Abstract
The pandemic of coronavirus disease 2019 (COVID-19) and lockdown measures, that were implemented in many countries in order to control the virus transmission, had negatively influenced the lifestyle of millions of people worldwide. In this study we aimed to investigate the impact of the first COVID-19 lockdown period (March–May 2020) on snacking behavior, fast-food and alcohol consumption. A systematic search in PubMed®, Scopus® and Web of Science® databases was conducted and 32 studies were included. Changes in snacking, in fast-food and ordered food consumption and in alcohol intake were examined. Snacking was found to be increased for a significant portion of the population examined (18.9–45.1%), whereas fast food (15.0–41.3%) and ordered food (33.9%) showed a tendency towards decrease. As per alcohol consumption, an upward trend was observed in a significant part (10.4–51.0%) of the participants examined. The increased snacking and alcohol consumption observed for almost a third of the examined population could be alarming because long-term health problems could arise in cases of repeated lockdowns in the future. The observed downward trend in fast-food consumption and in frequency of ordered food could be an encouraging sign of turning to home-prepared foods, but further research is needed in this field.
Keywords: Alcohol, Drinking, COVID-19, Fast food, Ordered food, Sars-Cov-2
Abbreviations: COVID-19, Coronavirus Disease 2019; CVD, Cardiovascular Diseases; Τ2DM, Diabetes Mellitus Type 2; MENA, Middle East and North Africa; NOS, Newcastle Ottawa Scale; PRISMA, Preferred Reporting Items for Systematic Reviews and Meta-Analyses; QoL, Quality Of Life; UK, United Kingdom; USA, United States of America; WHO, World Health Organization
1. Introduction
The coronavirus disease 2019 (COVID-19), a severe acute respiratory syndrome, was first reported in Wuhan, China and on March, 11th 2020 the World Health Organization (WHO) declared a pandemic due to its rapid spread throughout the world [1]. In order to combat the pandemic, many governments enforced preventive measures of self-isolation and nationwide lockdowns of several degrees, so as by April 2020 more than a third of the global population was under lockdown [2]. People were forced to stay at home and practice online working and/or online learning and were allowed to leave their homes only for prespecified occasions, such as medical reasons, essential work, physical activity, purchasing food and in emergencies [2]. Such sudden changes in people's life can have a negative impact both on their mental health and their lifestyle behaviors, such as alcohol consumption [3] and dietary habits [4]. Moreover, shifts in the daily routine and abstention from work, which can be associated with stress and boredom could lead to a greater energy intake and/or overeating [5]. During the first COVID-19 lockdown a high prevalence of sleep disorders was reported [6,7], which could also be linked to imbalanced dietary patterns [8]. Overeating is directly related to an increased risk of developing obesity [9] and subsequently the risk for cardiovascular diseases (CVD) [10] and type-2 diabetes mellitus (T2DM) [11] is increased. In addition, identification of the alcohol consumption pattern during the lockdown period is important, as this is related to an increased prevalence of negative health outcomes and also negatively influences the quality of life (QoL) for both the consumer and his/her family members [12].
Undoubtedly, there is inadequate information about related changes in eating behaviors as well as alcohol consumption during this global health crisis, although several studies have been conducted at national level. This systematic review aims to investigate changes in specific dietary habits (snacking, fast-foods, ordered food) and alcohol consumption during the COVID-19 lockdown period compared to pre lockdown time.
2. Material and methods
An electronic search was conducted in PubMed®, Scopus® and Web of science® databases (up to 28 November 2020) using the index terms “junk food”, “fast food”, “take away”, “alcohol”, “ethanol”, “covid-19”, “Sars-Cov-2” and the final search string as well as more info about our search strategy can be found in Supplementary File 1.
Total records identified through database searching were 1485 and were added in a reference database. (EndNote X7 for Windows, Thomson Reuters). After removal of duplicates studies were screened independently by two reviewers DB and MC. Any disagreements regarding selection of the included studies and data extraction were solved by consensus. Inclusion criteria were adolescent (≥16 years old) and adult populations who were under lockdown restrictions due to the COVID-19. Studies in which included children (<16 years old) or symptomatic COVID-19 patients were excluded. Studies not in English language were also excluded.
This systematic review was conducted in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement [13] (Supplementary Table 1). The quality of the eligible studies was assessed using the modified Newcastle Ottawa Scale (NOS) for cross-sectional studies (Supplementary Table 2) [14]. Due to the fact that this is a rapid systematic review as COVID-19 is an emerging, rapidly evolving situation, a protocol for this systematic review was not written.
Data extraction of the included studies was independently conducted by two reviewers (DB and MC) using a previous standardized excel form. All disagreement were solved by consensus. Data extracted from each study were country origin, sex and number of participants, period and type of the survey. Moreover, we examined dietary changes and we extracted information regarding changes in snacking habit, fast-food and ordered food as well as alcohol consumption. Variables referred to dietary and alcohol changes were presented as percentages. Statistical significance of each study's results was stated by p-values where this data was available.
3. Results
3.1. Search results
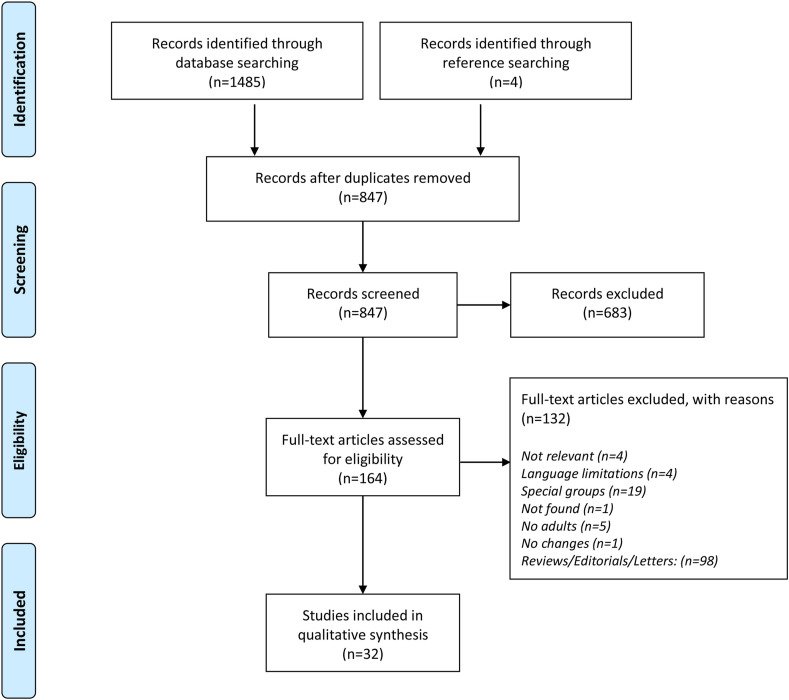
The process for the studies selection is presented as a flow diagram in Fig. 1 . A total of 1489 studies were identified through databases and reference searching and after removal of 642 duplicates, 847 studies were screened. Hence, 32 studies [[15], [16], [17], [18], [19], [20], [21], [22], [23], [24], [25], [26], [27], [28], [29], [30], [31], [32], [33], [34], [35], [36], [37], [38], [39], [40], [41], [42], [43], [44], [45], [46]] (all cross-sectional) were included in this systematic review. Characteristics of the 32 cross-sectional included studies can be found in Table 1 .
Fig. 1.
Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) flow diagram of eligibility process of included studies.
Table 1.
Characteristics of Included studies (All online surveys).
| Study ID (Country) | Subjects | Period survey conducted (already time spent in lockdown) |
|---|---|---|
| Allhuseini et al., 2020 [15] (Saudi Arabia) |
2706 (Μ:1240, F:1466) | 5–15 May (NA) |
| Ammar et al., 2020 [16] (International) | 1047 (Μ:484, F: 563) | 1–11 April (NA) |
| Avery et al., 2020 [17] (USA) | 3871 (Μ:1125, F:2746) | 26 March-5 April (NA) |
| Błaszczyk-Bębenek et al., 2020 [18] (Poland) | 312 (Μ:112, F:200) | 29 April-19 May (NA) |
| Cheikh Ismail et al., 2020 [19] (UAE) |
1012 (Μ:244, F:768) | April–May (NA) |
| Cheikh Ismail et al., 2020 [20] (International) | 2970 (Μ:844, F:2126) | 15–29 April (NA) |
| Chodkiewicz et al., 2020 [21] (Poland) | 443 (Μ:95, F:348) | 10–22 April (1 month) |
| Constant et al., 2020 [22] (France) |
4005 (Μ:1954, F:2051) | 8 and 20 April (3–4 weeks) |
| Gerritsen et al., 2020 [23] (New Zealand) |
3028 (Μ:314, F:2682, O:32) | 24 April-13 May (31–51 days) |
| Górnicka et al., 2020 [24] (Poland) |
2381 (F:2138, Μ:243) | 30 April-23 May (NA) |
| Husain et al., 2020 [25] (Kuwait) |
415 (Μ:130, F:285) | 30 March-15 April (NA) |
| Ingram et al., 2020 [26] (UK) |
399 (M:168, F:226, O:5) | NA (NA) |
| Knell et al., 2020 [27] (USA) |
1809 (Μ:589, F:1220) | 15 April-5 May (NA) |
| Kriaucioniene et al., 2020 [28] (Lithuania) | 2447 (Μ:198, F:2149) | 14–28 April (1 month) |
| Malta et al., 2020 [29] (Brazil) |
45161 (Μ:20956, F:24205) | NA (NA) |
| Mehta, 2020 [30] (India) |
50 (Μ:25, F:25) | 23–29 March (NA) |
| Panagiotidis et al., 2020 [31] (Greece) | 705 (Μ:177, F:528) | 25–28 April (36 days) |
| Pellegrini et al., 2020 [32] (Italy)a |
150b (Μ:34, F:116) | 14–21 April (NA) |
| Robinson et al., 2020 [33] (UK) |
723 (Μ:235, F:488) | 19–22 April (28–32 days) |
| Rodríguez-Pérez et al., 2020 [34] (Spain) | 7509 (Μ:2204, F:5305) | 20 March-10 April (1–3 Weeks) |
| Rolland et al., 2020 [35] (France) |
11391 (M:2557, F:8782, O:52) | 18–25 March (NA) |
| Rossinot et al., 2020 [36] (France) |
1454 (Μ:530, F:924) | 23 April-27 May (NA) |
| Sánchez-Sánchez et al., 2020 [37] (Spain) | 1065 (Μ:290, F:775) | May (NA) |
| Scarmozzino et al., 2020 [38] (Italy) |
1929 (Μ:637, F:1292) | 15 April (NA) |
| Sharma et al., 2020 [39] (USA) |
542 (Μ:106, F:436) | April (NA) |
| Sidor et al., 2020 [40] (Poland) |
1097 (Μ:54, F:1043) | 17 April-1 May (NA) |
| Stanton et al., 2020 [41] (Australia) | 1483 (Μ:484, F:999) | 9–19 April (NA) |
| Sun et al., 2020 [42] (China) |
6416 (Μ:3015, F:3401) | 24–31 March (NA) |
| Tran et al., 2020 [43] (Australia) |
13829 (NA) | 3 April-2 May (4–32 days) |
| Vanderbruggen et al., 2020 [44] (Belgium) | 3624 (M:1083, F:2541) | 9–29 April (NA) |
| Yan et al., 2020 [45] (China) |
8431 (M:3486, F:4945) | 15 April-11 May (NA) |
| Zajacova et al., 2020 [46] (Canada) |
4319 (M:2116, F:2203) | 29 March-3 April (NA) |
F: Female, M: Male, O: Other.
NA: Not available.
Online and via telephone survey.
Obese subjects.
3.2. Snacking habits
Several studies had examined changes in snacking behavior during the period of lockdown [22,24,[28], [29], [30],32,34,37,38] and the results are shown in Table 2 . In these studies 34.0–62.2% stated no changes in either frequency or portion of snacking consumption throughout the day [22,24,28,29,34,37,38]. Regarding the subjects who reported changes in snacking a tendency towards increase can be observed [22,24,29,34]. The highest increase (~45%) for snacking consumption compared to the pre-lockdown period was reported among the Lithuanian population [28].
Table 2.
Changes in snacking during lockdown.
| Study ID (Country) | Increased | Decreased | No changes | P value |
|---|---|---|---|---|
| Constant et al., 2020 [22] (France) |
24.0% | 18.2% | 57.9% | NA |
| Gornicka et al., 2020 [24] (Poland)a |
32.0% | 18.8% | 62.2% | <0.001 |
| Kriaucioniene et al., 2020 [28] (Lithuania) | 45.1% | 9.8% | 45.1% | NA |
| Malta et al., 2020 [29] (Brazil) |
a | NA | NA | NA |
| Mehta, 2020 [30] (India) |
38.0% | 28.0% | 34.0% | NA |
| Pellegrini et al., 2020 [32] (Italy) |
32.7% | 11.3% | 56.0% | NA |
| Rodríguez-Pérez et al., 2020 [34] (Spain) | 37.6% | 15.7% | 46.7% | <0.001 |
| Sánchez-Sánchez et al., 2020 [37] (Spain) | b | NA | NA | <0.001 |
| Scarmozzino et al., 2020 [38] (Italy)a |
18.9% | 23.5% | 57.6% | NA |
NA not available.
a before lockdown: snacks more than 2 days: 9.5%/during lockdown snacks more than 2 days: 13.2%.
b before lockdown: 2 or less portions per week: 72.2%, 3 or more portions per week: 27.8%/After lockdown: 2 or less portions per week: 55.6%, 3 or more portions per week: 44.4%.
The total from those studies is not 100%.
3.3. Fast-food and ordered food consumption
Changes in fast-food consumption were reported in eight studies [19,20,24,25,28,34,35,46] and changes in ordered food were examined in three studies [15,18,23], whereas relevant results are summarized in Table 3, Table 4 respectively. In four studies, more than 50% of the participants’ fast-food consumption remained unchanged during lockdown [24,28,34,46]. In studies where consumption of fast food had changed during the lockdown restrictions, a downward trend was identified [19,20,24,25,28,34,35,46]. Less than 10% of the participants examined reported an increase in junk food consumption [24,28,34], in contrast to one study by Zajacova et al., in which an increased consumption was stated by 25.0% of the survey participants [46]. Regarding the frequency of food ordering and having food delivered at home, results varied as can be seen in Table 4, with two studies showing a decline [15,18], and one showing an increase [23] (see Table 5 ).
Table 3.
Changes in consumption of fast-food during lockdown.
| Study ID (Country) | Increased | Decreased | No changes | P value |
|---|---|---|---|---|
| Cheikh Ismail et al., 2020 [19] (UAE) | NA | b | NA | <0.001 |
| Cheikh Ismail et al., 2020 [20] (International) | NA | a | NA | <0.001 |
| Górnicka et al., 2020 [24] (Poland) |
8.1% | 36.6% | 55.3% | <0.001 |
| Husain et al., 2020 [25] (Kuweit) |
NA | c | NA | NA |
| Kriaucioniene et al., 2020 [28] (Lithuania) | 6.7% | 41.3% | 71.1% | NA |
| Rodríguez-Pérez et al., 2020 [34] (Spain) | 5.1% | 34.9% | 60.0% | <0.001 |
| Rolland et al., 2020 [35] (France) |
NA | d | NA | NA |
| Zajacova et al., 2020 [46] (Canada) |
25.0% | 15.0% | 60.0% | NA |
NA not available.
a Before lockdown: 28.8%/After lockdown 5.3%.
b Before lockdown: 26.7%/After lockdown 7.9%.
c Before lockdown: Other: 2.7%, 1–2 times per week: 49.4%, 3–4 times per week: 17.3%, 5 or more times per week: 5.3%/After lockdown: Other: 0.2%, 1–2 times per week: 13.7%, 3–4 times per week: 2.2%, 5 or more times per week: 1.9%.
d Before lockdown: >1 time per day: 1.5%, once per day: 6.3%, few times per week: 22.6%, once per week: 25.3%, once per month: 19.8%, occasionally: 13.7%, never: 10.8%/After lockdown: >1 time per day: 0.3%, once per day: 0.7%, few times per week: 6.7%, once per week: 12.8%, once per month: 27.8%, occasionally: 28.3%, never: 23,4%.
Table 4.
Changes in frequency of ordered food during lockdown.
| Study ID (Country) | Increased | Decreased | No changes | P value |
|---|---|---|---|---|
| Allhuseini et al., 2020 [15] (Saudi Arabia) |
NA | a | NA | <0.001 |
| Błaszczyk-Bębenek et al., 2020 [18] (Poland) | NA | b | NA | <0.0001 |
| Gerritsen et al., 2020 [23] (New Zealand) |
52.2% | 33.9% | 13.9%a | NA |
NA not available.
a Before lockdown: Never: 15%, 1–2 times per week: 50.6%, 3–6 times per week: 25.8%, daily: 8.6%/After lockdown: never: 74.8%, 1–2 times per week: 17.5%, 3–6 times per week: 4.4%, daily: 3.4%.
b Before lockdown: Never: 15.7%, 1–3 times per month: 45.5%, 1 time per week: 17.3%, few times per week: 17.3%, 1 time per day: 3.5%, few times a day: 0.6%/After lockdown: Never: 51.6%, 1–3 times per month: 34.6%, 1 time per week: 9.0%, few times per week: 3.50%.
c time per day: 1.3%, few times a day: 0%.
Not stated in the study. Calculated according to existing results.
Table 5.
Changes in alcohol consumption during lockdown.
| Study ID (Country) | Increased | Decreased | No changes | P value |
|---|---|---|---|---|
| Ammar et al., 2020 [16] (International) | NA | a | NA | <0.001 |
| Avery et al., 2020 [17] (USA) |
14.3% | 10.9% | 74.8% | NA |
| Chodkiewicz et al., 2020 [21] (Poland)d | 13.8% | 17.4% | 68.4% | NA |
| Gerritsen et al., 2020 [23] (New Zealand) |
32.8% | 9.1% | 58.1%e | <0.001 |
| Gornicka et al., 2020 [24] (Poland) |
18.1% | 10.6% | 71.3% | NA |
| Ingram et al., 2020 [26] (UK) |
35.4% | 25.3% | 39.3% | 0.033 |
| Knell et al., 2020 [27] (USA) |
38.5% | 11.9% | 49.6% | 0.01 |
| Kriaucioniene et al., 2020 [28] (Lithuania) | 14.2% | 15.9% | 69.9% | NA |
| Malta et al., 2020 [29] (Brazil) |
17.6%a | NA | NA | NA |
| Panagiotidis et al., 2020 [31] (Greece) | 21.5% | 45.2% | 33.3%b | NA |
| Robinson et al., 2020 [33] (UK) |
28.0% | 30.0% | 41.0% | NA |
| Rodríguez-Pérez et al., 2020 [34] (Spain) | 10.4% | 57.3% | 32.3% | <0.001 |
| Rolland et al., 2020 [35](France)d | 17.76% | 12.0% | 68.05% | NA |
| Rossinot et al., 2020 [36] (France)d |
12.2% | 12.2% | 61.8% | NA |
| Scarmozzino et al., 2020 [38] (Italy)d | 36.8% | 7.9% | 53.1% | NA |
| Sharma et al., 2020 [39] (USA) |
23.6% | 7.9% | 68.5% | NA |
| Sidor et al., 2020 [40] (Poland) |
14.6% | 0.01%e | 85.3% | NA |
| Stanton et al., 2020 [41] (Australia) | 26.6% | 18.1% | 55.3% | NA |
| Sun et al., 2020 [42] (China) |
51.0%c | NA | NA | NA |
| Tran et al., 2020 [43] (Australia) |
20.9% | 10.5% | 68.6% | NA |
| Vanderbruggen et al., 2020 [44] (Belgium) | 30.3% | 13.7% | 56.0% | <0.001 |
| Yan et al., 2020 [45] (China) |
25.5% | 39.3% | 35.2% | <0.001 |
| Zajacova et al., 2020 [46] (Canada) |
14.0% | 10.0% | 76.0% | NA |
d the total from those studies is not 100%.
a higher among people aged 30-39.
b Before lockdown: Never: 87.68%, sometimes: 10.12%, most of time: 1.81%, always: 0.38% / After lockdown: Never: 93.22%, sometimes: 5.35%, most of time: 1.24%, always: 0.19%.
b Quit: 14.5 %.
c Relapses to abuse from alcohol: 19% / Increase in regular drinkers: 32%.
∗ Not stated. Calculated by the existing results.
NA: not available.
3.4. Alcohol consumption
Changes in alcohol consumption during the lockdown period were reported in 23 cross-sectional studies [16,17,21,23,24,[26], [27], [28], [29],31,[33], [34], [35], [36],[38], [39], [40], [41], [42], [43], [44], [45], [46]]. Results showed that in 17 out of those 23 studies, alcohol consumption remained unchanged during the lockdown for the majority of participants [17,21,23,24,[26], [27], [28],33,35,36,[38], [39], [40], [41],43,44,46]. However, a tendency towards increased alcohol consumption has been be observed for the rest of their examined participants (14.2–38.5%) in the majority of these studies (13 of 17) [17,23,24,26,27,35,[38], [39], [40], [41],43,44,46]. A decline in alcohol consumption for the majority of participants during the lockdown period was reported in four studies [16,31,34,45] and an increase of alcohol consumption was reported for the majority of the survey participants in two studies [29,42].
4. Discussion
According to our knowledge, this is the first systematic review which aim was to examine changes in snacking behavior (including both sweet and salty snacks), fast-food, food ordering habits, and alcohol consumption. In total 128292 subjects from 34 different countries around the world (Algeria, Australia, Bahrain, Belgium, Brazil, Canada, China, Egypt, France, Greece, India, Iraq, Italy, Jordan, Kuwait, Lebanon, Libya, Lithuania, Morocco, New Zealand, Oman, Palestine, Poland, Qatar, Saudi Arabia, Spain, Sudan, Syria, Tunisia, UAE, UK, USA, Yemen) were included in our systematic review, aiming to investigate potential changes in snacking and/or alcohol consumption during the first lockdown period of COVID-19.
The results of our study regarding snacking showed that although for the majority of the population examined (34.0–62.2%) snacking behavior remained unchanged during the lockdown [22,24,28,30,32,34,38], an increased consumption of both salty and sugar snacks was reported for a significant part of individuals (18.9–45.1%) [22,24,[28], [29], [30],32,34,37,38]. It has to be noted that despite the considerable heterogeneity in the definition of “snacks” (including desserts, candy, chips, nuts, crackers, popcorns, etc. [[47], [48], [49]]; most of such food items are rich in calories and poor in nutrients.
Differences in snacking behavior could be seen even within the same country. In particular, in a study lead by Pellegrini including only obese participants, 32.7% stated an increase in their daily snacking consumption during lockdown [32], whereas in the study lead by Scarmozzino, in which the population was not limited to obese people, only 18.9% reported increased consumption [38]. This could imply that for obese people, it was more difficult to control their snacking consumption during the lockdown period. Moreover, according Leech et al., snack consumption is not necessarily associated with amelioration in the overall quality of diet (especially in micronutrients intake) [50], but increase in adipose tissue had been observed [51]. Overeating (including mainly snacking) and weight gain during lockdown could lead to “Covibesity” that should not be disregarded, as it can be a potential risk factor for COVID-19 infection [52,53]. In addition, with respect to COVID-19 disease, due to the fact that a vaccine is not yet available for everyone, a balanced in macro- and micronutrients nutrition could be a method of prevention and management of the disease [54]. Therefore, these subjects could be at risk of becoming symptomatic COVID-19 patients compare to those following a balanced diet [55].
Our results regarding fast food habit showed a significant decrease in fast-food consumption during the lockdown period [19,20,24,25,28,34,35]. Only, in one study conducted in Canada, 25.0% of the participants stated increased consumption of junk food [46]. Similar results emerged after examination of the frequency of ordered food (Table 4). Only in the study from New Zealand an increased trend was observed [23]. Provided that fast food consumption as well as frequency of ordered food tended to decrease, a possible explanation could be that the long time staying at home during lockdown made people to spend more time in cooking and preparing homemade food, as has already be found in some studies [24,40,56]. In addition, an Italian study reported an increase of homemade recipes for pizza and/or sweets [56]. Another explanation could be the fear of transmission of COVID-19 disease via packets of food and delivery services, but further research is needed in this field.
Our results with respect to alcohol during the lockdown period showed that for the majority of the population examined the consumption remained stable [17,21,23,24,[26], [27], [28],33,35,36,[38], [39], [40], [41],43,44,46]. However, a significant portion of the population examined increased its alcohol consumption during the confinement time [17,23,24,26,27,29,35,[38], [39], [40], [41], [42], [43], [44],46]. Heterogeneity in results regarding alcohol consumption can be observed even in the same country. Results from China varied, where in Sun et al. [42] more than a half of the included population has increased its alcohol consumption, whereas in Yan et al. around 25% reported an increase [45]. However, in both studies the sample was not representative of the country's population. Moreover, the period of survey between these studies was different (24–31 March in Sun et al./and 15 April-11 May in Yan et al.) [42,45]. An explanation of the fact that different results emerged could be that in the beginning of the lockdown the anxiety and the fear of this unknown situation as well as the sudden change of daily life made people more prone to alcohol consumption compared to the end of lockdown.
Similar assumptions were also made about results from France [35,36] and Australia [41,43], where a tendency towards decrease in alcohol consumption at the end of the lockdown in comparison to the beginning was observed. Results from USA were also differed between the studies [17,27,39]. In Avery et al. study, which was started in March, 14.3% of the participants reported increased alcohol consumption [17], in Sharma et al. study, which was conducted in April, 23.6% of the participants increased their alcohol consumption [39], and in Knell et al. study of which the survey ended in May, 38.5% of the participants reported an increase in their alcohol consumption [27]. The same pattern was also observed in polish population where 13.8–14.6% of subjects reported increased consumption in April [21,40] and 18.1% in May [24]. Therefore, the population in USA and Poland, in contrast to Chinese, French and Australian population, found to consume more alcohol in the end compared to the beginning of the lockdown. Data regarding the period of the survey conduction was not available in Ingram et al. study [26] so as to make an assumption for the heterogenous result from UK [26,33]. However, in Ingram et al. study [26], the sample was characterized as representative, whereas in the study led by Robinson as not representative [33].
COVID-19 pandemic, led to several and sudden changes in people’ daily life and the lockdown period was full of stressf and anxiety for unknown duration [41]. In order to cope with this, a significant portion of the population relapsed to previous abuse as reported by Zhao et al. [57]. Nevertheless, subjects who often consume alcohol are not only more prone to viral and bacterial infections (including COVID-19) due to their impaired immune system [58,59], to CVD in heavy drinking occasions [60], liver [61], and pancreas diseases [62], but they also affect the quality of life of people living around them (e.g. domestic violence, neuropsychiatric disorders) [63]. However, according to a recent systematic review the evidence is not enough regarding domestic violence and alcohol abuse during COVID-19 [64], but awareness of reliability of this data is always needed [65].
Among the strengths of our study is the number of studies included as well as the fact that a significant geographical part of the world was covered. Moreover, this is the first systematic review examining changes in eating patterns (snacking, fast-food, and ordered food) as well as in alcohol consumption. In addition, all studies included in this review were assessed according to the Newcastle–Ottawa Scale (Suppl. Table 2) and were characterized from satisfactory (5∗) to very good (9∗) quality. Limitations of our studies include the fact that the sample of some studies was not representative for the population of each country and this could affect the accuracy of our results. Moreover, p-values were not reported in all our included studies, therefore not allowing us to provide information on the statistical significance of related results. Furthermore, it needs to be noted that the fact that only online/or via telephone questionnaires were used as a tool for all the surveys without any verification by other methods such as focused interviews, food diaries etc., can influence the reliability of the collected data. Lastly, in this systematic review studies only in English language were included and therefore related studies published in other languages might have been missed.
5. Conclusions
During the period of lockdown due to the COVID-19 pandemic, changes in lifestyle behaviors were observed for a significant percentage of the global population. A tendency towards increased in snacking as well as in alcohol consumption should not be disregarded because long-term problems could be arising especially in cases of repeated lockdowns in future. The observed decrease in fast-food consumption and in frequency of ordered food demonstrate an encouraging turn to home-made foods. However, provision and campaigns regarding nutritional information could be useful in order to combat with this pandemic.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author distribution
DB and MC searched the databases; DB, DJ and MC. wrote the paper; , RJ, and MC made the necessary recommendations; and DB, DJ, R.J, and MC revised the manuscript. All authors have read and approved the final version of manuscript.
Conflict of interest
The authors declare no conflict of interest.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.clnu.2021.04.020.
Appendix A. Supplementary data
The following are the Supplementary data to this article:
References
- 1.Baloch S., Baloch M.A., Zheng T., Pei X. The coronavirus disease 2019 (COVID-19) pandemic. Tohoku J Exp Med. 2020;250:271–278. doi: 10.1620/tjem.250.271. [DOI] [PubMed] [Google Scholar]
- 2.Koh D. COVID-19 lockdowns throughout the world. Occup Med (Lond). 2020:kqaa073. doi: 10.1093/occmed/kqaa073. [DOI] [Google Scholar]
- 3.Clay J.M., Parker M.O. Alcohol use and misuse during the COVID-19 pandemic: a potential public health crisis? Lancet Publ Health. 2020;5:e259. doi: 10.1016/S2468-2667(20)30088-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Anton S.D., Miller P.M. Do negative emotions predict alcohol consumption, saturated fat intake, and physical activity in older adults? Behav Modif. 2005;29:677–688. doi: 10.1177/0145445503261164. [DOI] [PubMed] [Google Scholar]
- 5.Moynihan A.B., van Tilburg W.A., Igou E.R., Wisman A., Donnelly A.E., Mulcaire J.B. Eaten up by boredom: consuming food to escape awareness of the bored self. Front Psychol. 2015;6:369. doi: 10.3389/fpsyg.2015.00369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Janati Idrissi A., Lamkaddem A., Benouajjit A., Ben El Bouaazzaoui M., El Houari F., Alami M., et al. Sleep quality and mental health in the context of COVID-19 pandemic and lockdown in Morocco. Sleep Med. 2020;74:248–253. doi: 10.1016/j.sleep.2020.07.045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Pinto J., van Zeller M., Amorim P., Pimentel A., Dantas P., Eusébio E., et al. Sleep quality in times of Covid-19 pandemic. Sleep Med. 2020;74:81–85. doi: 10.1016/j.sleep.2020.07.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Crispim C.A., Zalcman I., Dáttilo M., Padilha H.G., Edwards B., Waterhouse J., et al. The influence of sleep and sleep loss upon food intake and metabolism. Nutr Res Rev. 2007;20:195–212. doi: 10.1017/S0954422407810651. [DOI] [PubMed] [Google Scholar]
- 9.Muscogiuri G., Pugliese G., Barrea L., Savastano S., Colao A. Commentary: obesity: the "achilles heel" for COVID-19? Metabolism. 2020;108:154251. doi: 10.1016/j.metabol.2020.154251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Van Gaal L.F., Mertens I.L., De Block C.E. Mechanisms linking obesity with cardiovascular disease. Nature. 2006;444:875–880. doi: 10.1038/nature05487. [DOI] [PubMed] [Google Scholar]
- 11.Chobot A., Górowska-Kowolik K., Sokołowska M., Jarosz-Chobot P. Obesity and diabetes-Not only a simple link between two epidemics. Diab Metab Res Rev. 2018;34 doi: 10.1002/dmrr.3042. e3042-e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Health risks and benefits of alcohol consumption. Alcohol Res Health : J Natl Inst Alcohol Abuse Alcohol. 2000;24:5–11. [PMC free article] [PubMed] [Google Scholar]
- 13.Liberati A., Altman D.G., Tetzlaff J., Mulrow C., Gøtzsche P.C., Ioannidis J.P.A., et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ (Clin Res Ed) 2009;339:b2700. doi: 10.1136/bmj.b2700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Herzog R.A.-P.M., Diaz C., Del Barrio J.L., Estrada J.M., Gil A. 2013. Newcastle-Ottawa Scale adapted for cross-sectional studies. [Google Scholar]
- 15.Alhusseini N., Alqahtani A. COVID-19 pandemic's impact on eating habits in Saudi Arabia. J Publ Health Res. 2020;9:1868. doi: 10.4081/jphr.2020.1868. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ammar A., Brach M., Trabelsi K., Chtourou H. Effects of COVID-19 home confinement on eating behaviour and physical activity: results of the ECLB-COVID19. Int Online Surv. 2020;12 doi: 10.3390/nu12061583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Avery A.R., Tsang S., Seto E.Y.W., Duncan G.E. Stress, anxiety, and change in alcohol use during the COVID-19 pandemic: findings among adult twin pairs. Front Psychiatr. 2020;11:571084. doi: 10.3389/fpsyt.2020.571084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Błaszczyk-Bębenek E., Jagielski P., Bolesławska I., Jagielska A., Nitsch-Osuch A., Kawalec P. Nutrition behaviors in polish adults before and during COVID-19 lockdown. Nutrients. 2020;12 doi: 10.3390/nu12103084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Cheikh Ismail L., Osaili T.M., Mohamad M.N. 2020. Eating habits and lifestyle during COVID-19 lockdown in the United Arab Emirates: a cross-sectional study; p. 12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Cheikh Ismail L., Osaili T.M., Mohamad M.N., Al Marzouqi A., Jarrar A.H., Zampelas A., et al. Assessment of eating habits and lifestyle during coronavirus pandemic in the MENA region: a cross-sectional study. Br J Nutr. 2020:1–30. doi: 10.1017/S0007114520004547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Chodkiewicz J., Talarowska M., Miniszewska J., Nawrocka N., Bilinski P. Alcohol consumption reported during the COVID-19 pandemic: the initial stage. Int J Environ Res Publ Health. 2020;17 doi: 10.3390/ijerph17134677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Constant A., Conserve D.F., Gallopel-Morvan K., Raude J. Socio-cognitive factors associated with lifestyle changes in response to the COVID-19 epidemic in the general population: results from a cross-sectional study in France. Front Psychol. 2020;11:579460. doi: 10.3389/fpsyg.2020.579460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Gerritsen S., Egli V., Roy R., Haszard J., Backer C.D., Teunissen L., et al. Seven weeks of home-cooked meals: changes to New Zealanders' grocery shopping, cooking and eating during the COVID-19 lockdown. J Roy Soc N Z. 2020 doi: 10.1080/03036758.2020.1841010. [DOI] [Google Scholar]
- 24.Górnicka M., Drywień M.E., Zielinska M.A., Hamułka J. Dietary and lifestyle changes during covid-19 and the subsequent lockdowns among polish adults: a cross-sectional online survey plifecovid-19 study. Nutrients. 2020;12:1–23. doi: 10.3390/nu12082324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Husain W., Ashkanani F. Does COVID-19 change dietary habits and lifestyle behaviours in Kuwait: a community-based cross-sectional study. Environ Health Prev Med. 2020;25:61. doi: 10.1186/s12199-020-00901-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ingram J., Maciejewski G., Hand C.J. Changes in diet, sleep, and physical activity are associated with differences in negative mood during COVID-19 lockdown. Front Psychol. 2020;11:588604. doi: 10.3389/fpsyg.2020.588604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Knell G., Robertson M.C., Dooley E.E., Burford K., Mendez K.S. Health behavior changes during COVID-19 pandemic and subsequent "Stay-at-Home" orders. Int J Environ Res Publ Health. 2020;17 doi: 10.3390/ijerph17176268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kriaucioniene V., Bagdonaviciene L., Rodríguez-Pérez C. 2020. Associations between changes in health behaviours and body weight during the COVID-19 quarantine in Lithuania: the Lithuanian COVIDiet study; p. 12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Malta D.C., Szwarcwald C.L., Allard S.M., Knight R., Sweeney D.A., Swafford A.D. The COVID-19 Pandemic and changes in adult Brazilian lifestyles: a cross-sectional study, 2020. medRxiv : Preprint Server Health Sci. 2020;29 [Google Scholar]
- 30.V.M. Clinical Nutrition and Dietetics; Mumbai, India: 2020. The impact of COVID-19 on the dietary habits of middle-class population in mulund. [Google Scholar]
- 31.Panagiotidis P., Rantis K., Holeva V., Parlapani E., Diakogiannis I. Changes in alcohol use habits in the general population, during the COVID-19 lockdown in Greece. Dermatol Ther. 2020;55:702–704. doi: 10.1093/alcalc/agaa092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Pellegrini M., Ponzo V., Rosato R., Scumaci E., Goitre I., Benso A., et al. Changes in weight and nutritional habits in adults with obesity during the “lockdown” period caused by the COVID-19 virus emergency. Nutrients. 2020;12:1–11. doi: 10.3390/nu12072016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Robinson E., Gillespie S., Jones A. Weight-related lifestyle behaviours and the COVID-19 crisis: an online survey study of UK adults during social lockdown. Obes Sci Pract. 2020;6:735–740. doi: 10.1002/osp4.442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Rodríguez-Pérez C., Molina-Montes E., Verardo V., Artacho R., García-Villanova B., Guerra-Hernández E.J., et al. Changes in dietary behaviours during the COVID-19 outbreak confinement in the Spanish COVIDiet study. Nutrients. 2020;12:1–19. doi: 10.3390/nu12061730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Rolland B., Christensen H., Faasse K. Global changes and factors of increase in caloric/salty food intake, screen use, and substance use during the early COVID-19 containment phase in the general population in France: survey study. PloS One. 2020;6 doi: 10.2196/19630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Rossinot H., Fantin R., Venne J. Behavioral changes during COVID-19 confinement in France: a web-based study. Int J Environ Res Publ Health. 2020;17 doi: 10.3390/ijerph17228444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Sánchez-Sánchez E., Ramírez-Vargas G., Avellaneda-López Y., Orellana-Pecino J.I., García-Marín E., Díaz-Jimenez J. Eating habits and physical activity of the Spanish population during the covid-19 pandemic period. Nutrients. 2020;12:1–12. doi: 10.3390/nu12092826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Scarmozzino F., Visioli F. 2020. Covid-19 and the subsequent lockdown modified dietary habits of almost half the population in an Italian sample; p. 9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Sharma P., Dai J., Shi J., Huang J., Hu C., Wu L., et al. Changes in substance use among young adults during a respiratory disease pandemic. Hepatol Commun. 2020;8 doi: 10.1177/2050312120965321. 2050312120965321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Sidor A., Rzymski P. vol. 12. 2020. (Dietary choices and habits during COVID-19 lockdown: experience from Poland). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Stanton R., To Q.G. vol. 17. 2020. (Depression, anxiety and stress during COVID-19: associations with changes in physical activity, sleep, tobacco and alcohol use in Australian adults). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Sun Y., Li Y., Bao Y., Meng S., Sun Y., Schumann G., et al. Brief report: increased addictive internet and substance use behavior during the COVID-19 pandemic in China. 2020;29:268–270. doi: 10.1111/ajad.13066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Tran T.D., Hammarberg K., Kirkman M., Nguyen H.T.M., Fisher J. Alcohol use and mental health status during the first months of COVID-19 pandemic in Australia. J Affect Disord. 2020;277:810–813. doi: 10.1016/j.jad.2020.09.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Vanderbruggen N., Matthys F., Van Laere S., Zeeuws D., Santermans L., Van den Ameele S., et al. Self-reported alcohol, tobacco, and cannabis use during COVID-19 lockdown measures: results from a web-based survey. Eur Addiction Res. 2020;26:309–315. doi: 10.1159/000510822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Yan A.F., Sun X., Zheng J., Mi B., Zuo H., Ruan G., et al. Perceived risk, behavior changes and Health-related outcomes during COVID-19 pandemic: findings among adults with and without diabetes in China. Diabetes Res Clin Pract. 2020;167 doi: 10.1016/j.diabres.2020.108350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Zajacova A., Jehn A., Stackhouse M., Denice P., Ramos H. Changes in health behaviours during early COVID-19 and socio-demographic disparities: a cross-sectional analysis. Canad J Publ Health Revue canadienne de sante publique. 2020:1–10. doi: 10.17269/s41997-020-00434-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Piernas C., Popkin B.M. Snacking increased among U.S. adults between 1977 and 2006. J Nutr. 2010;140:325–332. doi: 10.3945/jn.109.112763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Wang Z., Zhai F., Zhang B., Popkin B.M. Trends in Chinese snacking behaviors and patterns and the social-demographic role between 1991 and 2009. Asia Pac J Clin Nutr. 2012;21:253–262. [PMC free article] [PubMed] [Google Scholar]
- 49.Johnson G.H., Anderson G.H. Snacking definitions: impact on interpretation of the literature and dietary recommendations. Crit Rev Food Sci Nutr. 2010;50:848–871. doi: 10.1080/10408390903572479. [DOI] [PubMed] [Google Scholar]
- 50.Leech R.M., Livingstone K.M., Worsley A., Timperio A., McNaughton S.A. Meal frequency but not snack frequency is associated with micronutrient intakes and overall diet quality in Australian men and women. J Nutr. 2016;146:2027–2034. doi: 10.3945/jn.116.234070. [DOI] [PubMed] [Google Scholar]
- 51.Leech R.M., Timperio A., Livingstone K.M., Worsley A., McNaughton S.A. Temporal eating patterns: associations with nutrient intakes, diet quality, and measures of adiposity. Am J Clin Nutr. 2017;106:1121–1130. doi: 10.3945/ajcn.117.156588. [DOI] [PubMed] [Google Scholar]
- 52.Khan M.A., Moverley Smith J.E. Covibesity," a new pandemic. Obes Med. 2020;19:100282. doi: 10.1016/j.obmed.2020.100282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Jayawardena R., Jeyakumar D.T., Misra A., Hills A.P., Ranasinghe P. Obesity: a potential risk factor for infection and mortality in the current COVID-19 epidemic. Diab Metab Syndr. 2020;14:2199–2203. doi: 10.1016/j.dsx.2020.11.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Jayawardena R., Sooriyaarachchi P., Chourdakis M., Jeewandara C., Ranasinghe P. Enhancing immunity in viral infections, with special emphasis on COVID-19: a review. Diab Metab Syndr. 2020;14:367–382. doi: 10.1016/j.dsx.2020.04.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Jayawardena R., Misra A. Balanced diet is a major casualty in COVID-19. Diab Metab Syndr. 2020;14:1085–1086. doi: 10.1016/j.dsx.2020.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Di Renzo L., Gualtieri P., Pivari F. Eating habits and lifestyle changes during COVID-19 lItal Survockdown: an Italian surve. y. 2020;18:229. doi: 10.1186/s12967-020-02399-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Zhao A., Li Z., Ke Y., Huo S., Ma Y., Zhang Y., et al. Dietary diversity among Chinese residents during the COVID-19 outbreak and its associated factors. Nutrients. 2020;12 doi: 10.3390/nu12061699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Rehm J., Parry C.D. Alcohol consumption and infectious diseases in South Africa. Lancet (London, England) 2009;374:2053. doi: 10.1016/S0140-6736(09)62150-4. [DOI] [PubMed] [Google Scholar]
- 59.Testino G. Are patients with alcohol use disorders at increased risk for covid-19 infection? Alcohol Alcohol. 2020;55:344–346. doi: 10.1093/alcalc/agaa037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Roerecke M., Rehm J. Irregular heavy drinking occasions and risk of ischemic heart disease: a systematic review and meta-analysis. Am J Epidemiol. 2010;171:633–644. doi: 10.1093/aje/kwp451. [DOI] [PubMed] [Google Scholar]
- 61.Osna N.A., Donohue T.M., Jr., Kharbanda K.K. Alcoholic liver disease: pathogenesis and current management. Alcohol Res Curr Rev. 2017;38:147–161. doi: 10.35946/arcr.v38.2.01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Irving H.M., Samokhvalov A.V., Rehm J. Alcohol as a risk factor for pancreatitis. A systematic review and meta-analysis. JOP : J Pancreas. 2009;10:387–392. [PMC free article] [PubMed] [Google Scholar]
- 63.Rehm J. The risks associated with alcohol use and alcoholism. Alcohol Res Health : J Natl Inst Alcohol Abuse Alcohol. 2011;34:135–143. [PMC free article] [PubMed] [Google Scholar]
- 64.Abdo C., Miranda E.P., Santos C.S., Júnior J.B., Bernardo W.M. Domestic violence and substance abuse during COVID19: a systematic review. Indian J Psychiatr. 2020;62:S337–S342. doi: 10.4103/psychiatry.IndianJPsychiatry_1049_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Sacco M.A., Caputo F., Ricci P., Sicilia F., De Aloe L., Bonetta C.F., et al. The impact of the Covid-19 pandemic on domestic violence: the dark side of home isolation during quarantine. Med Leg J. 2020;88:71–73. doi: 10.1177/0025817220930553. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.