Abstract
Cardiac resynchronization therapy (CRT) is a well-established form of the treatment for heart failure (HF) in patients with left ventricle contraction dyssynchrony. Apart from typical in-office management, remote monitoring enables constant surveillance on both the patient's and the device's condition. This way, in case of any problems, clinical decisions could be made earlier leading to better outcome of CRT patients. COVID-19 pandemic with following lockdowns in many countries resulted in getting more attention on remote monitoring systems. The aim of this paper was to gather and summarize worldwide experiences from CRT remote monitoring during COVID-19 pandemic and point out future possibilities for HF patients treated with CRT. Already published experiences from remote monitoring of CRT devices during COVID-19 restrictions confirmed previous advantages of telemedical approach, however, more publications in this area would be helpful.
Introduction
Heart failure (HF) is a disease that affects even 26 million people worldwide.1 It is associated with high prevalence, morbidity and mortality, implying financial and social burdens in society. One of the possible therapies for these patients is cardiac resynchronization therapy (CRT). This form of electrotherapy is dedicated for HF patients with dyssynchrony of left ventricle (LV) contraction which is usually caused by left bundle branch block (LBBB). Uncoordinated contraction of LV complicates and worsens HF patients’ symptoms. CRT is based on implantation of two main ventricle electrodes – one for right ventricle (RV) and one for LV. If applicable, CRT can have also additional electrode in right atrium. What is more, if patient is simultaneously eligible for defibrillation, the RV electrode can have also this function (CRT-D).
CRT is recommended for the symptomatic HF with all the following criteria fulfilled: sinus rhythm, QRS >130 ms, LBBB and left ventricle ejection fraction (LVEF) <35% despite previous treatment.2 It should be also considered for symptomatic HF patients with sinus rhythm and QRS >130 ms without typical LBBB or among analogical patients with atrial fibrillation (instead of sinus rhythm), but who are expected to retrieve sinus rhythm.2 Apart from this, it is also recommended for the HF affected patients with reduced ejection fraction (HFrEF), who have general indications for ventricular pacing (eg, high degree atrioventricular block) instead of typical only RV pacing. These indications make CRT a popular form of therapy among patients with HF.
As mentioned above, the main purpose of CRT is to improve patients’ outcome by coordination of the LV contraction dyssynchrony. It is achieved by maximum ventricle pacing percentage, that is why HF patients treated with CRT should be monitored by a qualified electrotherapist.3 , 4 Remote monitoring of these patients enables constant surveillance on the device functions and the patient's condition. That is why, it is a helpful tool to improve the HF treatment outcomes.
This paper is a summary of current knowledge about known benefits of remote monitoring in CRT patients with the focus on the new experiences coming from COVID-19 pandemic and its future perspectives.
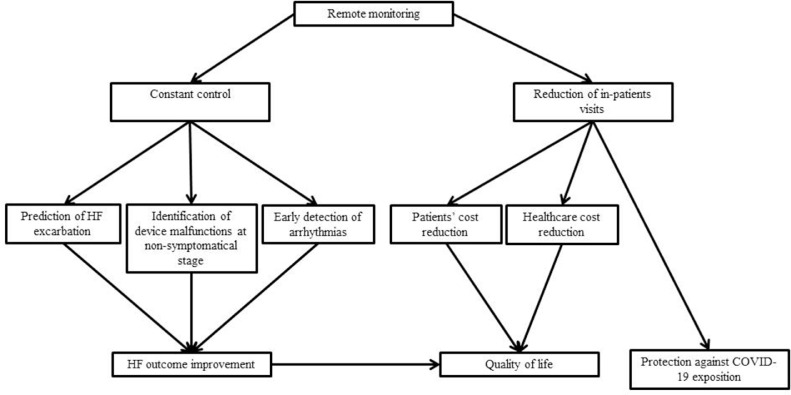
Advantages of Remote Monitoring in CRT Patients
The role of remote monitoring in CRT and other cardiac implantable electronic devices (CIED) – implantable cardioverter-defibrillators (ICD) and pacemakers (PM) has been pointed out in numerous papers.3, 4, 5, 6, 7, 8, 9, 10, 11 It has positive impact on patients’ quality of life, healthcare costs reduction and, what is the most important, clinical outcome of HF patients.5 , 6 , 8 , 10, 11, 12, 13, 14, 15, 16
Constant surveillance over monitoring functions of the device with the application of additional complex algorithms analyzing e.g. patients’ activity or hydration prevents appropriate shocks in CRT-D.5 , 9 What is more, with the application of specific algorithms, it could also be considered an instrument for the patients at risk of HF exacerbation identification.4 , 7 Early detection of other arrhythmias, for example, atrial fibrillation prevents inappropriate shocks in CRT-D.5 , 9 Apart from that, remote monitoring can identify device malfunctions (eg, lead damage) even at an early non-symptomatical stage, giving time to make a proper reaction.7 , 9 , 16
Remote monitoring is a part of the HF follow-up positive cycle. It leads to a reduction of in-person clinic visits and at the same time constant surveillance enables early detection of any abnormalities and this way their instant correction (if possible) often prevents patients’ hospitalization. Remote monitoring helps in healthcare cost reduction8 , 10 , 14 and also it may reduce patients’ costs (long-distance traveling for the in-person control, absence from work).12 , 17 This could also affect quality of life, as patients may feel safer having constant surveillance over their devices.12 However, the key advantage of this attitude is the improvement of general patients’ outcome. As mentioned above, it can reduce defibrillations shocks, detect arrhythmias at early stage, or diagnose device malfunctions. New algorithms can even predict HF worsening risk in advance.4 , 7
Numerous studies (eg, EFFECT, IN-TIME, CONNECT study) prove that remote monitoring is associated with reduced mortality and cardiovascular hospitalizations in patients treated with CRT.11 , 13 , 18 , 19 The EFFECT clinical trial was focused on ICD patients, however, there were also CRT-D patients included in both groups. It showed that remote monitoring was associated with reduced death and cardiovascular hospitalizations in patients with ICD, including CRT-D, comparing to the standard in-office follow-up.13 The IN-TIME clinical trial was based on similar groups that is, HF patients treated mainly with CRT-D (minority received ICD) and then divided into the groups of remote monitoring and standard non-remote monitoring care. The assessed outcome was a composite clinical score combining all-cause death, overnight hospital admission for heart failure, change in NYHA class, and change in patient global self-assessment, for the intention-to-treat population. The trial showed that telemonitoring can significantly improve clinical outcomes for patients with HF.18 In the CONNECT study, the group of patients was also ICD patients including CRT-D receivers. The study showed reduction in mean length of hospital stay due to cardiovascular reasons in the remote-controlled group.19 What is more, it also showed that remote monitoring can significantly shorten the time from the clinical event to the clinical decision in HF patients.19 The MORE-CARE trial showed no difference between remote and in-office monitored group in the terms of cardiovascular death.10 This way, even though remote monitoring did not change survival rate for HF patients, it also did not have any unfavorable influence on their safety.10 What is more, this trial showed the significant reduction of healthcare resources use among remote control group. It was achieved mainly by the reduction of in-office visits.10
More clinical research in this field could clarify it.15 , 16 , 20 However, remote monitoring generally became an advised approach in CRT treated patients’ follow-up.
COVID-19 Pandemic Impact on HF Patients
Coronavirus disease 2019 (COVID-19) pandemic became the biggest challenge for healthcare systems worldwide in 2020. Its impact on HF patients is particularly significant.
The patients suffering from HF are usually elderly people with multiple concomitant diseases. The HF patients are more susceptible to the COVID-19 and present more severe clinical course of it.21, 22, 23, 24 This way HF patients became a group that on one hand demands constant clinical surveillance, but on the other hand should currently avoid contact with healthcare providers, if it would not be necessary, as the way of protection against COVID-19 exposition and infection.23 , 25, 26, 27, 28 That is why medical practitioners and patients were greatly encouraged to implement more telemedical solutions in the course of the HF treatment.12 , 17 , 20 , 23 , 25 , 27 , 29, 30, 31 Already published experiences from remote monitoring of wireless CIEDs confirmed the advantages of telemedical approach equally important to the value of COVID-19 restrictions functioning.18 , 19 , 32 Even though remote monitoring for CIED patients, including CRT patients has already existed, it was not widely applied as a standard and a typical part of follow-up before 2020 in all countries. Cardiological patients receiving CIED treatment could definitely benefit from remote monitoring as the form of COVID-19 prevention.12 , 17 , 29 , 31 Possible advantages of this attitude refer to both general, mentioned above, HF treatment efficacy as well as HF patients’ safety in the context of COVID-19 pandemic. Novel method thus is improving chances of survival both directly and indirectly.
Constant surveillance on the device can improve HF patients’ clinical outcome, as mentioned in the previous paragraph. The benefits for HF patients with CRT can possibly sum up together, however, there has not been any study considering only CRT patients’ outcome in the context of COVID-19 pandemic. There is reported only single case report of COVID-19 patient with CRT device.33 It refers to HeartLogic algorithm application during COVID-19 pandemic in a CRT patient. It helped with early detection of fluid retention and enabled quick clinical decision and remote management. The conclusions from this case are very promising and prove the benefits of CRT remote monitoring, especially during COVID-19 pandemic.33 Another case reported by Vetta et al. was focused on side effects of COVID-19 treatment in patient with CRT that is, electrical storm in a patient treated with hydroxychloroquine, but not remote monitoring in HF itself.34
There is also a very interesting case report published by Mascioli et al, which suggest possibility of COVID-19 infection suspicion on the basis of CRT parameters change observed during remote monitoring.35 The idea was made retrospectively, when the parameters archived by remote monitoring of CRT-D device were analyzed after the patient was already diagnosed with COVID-19 and its typical symptoms.35 The patient presented for example, higher heart rate and lower general activity prior to the hospitalization due to COVID-19.35 This case report however does not mention any HF aspects of the patient performance.
HF patients benefit from active supervision.36 , 37 These findings are the basics of current complex HF care programs.38 , 39 They are focused on prehospital care that can introduce immediate diagnosis and proper treatment and this way preventing patients from further exacerbation of HF and hospitalization, which can be evitable.38 , 39 The principles of this kind of active care require cooperation between general practitioners and cardiologists. Currently it can be complicated or even impossible in case of CRT patients as remote monitoring of CRT is not yet a standard in several countries due to financial and organizational reasons. COVID-19 pandemic made national lawmakers adjust foregoing regulations. This way telemedicine became more nationally funded and medical providers were encouraged to use it widely. It also included CIED remote monitoring, which was often mainly used for research purposes until that time. These changes will hopefully become permanent, which will lead to development of remote monitoring and consultations for CRT and other CIED patients.
There have not been published any results of the studies focused only on CRT remote monitoring during COVID-19 pandemic yet. CRT devices offer more algorithms dedicated to HF patients, that can be analyzed remotely comparing to ICDs.40 As CRT patients belong to a special group of HF patients that can greatly benefit from the current progress in telemedicine this kind of observation would be very valuable.
However, there are already published experiences from remote monitoring in a mixed group of patients with ICD and CRT-D devices during COVID-19 pandemic.12 , 41
The Canadian study performed by De Larochellière et al compared the outcome of patients who were already regularly scheduled for remote monitoring sessions with the ones whose in-office visits were substituted for it due to pandemic.41 The 34% (113 of 329) of the investigated group were CRT-D patients. The study did not show any significant differences in clinical events or physician interventions among these groups. It showed that ICD and CRT-D remote monitoring was very useful during COVID-19 pandemic for clinical assessment of HF patients no matter if a patient has already received this kind of follow-up or if it was a sudden change.41 It also allowed reducing the number of in-office visits which was a part of COVID-19 exposure prevention.41
The Polish observation performed by Pastwa et al also confirmed benefits of remote monitoring during COVID-19 pandemic.12 The observed group of 100 patients included both ICD and CRT-D patients, however the authors did not reveal the exact number of individual different CIED receivers. In the paper there are mentioned examples of interventions taken thanks to remote monitoring (eg, atrioventricular node ablation in 3 CRT-D patients or newly diagnosed atrial flutter ablation), but the authors did not report statistical data on the events.12 The authors emphasized the patients’ positive feedback on this kind of follow-up comparing to standard in-office control in terms of COVID-19 safety and the general quality of life.12 It can be also counted in advantages of remote follow-ups in terms of patients’ quality of life which is consequence of therapy monitoring change (Figure ).
FIG.
Positive outcomes of CRT remote monitoring.
The experiences from Italy are also promising and show remote monitoring as a valuable tool for practitioners during this period.42 The remote control of 2955 mixed CIEDs (PM, ICD, CRT, ILR) triggered clinical decisions in 60% of monitored events (77 of 129 events). It mainly referred to a drug therapy remote modification. Thirty events (23%) were delivered by CRT devices, however, the authors did not describe how many CRT patients were in the general remote monitoring group.42 Nevertheless this observation showed the potential of remote monitoring in terms of drug therapy adjustments, without hospitalization and its value during COVID-19 pandemic.42
Similar results were observed by Piro et al in another Italian observation. However authors mention also the main challenges with the implementation of remote monitoring.43 They are namely proper patient education, which should be performed in person and/or via telephonic contact, ensuring adoption of remote monitoring system. Despite overall positive feedback of patients and general facility of monitoring in discussion some limitations were described, indicating that various lockdown approaches in countries may influence the results. Works presented to date also origins from Europe, but this report is first to the authors knowledge reviewing experience in remote monitoring of CRT patients regarding COVID-19. It is crucial to continue observations on the topic in the future, possibly providing more valuable information on the topic.
Development of the Transmission Techniques
Even though the main topic of 2020 was COVID-19 pandemic, there were also important steps in the development of CRT remote monitoring during this period. The new generation of CRT devices (Gallant, Abbott, IL) received the European Union Conformité Européenne mark in February 2020 and the approval of Food and Drug Administration in the United States in July 2020. Following first implantations were also performed this year in both Europe and United States. This was a breakthrough because of novel Bluetooth connectivity functions implemented in these devices. Until this time, remote monitoring, if available in particular devices, was possible only through a special transmitter. That is why, even though there are so many transplants of CRT remote control friendly devices, it is not always possible for doctors and patients to use this function. The new, mentioned above, technology enables remote monitoring of the CRT device via smartphone application and this way does not require additional transmitter. That is why remote monitoring can become more available for doctors and patients in the future.
Conclusions
COVID-19 pandemic was one of the biggest challenges of 2020. It forced changes in typical attitude to HF patients’ care including patients receiving CRT. However, this challenging time was also an opportunity for the rapid development of new telemedical solutions at organizational, legal, and technological levels. Experiences referring to remote control of mixed types of CIED, including CRT, during 2020 were very optimistic. They will hopefully become a part of standard coordinated HF care in the close future. CRT remote monitoring has been proven to be beneficial for HF patients even before COVID-19 pandemic. Nevertheless, more research and observations, particularly in CRT patients, need to be done to provide better evidence on usefulness of telemedical solutions.
Footnotes
JPK received trainings from Medtronic and Abbott.
References
- 1.Savarese G, Lund LH. Global public health burden of heart failure. Card Fail Rev. 2017;03:7. doi: 10.15420/cfr.2016:25:2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ponikowski P, Voors AA, Anker SD. ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure. Eur Heart J. 2016;37:2129–2200. doi: 10.1093/eurheartj/ehw128. [DOI] [PubMed] [Google Scholar]
- 3.Dauw J, Martens P, Mullens W. CRT optimization: what is new? What is necessary? Curr Treat Options Cardiovasc Med. 2019;21:45. doi: 10.1007/s11936-019-0751-2. [DOI] [PubMed] [Google Scholar]
- 4.Chatterjee NA, Heist EK. Cardiac resynchronization therapy—Emerging therapeutic approaches. Curr Treat Options Cardiovasc Med. 2018;20:20. doi: 10.1007/s11936-018-0614-2. [DOI] [PubMed] [Google Scholar]
- 5.Linde C, Braunschweig F. Cardiac resynchronization therapy follow-up. Heart Fail Clin. 2017;13:241–251. doi: 10.1016/j.hfc.2016.07.020. [DOI] [PubMed] [Google Scholar]
- 6.Health Quality Ontario Remote monitoring of implantable cardioverter-defibrillators, cardiac resynchronization therapy and permanent pacemakers: a health technology assessment. Ont Health Technol Assess Ser. 2018;18:1–199. http://www.ncbi.nlm.nih.gov/pubmed/30443279. [PMC free article] [PubMed] [Google Scholar]
- 7.Lucà F, Cipolletta L, Di Fusco SA. Remote monitoring: Doomed to let down or an attractive promise? IJC Hear Vasc. 2019;24 doi: 10.1016/j.ijcha.2019.100380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Buchta P, Tajstra M, Kurek A. The impact of remote monitoring of implanted cardioverter-defibrillator (ICD) and cardiac resynchronisation therapy device (CRT-D) patients on healthcare costs in the Silesian population: three-year follow-up. Kardiol Pol. 2017;75:573–580. doi: 10.5603/KP.a2017.0019. [DOI] [PubMed] [Google Scholar]
- 9.Smeets CJP, Verbrugge FH, Vranken J. Protocol-driven remote monitoring of cardiac resynchronization therapy as part of a heart failure disease management strategy. Acta Cardiol. 2018;73:230–239. doi: 10.1080/00015385.2017.1363022. [DOI] [PubMed] [Google Scholar]
- 10.Boriani G, Da Costa A, Quesada A. Effects of remote monitoring on clinical outcomes and use of healthcare resources in heart failure patients with biventricular defibrillators: results of the MORE-CARE multicentre randomized controlled trial. Eur J Heart Fail. 2017;19(3):416–425. doi: 10.1002/ejhf.626. [DOI] [PubMed] [Google Scholar]
- 11.Bogyi P, Vamos M, Bari Z. Association of remote monitoring with survival in heart failure patients undergoing cardiac resynchronization therapy: retrospective observational study. J Med Internet Res. 2019;21:e14142. doi: 10.2196/14142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Pastwa Ł, Galbierczyk A, Bednarski J. Telemonitoring urządzeń wszczepialnych jako narzędzie zapobiegania szerzeniu się pandemii Covid-19 (Telemonitoring of implantable devices as a tool to prevent the spread of COVID-19 pandemic) W Dobrym Rytmie. 2020;54:10–14. doi: 10.5604/01.3001.0014.1502. [DOI] [Google Scholar]
- 13.De Simone A, Leoni L, Luzi M. Remote monitoring improves outcome after ICD implantation: the clinical efficacy in the management of heart failure (EFFECT) study. Europace. 2015;17:1267–1275. doi: 10.1093/europace/euu318. [DOI] [PubMed] [Google Scholar]
- 14.Ladapo JA, Turakhia MP, Ryan MP, Mollenkopf SA, Reynolds MR. Health care utilization and expenditures associated with remote monitoring in patients with implantable cardiac devices. Am J Cardiol. 2016;117:1455–1462. doi: 10.1016/j.amjcard.2016.02.015. [DOI] [PubMed] [Google Scholar]
- 15.Braunschweig F, Anker SD, Proff J, Varma N. Remote monitoring of implantable cardioverter-defibrillators and resynchronization devices to improve patient outcomes: dead end or way ahead? EP Eur. 2019;21:846–855. doi: 10.1093/europace/euz011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mittal S. Increasing role of remote monitoring of cardiac resynchronization therapy devices in improving outcomes. Card Electrophysiol Clin. 2019;11:123–130. doi: 10.1016/j.ccep.2018.11.011. [DOI] [PubMed] [Google Scholar]
- 17.Cleland JGF, Clark RA, Pellicori P, Inglis SC. Caring for people with heart failure and many other medical problems through and beyond the COVID-19 pandemic: the advantages of universal access to home telemonitoring. Eur J Heart Fail. 2020;22:995–998. doi: 10.1002/ejhf.1864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hindricks G, Taborsky M, Glikson M. Implant-based multiparameter telemonitoring of patients with heart failure (IN-TIME): a randomised controlled trial. Lancet. 2014;384:583–590. doi: 10.1016/S0140-6736(14)61176-4. [DOI] [PubMed] [Google Scholar]
- 19.Crossley GH, Boyle A, Vitense H, Chang Y, Mead RH. The CONNECT (Clinical Evaluation of Remote Notification to Reduce Time to Clinical Decision) trial: the value of wireless remote monitoring with automatic clinician alerts. J Am Coll Cardiol. 2011 doi: 10.1016/j.jacc.2010.12.012. [DOI] [PubMed] [Google Scholar]
- 20.Galinier M, Roubille F, Berdague P. Telemonitoring versus standard care in heart failure: a randomised multicentre trial. Eur J Heart Fail. 2020 doi: 10.1002/ejhf.1906. [DOI] [PubMed] [Google Scholar]
- 21.Tomasoni D, Italia L, Adamo M. COVID-19 and heart failure: from infection to inflammation and angiotensin II stimulation. Searching for evidence from a new disease. Eur J Heart Fail. 2020;22:957–966. doi: 10.1002/ejhf.1871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Faconti L, Chowienczyk PJ, Shah AM. Cardiovascular disease, heart failure and COVID-19. JRAAS - J Renin-Angiotensin-Aldosterone Syst. 2020 doi: 10.1177/1470320320926903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Harikrishnan S, Mohanan PP, Chopra VK. Cardiological society of India position statement on COVID-19 and heart failure. Indian Heart J. 2020 doi: 10.1016/j.ihj.2020.04.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Alvarez-Garcia J, Lee S, Gupta A. Prognostic Impact of Prior Heart Failure in Patients Hospitalized With COVID-19. J Am Coll Cardiol. 2020 doi: 10.1016/j.jacc.2020.09.549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.DeFilippis EM, Reza N, Donald E, Givertz MM, Lindenfeld JA, Jessup M. Considerations for heart failure care during the COVID-19 pandemic. JACC Hear Fail. 2020 doi: 10.1016/j.jchf.2020.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Jiménez-Blanco Bravo M, Cordero Pereda D, Sánchez Vega D. Heart failure in the time of COVID-19. Cardiol. 2020 doi: 10.1159/000509181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Gorodeski EZ, Goyal P, Cox ZL. Virtual visits for care of patients with heart failure in the era of COVID-19: a statement from the Heart Failure Society of America. J Card Fail. 2020 doi: 10.1016/j.cardfail.2020.04.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Reza N, DeFilippis EM, Jessup M. Secondary impact of the COVID-19 pandemic on patients with heart failure. Circ Hear Fail. 2020;13 doi: 10.1161/CIRCHEARTFAILURE.120.007219. [DOI] [PubMed] [Google Scholar]
- 29.Zhang Y, Coats AJS, Zheng Z. Management of heart failure patients with COVID-19: a joint position paper of the Chinese Heart Failure Association & National Heart Failure Committee and the Heart Failure Association of the European Society of Cardiology. Eur J Heart Fail. 2020;22:941–956. doi: 10.1002/ejhf.1915. [DOI] [PubMed] [Google Scholar]
- 30.Albert NM, Prasun MA. Telemedicine in heart failure during COVID-19: like it, love it or lose it?Hear Lung. 2020;49:A11-A12. doi:10.1016/j.hrtlng.2020.10.014 [DOI] [PMC free article] [PubMed]
- 31.Varma N, Marrouche NF, Aguinaga L. HRS/EHRA/APHRS/LAHRS/ACC/AHA worldwide practice update for telehealth and arrhythmia monitoring during and after a pandemic. Hear Rhythm. 2020 doi: 10.1016/j.hrthm.2020.06.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Varma N, Epstein AE, Irimpen A, Schweikert R, Love C. Efficacy and safety of automatic remote monitoring for implantable cardioverter-defibrillator follow-up: the lumos-t safely reduces routine office device follow-up (TRUST) trial. Circulation. 2010 doi: 10.1161/CIRCULATIONAHA.110.937409. [DOI] [PubMed] [Google Scholar]
- 33.Egolum UO, Parikh K, Lekavich C, Wosik J, Frazier-Mills C, Fudim M. Applications of the Multisensor HeartLogic Heart Failure Monitoring Algorithm During the COVID-19 Global Pandemic. JACC Case Reports. 2020;2:2265–2269. doi: 10.1016/j.jaccas.2020.09.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Vetta F, Marinaccio L, Vetta G, Marchese D. Electrical storm in a patient with COVID-19 treated with hydroxychloroquine: a case report. SAGE Open Med Case Rep. 2020 doi: 10.1177/2050313x20974217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Mascioli G, Lucca E, Annunziata L, Giacopelli D. Remote monitoring temporal trends during COVID-19 pneumonia in patients with implanted defibrillators. J Cardiol Cases. 2021 doi: 10.1016/j.jccase.2021.01.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Lainscak M, Blue L, Clark AL. Self-care management of heart failure: Practical recommendations from the patient care committee of the heart failure association of the European society of cardiology. Eur J Heart Fail. 2011 doi: 10.1093/eurjhf/hfq219. [DOI] [PubMed] [Google Scholar]
- 37.McDonagh TA, Blue L, Clark AL. European Society of Cardiology Heart Failure Association Standards for delivering heart failure care. Eur J Heart Fail. 2011;13:235–241. doi: 10.1093/eurjhf/hfq221. [DOI] [PubMed] [Google Scholar]
- 38.Nessler J, Kozierkiewicz A, Gackowski A. Comprehensive Heart Failure Care pilot study: starting point and expected developments. Kardiol Pol. 2019;77:994–999. doi: 10.33963/KP.15035. [DOI] [PubMed] [Google Scholar]
- 39.Nessler J, Kozierkiewicz A, Gackowski A. Coordinated heart failure care in Poland: Towards optimal organisation of the health care system. Kardiol Pol. 2018;76:479–487. doi: 10.5603/KP.2018.0050. [DOI] [PubMed] [Google Scholar]
- 40.Vamos M, Nyolczas N, Bari Z. Refined heart failure detection algorithm for improved clinical reliability of OptiVol alerts in CRT-D recipients. Cardiol J. 2018;25:236–244. doi: 10.5603/CJ.a2017.0077. [DOI] [PubMed] [Google Scholar]
- 41.De Larochellière H, Champagne J, Sarrazin J. Findings of remote monitoring of implantable cardioverter defibrillators during the COVID-19 pandemic. Pacing Clin Electrophysiol. 2020;43:1366–1372. doi: 10.1111/pace.14086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Iacopino S, Placentino F, Colella J. Remote monitoring of cardiac implantable devices during COVID-19 outbreak: “keep people safe” and “focus only on health care needs”. Acta Cardiol. 2020:1–4. doi: 10.1080/00015385.2020.1847459. [DOI] [PubMed] [Google Scholar]
- 43.Piro A, Magnocavallo M, Della Rocca DG. Management of cardiac implantable electronic device follow-up in COVID-19 pandemic: lessons learned during Italian lockdown. J Cardiovasc Electrophysiol. 2020;31:2814–2823. doi: 10.1111/jce.14755. [DOI] [PMC free article] [PubMed] [Google Scholar]