Abstract
Context:
One fundamental way to honor patient autonomy is to establish and enact their wishes for end of life care. Limited research exists regarding adherence with code status.
Objectives:
This study aimed to characterize cardiopulmonary resuscitation attempts discordant with documented code status at the time of death in the United States and to elucidate potential contributing factors.
Methods:
The Cerner APACHE outcomes database, which includes 237 U.S. hospitals that collect manually abstracted data from all critical care patients, was queried for adults admitted to intensive care units with a documented code status at the time of death from January 2008 to December 2016. The primary outcome was discordant cardiopulmonary resuscitation at death. Multivariable logistic regression models were used to identify patient-, and hospital-level associated factors after adjustment for age, hospital, and illness severity (APACHE III score).
Results:
A total of 21,537 patients from 56 hospitals were included. Of patients with a do-not-resuscitate code status, 149 (0.8%) received cardiopulmonary resuscitation at death and associated factors included: Black race, higher APACHE III score or treatment in small or non-teaching hospitals. Of patients with a full code status, 203 (9.0%) did not receive cardiopulmonary resuscitation at death and associated factors included: higher APACHE III score, primary neurologic or trauma diagnosis, or admission in a more recent year.
Conclusion:
At the time of death, 1.6% of patients received or did not undergo cardiopulmonary resuscitation in a manner discordant with their documented code statuses. Race, and institutional factors were associated with discordant resuscitation, and addressing these disparities may promote concordant end-of-life care in all patients.
Keywords: Code Status, Discordant Care, Cardiopulmonary Resuscitation
Introduction
Of the 200,000 in-hospital cardiac arrests that occur annually in the United States, studies estimate only 22% of patients survive to discharge.1,2 Cardiac arrests occur most frequently in the intensive care unit (ICU), with 5.6–78.1 cardiac arrests per 1,000 admissions, and these events have worse outcomes.3,4 Current standard of care for cardiopulmonary arrest, regardless of where it occurs, is the immediate provision of cardiopulmonary resuscitation (CPR). CPR may involve chest compressions, defibrillation, intubation, and the administration of advanced cardiac life support medications. Cardiopulmonary arrest and the subsequent interventions can result in significant morbidity, including rib fractures (29% of patients) and/or debilitating brain injury.5 Of those who survive, 28% have clinically significant neurologic disability and 10% have severe disability.2 These complications can result in prolonged hospital length of stay (LOS), high rate of nursing home placement, increased healthcare costs, and poor quality of life.5 Given these poor outcomes, some patients elect to forgo CPR in the event of cardiopulmonary arrest. This decision is documented as a full or partial “Do-Not-Resuscitate” (DNR) rather than “Full Code” (FC) status.
There are many ethical issues surrounding resuscitation and code status. A code status exemplifies the ethical principle of patient autonomy, in which a patient (possessing decision-making capacity) has the right to dictate their own care.6 Additionally, the ethical principle of justice dictates that life-sustaining treatment preferences and delivery should be elicited and provided without variation due to racial, regional or other differences.7 While current practices have moved away from medical paternalism, physician judgment remains vital to promote non-maleficence when a potentially harmful intervention will not lead to benefit for patients.7 There are also potential consequences for caregivers involved in nonbeneficial interventions, including personal safety and moral distress.7–10
The ultimate realization of patient-centered end-of-life care is concordance between stated preferences and the care delivered.11 Studies to date report wide variation in over- or under-treatment inconsistent with patients’ wishes.12–18 Despite well-publicized accounts in the media, the national incidence of discordant CPR in the U.S. is unknown.19 Thus far, race has been identified as a significant risk factor for receiving discordant end-of-life care, and substantial variation exists between hospitals.13,16 Finally, discordance between a patient’s wishes documented in a chart and care delivered is not always a failure, as the chart cannot capture all of the nuance in a patient’s real time end-of-life care. Given the knowledge gap surrounding the frequency of and factors driving discordant CPR, the purpose of this study was quantify and characterize the prevalence of discordant CPR in patients admitted to ICUs in the US over the past decade.
Materials and Methods
Data Source
Data were abstracted from the Cerner APACHE outcomes database (Cerner Corporation, Kansas City, MO), which includes data from all patients requiring ICU admission at 237 participating hospitals.20 The APACHE database is a national quality improvement and benchmarking program that collects physiologic, clinical, demographic, and admission source data. These data are prospectively and manually abstracted by trained clinical abstractors. Data quality is ensured through recurring quality reviews and self-audits. Data collection, auditing, and validity have been previously described.21–26
This study was approved by the University of Minnesota Institutional Review Board (STUDY00001489). Individual patient consent was waived, as all data used in the study were obtained from a pre-existing de-identified database.
Participants
Adults (age ≥ 18 years old) admitted to the ICU at participating centers between January 1, 2008, and December 31, 2016 who died prior to hospital discharge were included in the analysis. Hospitals (n=56) that submitted code status at death were included. To ensure our analysis included patients with curative or comfort focused care, complete years of data, and hospitals with a sufficient census of critical care patients; we excluded patients if they were: undergoing maintenance of circulatory support for organ procurement, admitted during years with less than 350 total observations, if the hospital submitted data for less than 50 patients during the study period, or if the CPR at time of death (1.5%) or death code status (< 1%) fields were missing (Figure 1).
Figure 1.
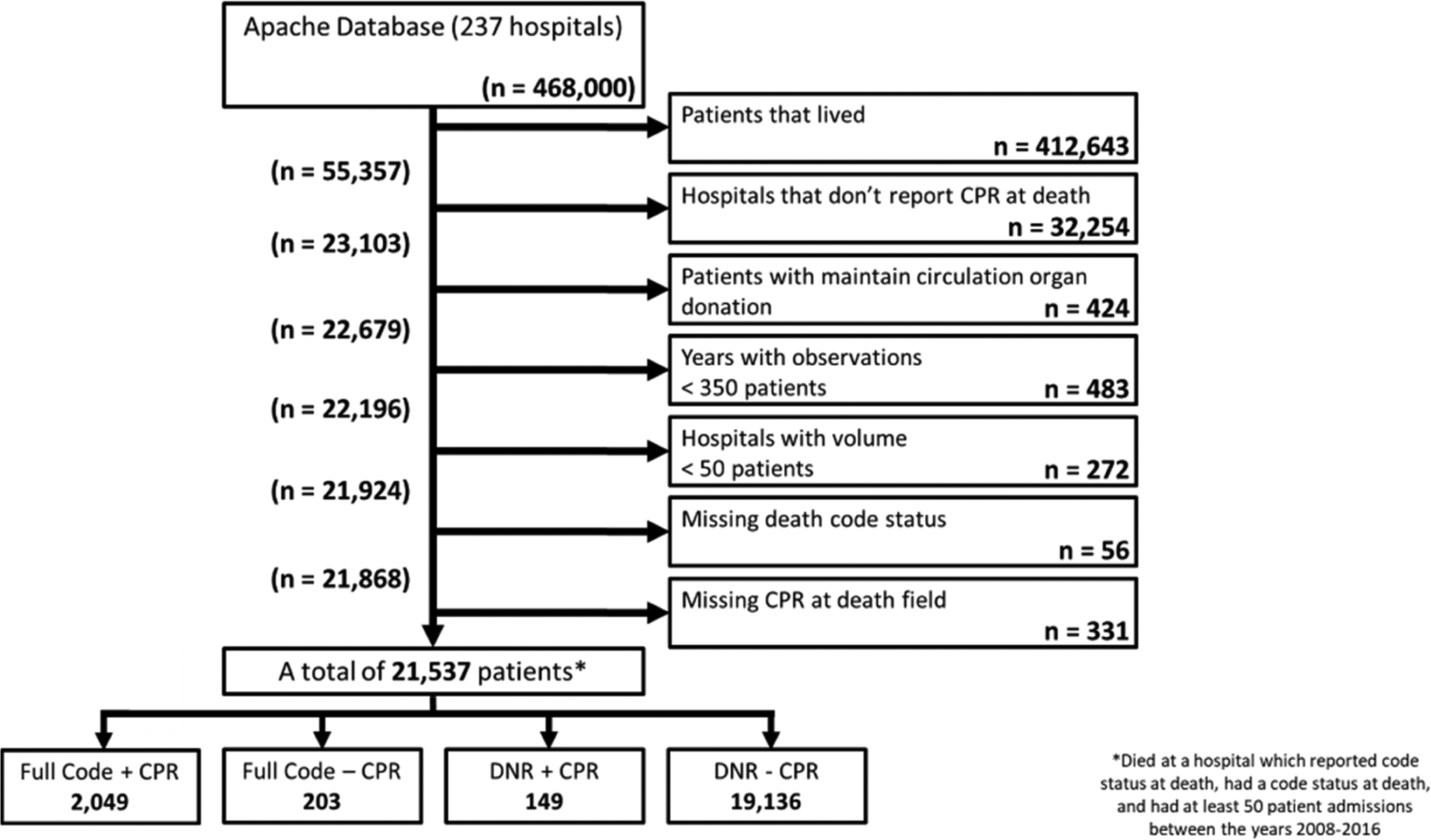
Inclusion and Exclusion Criteria
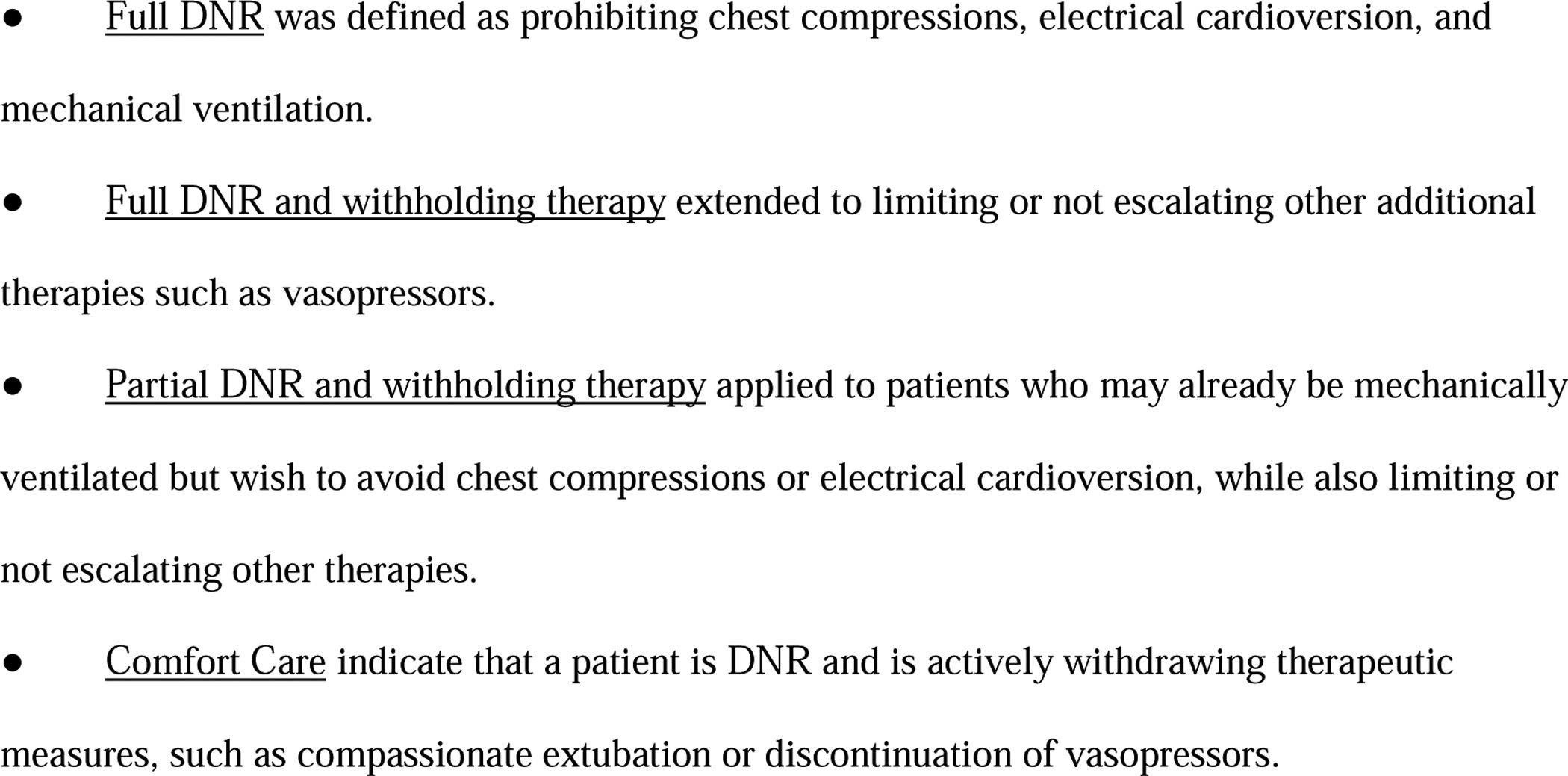
Cohort Classification
Admission and time of death code statuses that explicitly prohibited CPR (as listed in Appendix 1) were reclassified as DNR.27 Patients were divided into four cohorts based on code status and administration of CPR at death: FC with CPR, FC without CPR, DNR with CPR, and DNR without CPR. “Discordant CPR” was defined as a patient with DNR status receiving CPR or a FC patient not receiving CPR. Code status at death and CPR at death were unique variables in the APACHE database. Data for these variables were manually abstracted by APACHE personnel.
Outcomes and Measures
The primary outcome was the rate of discordant CPR and variables evaluated for their associations with the outcomes included patient- and hospital-level variables. Patient-level variables included demographics, illness severity, and admission characteristics. Illness severity was determined using APACHE III score which is commonly used for risk-adjusted outcome comparisons.21 It compliles physiologic and biochemical variables available within the first 24 hours of admission along with chornic health variables into a single score for each patient. Hospital-level variables included racial makeup of the patient population (categorized as minority [>50%], mixed-race [25%−50%], or majority [<25%]),28 bed size, teaching status, critical care management (i.e. intensivist-led ICU vs. non-intensivist-led, where the critical care team acts as a consulting rather than primary team), and regional location (U.S. Northeast, South, Midwest, and West).
Statistical Methods
For descriptive purposes we compared those who received concordant vs. discordant resusciatation within their respective code status at death groups. Normally distributed continuous variables were expressed as mean and standard deviation (SD) and non-normally distributed continuous variables were expressed as median and interquartile range (IQR). Continuous variables with normal distribution were compared using student t-tests, and non-normal distributions were compared using Wilcoxon rank-sum tests. Categorical variables were expressed as percentages, and compared using Pearson χ2 tests. Imputation was not performed as missingness of data was less than 5% (mean: 0.5%, median 0%, range: 0–2.6%).29 Multi-level mixed-effects logistic regression models were used to evaluate patient and hospital-level factors associated with discordant CPR, using separate models for DNR patients who received CPR and FC patients who did not receive CPR. Both models accounted for patient-level fixed effects (demographics [age, sex, race/ethnicity, insurance], admission characteristics [primary diagnosis, surgical vs non-surgical admission], illness severity [APACHE III score]), hospital-level fixed effects (racial makeup, size, teaching status, and location), and random effects at the hospital level. The Hosmer-Lemeshow goodness-of-fit test was used to confirm that the models adequately fit the data (P > 0.10). Discrimination was assessed by the C-statistic. Alpha was set at 0.05, 2-tailed. All analyses were conducted using Stata MP, version 15 (StataCorp, College Station, TX).
Results
A total of 21,537 patients from 56 hospitals were included in the final analysis (Figure 1). Table 1 shows patient characteristics for each cohort. A total of 352 patients (1.6%) had discordant CPR, including 203 FC patients (9%) who did not receive CPR and 149 DNR patients (08%) who received CPR at death. The percentage of both FC and DNR patients who underwent discordant resuscitation increased over time from 0.4% in 2008 to 1.3% in 2015 (Table 1). 85% of patients on admission to the ICU were FC, whereas by time of death, 62% were comfort care, 28% DNR and only 10% FC. Per code status, discordant CPR (either providing or not providing CPR discordant with wishes) was most common in FC (9%) and limited withholding treatment (7%) and least common in patients with a comfort care code status (0.3%). Cardiovascular was the most common primary admission diagnosis in patients who received CPR from both DNR and FC groups (63.1% and 61.2%, respectively). DNR patients that did not receive CPR more commonly died on the floor (17.6%) than the other three groups. In both code status groups, discordant CPR was more likely to occur when critical care was consulted compared to primary management by the critical care team.
Table 1.
Patient and Hospital Characteristics by Code +/− Cardiopulmonary Resuscitation Category
| Variable | Full Code (+) CPR | Full Code (−) CPR | DNR (+) CPR | DNR (−) CPR |
|---|---|---|---|---|
| Patients – no.(%) | 2049 (91.0) | 203 (9.0) | 149 (0.8) | 19136 (99.2) |
| Age – median (IQR) | 66 (55, 76) | 63 (49, 75) | 71 (57, 80) | 72 (61, 82) |
| Female – no.(%) | 879 (42.9) | 80 (39.4) | 64 (43.0) | 8883 (46.4) |
| Race – no.(%) † | ||||
| White | 1486 (74.0) | 158 (79.4) | 106 (73.1) | 16118 (85.8) |
| Black | 354 (17.6) | 17 (8.5) | 31 (21.4) | 1527 (8.1) |
| Hispanic | 38 (1.9) | 5 (2.5) | 2 (1.4) | 209 (1.1) |
| Asian | 28 (1.4) | 3 (1.5) | 2 (1.4) | 187 (1.0) |
| American Indian/Alaska Native/Australian Aborigine | 46 (2.3) | 3 (1.5) | 2 (1.4) | 387 (2.1) |
| Other | 56 (2.8) | 13 (6.5) | 2 (1.4) | 360 (1.9) |
| Insurance – no.(%) | ||||
| Managed Care | 189 (9.3) | 26 (12.9) | 8 (5.5) | 1358 (7.2) |
| Medicare | 1152 (56.9) | 90 (44.6) | 95 (65.1) | 13103 (69.1) |
| Self-Pay | 155 (7.7) | 21 (10.4) | 6 (4.1) | 873 (4.6) |
| Private | 205 (10.1) | 28 (13.9) | 18 (12.3) | 1564 (8.2) |
| Medicaid | 243 (12.0) | 32 (15.8) | 17 (11.6) | 1573 (8.3) |
| Government | 44 (2.2) | 2 (1.0) | 2 (1.4) | 313 (1.6) |
| Admission year – no.(% of all deaths that year) | ||||
| 2008 | 63 (3.1) | 2 (1.0) | 1 (0.7) | 612 (3.2) |
| 2009 | 109 (5.3) | 6 (3.0) | 3 (2.0) | 921 (4.8) |
| 2010 | 140 (6.8) | 9 (4.4) | 7 (4.7) | 1401 (7.3) |
| 2011 | 204 (10.0) | 13 (6.4) | 4 (2.7) | 1650 (8.6) |
| 2012 | 199 (9.7) | 19 (9.4) | 16 (10.7) | 1686 (8.8) |
| 2013 | 322 (15.7) | 40 (19.7) | 30 (20.1) | 2843 (14.9) |
| 2014 | 328 (16.0) | 48 (23.6) | 28 (18.8) | 3077 (16.1) |
| 2015 | 393 (19.2) | 38 (18.7) | 41 (27.5) | 3723 (19.5) |
| 2016 | 291 (14.2) | 28 (13.8) | 19 (12.8) | 3223 (16.8) |
| Location at death – no.(%) | ||||
| Floor | 66 (3.2) | 12 (5.9) | 5 (3.4) | 3377 (17.6) |
| Floor with Telemetry | 32 (1.6) | 1 (0.5) | 0 (0.0) | 366 (1.9) |
| Hospice | 0 (0.0) | 0 (0.0) | 0 (0.0) | 108 (0.6) |
| Intensive Care Unit | 1833 (89.5) | 175 (86.2) | 140 (94.0) | 14499 (75.8) |
| Procedure Suite | 18 (0.9) | 1 (0.5) | 0 (0.0) | 2 (<1) |
| Operating Room | 19 (0.9) | 1 (0.5) | 0 (0.0) | 2 (<1) |
| Other ‡ | 3 (0.1) | 0 (0.0) | 0 (0.0) | 17 (0.1) |
| Post Anesthesia Care Unit | 1 (<1) | 0 (0.0) | 1 (0.7) | 5 (<1) |
| Stepdown | 56 (2.7) | 11 (5.4) | 2 (1.3) | 613 (3.2) |
| Telemetry | 21 (1.0) | 2 (1.0) | 1 (0.7) | 147 (0.8) |
| APACHE III SCORE – mean (SD) | 90.8 (41.5) | 95.4 (39.8) | 99.1 (41.3) | 86.9 (35.3) |
| ICU LOS Days – median (IQR) | 2 (1.0, 5.0) | 3 (2.0, 5.0) | 2 (2.0, 5.0) | 4 (2.0, 7.0) |
| ICU Admit code status – no.(%) | ||||
| Full Code | 2027 (99.0) | 191 (94.1) | 131 (87.9) | 15826 (82.9) |
| DNR | 10 (0.5) | 8 (3.9) | 8 (5.4) | 2144 (11.2) |
| Limited/Withholding Treatment | 9 (0.4) | 4 (2.0) | 9 (6.0) | 667 (3.5) |
| DNR & Withholding Treatment | 2 (0.1) | 0 (0.0) | 1 (0.7) | 379 (2.0) |
| Comfort Care | 0 (0.0) | 0 (0.0) | 0 (0.0) | 77 (0.4) |
| Death code status – no.(%) | ||||
| Full Code | 2049 (100.0) | 203 (100.0) | 0 (0.0) | 0 (0.0) |
| DNR | 0 (0.0) | 0 (0.0) | 51 (34.2) | 4375 (22.9) |
| Limited/Withholding Treatment | 0 (0.0) | 0 (0.0) | 57 (38.3) | 757 (4.0) |
| DNR & Withholding Treatment | 0 (0.0) | 0 (0.0) | 7 (4.7) | 715 (3.7) |
| Comfort Care | 0 (0.0) | 0 (0.0) | 34 (22.8) | 13289 (69.4) |
| ICU Admit 1° Organ/System – no.(%) | ||||
| Cardiovascular | 1255 (61.2) | 100 (49.3) | 94 (63.1) | 9224 (48.2) |
| Respiratory | 348 (17.0) | 26 (12.8) | 30 (20.1) | 3734 (19.5) |
| Gastrointestinal | 172 (8.4) | 21 (10.3) | 5 (3.4) | 1823 (9.5) |
| Neurological | 93 (4.5) | 26 (12.8) | 11 (7.4) | 2619 (13.7) |
| Genitourinary | 41 (2.0) | 3 (1.5) | 0 (0.0) | 308 (1.6) |
| Metabolic/Endocrine | 18 (0.9) | 0 (0.0) | 0 (0.0) | 171 (0.9) |
| Hematologic | 15 (0.7) | 1 (0.5) | 1 (0.7) | 116 (0.6) |
| Musculoskeletal/Skin | 19 (0.9) | 1 (0.5) | 1 (0.7) | 118 (0.6) |
| Trauma | 84 (4.1) | 23 (11.3) | 7 (4.7) | 1016 (5.3) |
| Transplant | 4 (0.2) | 2 (1.0) | 0 (0.0) | 7 (<1) |
| Surgery 10 indication – no.(%) | 253 (12.3) | 26 (12.8) | 11 (7.4) | 1769 (9.2) |
| Critical Care Team – no.(%) | ||||
| Primary | 1550 (75.6) | 169 (83.3) | 100 (67.1) | 15771 (82.4) |
| Consulted | 511 (24.9) | 72 (35.5) | 62 (41.6) | 3871 (20.2) |
| Hospital Minority Population – no.(%) § | ||||
| Majority | 1528 (74.6) | 162 (79.8) | 94 (63.1) | 16075 (84.0) |
| Mixed-Race | 381 (18.6) | 35 (17.2) | 43 (28.9) | 2278 (11.9) |
| Minority | 140 (6.8) | 6 (3.0) | 12 (8.1) | 783 (4.1) |
| Hospital Bed # – median (IQR) | 400 (315, 600) | 529 (393, 954) | 450 (315, 1289) | 400 (325, 600) |
| Hospital Teaching Type – no.(%) ¶ | ||||
| Large Teaching | 888 (43.3) | 98 (48.3) | 28 (18.8) | 9913 (51.8) |
| Small Teaching | 565 (27.6) | 41 (20.2) | 56 (37.6) | 4618 (24.1) |
| Non-Teaching | 596 (29.1) | 64 (31.5) | 65 (43.6) | 4605 (24.1) |
| Hospital Regional Location – no.(%) | ||||
| Northeast | 446 (21.8) | 59 (29.1) | 23 (15.4) | 5333 (27.9) |
| South | 555 (27.1) | 50 (24.6) | 56 (37.6) | 3796 (19.8) |
| Midwest | 855 (41.7) | 74 (36.5) | 58 (38.9) | 8103 (42.3) |
| West | 193 (9.4) | 20 (9.9) | 12 (8.1) | 1904 (9.9) |
P values are based on Pearson’s chi-square test for categorical variables, student t-test for normally distributed continuous variables, and Wilcoxon rank-sum test for continuous variables with skewed distribution.
Race and ethnic group were determined from medical records.
Other locations include transfer or unknown.
Hospitals were stratified into 3 groups based on the proportion of minority patients: predominantly majority hospitals (<25% of patients are minority patients), mixed hospitals (25%–50% of patients are minority patients), and predominantly minority hospitals (>50% of patients are minority patients)
Hospitals were split in to teaching and non-teaching based on presence of trainees. Large defined as >600 hospital beds.
Discordant CPR rates varied across hospitals (FC without CPR [median 0.8%, range 0 – 4.3%], DNR with CPR [median 0.7%, range 0 – 3.8%]) (Figure 2). Only 4 (7.1%) hospitals had zero patients with discordant resuscitation. Forty-six hospitals (82.1%) had at least one patient not receive CPR in the setting of FC documentation at the time of death (maximum rate of 4.3%). Forty-three hospitals (76.8%) had at least one patient receive CPR despite DNR documentation (maximum rate 3.8%).
Figure 2.
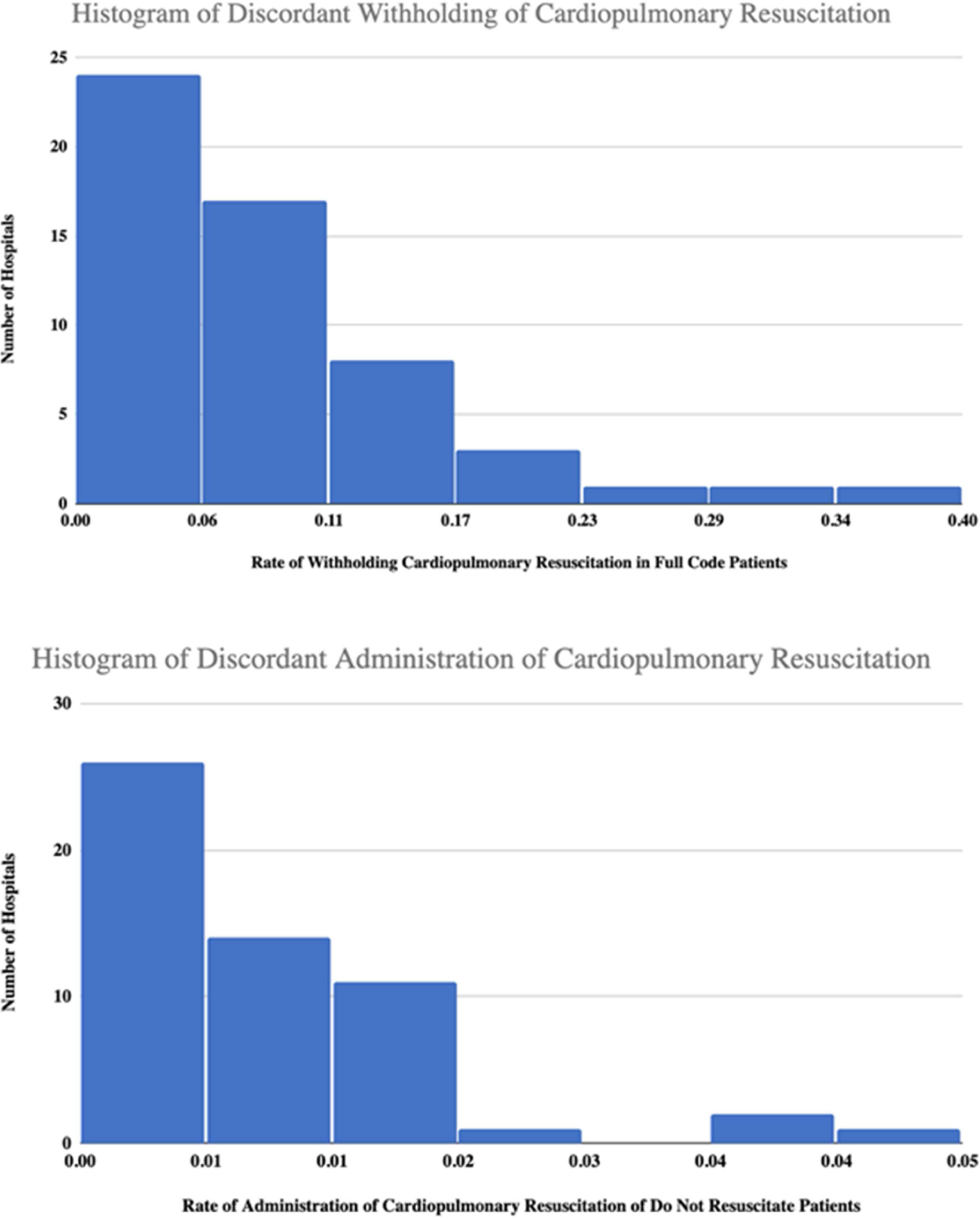
Histograms of Discordant Cardiopulmonary Resuscitation
Variables associated with an increased odds of not receiving CPR when FC included: DNR code status on admission (OR=16.9, 95% CI 5.2–54.7, p<0.001), a higher APACHE III score (OR=1.01, 95% CI 1.002–1.01, p=0.01), admission with a neurological (OR=3.7, 95% CI 2.1–6.4, p<0.001), trauma (OR=3.1, 95% CI 1.7–5.7, p<0.001), or gastrointestinal (OR=1.8, 95% CI 1.03–3.09, p=0.04) related admission diagnosis when compared to FC patients who received CPR (Table 2). Discordant CPR in FC patients increased over time with the highest association in 2014 (OR=8.2 95% CI 1.8–37.1, p=0.01). Protective factors were only seen at the hospital-level. FC patients admitted to a hospital in the South (OR=0.4, 95% CI 0.2–0.8, p=0.02) or Midwest regions (OR=0.5, 95% CI 0.3–0.8, p=0.01) had lower odds of not receiving CPR when compared to patients admitted to the Northeast.
Table 2.
Mixed-effects Model Comparing Discordant Cardiopulmonary Resuscitation to Concordant Care
| Variable | Full Code (−) CPR | DNR (+) CPR | ||||
|---|---|---|---|---|---|---|
| OR | 95% CI | P value | OR | 95% CI | P value | |
| Age | 1.00 | 0.98 – 1.01 | 0.42 | 0.99 | 0.98 – 1.00 | 0.18 |
| Sex | ||||||
| Female | - | ref | ||||
| Male | 1.03 | 0.75 – 1.41 | 0.88 | 1.20 | 0.86 – 1.69 | 0.29 |
| Race/Ethnicity | ||||||
| White | - | ref | ||||
| Black | 0.57 | 0.32 – 1.01 | 0.05 | 2.26 | 1.41 – 3.63 | <0.001 |
| Hispanic | 0.86 | 0.29 – 2.53 | 0.79 | 1.59 | 0.37 – 6.87 | 0.53 |
| Asian | 0.85 | 0.24 – 3.04 | 0.80 | 1.38 | 0.33 – 5.76 | 0.66 |
| American Indian/Alaskan Native/Australian Aborigine | 0.31 | 0.05 – 1.99 | 0.22 | 0.41 | 0.07 – 2.26 | 0.31 |
| Other | 1.62 | 0.82 – 3.20 | 0.16 | 0.46 | 0.11 – 1.90 | 0.28 |
| Admit Code Status | ||||||
| Full Code | - | ref | ||||
| DNR | 16.89 | 5.22 – 54.66 | <0.001 | 0.58 | 0.28 – 1.20 | 0.14 |
| Limited/Witholding Tx | 3.22 | 0.87 – 11.85 | 0.08 | 1.77 | 0.85 – 3.70 | 0.13 |
| Critical Care Involvement | ||||||
| Primary Critical Care Management | - | ref | ||||
| Critical Care Consulting | 1.42 | 0.93 – 2.17 | 0.11 | 1.35 | 0.83 – 2.21 | 0.23 |
| Insurance | ||||||
| Managed Care | - | ref | ||||
| Medicare | 0.71 | 0.41 – 1.23 | 0.22 | 1.32 | 0.61 – 2.88 | 0.48 |
| Self-Pay | 0.87 | 0.44 – 1.72 | 0.69 | 0.73 | 0.25 – 2.15 | 0.57 |
| Private | 1.13 | 0.60 – 2.13 | 0.71 | 1.61 | 0.68 – 3.84 | 0.28 |
| Medicaid | 1.00 | 0.54 – 1.83 | 0.99 | 1.27 | 0.53 – 3.00 | 0.59 |
| Government | 0.41 | 0.09 – 1.90 | 0.26 | 0.80 | 0.16 – 3.91 | 0.78 |
| Surgery as primary indication | 0.88 | 0.52 – 1.47 | 0.61 | 1.36 | 0.68 – 2.73 | 0.38 |
| ICU Admit 1° Organ/System Failure | ||||||
| Cardiovascular | - | ref | ||||
| Respiratory | 0.87 | 0.54 – 1.42 | 0.58 | 0.70 | 0.44 – 1.13 | 0.14 |
| Gastrointestinal | 1.79 | 1.03 – 3.09 | 0.04 | 0.30 | 0.12 – 0.78 | 0.01 |
| Neurological | 3.71 | 2.14 – 6.44 | <0.001 | 0.52 | 0.27 – 1.01 | 0.06 |
| Hematologic | 1.17 | 0.14 – 9.48 | 0.89 | 0.80 | 0.11 – 5.84 | 0.82 |
| Musculoskeletal/Skin | 0.53 | 0.06 – 4.38 | 0.56 | 0.85 | 0.11 – 6.70 | 0.88 |
| Trauma | 3.11 | 1.70 – 5.69 | <0.001 | 1.12 | 0.49 – 2.55 | 0.79 |
| APACHE III Score | 1.01 | 1.00 – 1.01 | 0.01 | 1.01 | 1.00 – 1.01 | 0.02 |
| Admission Year | ||||||
| 2008 | - | ref | ||||
| 2009 | 2.20 | 0.41 – 11.81 | 0.36 | 2.17 | 0.22 – 21.08 | 0.50 |
| 2010 | 2.10 | 0.41 – 10.72 | 0.37 | 4.03 | 0.49 – 33.12 | 0.20 |
| 2011 | 3.16 | 0.65 – 15.28 | 0.15 | 2.16 | 0.24 – 19.86 | 0.50 |
| 2012 | 5.24 | 1.11 – 24.67 | 0.04 | 6.01 | 0.77 – 47.07 | 0.09 |
| 2013 | 6.24 | 1.37 – 28.37 | 0.02 | 4.87 | 0.64 – 37.04 | 0.13 |
| 2014 | 8.22 | 1.82 – 37.11 | 0.01 | 3.96 | 0.52 – 30.21 | 0.19 |
| 2015 | 4.71 | 1.04 – 21.34 | 0.05 | 4.49 | 0.60 – 33.80 | 0.15 |
| 2016 | 4.84 | 1.05 – 22.34 | 0.04 | 2.98 | 0.39 – 23.01 | 0.30 |
| Hospital Number of Beds | 1.00 | 1.00 – 1.00 | 0.04 | 1.00 | 1.00 – 1.00 | 0.08 |
| Hospital Minority Population* | ||||||
| Majority | - | ref | ||||
| Mixed | 0.80 | 0.44 – 1.44 | 0.46 | 1.68 | 0.88 – 3.20 | 0.11 |
| Minority | 0.78 | 0.22 – 2.74 | 0.70 | 1.86 | 0.81 – 4.24 | 0.14 |
| Hospital Teaching Type† | ||||||
| Large teaching | - | ref | ||||
| Small teaching | 0.87 | 0.53 – 1.43 | 0.59 | 5.51 | 3.13 – 9.69 | <0.001 |
| Non-teaching | 1.15 | 0.58 – 2.29 | 0.69 | 6.77 | 3.13 – 14.63 | <0.001 |
| Hospital Regional Location | ||||||
| Northeast | - | ref | ||||
| South | 0.36 | 0.15 – 0.84 | 0.02 | 0.28 | 0.12 – 0.66 | <0.004 |
| Midwest | 0.53 | 0.34 – 0.83 | 0.01 | 0.64 | 0.35 – 1.16 | 0.14 |
| West | 1.39 | 0.63 – 3.04 | 0.42 | 0.41 | 0.16 – 1.00 | 0.05 |
Hospitals were stratified into 3 groups based on the proportion of minority patients: predominantly majority hospitals (<25% of patients are minority patients), mixed hospitals (25%–50% of patients are minority patients), and predominantly minority hospitals (>50% of patients are minority patients)
Hospitals were split in to teaching and non-teaching based on presence of trainees. Large defined as >600 hospital beds.
In DNR patients, Black (OR=2.3, 95% CI 1.4–3.6, p<0.001) compared to white patients, APACHE III score (OR=1.01, 95% CI 1.001–1.01, p=0.02), admission to a small-teaching (OR=5.5, 95% CI 3.1–9.7, p<0.001), or non-teaching hospital (OR=6.8, 95% CI 3.1–14.6, p<0.001) compared to large-teaching hospital was associated with higher odds of discordant CPR. DNR patients with a gastrointestinal related admission diagnosis (OR=0.30, 95% CI 0.12–0.78, p=0.01) or those admitted to a hospital in the South (OR=0.28, 95% CI 0.12–0.66, p=0.004) had lower to receive CPR at death.
Discussion
Of the 21,537 ICU patients included in this study, 0.8% of DNR patients received discordant CPR and 9.0% of FC patients had discordant CPR (i.e. not provided) at death. DNR patients were more likely to receive discordant CPR at death if they were Black, had a higher APACHE III score, or were treated in small or non-teaching hospitals, and less likely if they were treated in the South or had a primary gastrointestinal diagnosis. FC patients were less likely to have CPR not provided at death if they were treated in the South or Midwest, and more likely to have CPR not provided if they had a DNR code status on admission, higher APACHE III score, primary neurologic or trauma diagnosis or were admitted in a more recent year.
In this study of ICU non-survivors, Black patients were more likely to undergo CPR at death while DNR, and there was evidence (did not reach level of significance) of being less likely to have CPR not provided when FC (p=0.05). Current research demonstrates that Black and Hispanic patients are less likely to have a documented advance directive before admission and prefer more aggressive end-of-life care, even after controlling for socioeconomic status.30–32 End-of-life discussions in terminal cancer patients with physicians are associated with concordant care; however, this may not be true for all patients.13 Black patients who have an end-of-life discussion resulting in a DNR code status were just as likely to undergo ICU care, CPR, and mechanical ventilation in the last week of life as those without a DNR code status.13 The mere presence of an end-of-life conversation does not guarantee consistent content, timing, or continuity of such conversations across all patients.13,32 Mack et al. observed that end-of-life discussions occurred at similar rates for Black and White patients, but Black patients had lower awareness of their terminal illness, which may explain racial differences in care delivered.13 We hypothesize that a concerted effort to improve communication in all patients, with particular emphasis placed on minority patients and their families, may improve adherence to stated preferences.30 Importantly, a broad strokes approach will inappropriately project cultural assumptions that may not be accurate for each individual.33 As Betancourt describes, we must focus on clear communication, exploring hesitations, and addressing concerns; all of which require cultural humility.33 We recommend that all critical care team members receive communication intervention training regarding goals of care conversations.11,34,35
Another consideration surrounding racial disparities, espeically in the ICU, is the potential involvement of racism. The multi-level construct of racism limits the ability to draw a causal line between racism and our disparate findings in Black patients. Instituational racism exists in the ICU through subtle policies. For example, despite no evidence to support restricing family visiting hours,36 restrictions exist and disproportionately effect minority patients and their families.37 Our study was not designed to determine whether racism (on any level) contributed to our findings; however, the existance of disparate outcomes that we find here supports the continued efforts to identify and elimate discrimination in our health system.38
We observed significant variation in discordant CPR based on hospital size and teaching status. Compared to large-teaching hospitals, small-teaching and non-teaching hospitals were more likely associated with discordant CPR in DNR patients. A recent study found that non-teaching hospitals were more likely to have nurses and pharmacists lead resuscitations.39 Non-physician led resuscitation teams are an example of the complex environment that is encountered while caring for the critically ill, and highlights the importance of communication across professional roles, particularly code status.40 A study of interdisciplinary morbidity and mortality rounds found that 67% of adverse events could be attributed to issues with communication.41 The Department of Defense and Agency for Healthcare Research and Quality (AHRQ) developed a toolkit (TeamSTEPPS™) to optimize healthcare team performance.42 The APACHE database does not include information about the time of day that the deaths occurred, and as a result in our study, we were unable to draw associations related to issues with communication at shift changes.4 TeamSTEPPS™ suggests using the “I-PASS the BATON” tool for hand-offs during shift change, which includes stating the code status.43 Ultimately, clearly conveying end-of-life wishes across the care team encourages concordant care in the setting of a cardiac arrest.
In our study, rates for discordant CPR in full code patients ranged from 0–36% per hospital and rates for discordant administering of CPR ranged from 0–5% per hospital. In previous studies, compared to teaching hospitals (after adjusting for hospital size), non-teaching hospitals were less likely to have a CPR committee and were more likely to report the lack of clinical champion as an obstacle to quality improvement.39 We agree with the author’s recommendation that every hospital have a CPR committee that reviews resuscitations, and additionally suggest that quality improvement matrices measure concordance with the patient and family’s stated goals.39 Upon patient death, we recommend that the mortality be reviewed, and the presence or absence of CPR evaluated through the lens of promoting justice and patient dignity.44
There are many reasons why a code status may be changed acutely in real-time, including: “contemporaneous clinical assessment, not the envisaged circumstances and temporary suspension”.45 These motivators for circumstantial shifts in code status may explain some of the differences in CPR concordance in our study based on primary admission diagnosis. Neurologic and trauma FC patients were less likely to receive CPR relative to patients with a primary cardiovascular diagnosis on admission. A patient with a documented “do-not-resuscitate” code status may transition to FC if a trauma brings about an unanticipated need for intervention. Temporary suspension of code status can occur for a procedure, where the cause and treatment of cardiopulmonary arrest have improved survival rates over in-hospital cardiac arrest.46 The American Society of Anesthesiologists do not recommend automatic suspension of DNR for procedures given the ethical principle of patient self-determination.47
Furthermore, a cardiopulmonary arrest may occur from a rapidly reversible cause. In these instances, the patient’s refusal of resuscitation was not determined with this in mind, and limited resuscitative efforts may be initiated until the underlying cause has been treated.45 Similarly, our reference group for primary admission diagnosis was cardiovascular patients, who can develop rapidly reversible arrhythmias. DNR patients with a primary gastrointestinal diagnosis were significantly less likely to receive CPR in our study: this may be related to the differential outcomes in survival from a cardiac arrest based on etiology.
Without the ability to anticipate, inform, and get consent; conflict can occur, especially when human error plays a role. Specifically, in the setting of iatrogenic arrests, 29% of physicians reported that DNR orders do not apply, and 69% felt a greater obligation to resuscitate when arrest resulted from a physician error.48 Caution should be taken when disregarding code statuses in these “non-envisaged circumstances” to ensure that the patient’s right to self-determination is upheld.
Contemporaneous clinical assessment refers to the challenge of balancing the patient- and surrogate-stated or assumed preferences with physician judgement in a rapidly evolving clinical situation.45 As previously mentioned, the patient with a FC and a neurologic primary diagnosis was more likely to have CPR not provided in our study. A recent study found that critical care physicians reported that 11% of their patients had received futile care, and 85% of these patients died within 6 months.49 Beyond clinician perceptions, how does this translate into physician’s behaviors? In a survey of U.S. physicians in 2010, 50% endorsed unilateral (physician-determined) DNR code statuses as appropriate for certain patients and 6% reported performing a unilateral DNR in the last year.50,51 In our study, not providing CPR in FC patients was more likely in recent years. The increase may have occurred as court rulings have ruled in favor of physicians not providing CPR in futile situations.52 Why then, are provider’s perceptions of nonbeneficial care not translating into a documented DNR code status? We suggest having frank discussions surrounding prognosis, and the level of associated uncertainty, with patients to promote patient autonomy. Tools such as the validated Good Outcome Following Attempted Resuscitation (GO-FAR) clinical decision rule can be used to aid in predicting survival to hospital discharge without neurologic disability53 Similarly, a focus on functional status is needed given the increasing rates of functional status deterioration after critical illness.25 Additionally, we recommend transparent conversations, with the associated documentation, between all providers about the perceptions of appropriateness of care to promote beneficence and non-maleficence and reduce moral distress.40
There are several limitations to this study. First, our study was a retrospective review of the APACHE database which was not primarily built to address discordant CPR. Resultantly, the nuances of clinical decision-making surrounding discordant CPR were not captured. This limits the causal interpretation of our results and hinders our ability to elucidate reasons behind this discordance. The term “discordant CPR” was chosen so as to not overstate the appropriateness of the event. Second, given the retrospective nature of the study, we acknowledge the possibility of unknown or uncollected confounders. This also limits our ability to identify other modifiable risk-factors. Third, we created our hospital inclusion criteria to capture those that regularly managing critically ill patients and consistently participating in the benchmarking program (Figure 1). Excluding hospitals that do not meet this criteria may have introduced some selection bias, as we hypothesize that these hospitals may have higher rates of discordant CPR. Fourth, our analysis did not include patients who underwent CPR and survived. Code status was only documented at death or discharge which did not permit an assessment of code status between admission and death or discharge. Lastly, we were reliant on the code status that was documented at the time of death; several studies that have interviewed patients and/or their healthcare agents have stated that the documented advanced care planning orders were not consistent with patient’s goals.54–58 While APACHE’s trained abstractors meticulously record the documented code status at death, this data may not capture potential lags in communication, and the subsequent documentation after patient, family, and provider interaction. This precluded our ability to delineate discordant CPR from inaccurate documentation. Nonetheless, we present evidence that either the documentation or the provision of CPR was discordant with stated goals.
Conclusion
This study demonstrated that 1.6% of patients admitted to an ICU received resuscitation discordant with their documented code status at death. Racial disparities and hospital-level differences associated with receiving discordant CPR highlight areas for potential intervention. While causal inferences are unable to be made from this study, the prevalence of these inconsistencies calls for further investigation. Additionally, these results highlight the importance of communication with patients and between providers, and identifies potential quality improvement initiatives within hospitals. Additionally, frank conversations about prognosis may promote the balance of patient autonomy and non-maleficence.
Key Messsage:
At the time of death, 352 (1.6%) ICU patients did or did not receive cardiopulmonary resuscitation in a manner discordant with their documented code status. Race, and institutional factors were associated with discordant resuscitation.
Acknowledgements:
We would like to thank Cerner Corporation and Laura Freeseman-Freeman for the use of APACHE Outcomes data for research purposes.
Funding Source(s):
National Institutes of Health [NHLBI T32HL07741] (NEI)
Appendix 1.
Code Statuses Included in the Do Not Resuscitate Group
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflicts of Interest: The authors declare no competing interests.
References
- 1.Merchant RM, Yang L, Becker LB, et al. Incidence of treated cardiac arrest in hospitalized patients in the United States. Crit Care Med. 2011;39(11):2401–2406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Girotra S, Nallamothu BK, Spertus JA, et al. Trends in survival after in-hospital cardiac arrest. The New England journal of medicine. 2012;367(20):1912–1920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Efendijev I, Nurmi J, Castren M, Skrifvars MB. Incidence and outcome from adult cardiac arrest occurring in the intensive care unit: a systematic review of the literature. Resuscitation. 2014;85(4):472–479. [DOI] [PubMed] [Google Scholar]
- 4.Peberdy MA, Ornato JP, Larkin GL, et al. Survival from in-hospital cardiac arrest during nights and weekends. JAMA. 2008;299(7):785–792. [DOI] [PubMed] [Google Scholar]
- 5.Miller AC, Rosati SF, Suffredini AF, Schrump DS. A systematic review and pooled analysis of CPR-associated cardiovascular and thoracic injuries. Resuscitation. 2014;85(6):724–731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Guidelines 2000 for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Part 2: ethical aspects of CPR and ECC. Circulation. 2000;102(8 Suppl):I12–21. [PubMed] [Google Scholar]
- 7.Mentzelopoulos SD, Slowther AM, Fritz Z, et al. Ethical challenges in resuscitation. Intensive Care Med. 2018;44(6):703–716. [DOI] [PubMed] [Google Scholar]
- 8.Dzeng E, Colaianni A, Roland M, et al. Moral Distress Amongst American Physician Trainees Regarding Futile Treatments at the End of Life: A Qualitative Study. J Gen Intern Med. 2016;31(1):93–99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Elpern EH, Covert B, Kleinpell R. Moral distress of staff nurses in a medical intensive care unit. Am J Crit Care. 2005;14(6):523–530. [PubMed] [Google Scholar]
- 10.Houston S, Casanova MA, Leveille M, et al. The intensity and frequency of moral distress among different healthcare disciplines. J Clin Ethics. 2013;24(2):98–112. [PubMed] [Google Scholar]
- 11.Morrison RS. Advance Directives/Care Planning: Clear, Simple, and Wrong. Journal of Palliative Medicine. 2020. [DOI] [PubMed] [Google Scholar]
- 12.Turley M, Wang S, Meng D, Garrido T, Kanter MH. The Feasibility of Automating Assessment of Concordance Between Advance Care Preferences and Care Received Near the End of Life. Jt Comm J Qual Patient Saf. 2019;45(2):123–130. [DOI] [PubMed] [Google Scholar]
- 13.Mack JW, Weeks JC, Wright AA, Block SD, Prigerson HG. End-of-life discussions, goal attainment, and distress at the end of life: predictors and outcomes of receipt of care consistent with preferences. J Clin Oncol. 2010;28(7):1203–1208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kurella Tamura M, Montez-Rath ME, Hall YN, Katz R, O’Hare AM. Advance Directives and End-of-Life Care among Nursing Home Residents Receiving Maintenance Dialysis. Clin J Am Soc Nephrol. 2017;12(3):435–442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Teno JM, Fisher ES, Hamel MB, Coppola K, Dawson NV. Medical care inconsistent with patients’ treatment goals: association with 1-year Medicare resource use and survival. J Am Geriatr Soc. 2002;50(3):496–500. [DOI] [PubMed] [Google Scholar]
- 16.Heyland DK, Ilan R, Jiang X, You JJ, Dodek P. The prevalence of medical error related to end-of-life communication in Canadian hospitals: results of a multicentre observational study. BMJ Qual Saf. 2016;25(9):671–679. [DOI] [PubMed] [Google Scholar]
- 17.Chang Y, Huang CF, Lin CC. Do-not-resuscitate orders for critically ill patients in intensive care. Nurs Ethics. 2010;17(4):445–455. [DOI] [PubMed] [Google Scholar]
- 18.Wong J, Duane PG, Ingraham NE. A case series of patients who were do not resuscitate but underwent cardiopulmonary resuscitation. Resuscitation. 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Span P The Patients Were Saved. That’s Why the Families Are Suing. The New York Times. April 10th, 2017, 2017. [Google Scholar]
- 20.© Cerner Corporation. APACHE Outcomes. 2019; https://apacheoutcomes.cernerworks.com/criticaloutcomes-home/. Accessed 6/12/2019, 2019.
- 21.Knaus WA, Wagner DP, Draper EA, et al. The APACHE III prognostic system. Risk prediction of hospital mortality for critically ill hospitalized adults. Chest. 1991;100(6):1619–1636. [DOI] [PubMed] [Google Scholar]
- 22.Zimmerman JE, Kramer AA, McNair DS, Malila FM. Acute Physiology and Chronic Health Evaluation (APACHE) IV: hospital mortality assessment for today’s critically ill patients. Crit Care Med. 2006;34(5):1297–1310. [DOI] [PubMed] [Google Scholar]
- 23.Wallace DJ, Angus DC, Barnato AE, Kramer AA, Kahn JM. Nighttime intensivist staffing and mortality among critically ill patients. The New England journal of medicine. 2012;366(22):2093–2101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Iwashyna TJ, Kramer AA, Kahn JM. Intensive care unit occupancy and patient outcomes. Crit Care Med. 2009;37(5):1545–1557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ingraham NE, Vakayil V, Pendleton KM, et al. National Trends and Variation of Functional Status Deterioration in the Medically Critically Ill. Critical Care Medicine. 2020;Online First. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Vakayil V, Ingraham NE, Robbins AJ, et al. Epidemiological trends of surgical admissions to the intensive care unit in the United States. J Trauma Acute Care Surg. 2020;89(2):279–288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Sandroni C, Nolan J, Cavallaro F, Antonelli M. In-hospital cardiac arrest: incidence, prognosis and possible measures to improve survival. Intensive Care Med. 2007;33(2):237–245. [DOI] [PubMed] [Google Scholar]
- 28.Haider AH, Ong’uti S, Efron DT, et al. Association between hospitals caring for a disproportionately high percentage of minority trauma patients and increased mortality: a nationwide analysis of 434 hospitals. Arch Surg. 2012;147(1):63–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Jakobsen JC, Gluud C, Wetterslev J, Winkel P. When and how should multiple imputation be used for handling missing data in randomised clinical trials - a practical guide with flowcharts. BMC Med Res Methodol. 2017;17(1):162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Muni S, Engelberg RA, Treece PD, Dotolo D, Curtis JR. The influence of race/ethnicity and socioeconomic status on end-of-life care in the ICU. Chest. 2011;139(5):1025–1033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Smith AK, Earle CC, McCarthy EP. Racial and ethnic differences in end-of-life care in fee-for-service Medicare beneficiaries with advanced cancer. J Am Geriatr Soc. 2009;57(1):153–158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Brown CE, Engelberg RA, Sharma R, et al. Race/Ethnicity, Socioeconomic Status, and Healthcare Intensity at the End of Life. J Palliat Med. 2018;21(9):1308–1316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Betancourt JR, Green AR, Carrillo JE, Owusu Ananeh-Firempong I. Defining cultural competence: a practical framework for addressing racial/ethnic disparities in health and health care. Public health reports. 2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Bosslet GT, Hart JL, Turnbull AE. The Importance of Showing Our Work: Process Transparency in Dispute Resolution. Ann Am Thorac Soc. 2019;16(6):679–680. [DOI] [PubMed] [Google Scholar]
- 35.Becker C, Lecheler L, Hochstrasser S, et al. Association of Communication Interventions to Discuss Code Status With Patient Decisions for Do-Not-Resuscitate Orders: A Systematic Review and Meta-analysis. JAMA Netw Open. 2019;2(6):e195033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Rosa RG, Tonietto TF, da Silva DB, et al. Effectiveness and Safety of an Extended ICU Visitation Model for Delirium Prevention: A Before and After Study. Crit Care Med. 2017;45(10):1660–1667. [DOI] [PubMed] [Google Scholar]
- 37.Netzer G, Iwashyna TJ. Fair Is Fair: Just Visiting Hours and Reducing Inequities. Ann Am Thorac Soc. 2017;14(12):1744–1746. [DOI] [PubMed] [Google Scholar]
- 38.Wallis C Why racism, not race, is a risk factor for dying of COVID-19. Scientific American June. 2020;12. [Google Scholar]
- 39.Edelson DP, Yuen TC, Mancini ME, et al. Hospital cardiac arrest resuscitation practice in the United States: a nationally representative survey. J Hosp Med. 2014;9(6):353–357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Bruce CR, Miller SM, Zimmerman JL. A qualitative study exploring moral distress in the ICU team: the importance of unit functionality and intrateam dynamics. Crit Care Med. 2015;43(4):823–831. [DOI] [PubMed] [Google Scholar]
- 41.Tignanelli CJ, Embree GGR, Barzin A. House staff-led interdisciplinary morbidity and mortality conference promotes systematic improvement. J Surg Res. 2017;214:124–130. [DOI] [PubMed] [Google Scholar]
- 42.King HB, Battles J, Baker DP, et al. TeamSTEPPS(): Team Strategies and Tools to Enhance Performance and Patient Safety. In: Henriksen K, Battles JB, Keyes MA, Grady ML, eds. Advances in Patient Safety: New Directions and Alternative Approaches (Vol. 3: Performance and Tools). Rockville (MD)2008. [Google Scholar]
- 43.Starmer AJ, O’Toole JK, Rosenbluth G, et al. Development, implementation, and dissemination of the I-PASS handoff curriculum: A multisite educational intervention to improve patient handoffs. Acad Med. 2014;89(6):876–884. [DOI] [PubMed] [Google Scholar]
- 44.Huddleston JM, Diedrich DA, Kinsey GC, Enzler MJ, Manning DM. Learning from every death. J Patient Saf. 2014;10(1):6–12. [DOI] [PubMed] [Google Scholar]
- 45.Campbell R Do not attempt cardiopulmonary resuscitation decisions: joint guidance. J R Coll Physicians Edinb. 2017;47(1):47–51. [DOI] [PubMed] [Google Scholar]
- 46.Burkle CM, Swetz KM, Armstrong MH, Keegan MT. Patient and doctor attitudes and beliefs concerning perioperative do not resuscitate orders: anesthesiologists’ growing compliance with patient autonomy and self determination guidelines. BMC Anesthesiol. 2013;13:2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Anesthesiologists ASo. Ethical Guidelines for the Anesthesia Care of Patients with Do-Not-Resuscitate Orders or Other Directives that Limit Treatment. 2001; https://www.asahq.org/standards-and-guidelines/ethical-guidelines-for-the-anesthesia-care-of-patients-with-do-not-resuscitate-orders-or-other-directives-that-limit-treatment. Accessed 12/19/2019.
- 48.Casarett DJ, Stocking CB, Siegler M. Would physicians override a do-not-resuscitate order when a cardiac arrest is iatrogenic? J Gen Intern Med. 1999;14(1):35–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Huynh TN, Kleerup EC, Wiley JF, et al. The frequency and cost of treatment perceived to be futile in critical care. JAMA Intern Med. 2013;173(20):1887–1894. [DOI] [PubMed] [Google Scholar]
- 50.Putman MS, D’Alessandro A, Curlin FA, Yoon JD. Unilateral Do Not Resuscitate Orders: Physician Attitudes and Practices. Chest. 2017;152(1):224–225. [DOI] [PubMed] [Google Scholar]
- 51.Putman MS, Tak HJ, Curlin FA, Yoon JD. Quality of Life and Recommendations for Further Care. Crit Care Med. 2016;44(11):1996–2002. [DOI] [PubMed] [Google Scholar]
- 52.Downar J, Close E, Sibbald R. Do physicians require consent to withhold CPR that they determine to be nonbeneficial? Cmaj. 2019;191(47):E1289–e1290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Ebell MH, Afonso AM, Geocadin RG, American Heart Association’s Get With the Guidelines-Resuscitation I. Prediction of survival to discharge following cardiopulmonary resuscitation using classification and regression trees. Crit Care Med. 2013;41(12):2688–2697. [DOI] [PubMed] [Google Scholar]
- 54.Weinerman AS, Dhalla IA, Kiss A, Etchells EE, Wu RC, Wong BM. Frequency and clinical relevance of inconsistent code status documentation. J Hosp Med. 2015;10(8):491–496. [DOI] [PubMed] [Google Scholar]
- 55.Sepucha K, Ozanne EM. How to define and measure concordance between patients’ preferences and medical treatments: A systematic review of approaches and recommendations for standardization. Patient Educ Couns. 2010;78(1):12–23. [DOI] [PubMed] [Google Scholar]
- 56.Kirchhoff KT, Hammes BJ, Kehl KA, Briggs LA, Brown RL. Effect of a disease-specific advance care planning intervention on end-of-life care. J Am Geriatr Soc. 2012;60(5):946–950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Cosgriff JA, Pisani M, Bradley EH, O’Leary JR, Fried TR. The association between treatment preferences and trajectories of care at the end-of-life. J Gen Intern Med. 2007;22(11):1566–1571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Mirarchi FL, Juhasz K, Cooney TE, et al. TRIAD XII: Are Patients Aware of and Agree With DNR or POLST Orders in Their Medical Records. J Patient Saf. 2019;15(3):230–237. [DOI] [PMC free article] [PubMed] [Google Scholar]


