Abstract
Background:
To our knowledge, no meta-analyses or reviews have investigated the efficacy and safety of metformin on cardiovascular outcomes after acute myocardial infarction (AMI) in patients with type 2 diabetes mellitus (T2DM). We thus conduct a high-quality systematic review and meta-analysis to assess the efficacy and safety of metformin on cardiovascular outcomes after AMI in patients with T2DM.
Methods:
In this systematic review and meta-analysis, we will search PUBMED, Scopus, EMBASE, and Cochrane Library databases through April, 2021. The study is structured to adhere to PRISMA guidelines (i.e., Preferred Reporting Items for Systematic Reviews and Meta-analyses). The literature search, data extraction, and quality assessments are conducted independently by 2 authors. Outcome measures include all-cause mortality; complications such as acute kidney injury, lactic acidosis, hospitalization for AMI or stroke, or death. Where disagreement in the collection of data occurs, this is resolved through discussion. Review Manager Software (v 5.3; Cochrane Collaboration) is used for the meta-analysis. Two independent reviewers will assess the risk of bias of the included studies at study level.
Results:
It is hypothesized that metformin use at the post-AMI is associated with decreased risk of cardiovascular disease and death in patients with T2DM.
Conclusions:
This study expects to provide credible and scientific evidence for the efficacy and safety of metformin on cardiovascular outcomes after AMI in patients with T2DM.
Registration number:
10.17605/OSF.IO/S3MBP.
Keywords: acute myocardial infarction, meta-analysis, metformin, protocol, type 2 diabetes mellitus
1. Introduction
Type 2 diabetes mellitus (T2DM) is a very common chronic disease worldwide that is associated with an increased risk of mortality and cardiovascular mortality. The incidences of T2DM, tumor, cardiac, and cerebral vascular diseases in China occupy the top 3 in the noncommunicable diseases.[1,2] Meanwhile, T2DM is cardiovascular “risk equivalents,” with acute myocardial infarction (AMI) being the most common among T2DM complications. Intensive glucose control demonstrates decreased development of microvascular complications and even macrovascular complication with early intervention.[3]
Metformin, an oral antidiabetic drug of the biguanide class, exerts its effect by increasing gluconeogenesis and peripheral glucose uptake. A large randomized, multicenter trial showed that metformin users had a lower risk of AMI compared with participants on the diet alone.[4] Moreover, despite achieving similar glycemic control, metformin users had lower all-cause and cardiovascular mortality than sulfonylurea and insulin users. However, the role of metformin in reducing cardiovascular disease remains controversial, and in recent meta-analyses, no cardiovascular results have reached statistical significance.[6–8]
Nevertheless, the potential of metformin to confer acute cardioprotective effects in AMI has been well established in the preclinical literature. It has been hypothesized that the favorable effects of pretreatment with metformin in patients with AMI relate to cardioprotection against IRI, independent of its hypoglycaemic actions.[9,10] However, to our knowledge, no meta-analyses or reviews have investigated the efficacy and safety of metformin on cardiovascular outcomes after AMI in patients with T2DM. We thus conduct a high-quality systematic review and meta-analysis to assess the efficacy and safety of metformin on cardiovascular outcomes after AMI in patients with T2DM. It is hypothesized that metformin use at the post-AMI is associated with decreased risk of cardiovascular disease and death in patients with T2DM.
2. Materials and methods
2.1. Study registration
The systematic review protocol has been registered on Open Science Framework registries. The registration number is 10.17605/OSF.IO/S3MBP. The systematic literature review is structured to adhere to PRISMA guidelines (i.e., preferred reporting items for systematic reviews and meta-analyses), which include requirements deemed essential for the transparent reporting of results. Ethical approval and patient consent are not required because this study is a literature-based study. We will update our protocol for any changes in the entire research process if needed.[11]
2.2. Data sources and search strategy
We will search PUBMED, Scopus, EMBASE, and Cochrane Library databases through April, 2021. Search algorithm are identified as follows: (type 2 diabetes) OR (diabetes mellitus) OR (DM) AND (acute myocardial infarction) OR (AMI) AND (metformin). The literature search, data extraction, and quality assessments are conducted independently by 2 authors. We also search references cited in all included articles to avoid missing other relevant articles. If the effective data are not included in the original articles, we will contact the authors to get them. The studies are screened and evaluated by 2 authors independently for eligibility. Flow diagram of study identification is shown in Figure 1.
Figure 1.
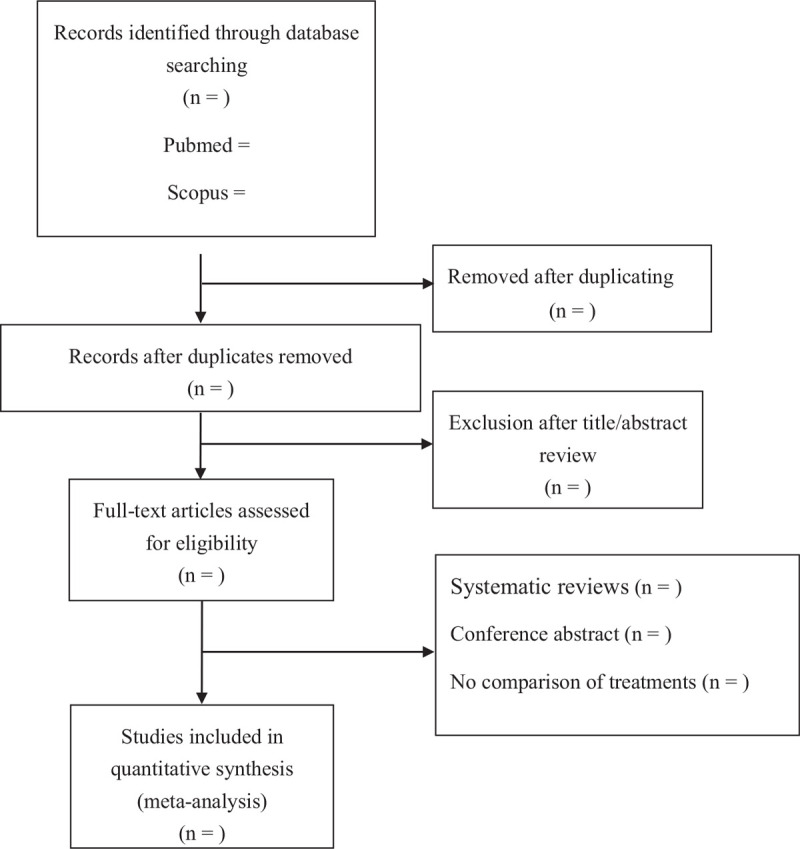
Flow diagram of study identification.
2.3. Eligibility criteria
The study included in our meta-analysis have to meet all of the following inclusion criteria:
-
1.
all clinical trials to assess the efficacy and safety of metformin in the treatment of T2DM after AMI were considered eligible for analysis;
-
2.
adult T2DM patients with a duration of at least 12 weeks (with a glycated hemoglobin level of 7.0% or more);
-
3.
comparing metformin with another antidiabetic therapy or placebo, the cases with metformin treatment and controls with another antidiabetic therapy or placebo;
-
4.
reporting the available data on cardiovascular events.
Studies with overlapping data or insufficient data to calculate or extract effect estimates will be excluded. Case reports, biochemical trials, letters, and reviews will also be eliminated. Articles are exported to EndNote, and duplicates remove. Two independent authors screen the titles and abstracts of potentially relevant studies to determine their eligibility based on the criteria.
2.4. Data extraction
Two independent authors extract the following descriptive raw information from the selected studies: study characteristics such as author, publication year, study design; patient demographic details such as patients’ number, average age, body mass index, and gender ratio. Outcome measures include all-cause mortality; complications such as acute kidney injury, lactic acidosis, hospitalization for AMI or stroke, or death. Where disagreement in the collection of data occurs, this is resolved through discussion. If the data are missing or can not be extracted directly, we will contact the corresponding authors to ensure that the information integrated. If necessary, we will abandon the extraction of incomplete data.
2.5. Statistical analysis
Review Manager software (v 5.3; Cochrane Collaboration) is used for the meta-analysis. Extracted data are entered into Review Manager by the first independent author and checked by the second independent author. Risk ratio with a 95% confidence interval or standardized mean difference with 95% CI are assessed for dichotomous outcomes or continuous outcomes, respectively. The heterogeneity is assessed by using the Q test and I2 statistic. An I2 value of <25% is chosen to represent low heterogeneity and an I2 value of >75% to indicate high heterogeneity. All outcomes are pooled on random-effect model. A P value of <.05 is considered to be statistically significant.
2.6. Quality assessment
In order to achieve a consistency (at least 80%) of risk of bias assessment, the risk of bias assessors will preassess a sample of eligible studies. Results of the pilot risk of bias will be discussed among review authors and assessors. Two independent reviewers will assess the risk of bias of the included studies at the study level. We will follow the guidance in the latest version of Cochrane Handbook for systematic reviews of interventions when choosing and using tools to assessing risk of bias for randomized trials (version 2 of the Cochrane risk of bias tool for randomized trials, RoB 2) and nonrandomized trials (the Risk Of Bias In nonrandomized Studies of Interventions, ROBINS-I tool). Any disagreements will be discussed and resolved in discussion with a third reviewer. Studies with high risk of bias or unclear bias will be given less weight in our data synthesis.
3. Discussion
T2DM is a chronic metabolic disorder that results from defects in both insulin secretion and insulin action. Meanwhile, T2DM is cardiovascular “risk equivalents,” with AMI being the most common among T2DM complications. To our knowledge, no meta-analyses or reviews have investigated the efficacy and safety of metformin on cardiovascular outcomes after AMI in patients with T2DM. We thus conduct a high-quality systematic review and meta-analysis to assess the efficacy and safety of metformin on cardiovascular outcomes after AMI in patients with T2DM. It is hypothesized that metformin use at the post-AMI is associated with decreased risk of cardiovascular disease and death in patients with T2DM. The results of this research will be delivered in a peer-reviewed journal. This study expects to provide credible and scientific evidence for the efficacy and safety of metformin on cardiovascular outcomes after AMI in patients with T2DM.[5]
Author contributions
Conceptualization: Jun Yang.
Data curation: Chuanwen Shen, Shuying Tan.
Formal analysis: Chuanwen Shen, Shuying Tan.
Funding acquisition: Jun Yang.
Investigation: Chuanwen Shen, Shuying Tan.
Methodology: Jun Yang.
Resources: Jun Yang.
Software: Chuanwen Shen, Shuying Tan.
Supervision: Jun Yang.
Validation: Chuanwen Shen, Shuying Tan.
Visualization: Shuying Tan.
Writing – original draft: Chuanwen Shen, Shuying Tan.
Writing – review & editing: Jun Yang.
Footnotes
Abbreviations: AMI = acute myocardial infarction, T2DM = type 2 diabetes mellitus.
How to cite this article: Shen C, Tan S, Yang J. Effects of continuous use of metformin on cardiovascular outcomes in patients with type 2 diabetes after acute myocardial infarction: a protocol for systematic review and meta-analysis. Medicine. 2021;100:15(e25353).
CS and ST equally contributed to the study.
This study was supported by Chongqing Qianjiang District Science And Technology Bureau Project (2019016).
The authors report no conflicts of interest.
Data sharing not applicable to this article as no datasets were generated or analyzed during the current study.
References
- [1].Roumie CL, Hung AM, Greevy RA, et al. Comparative effectiveness of sulfonylurea and metformin monotherapy on cardiovascular events in type 2 diabetes mellitus: a cohort study. Ann Intern Med 2012;157:601–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Gurung RL, Yiamunaa M, Liu S, et al. Association of haptoglobin phenotype with incident acute myocardial infarction in Chinese patients with type 2 diabetes. Cardiovasc Diabetol 2019;18:65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Mizuno M, Kuno A, Yano T, et al. Empagliflozin normalizes the size and number of mitochondria and prevents reduction in mitochondrial size after myocardial infarction in diabetic hearts. Physiol Rep 2018;6:e13741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Korkmaz-Icöz S, Vater A, Li S, et al. Mild type 2 diabetes mellitus improves remote endothelial dysfunction after acute myocardial infarction. J Diabetes Complications 2015;29:1253–60. [DOI] [PubMed] [Google Scholar]
- [5].Bromage DI, Godec TR, Pujades-Rodriguez M, et al. Metformin use and cardiovascular outcomes after acute myocardial infarction in patients with type 2 diabetes: a cohort study. Cardiovasc Diabetol 2019;18:168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Cho EH, Han K, Kim B, et al. Gliclazide monotherapy increases risks of all-cause mortality and has similar risk of acute myocardial infarction and stroke with glimepiride monotherapy in Korean type 2 diabetes mellitus. Medicine (Baltimore) 2020;99:e21236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Oidor-Chan VH, Hong E, Pérez-Severiano F, et al. Fenofibrate plus metformin produces cardioprotection in a type 2 diabetes and acute myocardial infarction model. PPAR Res 2016;2016:8237264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Yu Q, Zhu JJ, Liu WX. Effect of continuous use of metformin on kidney function in diabetes patients with acute myocardial infarction undergoing primary percutaneous coronary intervention. BMC Cardiovasc Disord 2020;20:187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Jil M, Rajnikant M, Richard D, et al. The effects of dual-therapy intensification with insulin or dipeptidylpeptidase-4 inhibitor on cardiovascular events and all-cause mortality in patients with type 2 diabetes: A retrospective cohort study. Diab Vasc Dis Res 2017;14:295–303. [DOI] [PubMed] [Google Scholar]
- [10].Mellbin LG, Malmberg K, Norhammar A, et al. DIGAMI 2 Investigators. Prognostic implications of glucose-lowering treatment in patients with acute myocardial infarction and diabetes: experiences from an extended follow-up of the Diabetes Mellitus Insulin-Glucose Infusion in Acute Myocardial Infarction (DIGAMI) 2 Study. Diabetologia 2011;54:1308–17. [DOI] [PubMed] [Google Scholar]
- [11].Moher D, Liberati A, Tetzlaff J, et al. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ 2009;339:2535. [PMC free article] [PubMed] [Google Scholar]


