Abstract
Introduction
The role of telemedicine is rapidly evolving across medical specialties and orthopaedics. The utility of telemedicine to identify operative candidates and determine surgical plans has yet to be demonstrated. We sought to assess whether surgical plans proposed following telemedicine visits changed after subsequent in-person interaction across orthopaedic subspecialties.
Materials and methods
We identified all elective telemedicine encounters across two academic institutions from March 1, 2020 to July 31, 2020. We identified patients indicated for surgery with a specific surgical plan during the virtual visit. The surgical plans delineated during the telemedicine encounter were then compared to final pre-operative plans documented following subsequent in-person evaluation. Changes in the surgical plan between telemedicine and in-person encounters were defined using a standardised schema. Regression analysis was used to evaluate factors associated with a change in surgical plan between visits across specialties, including the number of virtual examination manoeuvres performed.
Results
We identified 303 instances of a patient being indicated for orthopaedic surgery during a telemedicine encounter. In 11 cases (4%), the plan was changed between telemedicine and subsequent in-person encounter. No plans were changed amongst patients indicated for joint arthroplasty and foot and ankle surgery, whilst 4% of plans were changed amongst sports surgery and upper extremity/shoulder surgery. Surgical plans had the highest rate of change amongst spine surgery patients (8%). There was notable variability in the conduct of virtual examinations across subspecialties.
Conclusion
Our results demonstrate the capability of telemedicine to support development of accurate surgical plans for orthopaedic patients across several subspecialties. Our findings also highlight the substantial variation in the utilisation of physical examination manoeuvres conducted via telemedicine across institutions, subspecialties, and providers.
Description of study type
Level IV, retrospective cohort study.
Keywords: Telemedicine, Telehealth, Surgical planning
Introduction
The role of telemedicine is rapidly evolving in all medical specialties, including orthopaedic surgery. Advanced imaging, technological growth, communication platforms, and the near ubiquitous access to home and mobile communications devices have created a connectivity ecosystem of substantial potential [1, 2]. Nonetheless, reimbursement barriers from payers, lack of integration into electronic medical records platforms, and limited patient acceptance of telehealth have prevented the widespread adoption of these platforms in the United States [3]. The recent pandemic catalysed the growth of telemedicine by driving payer reimbursement and forcing health systems to adopt and integrate telecommunications platforms to serve patients and remain financially viable. The rapid pace of telemedicine adoption has left orthopaedic practices and health systems unsure how to best leverage these technologies, despite availability [3, 4]. In particular, the utility of telemedicine to identify operative orthopaedic surgery candidates and determine surgical plans is an area of active interest.
The primary limitation of telemedicine is the inability to perform a traditional in-person physical examination, which has long been taught to be paramount to the accurate diagnosis and treatment of musculoskeletal pathologies. As such, much of the recent clinical telemedicine literature within orthopaedics has focused on addressing and adapting to this limitation, with innovative virtual alternatives to traditional exams [5–10]. Nonetheless, these virtual exams have yet to be validated and standardised. Rather than focus on creating telemedicine functions to substitute for the in-person evaluation, our group chose to evaluate a different question, which is how telemedicine might affect the ultimate disposition of patients. In other words, if telemedicine interactions produce the same surgical plan and outcome for an orthopaedic patient’s disposition, the nuances and granular components of the interaction may be less important.
With these considerations in mind, our group recently performed a pilot investigation in spine patients at a single institution to determine whether surgical plans proposed following telemedicine visits changed after in-person evaluation [11]. We found that surgical plans for 94% (31/33) of patients did not change; furthermore, in the two patients where surgical plans were modified, the changes were based on further review of previous imaging, rather than additional information gained from in-person examination [11].
In this context, we sought to expand the scope of our initial query to encompass all elective orthopaedic subspecialties across multiple institutions. Specifically, our primary objective was to assess whether surgical plans proposed following telemedicine visits changed after subsequent in-person interaction and to explore these changes across subspecialties. The secondary aim consisted of characterising the extent and types of virtual exams across providers. Based on our prior research [11, 12], our hypothesis was that surgical plans made via telemedicine would rarely change after in-person examination.
Materials and methods
Institutional investigational review board approval was received prior to the start of this research effort. We obtained data from the clinical registry of Mass General Brigham (MGB). MGB is the parent healthcare corporation of the two institutions (Massachusetts General Hospital and Brigham and Women’s Hospital, both in Boston, MA) where this research was performed. Created in 1991, the means through which data are captured and made available through the MGB clinical registry have been described in detail in previous work [13, 14]. In brief, the registry links with billing and electronic health records from MGB subsidiary institutions to capture sociodemographic and encounter data for all inpatient and outpatient events, by international classification of disease and current procedure terminology code. Data from this registry have been previously used to support investigations around orthopaedic healthcare delivery, clinical practice and policy.
We queried the MGB registry by CPT code to identify all new outpatient telemedicine encounters performed within the divisions of Arthroplasty, Sports Medicine, Spine Surgery, Upper Extremity/Shoulder Surgery, and Foot and Ankle Surgery in the Departments of Orthopaedic Surgery at both institutions between March 1, 2020 and July 31, 2020. These dates encompass the time frame during which Massachusetts Department of Public Health and MGB internal regulations restricted in-person evaluations as a result of the coronavirus pandemic.
We reviewed all telemedicine encounters during this time-period and identified those patients who were indicated for a surgery during the virtual visit. Eligible cases had to demonstrate clear and specific surgical plans documented within the encounter, and a subsequent in-person evaluation prior to surgery to be included in this investigation. Those patients who were indicated for surgery but lacked description of a specific plan were excluded from further review.
We abstracted the initial telemedicine encounter, as well as all subsequent telemedicine and in-person clinical visits and obtained patient age, biologic sex, race/ethnicity, indication for visit, orthopaedic subspecialty service, indication for surgery, the extent of the virtual physical examination including number of examination manoeuvres, and pre-operative surgical plans.
Virtual physical examinations were categorised based on the extent of manoeuvres performed and assigned a value ranging from 0 (no exam) to 3 (three or more manoeuvres performed). Manoeuvers consisted of measures that could be performed using videoconferencing technology; inspection of the area of interest, gait analysis, active range of motion, palpation, strength testing, sensation testing, perfusion, and special tests (e.g. Spurling’s manoeuvre and Durkin’s manoeuvre). Consultations using telephone-only technology were recorded as 0, as providers were unable to directly witness or assist with performance of the manoeuvres.
The surgical plans delineated during the telemedicine encounter were compared to final pre-operative plans as documented following the in-person encounters. We previously developed a rubric for defining changes in the surgical plan between telemedicine and in-person encounters during a pilot study that relied on data from a single service at one hospital. Using this scheme, we defined changes in surgical plans as having occurred when one of three scenarios was met: (1) a patient indicated for surgery via telemedicine was not found to warrant surgery after in-person evaluation; (2) the procedure described during the telemedicine encounter was changed, or additional procedures added, following in-person evaluation (e.g. unicompartmental knee arthroplasty indicated during telemedicine and changed to total knee arthroplasty after in-person evaluation; decompression laminectomy indicated during telemedicine changed to decompression and fusion following in-person evaluation); or (3) additional procedures were added after in-person evaluation, to the surgical procedure described at the time of the telemedicine visit, such that a new consent form would have been required (e.g. single level spinal fusion changed to a multilevel fusion; knee arthroscopy with partial meniscectomy changed to knee arthroscopy with meniscus repair). Initial chart abstractions were performed by a single author (AMC) and cases where the surgical plan was felt to have changed were reviewed by all the authors, with disagreements resolved through peer discussion and consensus.
We defined the primary outcome as a change in the surgical plan with orthopaedic subspecialty defined as the primary predictor. All other variables abstracted were considered co-variates for the purposes of this analysis. Baseline differences amongst demographic and clinical characteristics between groups were evaluated using chi-square testing and assessment of 95% confidence intervals (CI), based on the event rate and sample size. Results are presented using the proportion of change in the surgical plan and 95% CI. A p value < 0.05 was defined a priori as denoting statistical significance. Statistical testing was performed using STATA v15.0 (STATA Corp., College Station, TX).
Results
Review of all new patient telehealth visits from March 1, 2020 to July 31 yielded 3408 virtual visits. Overall, 303 out of 3408 virtual encounters (8.89%) led to patients being indicated for surgery with specific pre-operative plans documented in the chart. Demographic characteristics did not differ with respect to age, gender, or BMI (Table 1).
Table 1.
Demographics by surgical plan status
| Surgical plan status | p value | ||||||
|---|---|---|---|---|---|---|---|
| No change (n = 292) | Change (n = 11) | Total | |||||
| Freq or mean | % or SD | Freq or mean | % or SD | Freq or mean | % or SD | ||
| Age | 54.1 | 17.3 | 51.6 | 23.0 | 54.0 | 17.5 | 0.64 |
| BMI | 28.0 | 5.7 | 27.6 | 5.8 | 28.0 | 5.2 | 0.80 |
| Gender | |||||||
| Female (n = 137) | 134 | 45.9 | 3 | 27.3 | 137 | 45.2 | – |
| Male (n = 166) | 158 | 54.1 | 8 | 72.7 | 166 | 54.8 | 0.24 |
| Total (n = 303) | 292 | 100.0 | 11 | 100.0 | 303 | 100.0 | |
| Smoking status | |||||||
| Never smoker (n = 153) | 148 | 50.9 | 5 | 45.5 | 153 | 50.7 | Ref |
| Current smoker (n = 44) | 44 | 15.1 | 0 | 0.0 | 44 | 14.6 | –† |
| Former smoker (n = 105) | 99 | 34.0 | 6 | 54.5 | 105 | 34.8 | 0.35 |
| Total (n = 302) | 291 | 100.0 | 11 | 100.0 | 302 | 100.0 | |
| ASA class | |||||||
| Class I (n = 52) | 47 | 16.2 | 5 | 45.5 | 52 | 17.3 | Ref |
| Class II (n = 166) | 164 | 56.6 | 2 | 18.2 | 166 | 55.1 | 0.01 |
| Class III (n = 83) | 79 | 27.2 | 4 | 36.4 | 83 | 27.6 | 0.29 |
| Total (n = 301) | 290 | 100.0 | 11 | 100.0 | 301 | 100.0 | |
| Number of exam manoeuvres | |||||||
| None (n = 131) | 124 | 42.5 | 7 | 63.6 | 131 | 43.2 | Ref |
| One (n = 39) | 39 | 13.4 | 0 | 0.0 | 39 | 12.9 | –† |
| Two (n = 30) | 27 | 9.2 | 3 | 27.3 | 30 | 9.9 | 0.35 |
| Three or more (n = 103) | 102 | 34.9 | 1 | 9.1 | 103 | 34.0 | 0.10 |
| Total (n = 303) | 292 | 100.0 | 11 | 100.0 | 303 | 100.0 | |
| Sub-specialty | |||||||
| Arthroplasty (n = 77) | 77 | 26.4 | 0 | 0.0 | 77 | 25.4 | Ref |
| Foot and ankle (n = 11) | 11 | 3.8 | 0 | 0.0 | 11 | 3.6 | –† |
| Spine (n = 59) | 54 | 18.5 | 5 | 45.5 | 59 | 19.5 | 0.28 |
| Sports (n = 80) | 77 | 26.4 | 3 | 27.3 | 80 | 26.4 | 0.95 |
| Upper extremity (n = 76) | 73 | 25.0 | 3 | 27.3 | 76 | 25.1 | –* |
| Total (n = 303) | 292 | 100.0 | 11 | 100.0 | 303 | 100.0 | |
Ref baseline reference for logistic regression
*Subgroup omitted due to multicollinearity
†No comparison group (one group equals 0)
Analysis of whether telemedicine pre-operative plans changed following in-person evaluation demonstrated no change in plans for 96% (292 of 303) of patients (proportion of change: 0.04, 95% CI 0.02–0.06). By subspecialty, plans remained the same for 77/77 patients (100%) in hip and knee arthroplasty, 77/80 patients (96%) in sports surgery (proportion of change: 0.04, 95% CI 0.01–0.11), 73/76 patients (96%) in upper extremity/shoulder surgery (proportion of change: 0.04, 95% CI 0.01–0.11), 54/59 patients (92%) in spine surgery (proportion of change: 0.08, 95% CI 0.03–0.19), and 11/11 patients (100%) in foot and ankle surgery. In an effort to understand the impetus for changes in surgical plans, the respective surgeons were queried, and we provide a summary of clinical rationales for alterations in surgical plans (Table 2).
Table 2.
Surgical plan change
| Specialty | Virtual visit plan | Change after in-person visit | Reason for change |
|---|---|---|---|
| Sports | ACL reconstruction w/autograft | ACL reconstruction w/allograft | Patient preference |
| Sports | TTO with medialization and distalization, MPFL reconstruction, trochleoplasty | No distalization needed | Physical examination revealed patella alta was not as significant as expected |
| Sports | Knee arthroscopy | Knee arthroscopy, loose body removal, MACI biopsy | Additional components added to surgical plan |
| UE/shoulder | Ulnar collateral ligament reconstruction | Ulnar collateral ligament reconstruction with hamstring autograft, ulnar nerve transposition | Physical examination revealed poor palmaris autograft potential and subluxating ulnar nerve |
| UE/shoulder | Revision rotator cuff repair | Added consideration for lower trapezius tendon transfer based on intraoperative findings | Physical exam revealed significant external rotation weakness |
| UE/shoulder | Rotator cuff repair | Added subacromial decompression and subpectoral biceps tenodesis | Physical examination revealed biceps tenderness |
| Spine | L3–L5 laminectomy and non-instrumented fusion | Extended to include L2–L3 | Re-review of prior MRI |
| Spine | C4–C5 ACDF | Extended to include C3–C4 | New C spine radiographs revealed more prominent degenerative findings |
| Spine | L5–S1 foraminotomy vs TLIF | Committed to TLIF | Patient preference after in-person visit |
| Spine | C2 laminectomy, C2-T2 fusion | Extended laminectomy to include C3–C6 | Additional specific decompression levels added to surgical plan |
| Spine | Sacral laminectomy, radiation, 2-stage en bloc spondylectomy | Abandoned initial sacral laminectomy, converted to neoadjuvant XRT prior to 2-stage en bloc spondylectomy | Lack of clarity in virtual visit |
Breakdown of cases with change to surgical plan for patients initially scheduled for surgery after virtual visit only. Attending surgeon reported justification for change in surgical plan located in right-most column
UE upper extremity, ACL anterior cruciate ligament, TTO tibial tubercle osteotomy, MPFL medial patellofemoral ligament, MACI matrix-induced autologous chondrocyte implantation, ACDF anterior cervical discectomy and fusion, TLIF transforaminal lumbar interbody fusion, PSIF posterior spinal instrumented fusion, XRT external-beam radiation therapy
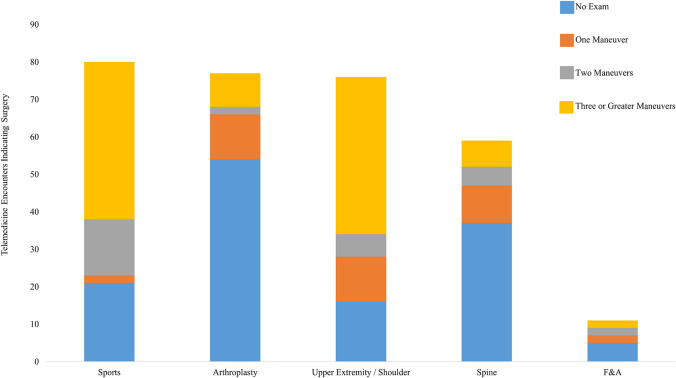
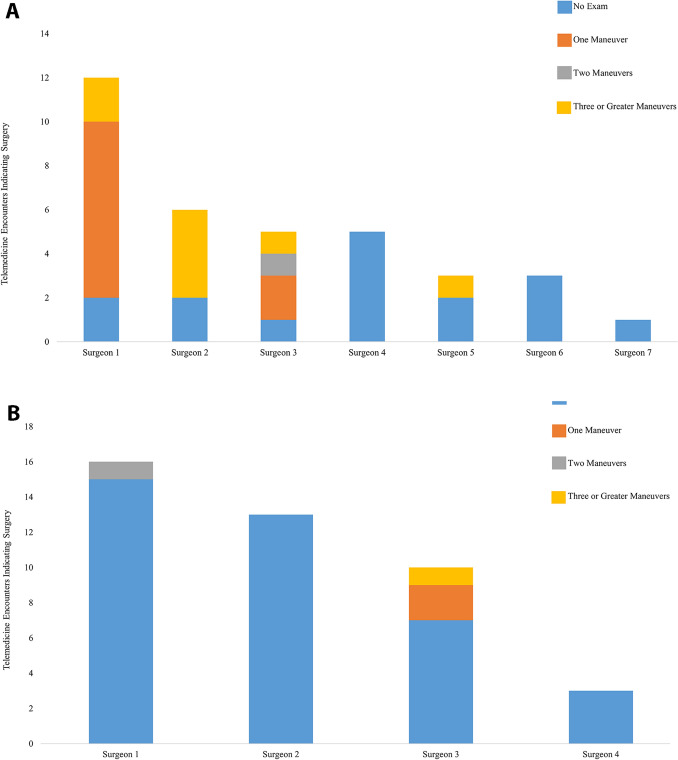
Review of virtual physical examination manoeuvres demonstrated notable variability across MGB subspecialties (Fig. 1), with upper extremity and sports surgery utilising more examination manoeuvres than others. Furthermore, there was substantial variability across institutions and individual surgeons (Fig. 2a and b).
Fig. 1.
Variability in the number of physical exam manoeuvres performed across both institutions as sorted by subspecialty. Included encounters are those virtual encounters in which a patient was indicated for surgery
Fig. 2.
Variability in the number of physical exam manoeuvres performed by each individual surgeon within the Arthroplasty department of both included institutions. Included encounters are those virtual encounters in which a patient was indicated for surgery. a Refers to the Arthroplasty Department at Brigham and Women’s Hospital. b Refers to the Arthroplasty Department and Massachusetts General Hospital
Discussion
The role of telemedicine in the evaluation and treatment of musculoskeletal patients, as it is in all medical specialties, is rapidly evolving. The value it affords with regard to access to care, patient convenience, cost-savings, and efficiency is tempered by notable clinical and logistical drawbacks, including inability to perform a physical exam, need for and understanding of technology, and concerns with patient privacy and medicolegal exposure. The coronavirus pandemic prompted widespread adoption of this previously underutilised system, at a pace beyond the capacity of health systems to fully understand the optimal role of these platforms [4, 15, 16]. External forces limiting in-person evaluations forced orthopaedic providers to carve out a novel role for telemedicine in the pre-operative assessment of patients, and challenged the perceptions of many patients, providers, and healthcare systems. Specifically, much of the literature thus far has focused on the use and validity of various virtual physical exam manoeuvres [5–10]. However, given the significant breakthroughs in advanced imaging, technology, and communications systems, it is not clear that the physical exam itself is as important as it once was for most orthopaedic diagnoses.
This study demonstrates that surgical plans generated for orthopaedic patients across all the elective orthopaedic subspecialties are rarely changed by in-person evaluation. This finding confirms our hypothesis and is consistent with the results of our prior investigations [11, 12]. The aggregated accuracy of surgical plans from telemedicine across all elective orthopaedic subspecialties was 96%, with various subspecialties ranging from 92 to 100%.
There was substantial variability in the utilisation of physical examination manoeuvres conducted via telemedicine between individuals, subspecialties, and institutions. The highest utilisation of physical examination manoeuvres was in the Upper Extremity/Shoulder division, where 80% of virtual visits involved some form of examination and 55% of encounters included virtual exams with three or more manoeuvres performed. The Sports department similarly utilised multiple virtual physical exam manoeuvres (Fig. 1). By contrast, relatively few virtual exam manoeuvres were performed by Arthroplasty surgeons (Fig. 1). This variability may be related to the relative nuance of different diagnoses within subspecialities of Orthopaedics, though it could also represent conformity bias within these subspecialties. Whilst there was substantial heterogeneity in individual provider examination strategies, there also seemed to be institutional trends when comparing practices at different facilities within the same subspecialties. These institutional trends may be reflective of institutional culture or agreement within the division on strategic implementation of telemedicine practices. Nonetheless, regardless of the heterogeneity in physician, division, and institutional practices, the end result similarly produced accurate telemedicine-generated surgical plans. Further, the substantial heterogeneity in virtual physical exam practices, including the lack of any virtual exam for many providers, challenges the long-held belief that the physical examination is paramount to orthopaedic diagnosis and care delivery. With the evolution of advanced imaging and resultant growth of diagnostic capabilities, it is possible that the utility of the physical examination itself may be diminishing over time.
Changes in operative plans after in-person evaluation, though rare, did occur (Table 2). Amongst the 11 patients in whom operative plans changed, only four instances were attributed to findings from in-person physical examination. Except for these four cases, most surgeons did not believe that changes in operative plans were a result of the in-person examination per se. Rather, all other instances of a changed plan were attributed to patient preference, additional imaging, or were simply additional components added to a surgical plan. Such retrospective analysis on the part of the surgeon, however, is prone to recall bias.
Reflecting back on the ultimate goal of leveraging telemedicine to provide a higher level of orthopaedic care to a greater number of patients at a lower cost, we can appreciate the clinical significance of this work. If orthopaedic patients can be assessed via telemedicine platforms and accurately indicated for a specific surgical procedure, then the geographic barriers to care are largely mitigated, and the downstream effects are substantial. Our results indicate that the telemedicine visit alone can identify a surgical plan with relatively high accuracy (96%) when considering all subspecialties. Our use of 95% CI also allows a more conservative assessment of the rate at which this estimate could change in the event of a larger sample. For example, changes in sports surgery and upper extremity surgery plans might occur as frequently as 11%, with the estimate for spine surgery approximating 1 in 5 telemedicine encounters. At the same time, even with these more conservative figures in mind, it would appear that the majority of surgical plans generated via telemedicine visits would remain unchanged following in-person evaluation. From a patient perspective, these findings mean that a patient anywhere across the globe could be accurately indicated for an orthopaedic procedure. In this instance, a patient could then identify a centre particularly suited to their particular procedural need without ever having to leave their home. On the health system side, this could expand institutional reach to broader geographic markets. These findings add to Petersen et al.’s recent systematic review, and reinforce its recommendation for the use of telemedicine in orthopaedic surgery [17].
This investigation carries with it all the typical limitations of a retrospective design, the greatest of which is the inability to decipher nuanced surgical planning rationale, unless it was specifically documented by the orthopaedic surgeon. However, the potential to influence surgeon behaviour, if physicians were prospectively instructed regarding intentions to compare surgical planning accuracy, makes this approach advantageous for our study purposes, especially in light of our standardised scoring rubric. Whilst this study does include multiple institutions, the fact that the institutions are contained within a single health system does limit heterogeneity, both in terms of practice patterns and telecommunication platforms. To the extent that decision-making processes and information needed to develop surgical plans differ from other clinical contexts, our findings may not be generalizable. In this regard, our 95% CIs may provide a better assessment of the range of variation in surgical plan alteration that may occur across subspecialties in the wide community. An additional important factor to note is that this transition to telemedicine utilisation occurred in the context of a pandemic. As such, the types of patients who sought orthopaedic evaluation and the types of diagnoses that were indicated for surgery are likely systematically different from more “typical” patterns. Specifically, patients with milder problems may have been more likely to delay care and providers who identified less urgent diagnoses may have also been more likely to delay intervention. Furthermore, the limited number of instances of changes to surgical plans constrained possible analyses, preventing our group from performing adjusted analyses and attempting to identify factors predictive of changes in surgical plans. These remain viable lines of research we intend to explore going forward. Finally, virtual identification of appropriate surgical candidates is naturally prone to selection bias. We do believe that this bias persists both virtually and in-person, and therefore, is not unique to our research question, though we do not have a comparison group to test this hypothesis against. Given each of these limitations, the outlook of this work should be considered exploratory at this time and our findings should be replicated in larger samples with more clinical diversity before they can be considered actionable.
Despite these limitations, we believe that this investigation is the first, to our knowledge, to demonstrate the capability of telemedicine to generate accurate surgical plans for orthopaedic patients across a broad range of subspecialties. These findings support the sustained use of telemedicine technology going forward and raise the prospect of broader opportunities for telehealth to improve access for patients. Whilst this study has substantial implications for the future implementation of telemedicine, further work remains to be done to determine how to best leverage the synergies between telemedicine and in-person evaluation in orthopaedic patients. For example, one area of distinct importance that is yet to be fully elucidated is patient perception surrounding telemedicine.
Author contributions
All the authors contributed to the study conception and design. Abstraction was performed by AMC. Material preparation, analysis, and manuscript drafting was performed by all the authors. All the authors commented on previous versions of the manuscript. All the authors read and approved the final manuscript.
Funding
The authors did not receive support from any organisation for the submitted work.
Declarations
Conflict of interest
Dr. Schoenfeld reports grants from NIH-NIAMS, grants from the Department of Defense, grants from OREF, personal fees from Commonwealth Fund, personal fees from Wolters Kluwer, and personal fees from Springer. These disclosures are all outside the submitted work. All the other authors have no disclosures.
Ethics approval
Institutional investigational review board approval was provided for this study. This approval is uploaded with our submission.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Keesara S, Jonas A, Schulman K. COVID-19 and health care’s digital revolution. N Engl J Med. 2020;382:e82. doi: 10.1056/NEJMp2005835. [DOI] [PubMed] [Google Scholar]
- 2.Hollander JE, Carr BG. Virtually perfect? Telemedicine for COVID-19. N Engl J Med. 2020;382:1679–1681. doi: 10.1056/NEJMp2003539. [DOI] [PubMed] [Google Scholar]
- 3.Makhni MC, Riew GJ, Sumathipala MG. Telemedicine in orthopaedic surgery: challenges and opportunities. J Bone Jt Surg. 2020 doi: 10.2106/JBJS.20.00452. [DOI] [PubMed] [Google Scholar]
- 4.Hurley ET, Haskel JD, Bloom DA, et al. The use and acceptance of telemedicine in orthopedic surgery during the COVID-19 pandemic. Telemed J E Health. 2020 doi: 10.1089/tmj.2020.0255. [DOI] [PubMed] [Google Scholar]
- 5.Satin A, Lieberman I. The virtual spine examination: telemedicine in the era of COVID-19 and beyond. Glob Spine J. 2020 doi: 10.1177/2192568220947744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Iyer S, Shafi K, Lovecchio F, et al. The spine physical examination using telemedicine: strategies and best practices. Glob Spine J. 2020 doi: 10.1177/2192568220944129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Van Nest DS, Ilyas AM, Rivlin M. Telemedicine evaluation and techniques in hand surgery. J Hand Surg Glob Online. 2020;2:240–245. doi: 10.1016/j.jhsg.2020.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Yoon J, Welch R, Alamin T, et al. Remote virtual spinal evaluation in the era of COVID-19. Int J Spine Surg. 2020;14:7057. doi: 10.14444/7057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Tanaka MJ, Oh LS, Martin SD, Berkson EM. Telemedicine in the era of COVID-19: the virtual orthopaedic examination. J Bone Jt Surg. 2020;102:e57. doi: 10.2106/JBJS.20.00609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Rao SS, Loeb AE, Amin RM, et al. Establishing telemedicine in an academic total joint arthroplasty practice: needs and opportunities highlighted by the COVID-19 pandemic. Arthroplast Today. 2020;6:617–622. doi: 10.1016/j.artd.2020.04.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lightsey HM, Crawford AM, Xiong GX, et al. Surgical plans generated from telemedicine visits are rarely changed after in person evaluation in spine patients. Spine J. 2020 doi: 10.1016/j.spinee.2020.11.009. [DOI] [PubMed] [Google Scholar]
- 12.Crawford AM, Lightsey HM, Xiong GX, Striano BM, Greene N, Schoenfeld AJ, Simpson AK. Interventional procedure plans generated by telemedicine visits in spine patients are rarely changed after in-person evaluation. Reg Anesth Pain Med. 2021 doi: 10.1136/rapm-2021-102630. [DOI] [PubMed] [Google Scholar]
- 13.Schoenfeld AJ, Losina E, Ferrone ML, et al. Ambulatory status after surgical and nonsurgical treatment for spinal metastasis. Cancer. 2019 doi: 10.1002/cncr.32140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Schoenfeld AJ, Tobert DG, Le HV, et al. Utility of adding magnetic resonance imaging to computed tomography alone in the evaluation of cervical spine injury: a propensity-matched analysis. Spine. 2018;43:179–184. doi: 10.1097/BRS.0000000000002285. [DOI] [PubMed] [Google Scholar]
- 15.Wongworawat MD, Capistrant G, Stephenson JM. The opportunity awaits to lead orthopaedic telehealth innovation: AOA critical issues. J Bone Jt Surg. 2017;99:e93. doi: 10.2106/JBJS.16.01095. [DOI] [PubMed] [Google Scholar]
- 16.Parisien RL, Shin M, Constant M, et al. Telehealth utilization in response to the novel coronavirus (COVID-19) pandemic in orthopaedic surgery. J Am Acad Orthop Surg. 2020;28:6. doi: 10.5435/JAAOS-D-20-00339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Petersen W, Karpinski K, Backhaus L, et al. A systematic review about telemedicine in orthopedics. Arch Orthop Trauma Surg. 2021 doi: 10.1007/s00402-021-03788-1. [DOI] [PMC free article] [PubMed] [Google Scholar]