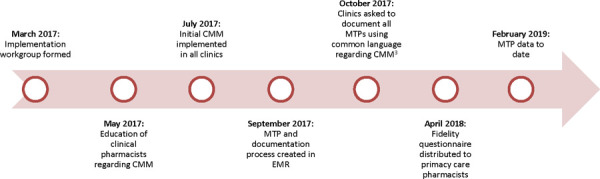
Implementation Timeline
CMM: Comprehensive medication management; EMR: Electronic medical record; MTP: Medication therapy problem
Stage 2: Installation
Examine Implementation Drivers
The CMM implementation team determined that the key drivers for this project were associated with a shared philosophy of practice and a consistent care process. Initial implementation would focus mainly on developing each pharmacist’s ability to utilize the CMM patient care process consistently and with fidelity. Subsequent efforts in CMM implementation would revolve around practice management systems.
Develop Practitioner Readiness
The CMM philosophy of practice and patient care process were ultimately introduced to the PPCS pharmacist group via education at monthly staff meetings beginning in May 2017. During these staff meetings, the implementation team presented the CMM patient care process for clinical encounters and guidance on appropriate documentation in the electronic medical record (EMR). Resources included published literature on CMM and those developed by the American College of Clinical Pharmacy and the Patient Centered Primary Care Collaborative.2,3 Once the foundation was set for the CMM philosophy of practice and patient care process, data collection tools, such as an MTP tracking tool in the EMR, were created so initial measurement of CMM implementation could begin. Clinical pharmacists were encouraged to discuss CMM and its benefits with the primary care providers at their clinics. While many of the daily functions performed within the clinics would be unchanged, pharmacists were encouraged to discuss the development of more comprehensive practices which would necessitate enhanced collaboration with health care teams and medical providers.
Develop Fidelity Measures
Based on the identified drivers, two measures were selected to assess fidelity to CMM implementation: 1) identification and resolution of medication therapy problems (MTPs) and 2) a pharmacist questionnaire. Medication therapy problems were adopted as a means to assess competency of pharmacists in operationalizing the patient care process and were defined according to the Pharmacy Quality Alliance (PQA) MTP Categories Framework.3,10 Using the EMR, MTP data was tracked and collected. The number and type of MTPs identified were tracked from September 2017 to February 2019 and the resolution of MTPs was tracked from July 2018 to February 2019. MTP resolution was defined as an action step actually taken to address the identified problem, and it was deemed an important measure to ensure that patients’ needs regarding their medications were fulfilled rather than only noting the presence of a problem.
The second fidelity measure built upon the foundation of MTP identification and resolution and consisted of a questionnaire instrument to self-report understanding and implementation of CMM key elements. This instrument was distributed to pharmacists in April 2018, 9 months after initial implementation. The questionnaire was developed by the authors, based on elements in the Patient Care Process for Delivering Comprehensive Medication Management document, to assess understanding of the core elements of CMM, specifically the patient care process and what improvements were needed.3 The questionnaire was anonymous and distributed electronically, consisting of questions to collect demographics, frequency of reporting of clinical activities, and assessments of the understanding and use of the CMM patient care process via 5-point Likert scale and free-text questions (Appendix A).
Stage 3: Initial Implementation
Initiate Improvement Cycles
After the CMM implementation process began, ongoing discussion among all clinical pharmacists occurred monthly to ensure the process was used consistently across clinics. Discussions were held during previously scheduled staff meetings to minimize outside time obligations for the PPCS team, primarily consisting of didactic presentations, discussions with pharmacist feedback and distribution of preliminary results of MTP data. Feedback on additional mechanisms to support the adoption of CMM and improve patient outcomes was informally sought from clinical pharmacists throughout the project. Pharmacists also spent time shadowing each other for peer review and further standardization, which consisted of a half-day shadowing experience using a standardized process and documentation form.
Results
Medication Therapy Problems (MTPs):
Within the measurement window of 18 months, clinical pharmacists identified 17,953 MTPs. Of the total number of MTPs identified, 21% were related to indication, 53% to efficacy, 15% to safety and 11% to adherence (Figure 2). The monthly resolution rate for identified MTPs ranged from 98.0 to 99.9% from July 2018 to February 2019.
Figure 2.
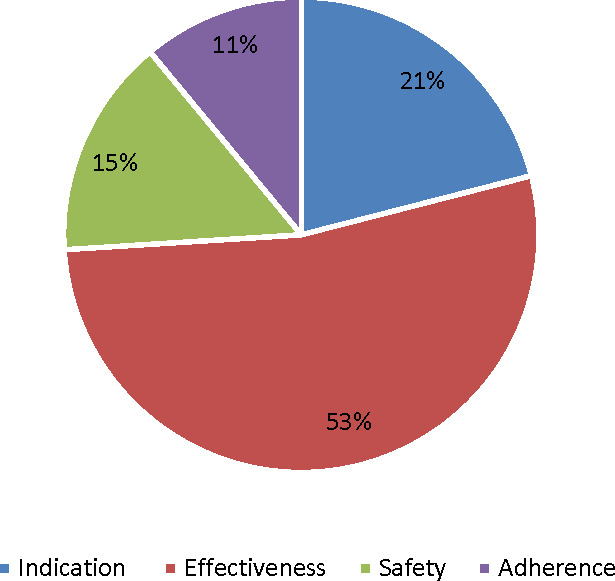
Medication Therapy Problems (MTP) Documented by Category
Pharmacist Questionnaire:
Regarding the questionnaire sent to all primary care clinical pharmacists and primary care pharmacy residents at the institution, 15 of 21 (71%) completed the questionnaire in its entirety. Time in practice averaged 5.9 years, and most completed PGY1 or PGY2 residency (76 and 53%, respectively) and earned board certification (88%). When asked to define the CMM patient care process, pharmacists demonstrated they understood the comprehensive nature of the care process, as most who responded discussed a holistic or systematic component of CMM. Pharmacists reported “always” or “often” performing each step in the patient care process as follows: indication (93%), effectiveness (93%), safety (87%), and adherence (93%). Only 60% reported completing those steps in the precise order “often” or “always” (Figure 3 and Table 1). Pharmacists reported benefits of implementing the process included better structuring for learner education, giving more organization to patient medication reviews, and being more cognizant of a consistent and comprehensive approach to medication management. Reported barriers to implementation of the CMM care process included lack of time to complete all aspects of the process efficiently, lack of a standardized format for documentation in the EMR, and changing practice habits.
Figure 3.
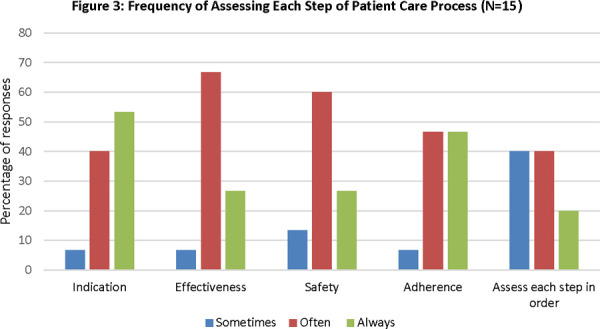
Frequency of Assessing Each Step of Patient Care Process (N=15)
Table 1. Patient Care Process Questionnaire.
During a patient initial comprehensive medication review, do you do the following > 80% of the time? (N=15) |
Yes |
No |
|---|---|---|
Inquire about patient’s alcohol, tobacco, caffeine use? |
53% |
47% |
Inquire about immunizations? |
80% |
20% |
Obtain and document a complete medication list? |
100% |
0% |
Gather past medication history? |
80% |
20% |
Inquire about ability to access medications? |
100% |
0% |
Inquire as to whether the patient independently manages medications or has help at home? |
93% |
7% |
Inquire how the process of managing medications works at home (e.g. pillboxes, calendars, reminders)? |
93% |
7% |
Inquire about adherence to medications? |
100% |
0% |
Improvement Cycles:
Several improvements to CMM implementation occurred during the project. The majority centered on standardization of MTP documentation among clinical pharmacists and increasing the number of actual MTPs identified to more accurately quantify the effort of the pharmacists. Improvements were also made to the MTP data collection tool in the EMR to help with efficiency and documentation. Continued effort was devoted to encouraging a comprehensive assessment of all medications and maintaining fidelity to the CMM patient care process during monthly staff meetings. This included sample patient cases using the CMM care process, discussions around categorization of MTPs and peer review. Improvements were made per recommendations of the implementation team in consultation with National A3 Collaborative coaches, which included framing issues with quality improvement methodology, reinforcement of implementation science principles (i.e. fidelity measures, etc.), consultation on creating a value proposition for internal and external stakeholders, training and onboarding new pharmacists and seeking to further define and refine a patient population most in need of CMM.
Discussion
To our knowledge, this is the first study reporting system-wide implementation of CMM in a novel environment with attention to fidelity measurement. Early implementation of CMM showed improvement in adoption of elements of the CMM patient care process and the identification and resolution of MTPs. Results of the questionnaire revealed that aspects of CMM are being utilized by PPCS pharmacists to provide a more holistic approach to assessing medications during patient interactions, but further efforts are needed in following the patient care process consistently. Throughout the implementation process team members identified several practice changes and tools to enhance implementation of CMM including a standardized note template, enhancement of existing peer review processes and a more formalized and user-friendly mechanism for capturing MTPs.
The identification of the majority of MTPs in the indication and effectiveness categories is consistent with previous literature; however, this institution’s project showed a higher percentage of effectiveness problems as compared to previously published studies.5–8 These studies have also shown an improvement in clinical outcomes and resolution of MTPs, including an increase in patients meeting clinical goals as well as reductions in health care expenditures.5–8 It is possible that the higher percentage of MTPs in the effectiveness category identified in this project was due to clinical pharmacists not documenting all possible MTPs, which would have resulted in more MTPs in the other categories. The lack of documentation could have been caused by confusion on whether an identified issue needed to be documented, which category to use and how many MTPs to document if a high number was identified.
Documenting and tracking MTPs was time consuming and seen as additive work as they were not documented into progress notes directly but in a separate format that could be traceable through reports in the EMR. It was also noticed throughout the implementation process that there were variations in pharmacist reporting of MTPs, as several interventions may be interpreted and categorized differently. Enhancing the capture rate of MTPs is an area of continued emphasis. A standardized process to document patient progress notes and MTPs in the EMR would help the PPCS team use a consistent CMM process and make the data more easily retrievable for internal quality improvement.
Limitations of the implementation included the utilization of a questionnaire that had not been validated although constructed from previously published resources.3 Not all clinical pharmacists completed the questionnaire meaning key information from select individuals was not captured. While two potential means to assess implementation fidelity were included, these are not complete measures. The focus of the two fidelity measures created only centered on the patient care process and did not address philosophy of practice or practice management which are core tenets of CMM.
The implementation of CMM within University of Utah Health is still ongoing. Future work in CMM implementation will include assessment and improvement in practice management, additional means of testing fidelity to the patient care process and expanding coaching as a means to enhance adoption and fidelity by individual clinical pharmacists. Further efforts will be needed to demonstrate positive clinical, financial and humanistic outcomes from CMM adoption, with specific emphasis on cost-savings assessments of those receiving CMM by PPCS clinical pharmacists compared to those not receiving the service in collaboration with local payers.
Conclusion
Implementation of a CMM process within University of Utah Health’s primary care clinical pharmacy services with the help of a national collaborative yielded identification of 17,953 MTPs over 18 months and foundational fidelity to core principles. Further refinement of CMM implementation is needed to increase understanding, utilization and consistency.
Acknowledgments
Acknowledgements: The authors recognize the contributions of clinical pharmacists, pharmacy technicians, students and residents for their efforts in implementing CMM within University of Utah Health
Funding: none
Conflicts of interest: none
Treatment of Human Subjects: This project was deemed exempt from review by the University of Utah Institutional Review Board
Appendix A: PPCS Clinical Pharmacist Questionnaire
Q1. How many years of practice experience do you have inambulatory care?
Q2. What year did you graduate from pharmacy school?
-
Q3. Did you complete a PGY-1 residency?
Did you complete a PGY-2 residency?
Have you ever practiced ambulatory clinical pharmacy at another institution?
Q4. What was your PGY-2 specialty?
Q5. Please check what board certifications do you currently hold?
Q6. Without looking at other resources, how would youpersonally define the CMM patient care process?
Q7. How has the implementation of the CMM patient care process benefited your practice?
Q8. What barriers have you encountered in theimplementation of the CMM patient care process?
-
Q9. When conducting an initial visit for a comprehensivemedication review, do you do the following >80% of thetime:
Inquire about use of alcohol, tobacco, and caffeine?
Inquire about immunizations?
Obtain and document a complete medication list that includes nonprescription medications?
Gather past medication history?
Inquire about the patient’s ability to access medications (e.g., ability to pick up or afford medications)?
Inquire as to whether the patient independently manages his/her medications, or if they have help at home?
Inquire as to how the process of managing medications works at home (e.g., pill boxes, calendars, reminders)?
Inquire about the patient’s adherence to his/her medications?
-
Q10. Please answer the following questions regarding initialpatient visits:
Likert scale:
Never --- Seldom --- Sometimes --- Often --- Always
How often do you assess the indication of EACH medication the patient is taking?
How often do you assess the effectiveness (i.e. meeting clinical goals, appropriate monitoring, etc) of EACH medication each patient is taking?
How often do you assess the safety (i.e adverse events, drug interactions) of EACH medication the patient is taking?
How often do you assess the adherence (i.e. access, affordability, missing doses, etc.) of EACH medication the patient is taking?
How often do you complete the previous four steps in THAT ORDER (indication, effectiveness, safety, adherence)?
How often do you formulate and document medication therapy problems in EPIC as I-vents, classifying the patient’s medication therapy problems based on indication, effectiveness, safety, and adherence?
How often are you able to resolve the identified medication therapy problems?
Q11. If frequently unable to resolve the MTP, what is the mainbarrier to resolution?
Q12. What questions do you have about CMM at this point?
Q13. What would you like to know more about regarding CMM?
References
- 1.Blanchard C, Livet L, Ward C, et al. The Active Implementation Frameworks: A roadmap for advancing implementation of Comprehensive Medication Management in primary care. Res Social Adm Pharm. 2017;13(5):922–929. doi: 10.1016/j.sapharm.2017.05.006. [DOI] [PubMed] [Google Scholar]
- 2.McInnis T, Webb E, Strand L. The patient-centered medical home: integrating comprehensive medication management to optimize patient outcomes (June 2012). www.pcpcc.org/sites/default/files/media/medmanagement.pdf Available at.
- 3.The Patient Care Process for Delivering Comprehensive Medication Management (CMM): Optimizing Medication Use in Patient-Centered, Team-Based Care Settings CMM in Primary Care Research Team. Jul, 2018. http://www.accp.com/cmm_care_process Available at.
- 4.Livet M, Blanchard C, Sorensen TD, et al. An implementation system for medication optimization: Operationalizing comprehensive medication management delivery in primary care. J Am Coll Clin Pharm. 2018;1:14–20. [Google Scholar]
- 5.de Oliveira DR, Brummel AR, Miller DB. Medication therapy management: 10 years of experience in a large integrated health care system. J Manag Care Pharm. 2010;16(3):185–95. doi: 10.18553/jmcp.2010.16.3.185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Isetts BJ, Schondelmeyer SW, Artz MB, et al. Clinical and economic outcomes of medication therapy management services: the Minnesota experience. J Am Pharm Assoc (2003) 2008;48(2):203–11. doi: 10.1331/JAPhA.2008.07108. [DOI] [PubMed] [Google Scholar]
- 7.Smith M, Giuliano MR, Starkowski MP. In Connecticut: improving patient medication management in primary care. Health Aff (Millwood) 2011;30(4):646–54. doi: 10.1377/hlthaff.2011.0002. [DOI] [PubMed] [Google Scholar]
- 8.Isetts BJ, Brummel AR, de Oliveira DR, Moen DW. Managing drug-related morbidity and mortality in the patient-centered medical home. Med Care. 2012;50(11):997–1001. doi: 10.1097/MLR.0b013e31826ecf9a. [DOI] [PubMed] [Google Scholar]
- 9.A3 Collaborative American Society of Health System Pharmacists. [Jun 14;2018 ]. https://www.ashp.org/Pharmacy-Practice/A3-Collaborative Accessed.
- 10.Pharmacy Quality Alliance (PQA) MTP Categories Framework. [Jun 14;2018 ]. http://pqaalliance.org/images/uploads/files/PQA Available at. Accessed.


