Abstract
Findings have been mixed regarding the relationship between comorbid depression and anxiety and treatment outcomes for anxious youth. The current study compared a sample of anxious youth with a comorbid depressive disorder (n=20) and those without comorbid depression (n=137). All participants received 16 weekly sessions of Coping Cat and completed measures assessing anxiety/depression severity, impairment, and functioning at pretreatment and posttreatment. Results indicated that anxiety-focused CBT is efficacious for anxious youth with and without comorbid depressive disorders, with a higher rate of symptom improvement for youth with comorbid depression during treatment. However, comorbid depression was associated with higher severity at baseline and after treatment. Thus, despite the higher rate of symptom improvement, anxious youth with comorbid depression may benefit from additional treatment to address remaining symptoms.
Keywords: Anxiety, Depression, Youth, Cognitive Behavioral Therapy
Depression and anxiety are among the most common mental health disorders in youth [1]. Considered separately, anxiety disorders are present in 10–20% of youth [1]. Similarly, depression has a lifetime prevalence of approximately 20% by late adolescence, and 2–6% prevalence at any given time [2]. Among youth diagnosed with an anxiety disorder, 25–28% also exhibit a comorbid depressive disorder [1]. Several models have been proposed to explain the high co-occurrence of the two disorders, which likely arises through one of several possible pathways [3, 4]. With regard to baseline symptoms, youth with comorbid anxiety and depression have been shown to have lower global functioning, greater impairment, poorer family functioning, higher levels of negative affect, and poorer emotion regulation than youth with either disorder alone [5–9]. These indicators of greater severity across several measures are well-documented, but the role of comorbid conditions in predicting anxiety treatment outcomes remains less clear.
Although cognitive behavioral therapy (CBT) for anxiety is considered a well-established treatment [10], approximately one third of youth do not respond to CBT for anxiety. Understanding the role of comorbid conditions on treatment outcomes may provide insights about why some youth do not fully respond to CBT for anxiety and also may have implications for tailoring interventions to an individual child. However, the findings in the literature examining the relationship between comorbid depression and anxiety treatment outcomes are mixed. Several studies have demonstrated a link between comorbid depression and anxiety and poorer anxiety treatment outcomes [11]. In a study by Berman and colleagues [12], youth with primary anxiety diagnoses were divided into treatment success and treatment failure groups based on reductions in primary anxiety disorder severity. Findings indicated that comorbid depression diagnoses predicted treatment failure, and that the treatment failure group scored higher than the treatment success group on the Children’s Depression Inventory (CDI) at pretreatment. Other studies have replicated these findings, with comorbid depression being associated with higher principal anxiety severity at pretreatment, posttreatment, and follow-up [6], less reduction in primary anxiety disorder severity [12], and lower likelihood of remission of primary anxiety diagnoses [13, 14]. Anxious youth with comorbid depressive disorders also have been found to be less likely to be free of their primary anxiety diagnosis at posttreatment, and are rated as more impaired at the end of treatment and at follow-up in terms of anxiety severity, negative thinking, and externalizing symptoms [15]. Despite these findings, children with comorbid depressive disorders who are treated with CBT for anxiety also have been reported to experience a posttreatment reduction in untargeted depressive symptoms [11, 16].
Taken together, the findings present a strong link between comorbid depression and treatment outcomes. Yet, not all findings have been consistent. A study conducted by Southam-Gerow and colleagues [17] found that, although youth with social anxiety separated into “good” and “poor” treatment response groups differed significantly on parent- and teacher-report of depressive symptoms, no difference was found on child report of depressive symptoms. Similarly, studies by Kley, Heinrichs, Bender, and Tuschen-Caffier [18] and Alfano and colleagues[19] both found that child self-report of symptoms on the CDI was not a significant predictor of social anxiety treatment outcomes. In O’Neil and Kendall’s [6] study, although youth with depressive diagnoses had higher anxiety at post-treatment, depression diagnoses did not predict reductions in primary diagnosis severity. When these findings are taken into consideration, the link between comorbid depression and treatment outcomes in anxious youth becomes less clear.
A number of methodological differences may account for the discrepant findings regarding the relationship between comorbid depression and anxiety treatment outcomes. Studies that have examined the relationship between depression and treatment outcomes have varied methodologically, with some studies examining depression at a symptom level (typically self-report), and others examining it at a diagnostic level (based on clinician interview). Some samples are restricted in age, whereas others included a broader age range. Several studies included children with relatively low CDI scores, which may indicate that the lack of significant findings in some studies may be a floor effect. In addition, although many studies have examined the reduction in anxiety symptoms over the course of treatment, to our knowledge, there have not been any studies that specifically examined whether changes in depression symptoms over the course of treatment differ between youth with and without comorbid depression.
The present study (1) reexamines the findings that youth with comorbid anxiety and depressive disorders have more severe baseline characteristics, and (2) conducts a further test of the otherwise mixed findings with regard to treatment outcomes. The present study examined anxious youth treated with Coping Cat, a 16-session CBT protocol with evidence for its efficacy and effectiveness in treating anxiety among youth ages 6–17 [20, 21]. Youth included in this study were diagnosed with an anxiety disorder, and a subset were diagnosed with a comorbid depressive disorder (i.e., major depressive disorder - current or past and/or dysthymia). Comparisons were made between youth with a comorbid depressive diagnosis and those without on measures of baseline severity and treatment outcomes. We expected to replicate the finding that youth with a comorbid depressive disorder would have more severe baseline characteristics across several measures (i.e., depressive symptoms, primary anxiety disorder severity, impairment, global functioning). We hypothesized that youth with comorbid depressive disorders would still have more severe symptoms after treatment (i.e., more depressive symptoms, higher primary anxiety disorder severity, higher impairment, worse global functioning) and be less likely to achieve remission of their primary anxiety disorder diagnosis. However, we predicted that both groups would have a similar magnitude of change in symptoms and functioning from pre to post treatment. Finally, we expected that youth with a depressive diagnosis would experience similar levels of overall clinician-rated improvement.
Methods
Participants
Participants included 157 youth (ages 6–17) who received treatment at an anxiety specialty clinic in the Northeastern United States. For inclusion in this study, youth were required to meet diagnostic criteria for at least one primary anxiety disorder (i.e., generalized anxiety disorder, social anxiety disorder, separation anxiety disorder, or specific phobia) and to complete pretreatment and posttreatment diagnostic assessments. Completion of all 16 sessions of Coping Cat was required prior to completing a posttreatment assessment. All assessments included a semi-structured diagnostic interview, as well as the completion of self-report questionnaires. The average length of time between pretreatment and posttreatment assessments was 6.38 months (SD=1.92).
Participants were divided into two groups. The first group met criteria for both an anxiety disorder and a depressive disorder (A+D) per DSM-IV criteria (n=20, 12.7%). Depressive disorder diagnoses included major depressive disorder (MDD) current, MDD in remission, and/or dysthymia. The second group (A) met criteria for an anxiety disorder but did not meet criteria for a depressive disorder (n=137, 87.3%). Additional descriptive characteristics are in Table 1.
Table 1.
Descriptive Statistics for Youth Included in Final Sample (N=157)
| Anxiety Only n=137 |
Anxiety + Depression n=20 |
Overall | |||||
|---|---|---|---|---|---|---|---|
| Mean/N | SD/% | Mean/N | SD/% | T/χ 2 | Mean/N | SD/% | |
| Age (Years) | 10.63 | 2.62 | 13.62 | 2.81 | −4.72** | 11.01 | 2.82 |
| Race/Ethnicitya | 4.04 | ||||||
| White | 111 | 82.84% | 20 | 100% | 131 | 85.06% | |
| Black | 3 | 2.24% | 0 | 0% | 3 | 1.95% | |
| Asian | 5 | 3.73% | 0 | 0% | 5 | 3.25% | |
| Hispanic/Latinx | 8 | 5.97% | 0 | 0% | 8 | 5.19% | |
| Other | 7 | 5.22% | 0 | 0% | 7 | 4.55% | |
| Sex | 0.56 | ||||||
| Male | 70 | 51.09% | 12 | 60.00% | 82 | 52.23% | |
| Female | 67 | 48.91% | 8 | 40.00% | 75 | 47.77% | |
| Primary Anxiety Diagnosis | 16.25* | ||||||
| GAD | 67 | 48.90% | 6 | 30.00% | 73 | 46.50% | |
| Separation Anxiety | 20 | 14.60% | 0 | 0% | 20 | 12.74% | |
| Social Anxiety Disorder | 25 | 18.25% | 11 | 55.00% | 36 | 22.93% | |
| GAD + Social | 15 | 10.95% | 3 | 15.00% | 18 | 11.46% | |
| GAD + Separation | 7 | 5.11% | 0 | 0% | 7 | 4.46% | |
| Social + Separation | 1 | 0.73% | 0 | 0% | 1 | 0.64% | |
| All 3 | 2 | 1.46% | 0 | 0% | 2 | 1.27% | |
| Depressive Diagnosis | |||||||
| MDD (current) | 0 | 0% | 8 | 40% | 8 | 40% | |
| MDD (in remission) | 0 | 0% | 7 | 35% | 7 | 35% | |
| Dysthymia | 0 | 0% | 9 | 45% | 9 | 45% | |
| Co-Primary Diagnosis | 38 | 27% | 8 | 40% | 2.84 | 46 | 29.3% |
| Any Comorbid Diagnosis | 123 | 89.8% | 20 | 100% | 2.24 | 143 | 91.0% |
p <.10
p <.05
p <.01
Race was not reported by 3 children
Abbreviations: GAD=Generalized Anxiety Disorder; MDD=Major Depressive Disorder
Note: Depressive Diagnoses total more than 100% because some participants had dysthymia and MDD (current or in remission)
Measures
Anxiety Disorders Interview Schedule for Children and Parents (ADIS-IV-C and ADIS-IV-P; [22]).
The ADIS is a semi-structured, clinician-rated interview that yields DSM-IV diagnoses for anxiety, mood, and externalizing disorders in children ages 6–17. Psychometric properties are good to excellent (Silverman, Saavedra, & Pine, 2001). Separate parent- and child-report versions were administered and diagnoses were made by combining information from parent and child reports. Clinicians provided clinical severity ratings (CSRs) ranging from 1–8, for each disorder a parent or child endorsed. CSRs of 4 or greater indicate a clinical diagnosis. The primary diagnosis/es for each child or adolescent was determined by whichever disorder(s) had the highest CSR rating (ranging from 1–8). The ADIS was administered at pre- and post-treatment by clinicians trained to reliability.
Child Depression Inventory ([CDI; 23]).
The CDI is a 27-item youth self-report measure of depressive symptoms that yields T-scores. T-scores of 65 or greater indicate clinical severity of depressive symptoms. The CDI has demonstrated internal consistency and moderate test-retest reliability [24], and has been shown to have good predictive validity in predicting depressive disorders [25]. Participants completed the CDI at pretreatment and posttreatment.
Children’s Global Assessment Scale ([CGAS; 26]).
The CGAS is a clinician-rated measure of overall functioning and impairment. Scores range from 1 to 100, with higher numbers indicating higher functioning. Descriptions of the associated level of functioning are provided in 10-point intervals (e.g., a description is provided for the functioning of a child whose CGAS score is 80–90). It has been shown to have high test-retest reliability, and to effectively discriminate between youth in inpatient and outpatient settings.
Clinical Global Impression Scale –Severity (CGI-S; 25) and Clinical Global Impression Scale – Improvement ([CGI-I; 27]).
The CGI is a 7-point clinician-rated scale used to assess overall clinical severity and improvement based on symptoms observed and impairment reported. Higher numbers indicate more severe symptoms and worse functioning. The CGI-S was completed at pretreatment and posttreatment; the CGI-I was completed at posttreatment. CGI-S scores range from 1 (normal, not at all ill) to 7 (extremely ill). CGI-I scores range from 1 (very much improved) to 7 (very much worse). Youth with a CGI-I score of 1 (very much improved) or 2 (much improved) at post-treatment were considered treatment responders.
Procedures
All study procedures were approved by the Temple University Institutional Review Board. Participants were referred to the clinic via multiple sources (e.g., school counselors, pediatricians, word-of-mouth). Prior to completing an in-person assessment, parents completed a brief phone screen to assess eligibility for treatment. Those who were eligible based on the phone screen completed a pretreatment diagnostic assessment in person after completing informed consent/assent procedures. The assessment included child and parent diagnostic interviews, which were conducted separately, as well as the completion of self-report questionnaires. Posttreatment assessments followed the same procedures as pretreatment assessments.
All participants received CBT using the Coping Cat program [28]. Therapy was provided by advanced doctoral students supervised by a licensed clinical psychologist. Treatment included 16 weekly, 60-minute sessions prior to the posttreatment assessment. Coping Cat includes the following core components of CBT for youth anxiety: (1) recognizing somatic reactions and anxious cognitions; (2) learning coping strategies (e.g., relaxation, coping self-talk); (3) behavioral exposure; and (4) reinforcement for effort and brave behavior. The first eight sessions focus on learning each of these skills and the second half of treatment requires the child to engage in exposure tasks and practice the coping skills they developed earlier in treatment. Homework tasks to be completed between sessions are assigned to support the practice and generalization of skills. Although brief parent check-ins are included in every session, Coping Cat also includes two parent-only sessions during which parents ask questions, provide information about their child’s anxiety, and receive psychoeducation about how they can support their anxious child. Parents also received a parent companion that includes information about the Coping Cat program[29]. Additional details about Coping Cat are available elsewhere [30–32].
Data Analytic Strategy
The CDI was the only measure missing greater than 10% of data (11.5% missing at pretreatment; 13.4% missing at posttreatment). Multiple imputation was used to impute missing data for the CDI, as well as for other measures missing less than 10% of data (i.e., CGI-I, CGI-S, CGAS). Ten imputed datasets were generated, and analyses were conducted using the imputed values in SPSS. T-tests were used to compare groups at pre-treatment and at post-treatment on all variables of interest with Bonferroni corrections for multiple (10) comparisons. Chi square tests were used to examine group differences in anxiety diagnosis, as well as whether remission of primary anxiety diagnosis was more likely for those with depression. Treatment outcome analyses comparing the magnitude of change in symptoms and functioning between groups were conducted using repeated measures ANOVA with a Time (pretreatment and posttreatment) × Group (A+D versus A Only) design. Because CGI-I data only were collected at the post-treatment time point, multiple regression was used to examine predictors of CGI-I.
Results
Descriptive statistics for the full sample (N=157) are in Table 1. Chi-square tests and t-tests revealed differences between the A+D and A groups at pretreatment. The A+D youth were significantly older, t(155)=−4.72, p < .001, had higher depressive symptom (CDI) scores, t(241)=−3.01, p = .003, had lower scores on a measure of overall functioning (CGAS), t(8553)=3.90, p < .001, and had higher severity for their primary diagnosis (CSRs), t(155)=−3.04, p=.003. All comparisons remained significant after Bonferroni corrections. There were no significant group differences for global severity (CGI-S) at pretreatment. A Pearson chi-square test for independence revealed that the A+D group also was significantly more likely to have a diagnosis of social phobia or generalized anxiety disorder than the A group, X2 (6, N=157)=16.25, p = .01. Overall, the group with comorbid depression (A+D) appeared more severe at pretreatment. Full statistics for the t-tests and chi-square tests, as well as descriptive statistics for these measures at pre- and post-treatment are in Table 2.
Table 2.
T-tests Comparing Depressed and Non-depressed Groups
| Anxiety Only n=137 |
Anxiety + Depression n=20 |
||||
|---|---|---|---|---|---|
| Measure | Mean | SE | Mean | SE | T/χ 2 |
| CDI T-Scoresa | |||||
| Pre-treatment | 47.55 | 0.92 | 55.36 | 2.66 | −3.01** |
| Post-treatment | 42.70 | 0.68 | 45.59 | 2.69 | −1.44 |
| CGAS | |||||
| Pre-treatment | 53.82 | 0.57 | 47.57 | 1.50 | 3.90** |
| Post-treatment | 66.76 | 0.79 | 60.70 | 2.52 | 2.52** |
| CGI-I | |||||
| Pre-treatment | – | – | – | – | – |
| Post-treatment | 2.13 | 0.06 | 2.22 | 0.17 | −0.54 |
| CGI-S | |||||
| Pre-treatment | 4.56 | 0.06 | 4.82 | 0.19 | −1.52 |
| Post-treatment | 3.07 | 0.09 | 3.66 | 0.24 | −2.24* |
| CSR | |||||
| Pre-treatment | 5.58 | 0.07 | 6.15 | 0.17 | −3.04** |
| Post-treatment | 3.29 | 0.15 | 3.65 | 0.44 | −0.85 |
p <.10
p <.05
p <.005
Bonferroni adjusted alpha=.005
CDI scores are represented as scaled t-scores.
Abbreviations: CDI=Children’s Depression Inventory; CGAS=Children’s Global Assessment Scale; CGI-I=Clinical Global Impression Scale - Improvement; CGI-S=Clinical Global Impression Scale - Severity; CSR=Clinical Severity Rating
A Pearson chi-square test for independence tested whether remission of the primary anxiety diagnosis was more likely for children with comorbid depression. Results showed that primary anxiety disorder was significantly more likely to remit for children with anxiety only compared to anxious and depressed youth, X2 (1, N=157)=7.73, p = .005.
Treatment outcome analyses were conducted using four repeated measures ANOVA models to test assessment time point (pre/post) and group status (A+D/A) as predictors of primary anxiety diagnosis clinical severity (CSRs), overall clinical severity (CGI-S), overall functioning and impairment (CGAS), and depressive symptoms (CDI). Models with interaction terms for assessment time point (pre/post) and group (A+D/A) were run for all four models. CSRs for the primary anxiety disorder were significantly lower at posttreatment compared to pretreatment, F(1, 155)=142.40, p < .001. CSRs were marginally lower for the anxiety only (A) group, F(1, 155)=3.23, p = .07. There was not a significant interaction between time point and group (p >.05). In the second model, overall clinical severity (CGI-S) scores were significantly lower at posttreatment compared to pretreatment, F(1, 155)=94.92, p < .001, and significantly higher in the A+D group compared to the A group, F(1, 155)=6.05, p < .001. The interaction was not significant (p > .05). The third model showed that overall functioning (CGAS) scores were significantly higher at post- compared to pre-treatment, F(1, 155)=153.19, p < .001, and significantly lower in the A+D group compared to the A group, F(1, 155)=14.09, p < .001. The interaction between time point and group on the CGAS also was not significant (p > .05). In the final analysis examining depressive symptom severity score (CDI), the interaction between time point and group was significant, F(1, 155)=4.86, p < .001, as shown in Figure 1. This suggests that the A+D group improved more than the A group on the CDI from pre- to post-treatment. Of note, mean CDI scores were higher for the A+D group at both pre- and post-treatment.
Figure 1.
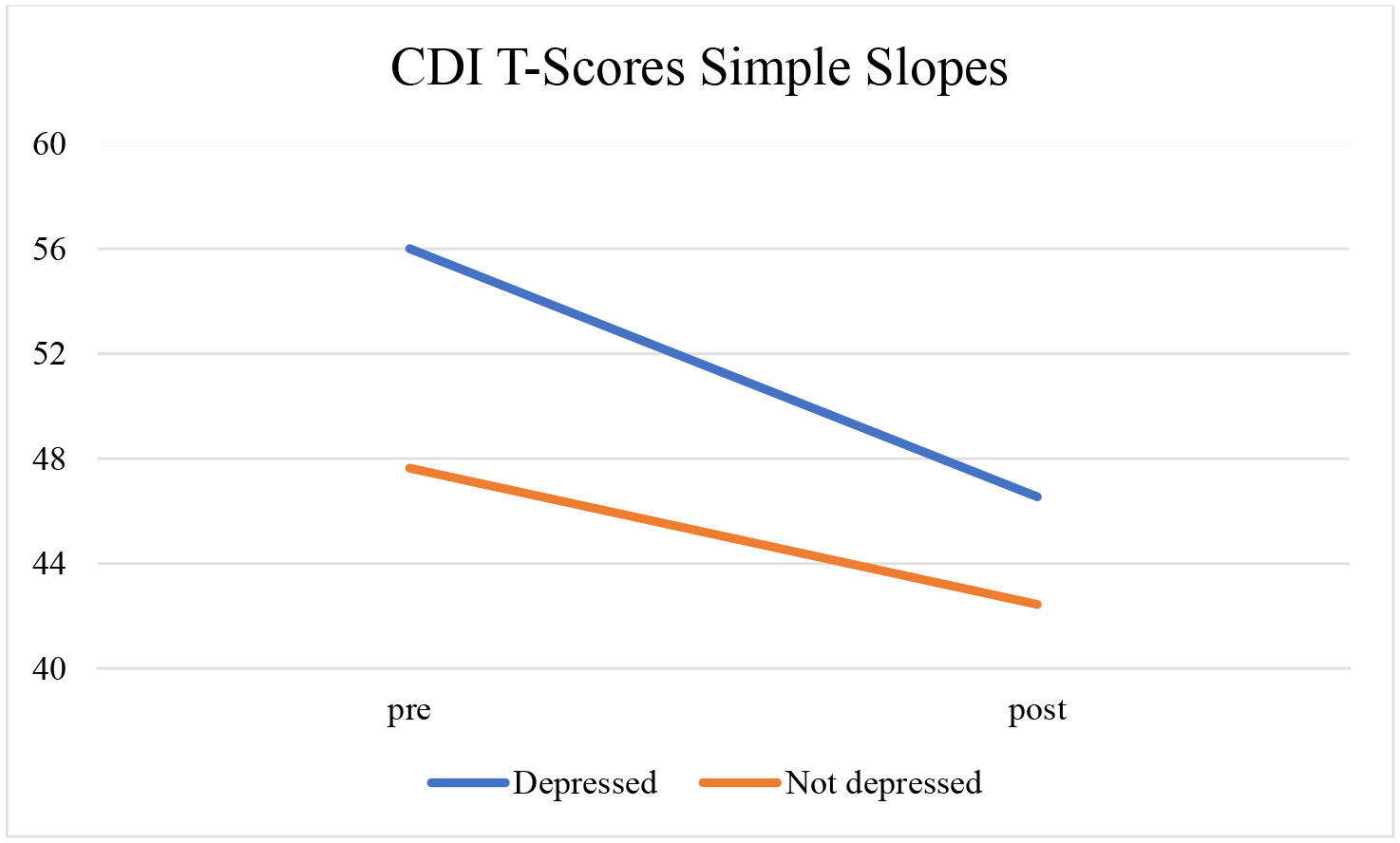
Interaction between time point and group on depressive symptom severity (CDI)
Finally, a multiple regression test examined group and sex as predictors of improvement of overall clinical severity (CGI-I score), and results showed no significant differences in CGI-I score between the A+D and A groups (p >.05). These findings suggest that both groups showed clinical improvement at similar rates, although the A+D group had lower functioning and more severe symptoms at both pre- and post-treatment than the A group.
Discussion
The findings regarding the relationship between comorbid depression and treatment outcomes for children with anxiety disorders have been mixed. Results of the present study indicate that depression comorbidity in children with anxiety disorders had significant associations at pretreatment with higher severity of primary anxiety disorder, depressive symptom severity, and poorer overall functioning. Both groups (A+D and A) improved significantly following CBT for anxiety on measures of severity of primary anxiety disorder, overall clinical severity, and overall functioning. Notably, the significant interaction between group and time point indicated that the amount of improvement in depressive symptom severity from pretreatment to posttreatment was greater among those in the anxious and depressed group than the anxiety only group. In contrast, the amount of improvement in overall symptoms, functioning, and anxiety severity was similar for both groups. The anxious and depressed group continued to have worse overall symptoms, functioning, and anxiety severity than the anxiety only group at post-treatment, suggesting that although anxiety-focused CBT improved symptoms, additional treatment may be warranted for youth with comorbid depression.
Results from the current study support previous findings that depression comorbidity is associated with poorer functioning and higher illness severity before treatment. Our results clarify the mixed findings regarding the effect of depression comorbidity on treatment outcomes for youth with anxiety disorders. Specifically, some studies have found comorbid depression to be associated with higher rates of less favorable treatment outcomes for anxiety [12, 33], whereas other studies have found that youth with comorbid depression improved just as much as those who had anxiety without comorbid depression [6, 18, 19]. Our results support that youth with comorbid depression improved as much as youth with anxiety only from pretreatment to posttreatment on numerous measures of severity and functioning. However, because youth with comorbid depression started with more severe anxiety, depression, and functioning deficits, they also were more severe at post-treatment; furthermore, it was less likely that their primary anxiety disorder had fully remitted at posttreatment, ostensibly due to the higher severity of their disorder at pretreatment. These findings are consistent with those of Rapee and colleagues [15], who concluded that children with comorbid depression experienced a similar amount of change in anxiety symptoms compared to those without comorbidity, but presented as more severe at pretreatment and remained more impaired at posttreatment. This has implications for the metric being used for “treatment success” or “efficacy” when considering the role of comorbidities in anxiety treatment outcome research. For instance, if treatment success is measured by comparing the symptoms and functioning of depression and anxiety only in the absolute, youth with comorbid depression may appear worse at posttreatment, whereas if treatment success is measured by comparing the rate or amount of improvement in groups, both groups appear to improve significantly and at similar rates on measures of overall symptom severity and functioning.
One exception to the pattern of reported findings in the literature was in the rate of improvement in depressive symptom severity. Our findings indicate that youth with depression demonstrated a greater magnitude of reduction in depressive symptom severity, with the mean CDI score showing what has been referred to as “clinical significance” [34] where the scores move from the “clinical” to the “non-clinical” range from pretreatment to posttreatment. In contrast, the reduction in depressive symptoms among the anxiety only group was of smaller magnitude and remained within the non-clinical range. Although this may reflect regression to the mean, the findings may support the conclusion that CBT for anxiety is efficacious in reducing depressive symptoms among those with comorbid depression [16]. Depressive symptom severity was not an explicit target of treatment, but it is possible that the reduction in depressive symptoms can be attributed to (a) the overlapping elements of CBT for anxiety and depression (e.g., cognitive restructuring, behavioral activation via exposure) and/or (b) that reducing anxiety permits the youth to engage in more prosocial and pleasant events. Findings are consistent with previous research that has shown that CBT for anxiety is successful in conferring protection from later suicidal ideation [35]. Even without explicitly targeting depressive symptomatology, CBT for anxiety may have secondary benefits for youth with comorbid depressive symptoms [36].
These findings have several clinical implications. First, CBT for anxiety in youth remains efficacious when depression comorbidity is present. That said, children with comorbid depression are likely to have a more severe baseline presentation, which also can be reflected in their posttreatment scores. This suggests that youth with comorbid anxiety and depression may require additional sessions or additional services to treat remaining symptoms following a 16-session treatment program. Future studies might explore how treatment programs and therapists can best address the co-occurring and remaining symptoms. Will it be wise to follow-up with depression-focused programs or with more sessions of the same program? Will modular approaches that contain a focus on both anxiety and depression have an advantage? In line with the preference for empirically supported treatments, research is needed to evaluate these options.
The use of a large, well-characterized sample assessed using multi-method and well-established measurements allowed for powerful within-subject comparisons. Generalizing from the findings, however, is constrained by a relatively homogenous racial composition (majority White) and socioeconomic status (majority middle class) of the sample. In addition, consistent with evidence that depressive diagnoses are more likely to develop in adolescence [37], this study included a small number of young children (under age 12) with depressive disorders (n=5). Thus, the degree to which these findings apply specifically to younger children remains in need of further examination. Another possible limitation concerns our choice to examine depression comorbidity dichotomously by diagnosis rather than continuously on a symptom severity spectrum, although an examination of our sample found that youth who were in the CDI clinical range overlapped considerably with those who were identified with a depression diagnosis. Future studies should explore similar questions regarding various comorbid conditions and differential outcomes for other CBT packages. Although previous research has demonstrated that Coping Cat outperforms placebo [38] and alternate approaches [39], the lack of a control group in the present study limits the conclusions that can be made. Finally, future work should examine changes in depression and anxiety symptoms across multiple time points beyond pretreatment and posttreatment in order to provide a more fine-grained analysis of the ways in which symptoms change over time (e.g., [40]).
Summary
This study explored treatment outcomes among a sample of anxious youth with and without comorbid depression who received CBT (i.e., Coping Cat) for anxiety. Findings indicate that treatment is efficacious among youth with and without comorbid depression, with both groups demonstrating comparable improvements after treatment. However, findings also support previous research demonstrating higher symptoms of pretreatment and posttreatment anxiety severity among the group with depressive disorder. Findings also suggest that, following CBT for anxiety, youth with comorbid depression may experience a greater decrease in depressive symptoms than non-depressed youth. Taken together, these findings suggest that anxious youth with comorbid depression may benefit from CBT for anxiety, while also underscoring that symptoms and functioning may be impacted even after a successful course of treatment.
Funding:
This study was funded by the National Institute of Mental Health (F31MH112211).
Footnotes
Publisher's Disclaimer: This Author Accepted Manuscript is a PDF file of an unedited peer-reviewed manuscript that has been accepted for publication but has not been copyedited or corrected. The official version of record that is published in the journal is kept up to date and so may therefore differ from this version.
Conflicts of Interest: Dr. Kendall receives royalties from the sales of materials related to the treatment of anxiety in youth.
Ethical Approval: All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
The article does not contain any studies with animals performed by any of the authors.
References
- 1.Costello E, et al. , Prevalence and development of psychiatric disorders in childhood and adolescence. Archives of General Psychiatry, 2003. 60(8): p. 837–844. [DOI] [PubMed] [Google Scholar]
- 2.Birmaher B, Arbelaez C, and Brent D, Course and outcome of child and adolescent major depressive disorder. Child and Adolescent Psychiatric Clinics of North America, 2002. 11(3): p. 619–637. [DOI] [PubMed] [Google Scholar]
- 3.Cummings C, Kazantzis N, and Kendall PC, Facilitating homework and generalization of skills to the real world, in Evidence-based CBT for anxiety and depression in children and adolescents: A competencies based approach., Sburlati E, et al. , Editors. 2014, Wiley-Blackwell: London. [Google Scholar]
- 4.Long EE, Young JF, and Hankin BL, Temporal dynamics and longitudinal co-occurrence of depression and different anxiety syndromes in youth: Evidence for reciprocal patterns in a 3-year prospective study. Journal of Affective Disorders, 2018. 234: p. 20–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.O’Neil KA, et al. , Comorbid Depressive Disorders in Anxiety-disordered Youth: Demographic, Clinical, and Family Characteristics. Child Psychiatry & Human Development, 2010. 41(3): p. 330–341. [DOI] [PubMed] [Google Scholar]
- 6.O’Neil KA and Kendall PC, Role of comorbid depression and co-occurring depressive symptoms in outcomes for anxiety-disordered youth treated with cognitive-behavioral therapy. Child & Family Behavior Therapy, 2012. 34(3): p. 197–209. [Google Scholar]
- 7.Guberman C and Manassis K, Symptomatology and family functioning in children and adolescents with comorbid anxiety and depression. Journal of the Canadian Academy of Child and Adolescent Psychiatry = Journal de l’Académie canadienne de psychiatrie de l’enfant et de l’adolescent, 2011. 20(3): p. 186–195. [PMC free article] [PubMed] [Google Scholar]
- 8.Queen AH and Ehrenreich-May J, Anxiety-Disordered Adolescents With and Without a Comorbid Depressive Disorder: Variations in Clinical Presentation and Emotion Regulation. Journal of Emotional and Behavioral Disorders, 2014. 22(3): p. 160–170. [Google Scholar]
- 9.Franco X, Saavedra LM, and Silverman WK, External validation of comorbid patterns of anxiety disorders in children and adolescents. Journal of Anxiety Disorders, 2007. 21(5): p. 717–729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Silverman WK and Hinshaw SP, The second special issue on evidence-based psychosocial treatments for children and adolescents: A 10-year update. Journal of Clinical Child and Adolescent Psychology, 2008. 37(1): p. 1–7. [DOI] [PubMed] [Google Scholar]
- 11.Walczak M, et al. , Does comorbidity predict poorer treatment outcome in pediatric anxiety disorders? An updated 10-year review. Clinical Psychology Review, 2018. 60: p. 45–61. [DOI] [PubMed] [Google Scholar]
- 12.Berman SL, et al. , Predictors of outcome in exposure-based cognitive and behavioral treatments for phobic and anxiety disorders in children. Behavior Therapy, 2000. 31(4): p. 713–731. [Google Scholar]
- 13.Hudson JL, et al. , Clinical predictors of response to cognitive-behavioral therapy in pediatric anxiety disorders: the Genes for Treatment (GxT) study. Journal of the American Academy of Child & Adolescent Psychiatry, 2015. 54(6): p. 454–463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hudson JL, et al. , Predicting outcomes following cognitive behaviour therapy in child anxiety disorders: the influence of genetic, demographic and clinical information. Journal of Child Psychology and Psychiatry, 2013. 54(10): p. 1086–1094. [DOI] [PubMed] [Google Scholar]
- 15.Rapee RM, et al. , Effect of comorbidity on treatment of anxious children and adolescents: results from a large, combined sample. Journal of the American Academy of Child & Adolescent Psychiatry, 2013. 52(1): p. 47–56. [DOI] [PubMed] [Google Scholar]
- 16.Mahdi M, et al. , Cognitive behavioral therapy for childhood anxiety disorders: What happens to comorbid mood and behavioral disorders? A systematic review. Journal of affective disorders, 2019. 251: p. 141–148. [DOI] [PubMed] [Google Scholar]
- 17.Southam-Gerow MA, Kendall PC, and Weersing VR, Examining outcome variability: Correlates of treatment response in a child and adolescent anxiety clinic. Journal of Clinical Child Psychology, 2001. 30(3): p. 422–436. [DOI] [PubMed] [Google Scholar]
- 18.Kley H, et al. , Predictors of outcome in a cognitive-behavioral group program for children and adolescents with social anxiety disorder. Journal of anxiety disorders, 2012. 26(1): p. 79–87. [DOI] [PubMed] [Google Scholar]
- 19.Alfano CA, et al. , Mediators and moderators of outcome in the behavioral treatment of childhood social phobia. Journal of the American Academy of Child & Adolescent Psychiatry, 2009. 48(9): p. 945–953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lenz AS, Meta-analysis of the coping cat program for decreasing severity of anxiety symptoms among children and adolescents. Journal of Child and Adolescent Counseling, 2015. 1(2): p. 51–65. [Google Scholar]
- 21.Villabø MA, et al. , Cognitive–behavioral therapy for youth anxiety: An effectiveness evaluation in community practice. Journal of consulting and clinical psychology, 2018. 86(9): p. 751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Silverman WK and Albano AM, Anxiety disorders interview schedule for DSM-IV child version: Clinical manual. 1996, Albany, NY: Graywind Publications. [Google Scholar]
- 23.Kovacs M, Children’s Depression Inventory Manual. 1992, North Tonawanda, NY: Multi-Health Systems, Inc. [Google Scholar]
- 24.Saylor CF, et al. , The children’s depression inventory: a systematic evaluation of psychometric properties. Journal of consulting and clinical psychology, 1984. 52(6): p. 955. [DOI] [PubMed] [Google Scholar]
- 25.Timbremont B, Braet C, and Dreessen L, Assessing depression in youth: relation between the Children’s Depression Inventory and a structured interview. Journal of Clinical Child and Adolescent Psychology, 2004. 33(1): p. 149–157. [DOI] [PubMed] [Google Scholar]
- 26.Shaffer D, et al. , A children’s global assessment scale (CGAS). Archives of General psychiatry, 1983. 40(11): p. 1228–1231. [DOI] [PubMed] [Google Scholar]
- 27.Guy W, Clinical global impressions, in ECDEU Asessment Manual for Psychopharmacology. 1976, National Institute for Mental Health: Rockville, MD. p. 218–222. [Google Scholar]
- 28.Kendall PC and Hedtke KA, Cognitive-behavioral therapy for anxious children: Therapist Manual. 3 ed. 2006, Ardmore, PA. [Google Scholar]
- 29.Kendall PC, Podell J, and Gosch E, The Coping Cat: Parent companion. 2010, Ardmore, PA: Workbook Publishing. [Google Scholar]
- 30.Beidas RS, et al. , Flexible applications of the coping cat program for anxious youth. Cognitive and behavioral practice, 2010. 17(2): p. 142–153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Norris LA and Kendall PC, A Close Look Into Coping Cat: Strategies Within an Empirically Supported Treatment for Anxiety in Youth. J Cogn Psychother, (1): p. 4–20. [DOI] [PubMed] [Google Scholar]
- 32.Podell JL, et al. , The Coping Cat Program for anxious youth: The FEAR plan comes to life. Cognitive and Behavioral Practice, 2010. 17(2): p. 132–141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Crawley SA, et al. , Treating socially phobic youth with CBT: Differential outcomes and treatment considerations. Behavioural and Cognitive Psychotherapy, 2008. 36(04): p. 379–389. [Google Scholar]
- 34.Kendall PC, et al. , Normative comparisons for the evaluation of clinical significance. Journal of consulting and clinical psychology, 1999. 67(3): p. 285. [DOI] [PubMed] [Google Scholar]
- 35.Wolk CB, Kendall PC, and Beidas RS, Cognitive-behavioral therapy for child anxiety confers long-term protection from suicidality. Journal of the American Academy of Child & Adolescent Psychiatry, 2015. 54(3): p. 175–179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Keeton CP, et al. , Mood and suicidality outcomes 3–11 years following pediatric anxiety disorder treatment. Depression and anxiety, 2019. 36(10): p. 930–940. [DOI] [PubMed] [Google Scholar]
- 37.Kessler RC, Merikangas KR, and Wang PS, Prevalence, comorbidity, and service utilization for mood disorders in the United States at the beginning of the twenty-first century. Annual review of clinical psychology, 2007. 3(1): p. 137–158. [DOI] [PubMed] [Google Scholar]
- 38.Walkup JT, et al. , Cognitive behavioral therapy, sertraline, or a combination in childhood anxiety. N Engl J Med, 2008. 359(26): p. 2753–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Silk JS, et al. , A randomized clinical trial comparing individual cognitive behavioral therapy and child-centered therapy for child anxiety disorders. Journal of Clinical Child & Adolescent Psychology, 2018. 47(4): p. 542–554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Settipani CA, et al. , Youth anxiety and parent factors over time: Directionality of change among youth treated for anxiety. Journal of Clinical Child & Adolescent Psychology, 2013. 42(1): p. 9–21. [DOI] [PMC free article] [PubMed] [Google Scholar]


