Abstract
Obesity is associated with detrimental changes in cardiovascular and metabolic parameters, including blood pressure, dyslipidemia, markers of systemic inflammation, and insulin resistance. In the elderly living with the human immunodeficiency virus (EPLHIV), and being treated with antiretroviral medications, the obesity complications escalate and expose the elderly to the risk of noncommunicable diseases. Given that over 3 million EPLHIV in sub-Sahara Africa, we assessed the prevalence of obesity and its associated factors among EPLHIV in a low-resource setting.
This was a cross sectional study of EPLHIV aged 50 years and older, being treated with antiretroviral medications from 2004 to 2018. HIV treatment data collected from multiple treatment sites were analyzed. Baseline characteristics of the participants were described, and multivariable relative risk model was applied to assess the associations between obesity (body mass index [BMI] ≥30 kg/m2) and the prespecified potential risk factors.
Of the 134,652 in HIV cohort, 19,566 (14.5%) were EPLHIV: 12,967 (66.3%) were normal weight (18.5 ≤ BMI < 25), 4548 (23.2%) were overweight (25 ≤ BMI < 30), while 2,051 (10.5%) were obese (BMI ≥30). The average age the normal weight (57.1; standard deviation 6.6) and the obese (56.5; standard deviation 5.5) was similar. We observed that being an employed (relative risk [RR] 1.71; 95% confidence interval [CI] 1.48–2.00; P < .001), educated (RR 1.93; 95% CI 1.54–2.41; P < .001), and presence of hypertension (RR 1.78; 95% CI 1.44–2.20; P < .001), increased the risk of obesity. Also, being male (RR 0.38; 95% CI 0.33–0.44; P < .001), stages III/IV of the World Health Organization clinical stages of HIV (RR 0.58; 95% CI 0.50–0.68; P < .001), tenofovir-based regimen (RR 0.84; 95% CI 0.73–0.96, P < .001), and low CD4 count (RR 0.56; 95% CI 0.44–0.71; P < .001) were inversely associated with obesity.
This study demonstrates that multiple factors are driving obesity prevalence in EPLHIV. The study provides vital information for policy-makers and HIV program implementers in implementing targeted-interventions to address obesity in EPLHIV. Its findings would assist in the implementation of a one-stop-shop model for the management of HIV and other comorbid medical conditions in EPLHIV.
Keywords: elderly, human immunodeficiency viruses/acquired immunodeficiency syndrome, low-resource setting, obesity, prevalence, risk-factors
1. Introduction
Obesity – the abnormal or excessive fat accumulation that may impair health[1] is a leading risk factor for global deaths; about 3.4 million adults die each year as a result of obesity.[2] In addition, 44% of the diabetes burden, 23% of the ischaemic heart disease burden, and between 7% and 41% of certain cancer burdens are attributable to obesity.[2] In 2016, more than 1.9 billion adults (18 years and older) were overweight, out of which, over 650 million were obese.[1] It has been estimated that by 2030, over 1.12 billion people would be obese worldwide, with sub-Sahara Africa (SSA) projected to account for 6.6% of the global burden.[3] However, these estimates may be exceeded because the factors that are driving the prevalence of obesity cut across genetics, age, wealth, alcohol consumption, physical inactivity, and consumption of unsaturated fat.[4] Most of these factors are being promoted in western societies and have been referred to as the western lifestyle, although emerging modern African societies are also facing these problems.[5]
The health-related conditions that have been linked with obesity include noncommunicable diseases, such as diabetes, cardiovascular diseases, high cholesterol, asthma, and arthritis.[6] Also, studies have shown that human immunodeficiency viruses (HIV)[7] antiretroviral medications (ARVs) are major risk factors for noncommunicable diseases. The ARVs do not have the same level of risk but some of the main drug classes that are used in combination antiretroviral therapy for treating HIV including nucleoside reverse transcriptase inhibitors, integrase strand transfer inhibitor and the protease inhibitors, promote obesity through complex mechanisms that are poorly understood.[8,9] Thus, the elderly who are living with HIV and on ARVs have multiple risks of obesity through the combined effect of aging, HIV, and the ARVs.
The prevalence of obesity in people living with HIV has been reported in the literature.[10–12] As antiretroviral therapy (ART) scale-up increased in the 1990s, there was a corresponding global increase in the prevalence of cardio-metabolic disorders, which include obesity.[13] A large multi-center, retrospective cohort study conducted in high-resource settings that included 14,084 participants who were followed up for 12 years, the authors found that the median body mass index (BMI) at ART initiation increased from 23.8 kg/m2 to 24.8 kg/m2 and the percentage of people with obesity at ART initiation increased from 9% to 18%.[12] After 3 years of ART initiation, 22% of the participants with normal BMI at ART initiation became overweight, and 18% of the overweight at baseline became obese.[12] In the sub-Saharan Africa region, a meta-analysis that included 29,755 individuals, found that ART was associated with higher low-density lipoprotein, high-density lipoprotein, and lower glycated hemoglobin in HIV positive individuals.[14]
The prevalence of HIV-infection among individuals older than 50 years of age is increasing regardless of geographical regions.[15,16] In SSA, it is estimated that approximately 3 million people older than 50 years are HIV infected, equivalent to an average of 14% of the adult HIV-infected populations and 11% of adults on ART.[17,18] In Nigeria, 54% of the 3.4 million people living with the HIV in 2012 were between 15 years and 64 years,[19] but given the effectiveness of ART at prolonging life, it is estimated that over 40% of the 3.4 million people will be 50 years and above in a few years.
With the increased prevalence of HIV-infections among older individuals and the complications associated with obesity in old age, it is important to identify factors associated with obesity among the elderly people living with HIV (EPLHIV) in Nigeria. To date, no study in Nigeria has examined obesity in the EPLHIV; all the previous studies overwhelmingly focused on obesity in the general population or on specific subpopulation, such as health services providers, market women.[20–22] Considering the huge population of EPLHIV in Nigeria,[23] the ambitious target to end HIV by 2030 and scarcity of information on obesity in EPLHIV, this study seeks to estimate the prevalence of obesity among EPLHIV and identify its associated factors.
2. Methods
2.1. Study design
This was a cross sectional study of ELPHIV being treated with ARVs from 2004 to 2018 in Nigeria. The study population includes ELPHIV who have attained at least 50 years at the time of enrollment in ART at the health facility. The analysis involved baseline data of the participants at the time of enrolment into the study.
2.2. Setting
The Institute of Human Virology Nigeria (IHVN) started implementing the United States President Emergency Plan for acquired immunodeficiency syndrome (AIDS) Relief with a Cooperative Agreement awarded by the U.S. Centers for Disease Control and Prevention to the University of Maryland School of Medicine's Institute of Human Virology in 2004 to support the government's free ART access program. Comprehensive HIV treatment and laboratory services were provided across all the IHVN supported health facilities in collaboration with the National Agency for the Control of AIDS – the agency regulating the control of HIV/AIDS under the Nigeria Federal Ministry of Health.
2.3. Data source
Since 2004 IHVN has supported a network of over 500 health facilities across the 6 regions in Nigeria to provide HIV treatment and care to people living the virus. All patient-level data from the health facilities are transmitted and stored in the central database with over 2 million entries, managed by the data management team. The database covers all HIV patients who are receiving HIV treatment and care from 2004 to 2018. Individuals were consecutively enrolled at first contact with an HIV treatment center. Collected data includes demographics, height, weight, date of HIV diagnosis, date of initiating therapy, AIDS-defining events, antiretroviral treatment, BMI, blood pressure, CD4 cell counts, HIV ribonucleic acid measurements, and other laboratory investigations.
2.4. Prespecified risk factors
The World Health Organization (WHO) generally applies 60 years and over as a statistical cut-off for old age.[24] However, for various reasons, some analyses refer to populations of different ages such as 50 years and over, 65 years and over or 80 years and over. Considering the life expectancy of people living in low resource settings such as Nigeria, we adopted ≥50 years as the cut-off for old age in this study. Participants who were ≥50 years at the time of testing positive to HIV were classified as elderly. Age was categorized as 50 to <60 years, 60 to <70 years, and 70 years and over. The marital status of the participants was classified as single, married, widowed, divorced, and separated. Educational attainment of the participants was categorized as no education, attended qur’anic, primary, secondary, and postsecondary. The ART regimens of the study population were classified as zidovudine (AZT)-, tenofovir (TDF)-based regimen and others.
2.5. Outcome
This study examined obesity as the outcome of interest. BMI is an index of weight-for-height that is commonly used to classify obesity in adults. It is defined as a person's weight in kilograms divided by the square of his height in meters (kg/m2). The WHO defined obesity as BMI of ≥30 kg/m2.[1] We adopted the WHO definition of obesity in this study.
2.6. Statistical analysis
The analysis included a total of 15,018 EPLHIV were available in the geriatrics cohort between 2004 and 2018. Chi-square and Wilcoxon tests were used to test for differences in the prevalence of obesity and potential risk factors. Univariable and multivariable relative risk models were used to assess the associations between obesity (BMI ≥30 kg/m2) and the prespecified potential risk factors. Log-binomial regression was used for the univariable regression model. However, when the multivariate log-binomial regressions did not converge, we applied multivariable Poisson regression model with robust error variance to estimate the relative risk of being obese. All variables in the univariable analyses were included in the multivariate models. We used the missing indicator method and set continuous variables to the mean value for missing covariates. All analyses were performed using SAS software version 9.3 (SAS Institute, Inc, Cary, NC). P-values < .05 were considered statistically significant.
2.7. Ethics approval and consent to participate
Ethical clearance for the use of routine HIV care was obtained from the National Health Research Ethics Committee of Nigeria (NHREC/01/01/2007-18/12/2019C). Informed consent was not obtained from the participants because we analyzed routine HIV care data and ethical approval to utilize the data had already been secured from the National Health Research Ethics Committee of Nigeria before the implementation of HIV treatment and care.
3. Results
Figure 1 shows the number of elderly patients living with HIV who were enrolled to care from 2004 to 2018, and those included in the analysis of this study. Of the cohort of 19,566 EPLHIV, (12,967 [66.3%]), had normal weight, 4548 (23.2%) were overweight and 2051 (10.5%) were obese. Overweight patients were excluded from the analysis in line with the study objectives. The baseline characteristics of the remaining participants are presented in Table 1. We included 15,018 EPLHIV in the analysis, and 12,967 (86%) of them have a normal weight (18.5 ≤ BMI < 25) while the remaining 2051 (14%) were obese (BMI ≥30). The average age of the patients with normal weight was 57.1 years (standard deviation [SD] = 6.6) while that of obese patients was 56.5 years (SD = 5.5). Nearly 3-quarters of the normal weight 72.1% (9347) and obese 72.3% (3287) patients were between 50 to 60 years.
Figure 1.
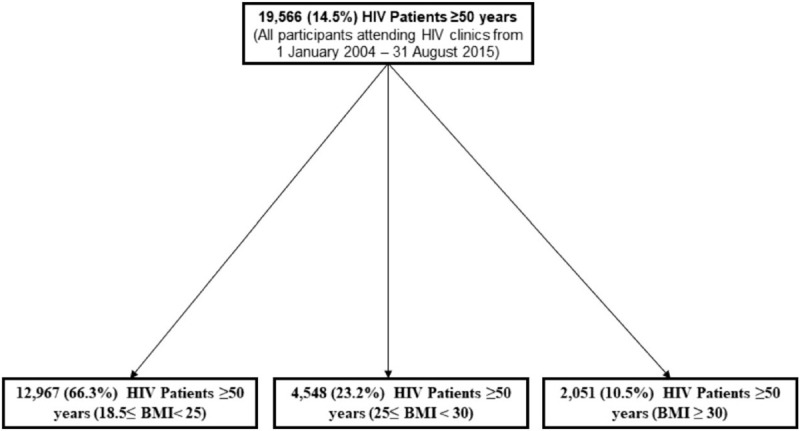
Flowchart of the study participants.
Table 1.
Baseline characteristics of elderly patients living with HIV/AIDS in Nigeria (N = 15,018).
| Variable | Normal weight (18.5 ≤ BMI < 25; N = 12967)∗ | Obese (BMI ≥30; N = 2015)∗ | P-value | Total participants (N = 15,018) |
| Socio-demographics | ||||
| Age (yr), mean (SD) | 57.1 (6.6) | 56.5 (5.5) | <.001 | 56.9 (6.4) |
| Age categories (yr) (%) | .09 | |||
| 50 – <60 | 9347 (72.1%) | 1510 (73.6%) | 10,857 (72.3%) | |
| 60 – <70 | 2881 (22.2%) | 473 (23.1%) | 3354 (22.3%) | |
| 70 and above | 739 (5.7%) | 68 (3.3%) | 807 (5.4%) | |
| Gender (%) | ||||
| Female | 6562 (50.6%) | 1402 (68.4%) | <.001 | 7964 (53.0%) |
| Male | 6405 (49.4%) | 649 (31.6%) | 7054 (47.0%) | |
| Marital status (%) | ||||
| Single | 583 (5.1%) | 79 (4.3%) | .009 | 662 (5.0%) |
| Married | 8099 (70.4%) | 1274 (69.5%) | 9.373 (70.3%) | |
| Widowed | 2101 (18.3%) | 354 (19.3%) | 2455 (18.4%) | |
| Divorced | 304 (2.6%) | 58 (3.2%) | 362 (2.7%) | |
| Separated | 422 (3.7%) | 67 (3.7%) | 489 (3.6%) | |
| Occupation (%) | ||||
| Unemployed | 5266 (49.9%) | 908 (56.2%) | <.001 | 6174 (50.7%) |
| Employed | 5287 (50.1%) | 707 (43.8%) | 5994 (49.3%) | |
| Education (%) | ||||
| None | 1832 (17.9%) | 212 (13.1%) | <.001 | 2044 (17.2%) |
| Quranic | 233 (2.3%) | 10 (0.6%) | 243 (2.1%) | |
| Primary | 2919 (28.5%) | 397 (24.5%) | 3316 (28.0%) | |
| Secondary | 3271 (32.0%) | 565 (34.9%) | 3836 (32.4%) | |
| Postsecondary | 1973 (19.3%) | 434 (26.8%) | 2407 (20.3%) | |
| Service entry point (%) | ||||
| HCT | 2177 (44.3%) | 267 (36.0%) | .003 | 2444 (43.3%) |
| VCT | 665 (13.5%) | 132 (17.8%) | 797 (14.1%) | |
| Others | 2068 (42.1%) | 342 (46.2%) | 2410 (42.6%) | |
| Clinical | ||||
| WHO clinical stage (%) | ||||
| I | 5415 (46.3%) | 1125 (61.2%) | <.001 | 6540 (61.2%) |
| II | 3135 (26.8%) | 384 (20.9%) | 3519 (20.9%) | |
| III | 2675 (22.9%) | 286 (15.7%) | 2961 (15.7%) | |
| IV | 466 (4.0%) | 43 (2.4%) | 509 (2.4%) | |
| BP systolic (mm Hg), mean (SD) | 123.3 (25.0) | 132.1 (23.9) | <.001 | 125.6 (24.7) |
| BP diastolic (mm Hg),mean (SD) | 78.5 (14.2) | 84.1 (14.5) | <.001 | 80.0 (14.3) |
| Hypertension (SBP >140 or DPB >90 mm Hg) (%) | 1013 (22.4%) | 320 (34.2%) | <.001 | 1333 (24.4%) |
| ART regimen line (%) | .11 | |||
| First line | 12,493 (98.5%) | 1978 (98.6%) | 14,471 (98.5%) | |
| Second line | 192 (1.5%) | 29 (1.4%) | 221 (1.5%) | |
| ART regimen (%) | ||||
| AZT-based | 2987 (25.4%) | 575 (30.3%) | <.001 | 3562 (26.2%) |
| TDF-based | 7672 (65.5%) | 1161 (61.2%) | 8833 (64.9%) | |
| Others | 1062 (9.1%) | 161 (8.5%) | 1223 (9.0%) | |
| CD4 count <500 cells/μL (%) | 4567 (66.0%) | 541 (47.5%) | <.001 | 5108 (63.4%) |
Almost half 47% (7054) of the participants were female. More female 1402 (68.4%) were obese than male 649 (31.6%), while the proportion of normal weight was more or less equal among males and females. The proportion of unemployment among the obese patients 56.2% (908) was higher compared with that of normal-weight patients 49.9% (5266). The majority of obese 82.1% (11,135) and normal weight 86.9% (1839) patients have at least qur’anic or primary school education. More than two-thirds of the obese 70.4% (8,099) and normal weight 69.5% (1274) patients were married. The proportion of patients with WHO clinical stage I was more predominant in the obese patients 61.2% (1125) than normal-weight patients 46.3% (5415), whereas a higher proportion of normal patients have WHO Clinical stage II, III, and IV than obese patients. The average CD4 count among the obese patients 547 (SD 308) was higher than that of normal-weight patients 427 (SD 283). The proportion of obese patients who were hypertensive (SBP >140 and DBP >90 mm Hg) was higher than that of normal-weight patients. More than 98% of the patients were on the first-line regimen, and majority of them were placed on TDF based regimen (normal-weight 7672 [65.5%] and obese 1161 [61.2%]).
Table 2 presents the results of the univariable and multivariable relative risk models that estimated the crude and the adjusted associations between the prespecified risk factors and obesity. Being male reduced the risk of obesity by 62% (RR 0.38; 95% CI 0.33–0.44; P-value < .001) while the likelihood of obesity among employed patients increased by 71% (RR 1.71; 95% CI 1.48–2.00; P-value < .001) when other confounding factors were considered. Higher educational attainment also increased the risk of obesity, such that patients with secondary education had a 48% (RR 1.48; 95% CI 1.20–1.82; P-value < .001) of the risk of obesity while the risk of obesity among those who attained postsecondary education was 93% (RR 1.93; 95% CI 1.54–2.41; P-value < .001) after adjusting for other confounding factors. Patients with the advanced WHO clinical disease stage III/IV were less likely to be obese (RR 0.58; 95% CI 0.50–0.68; P-value < .001) compared with those having normal weight after other confounding factors were considered. Being on TDF based regimen reduced the risk of obesity by 16% (RR 0.84; 95% CI 0.73–0.96; P-value < .001) compared with those on the AZT based regimen after considering confounding factors. The likelihood of having obesity increased by 78% (RR 1.78; 95% CI 1.44–2.20; P-value < .001) among hypertensive patients (SBP >140 and DBP >90 mm Hg) than in normotensive patients. CD4 count was observed to be inversely related with the risk of obesity; having CD4 count of <200 cells/μL and <500 cells/μL reduced the risk of obesity by 44% (RR 0.56; 95% CI 0.44–0.71; P-value < .001) and 44% (OR 0.56; 95% CI 0.49–0.66; P-value < .001) respectively.
Table 2.
Risk factors for obesity (BMI ≥30) among obese and normal-weight elderly patients living with HIV/AIDS in Nigeria.
| UnivariateRR (95% CI), P-value | MultivariateRR (95% CI), P-value | |
| Socio-demographics | ||
| Age categories (yr) | ||
| 50 – <60 | Reference | Reference |
| 60 – <70 | 0.92 (0.82–1.03), .14 | 0.94 (0.80–1.10), .42 |
| 70 and above | 0.56 (0.43–0.72), .047 | 0.82 (0.59–1.13), .22 |
| Gender | ||
| Female | Reference | Reference |
| Male | 0.47 (0.43–0.52), <.001 | 0.38 (0.33–0.44), <.001 |
| Married | ||
| No | Reference | Reference |
| Yes | 0.96 (0.86–1.07), .47 | 1.10 (0.95–1.26), .21 |
| Occupation | ||
| Unemployed | Reference | Reference |
| Employed | 1.63 (1.44–1.83), <.001 | 1.71 (1.48–2.00), <.001 |
| Education | ||
| None | Reference | Reference |
| Primary | 1.12 (0.94–1.33), .22 | 1.14 (0.92–1.41), .23 |
| Secondary | 1.49 (1.26–1.77), <.001 | 1.48 (1.20–1.82), <.001 |
| Postsecondary | 1.90 (1.59–2.27), <.001 | 1.93 (1.54–2.41), <.001 |
| Service entry point | ||
| Others | Reference | Reference |
| HCT/VCT | 0.85 (0.73–0.99), .035 | 0.95 (0.76–1.17), .62 |
| Clinical | ||
| WHO clinical stage | ||
| I/II | Reference | Reference |
| III/IV | 0.59 (0.53–0.67), <.001 | 0.58 (0.50–0.68), <.001 |
| ART regimen | ||
| AZT-based | Reference | Reference |
| TDF-based | 0.79 (0.71–0.88), <.001 | 0.84 (0.73–0.96), <.001 |
| Hypertension (SBP >140 or DPB >90 mm Hg) | ||
| No | Reference | Reference |
| Yes | 1.80 (1.55–2.10), <.001 | 1.78 (1.44–2.20), <.001 |
| CD4 count, cells/μL | ||
| ≥500 | Reference | Reference |
| <500 | 0.46 (0.41–0.53), <.001 | 0.56 (0.49–0.66), <.001 |
4. Discussion
This large cross sectional study reveals the burden of obesity in EPLHIV and demonstrates that obesity is being driven by multiple risk factors in a low-resource setting. We observed obesity in 1 out of 10 EPLHIV. An estimate that could be 2 to 6-fold higher than that of the general population of elderly people in Nigeria.[22,25,26] This partly explains the higher occurrence of cardio-metabolic diseases in EPLHIV than the general population of elderly people. As observed in this study, a high prevalence of obesity in EPLHIV had been reported in other settings.[9,27]
Furthermore, this study confirmed that being an elderly male patient on ART reduced the risk of obesity. The observed association is consistent with the findings from previous studies that examined weight gain after ART initiation in SSA and western countries.[11,28] The underlying mechanism driving this observation is yet to be fully established; however, plausible explanation for the high occurrence of obesity in female has been attributed to a complex interplay of multiple factors including inflammatory, immunologic, genetic, and hormonal factors.[29–32] Whether these factors are playing out in our setting is an observation that need to be investigated. Recent findings from both cross-sectional and prospective studies overwhelmingly support our observation,[11,28,33] a couple of studies conducted some years ago among patients on antiretroviral drugs that have now been abandoned yielded conflicting associations.[12,34] But since the medications that were examined in such studies are no longer in use, our findings present a surer hope for the elderly given that our findings are based on existing medications that are likely to remain relevant for many years to come.
Also, in this study, obesity was found to have a positive association with the occupational status of the participants. Employed EPLHIV were more prone to obesity than their unemployed counterparts. In low-resource settings like ours, the observed relationship between employment and obesity is not counterintuitive as this observation could be explained by the lack of access to good nutrition among unemployed EPLHIV as most unemployed people in low-resource settings do not receive social security benefits from the government whereas employed EPLHIV will have more than enough food to consume. To the best of our knowledge, this is the first study that examined this relationship in EPLHIV as most studies that examined the effect of unemployment in HIV patients on ART mainly reported on the risk of death and HIV disease progression.[35–37]
Education was also implicated: educated EPLHIV were more likely to be obese than the uneducated. The plausible explanation for this relationship could be that the educated people in low-resource settings live in opulence and are adopting an unhealthy dietary lifestyle of the Western world as a way of displaying their affluence. It has already been established that unhealthy lifestyle as seen in the western countries is a major risk factor for obesity.[38–40] Interestingly, the educated people in the Western world are shifting away from an unhealthy lifestyle because of its detrimental effects.[41]
Patients in the early stage of the WHO clinical stage of HIV/AIDS (stage I/II) were more likely to be obese than their counterparts at later stages and this is consistent with other findings.[11] This observation could be explained by the fact that the fact that EPLHIV who are at the EPLHIV in the later stage of the WHO clinical stage of HIV/AIDS (stage III/IV) are more likely to be immunocompromised with co-existing opportunistic infections, which in turn increase the energy expenditure and may be complicated with anorexia, vomiting, malabsorption, and increased nutritional losses through urine, feces, and skin.[42–44] As reported by several previous studies, our study found a positive relationship between CD4 count and obesity.[12,28] As expected, HIV-infected patients with a low CD4 count have a higher risk of opportunistic infections and disease progression, which will eventually lead to weight loss through increased energy consumption and nutritional losses.[42–44]
Moreover, in-line with the common medical knowledge and previous findings, we observed a significant association between hypertension and obesity.[45–47] The observed relationship between obesity and hypertension has been well established. Studies have explained that obesity will lead to atherosclerosis and arterial wall thickening, which may worsen in the presence of HIV infection.[48,49] Also, we observed that TDF based regimen has a protective effect on the occurrence of obesity than the AZT based regimen. Our finding is in agreement with a prior study conducted in the Southern part of Africa which showed that AZT based regimen increased the risk of metabolic syndrome more than the TDF based regimen.[50] Besides TDF based regimen, other antiretroviral drugs, including protease inhibitors and integrase strand transfer inhibitors have been found to have a positive association with obesity.[8,9] The protective effect of TDF is encouraging because the WHO recommended current regimen mix, has TDF as a key drug (TDF/Dolutegravir/Lamivudine). Thus, as people mature into older age with TDF as a key component of their regimen, we expect decline in the prevalence of obesity among EPLHIV.
This study has generated important findings that healthcare providers, HIV program implementers, and health policy-makers can utilize to estimate the health needs and improve the quality of health and health outcomes of EPLHIV in Nigeria and other similar settings. As this study provides information on the burden of obesity in EPLHIV, it will serve as a source of vital information on the health need of EPLHIV in Nigeria. We observed that being an employed, educated, female will increase the risk of obesity among the EPLHIV. These findings indicate the importance of deploying multiple interventions, including dietary control, physical activity, health education, and other population-level interventions to reduce the occurrence of obesity in EPLHIV. This will go a long way in reducing the occurrence of obesity-related diseases such as diabetes and hypertension. This study has also revealed an intriguing clinical finding that highlights why healthcare providers should pay attention to all EPLHIV regardless of their BMI. We found that some EPLHIV may appear nonobese but not stable clinically.
It is important to highlight the strengths and weaknesses of this study. It is worth mentioning that this is the largest cross sectional study of EPLHIV in Nigeria and among the first study that mainly examined obesity among EPLHIV in SSA. Further, the study has more than sufficient power to examine the outcome of interest. Also, in this study both genders were well represented and this allows sex-/gender-specific risk factors to be examined. Nevertheless, this study some limitations. Firstly, there was a lack of data on pregnancy, and no information was captured on the use of medications such as contraceptive pills, metformin, and psychiatric drugs that may affect the occurrence of obesity. Also, the possibility of measurement error in the assessment of BMI exist; although we expected such errors to be random. Being a prospective study, in our analysis, BMI could not be assessed repeatedly overtime at a regularly scheduled interval. Besides, potential confounders including diet, financial income, alcohol intake, switching ART regimen, and duration of exposure to ART were not considered.
5. Conclusions
In conclusion, this study has yielded interesting findings. The observed prevalence of obesity in the ELPHIV exceeds the national prevalence of obesity in the elderly. We observed that employed, educated females among EPLHIV are more likely to be obese. Also, the early stage of the WHO clinical stage of HIV infection, CD4 count, TDF-based regimen, and hypertension in EPLHIV were associated with obesity. Our findings emphasize the urgent need to deploy multiple interventions, including dietary control, physical activity, health education, and other population-level interventions to address the occurrence of obesity in EPLHIV.
Acknowledgments
The authors wish to appreciate all HIV program implementers at the Institute of Human Virology, Nigeria and healthcare providers working at the HIV treatment centers where the participants were recruited.
Author contributions
Conceptualization: Patrick Dakum, Gbenga Ayodele Kayode.
Data curation: Patrick Dakum, Yohanna K. Avong, James Okuma, Temilade Sorungbe, Gbenga Ayodele Kayode.
Formal analysis: Patrick Dakum, James Okuma, Gbenga Ayodele Kayode.
Funding acquisition: Patrick Dakum.
Investigation: Patrick Dakum, Gbenga Ayodele Kayode.
Methodology: Patrick Dakum, Yohanna K. Avong, James Okuma, Temilade Sorungbe, Bolajoko Jatau, Nicaise Nedmbi, Michael K. Odutola, Alash’le Abimiku, Charles O. Mensah, Gbenga Ayodele Kayode.
Project administration: Patrick Dakum.
Resources: Patrick Dakum.
Software: Patrick Dakum.
Supervision: Patrick Dakum.
Validation: Patrick Dakum.
Visualization: Patrick Dakum.
Writing – original draft: Patrick Dakum, Yohanna K. Avong, James Okuma, Temilade Sorungbe, Bolajoko Jatau, Nicaise Nedmbi, Michael K. Odutola, Alash’le Abimiku, Charles O. Mensah, Gbenga Ayodele Kayode.
Writing – review & editing: Patrick Dakum, Yohanna K. Avong, James Okuma, Temilade Sorungbe, Bolajoko Jatau, Nicaise Nedmbi, Michael K. Odutola, Alash’le Abimiku, Charles O. Mensah, Gbenga Ayodele Kayode.
Footnotes
Abbreviations: ART = antiretroviral therapy, ARVs = antiretroviral medications, AZT = zidovudine, EPLHIV = elderly people living with HIV, HIV = human immunodeficiency viruses, IHVN = Institute of Human Virology Nigeria, SSA = sub-Sahara Africa, TDF = tenofovir, WHO = World Health Organization.
How to cite this article: Dakum P, Avong YK, Okuma J, Sorungbe T, Jatau B, Nedmbi N, Odutola MK, Abimiku A, Mensah CO, Kayode GA. Prevalence and risk factors for obesity among elderly patients living with HIV/AIDS in a low-resource setting. Medicine. 2021;100:15(e25399).
The authors have no funding and conflicts of interest to disclose.
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
AIDS = acquired immunodeficiency syndrome, ART = antiretroviral therapy, AZT-based = zidovudine-based, BMI = body mass index, BP = blood pressure, HCT = HIV counseling and testing, TDF-based = tenofovir-based, VCT = voluntary counseling and testing, WHO = World Health Organization.
N (%) or mean (SD); P-values from Chi squared-test for categorical variables or Wilcoxon test for continuous variables.
AIDS = acquired immunodeficiency syndrome, ART = ARV therapy, AZT-based = zidovudine-based, BMI = body mass index, DBP = diastolic blood pressure, HCT = HIV counseling and testing, SBP = systolic blood pressure, TDF-based = tenofovir-based, VCT = voluntary counseling and testing, WHO = World Health Organization.
References
- [1].WHO. Obesity and Overweight. Available at: https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight [access date May 17, 2020]. [Google Scholar]
- [2].Food and Agriculture Organization of the United Nations. Obesity and Overweight. Available at: http://www.fao.org/about/meetings/icn2/preparations/document-detail/en/c/253841/ [access date May 17, 2020]. [Google Scholar]
- [3].Kelly T, Yang W, Chen C-S, et al. Global burden of obesity in 2005 and projections to 2030. Int J Obes 2008;32:1431–7. [DOI] [PubMed] [Google Scholar]
- [4].Little M, Humphries S, Patel K, et al. Factors associated with BMI, underweight, overweight, and obesity among adults in a population of rural south India: a cross-sectional study. BMC Obes 2016;3:01–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Mbanya JCN, Motala AA, Sobngwi E, et al. Diabetes in sub-Saharan Africa. Lancet 2010;375:2254–66. [DOI] [PubMed] [Google Scholar]
- [6].Mokdad AH, Ford ES, Bowman BA, et al. Prevalence of obesity, diabetes, and obesity-related health risk factors, 2001. JAMA 2003;289:76–9. [DOI] [PubMed] [Google Scholar]
- [7].Samaras K, Wand H, Law M, et al. Prevalence of metabolic syndrome in HIV-infected patients receiving highly active antiretroviral therapy using International Diabetes Foundation and Adult Treatment Panel III criteria: associations with insulin resistance, disturbed body fat compartmentalisation, elevated C-reactive protein, and [corrected] hypoadiponectinemia. Diabetes Care 2007;30:113–9. [DOI] [PubMed] [Google Scholar]
- [8].Anuurad E, Bremer A, Berglund L. HIV protease inhibitors and obesity. Curr Opin Endocrinol Diabetes Obes 2010;17:478–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Bakal DR, Coelho LE, Luz PM, et al. Obesity following ART initiation is common and influenced by both traditional and HIV-/ART-specific risk factors. J Antimicrob Chemother 2018;73:2177–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Crum-Cianflone N, Roediger MP, Eberly L, et al. Increasing rates of obesity among HIV-infected persons during the HIV epidemic. PloS One 2010;5:01–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Guehi C, Badjé A, Gabillard D, et al. High prevalence of being overweight and obese HIV-infected persons, before and after 24 months on early ART in the ANRS 12136 temprano trial. AIDS Res Ther 2016;13:01–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Koethe JR, Jenkins CA, Lau B, et al. Rising obesity prevalence and weight gain among adults starting antiretroviral therapy in the United States and Canada. AIDS Res Hum Retroviruses 2016;32:50–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Morse CG, Kovacs JA. Metabolic and skeletal complications of HIV infection: the price of success. JAMA 2006;296:844–54. [DOI] [PubMed] [Google Scholar]
- [14].Dillon DG, Gurdasani D, Riha J, et al. Association of HIV and ART with cardiometabolic traits in sub-Saharan Africa: a systematic review and meta-analysis. Int J Epidemiol 2013;42:1754–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Luther VP, Wilkin AM. HIV infection in older adults. Clin Geriatr Med 2007;23:567–83. [DOI] [PubMed] [Google Scholar]
- [16].Manfredi R. HIV infection and advanced age emerging epidemiological, clinical, and management issues. Ageing Res Rev 2004;3:31–54. [DOI] [PubMed] [Google Scholar]
- [17].Greig J, Casas EC, O’Brien DP, et al. Association between older age and adverse outcomes on antiretroviral therapy: a cohort analysis of programme data from nine countries. AIDS Lond Engl 2012;26: Suppl 1: S31–7. [DOI] [PubMed] [Google Scholar]
- [18].Negin J, Cumming RG. HIV infection in older adults in sub-Saharan Africa: extrapolating prevalence from existing data. Bull World Health Organ 2010;88:847–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Nigeria Federal Ministry of Health. 2016 National Guidelines for HIV Prevention, Treatment and Care. Available at: https://www.prepwatch.org/wp-content/uploads/2017/08/nigeria_national_guidelines_2016.pdf [access date May 26, 2020]. [Google Scholar]
- [20].Iwuala SO, Ayankogbe OO, Olatona FA, et al. Obesity among health service providers in Nigeria: danger to long term health worker retention? Pan Afr Med J 2015;22:01–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Chukwuonye II, Chuku A, John C, et al. prevalence of overweight and obesity in adult Nigerians - a systematic review. Diabetes Metab Syndr Obes Targets Ther 2013;6:43–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Iloh GUP, Amadi AN, Nwankwo BO, et al. Obesity in adult Nigerians: a study of its pattern and common primary co-morbidities in a rural Mission General Hospital in Imo state, south-eastern Nigeria. Niger J Clin Pract 2011;14:212–8. [DOI] [PubMed] [Google Scholar]
- [23].Nigeria Federal Ministry of Health. National HIV Sero-prevalence Sentinel Survey Among Pregnant Women Attending Antenatal Clinics in Nigeria. Abuja. Available at: https://naca.gov.ng/ANC_2008_survey.pdf [access date May 18, 2020]. [Google Scholar]
- [24].WHO. Good Health Adds Life to Years. In: WHO [Internet]. World Health Organization. Available at: http://www.who.int/ageing/publications/whd2012_global_brief/en/ [access date May 18, 2020]. [Google Scholar]
- [25].Cadmus EO, Adebusoye LA, Olowookere OO, et al. A descriptive study of the morbidity pattern of older persons presenting at a Geriatric Centre in Southwestern Nigeria. Niger J Clin Pract 2017;20:873–8. [DOI] [PubMed] [Google Scholar]
- [26].Okesina AB, Oparinde DP, Akindoyin KA, et al. Prevalence of some risk factors of coronary heart disease in a rural Nigerian population. East Afr Med J 1999;76:212–6. [PubMed] [Google Scholar]
- [27].Okeke OO, Ogunfowokan O, Moses LA, et al. Overweight and obesity among HIV infected patients in a West African population. Int J Med Biomed Res 2017;6:65–73. [Google Scholar]
- [28].Bares SH, Smeaton LM, Xu A, et al. HIV-infected women gain more weight than HIV-infected men following the initiation of antiretroviral therapy. J Womens Health 2018;27:1162–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29].Abella V, Scotece M, Conde J, et al. Leptin in the interplay of inflammation, metabolism and immune system disorders. Nat Rev Rheumatol 2017;13:100–9. [DOI] [PubMed] [Google Scholar]
- [30].Kelesidis T, Tran TTT, Stein JH, et al. Changes in inflammation and immune activation with atazanavir-, raltegravir-, darunavir-based initial antiviral therapy: ACTG 5260s. Clin Infect Dis Off Publ Infect Dis Soc Am 2015;61:651–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].Bouchard C, Després JP, Mauriège P. Genetic and nongenetic determinants of regional fat distribution. Endocr Rev 1993;14:72–93. [DOI] [PubMed] [Google Scholar]
- [32].Bouchard C. The causes of obesity: advances in molecular biology but stagnation on the genetic front. Diabetologia 1996;39:1532–3. [DOI] [PubMed] [Google Scholar]
- [33].Thompson-Paul AM, Wei SC, Mattson CL, et al. Obesity among HIV-infected adults receiving medical care in the United States: data from the cross-sectional medical monitoring project and National Health and Nutrition Examination Survey. Medicine (Baltimore) 2015;94:01–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [34].Achhra AC, Mocroft A, Reiss P, et al. Short-term weight gain after antiretroviral therapy initiation and subsequent risk of cardiovascular disease and diabetes: the D:A:D study. HIV Med 2016;17:255–68. [DOI] [PubMed] [Google Scholar]
- [35].Cunningham WE, Hays RD, Duan N, et al. The effect of socioeconomic status on the survival of people receiving care for HIV infection in the United States. J Health Care Poor Underserved 2005;16:655–76. [DOI] [PubMed] [Google Scholar]
- [36].McFarland W, Chen S, Hsu L, et al. Low socioeconomic status is associated with a higher rate of death in the era of highly active antiretroviral therapy, San Francisco. J Acquir Immune Defic Syndr 2003;33:96–103. [DOI] [PubMed] [Google Scholar]
- [37].Delpierre C, Cuzin L, Lauwers-Cances V, et al. Unemployment as a risk factor for AIDS and death for HIV-infected patients in the era of highly active antiretroviral therapy. Sex Transm Infect 2008;84:183–6. [DOI] [PubMed] [Google Scholar]
- [38].Kimani-Murage EW, Kahn K, Pettifor JM, et al. The prevalence of stunting, overweight and obesity, and metabolic disease risk in rural South African children. BMC Public Health 2010;10:158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [39].Rossouw HA, Grant CC, Viljoen M. Overweight and obesity in children and adolescents: the South African problem. South Afr J Sci 2012;108:31–7. [Google Scholar]
- [40].Porter P. Westernizing” women's risks? Breast cancer in lower-income countries. N Engl J Med 2008;358:213–6. [DOI] [PubMed] [Google Scholar]
- [41].Fransen HP, Boer JMA, Beulens JWJ, et al. Associations between lifestyle factors and an unhealthy diet. Eur J Public Health 2017;27:274–8. [DOI] [PubMed] [Google Scholar]
- [42].Schaible UE, Kaufmann SHE. Malnutrition and infection: complex mechanisms and global impacts. PLoS Med 2007;4:0806–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [43].Powanda MC, Beisel WR. Metabolic effects of infection on protein and energy status. J Nutr 2003;133:322S–7S. [DOI] [PubMed] [Google Scholar]
- [44].WHO. Nutritional Care for HIV-Infected Children. In: WHO [Internet]. World Health Organization. Available at: http://www.who.int/elena/titles/bbc/nutrition_hiv_children/en/ [access date May 16, 2020]. [Google Scholar]
- [45].Rodríguez-Arbolí E, Mwamelo K, Kalinjuma AV, et al. Incidence and risk factors for hypertension among HIV patients in rural Tanzania - a prospective cohort study. PloS One 2017;12:01–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [46].Benzekri NA, Seydi M, N Doye I, et al. Increasing prevalence of hypertension among HIV-positive and negative adults in Senegal, West Africa. PloS One 2018;13:01–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [47].Brennan AT, Jamieson L, Crowther NJ, et al. Prevalence, incidence, predictors, treatment, and control of hypertension among HIV-positive adults on antiretroviral treatment in public sector treatment programs in South Africa. PloS One 2018;13:01–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [48].Duprez DA, Kuller LH, Tracy R, et al. Lipoprotein particle subclasses, cardiovascular disease and HIV infection. Atherosclerosis 2009;207:524–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [49].Jiang S-Z, Lu W, Zong X-F, et al. Obesity and hypertension. Exp Ther Med 2016;12:2395–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [50].Labhardt ND, Müller UF, Ringera I, et al. Metabolic syndrome in patients on first-line antiretroviral therapy containing zidovudine or tenofovir in rural Lesotho, Southern Africa. Trop Med Int Health TM IH 2017;22:725–33. [DOI] [PubMed] [Google Scholar]


