Abstract
Treating to a target of clinical remission or low disease activity is an important principle for managing rheumatoid arthritis (RA). Despite the availability of biologic disease-modifying antirheumatic drugs (bDMARDs), a substantial proportion of patients with RA do not achieve these treatment targets. Upadacitinib is a once-daily, oral Janus kinase (JAK) inhibitor with increased selectivity for JAK1 over JAK2, JAK3, and tyrosine kinase 2. The SELECT phase III upadacitinib clinical program comprised five pivotal trials of approximately 4400 patients with RA, including inadequate responders (IR) to conventional synthetic (cs)DMARDs or bDMARDs. This review aims to provide insights into the benefit–risk profile of upadacitinib in patients with RA. Upadacitinib 15 mg once daily, in combination with csDMARDs or as monotherapy, achieved all primary and ranked secondary endpoints in the five pivotal trials across csDMARD-naïve, csDMARD-IR, and bDMARD-IR populations. Upadacitinib 15 mg also demonstrated significantly higher rates of remission and low disease activity in all five pivotal trials, compared with placebo, methotrexate, or adalimumab. Labeled warnings of JAK inhibitors include serious infections, herpes zoster, malignancies, major cardiovascular events, and venous thromboembolic events. Short- and long-term integrated analyses showed that upadacitinib 15 mg was associated with increased risk of herpes zoster and creatine phosphokinase elevations compared with methotrexate and adalimumab but otherwise had comparable safety with these active comparators. This review suggests that upadacitinib 15 mg had a favorable benefit–risk profile. The safety of upadacitinib will continue to be monitored in long-term extensions and post-marketing studies.
Supplementary Information
The online version contains supplementary material available at 10.1007/s40264-020-01036-w.
Key Points
| Upadacitinib is an oral Janus kinase inhibitor that demonstrates a favorable benefit–risk profile in patients with moderately to severely active rheumatoid arthritis at a dose of 15 mg once daily. |
| Upadacitinib-related benefits include durable efficacy, including achievement of remission and low disease activity, improved physical function, and prevention of structural joint damage. |
| Labeled warnings of upadacitinib include serious infections, herpes zoster, malignancies, major cardiovascular events, and venous thromboembolic events, and upadacitinib was associated with increased rates of herpes zoster and creatine phosphokinase elevations compared with methotrexate and adalimumab based on integrated clinical data. |
Unmet Needs in Rheumatoid Arthritis
Rheumatoid arthritis (RA) is a chronic, systemic inflammatory autoimmune disease that causes significant pain, disability, and progressive joint destruction. Over time, without adequate treatment, irreversible joint destruction and loss of function can lead to significant disability and impaired quality of life (QoL) [1, 2]. The prevalence of RA ranges from 3.1 to 10.7 per 1000 in Europe, the USA, and Japan [3, 4], and up to 60–69% of patients with RA manifest moderately to severely active disease [5].
Conventional synthetic disease-modifying antirheumatic drugs (csDMARDs) such as methotrexate with or without short-term corticosteroids are the first-line treatment for RA [6, 7]. For patients who become inadequate responders (IRs) to csDMARDs or experience csDMARD toxicities [8], treatment with biologic DMARDs (bDMARDs) or targeted synthetic DMARDs (tsDMARDs) in combination with a csDMARD or as monotherapy is recommended [6, 7, 9]. Every patient with RA should be treated to the targets of clinical remission or low disease activity (LDA) [6, 10]. However, approximately half of patients in the real world do not achieve remission or LDA after 12 months of treatment [11].
Use of bDMARDs including inhibitors of tumor necrosis factor (TNF), interleukin-6 receptors, and T/B-cell activity provides significant improvements in efficacy when compared with csDMARDs alone, including greater inhibition of radiographic progression [12, 13]. However, these drugs must be administered subcutaneously or intravenously and are recommended for use with methotrexate to optimize outcomes, in part by reducing the development of antidrug antibodies (i.e., immunogenicity) [14]. Up to 40% of patients treated with a bDMARD do not achieve a 20% improvement in American College of Rheumatology (ACR) criteria (ACR20; primary failure), with most patients also not achieving treatment targets such as clinical remission or LDA. Further, patients who initially respond to therapy may lose response over time (secondary failure) or experience adverse events (AEs) [15]. This suggests that, despite the availability of bDMARDs, there is still an unmet need for effective RA management.
Janus Kinase Inhibitors for the Management of Rheumatoid Arthritis
Inhibition of Janus kinase (JAK) with small-molecule inhibitors (i.e., tsDMARDs) has been shown to be an effective mechanism for the treatment of RA based on data from multiple randomized controlled trials of JAK inhibitors across csDMARD-naïve, csDMARD-IR, and bDMARD-IR patient populations [16–19]. Three JAK inhibitors have received regulatory approval for use in treating RA in the EU, the USA, and other countries worldwide: tofacitinib, baricitinib, and upadacitinib. Filgotinib is approved in the EU for the treatment of RA, but it has not received approval (at the time of writing) from the USA, whose regulatory authorities have requested additional data [19, 20]. Additionally, peficitinib is approved in Japan, South Korea, and Taiwan for the treatment of RA.
It has been hypothesized that JAK inhibitors, by targeting multiple cytokines involved in RA pathogenesis, could provide superior efficacy to bDMARDs that target single pathways [21], and the efficacy of JAK inhibitors versus bDMARDs has been assessed in several head-to-head studies. In ORAL STRATEGY, tofacitinib 5 mg twice daily (BID) + weekly methotrexate was shown to be non-inferior but not superior to adalimumab + methotrexate at month 6 based on 50% improvement in ACR criteria (ACR50) [22]. In RA-BEAM, baricitinib 4 mg once daily + methotrexate was superior to adalimumab 40 mg every other week (EOW) + methotrexate at week 12 based on ACR20 response and improvement in Disease Activity Score of 28 joints with C-reactive protein (DAS28[CRP]) but was not significantly different to adalimumab + methotrexate for more stringent outcomes such as DAS28(CRP) < 2.6 or remission determined by either Clinical Disease Activity Index (CDAI) < 2.8 or EULAR/ACR Boolean criteria [23, 24]. Baricitinib 2 mg once daily (the recommended dose in the USA and in certain populations in the EU and Japan) has not been compared with adalimumab [17]. Upadacitinib 15 mg once daily + methotrexate has demonstrated superiority over adalimumab + methotrexate based on ACR50 and improvement in both pain and physical function, as well as significantly higher DAS28(CRP) < 2.6 response rates and remission rates determined by CDAI < 2.8 and EULAR/ACR Boolean criteria than adalimumab + methotrexate at week 12 [25]. Filgotinib 200 mg once daily + methotrexate demonstrated non-inferiority based on DAS28(CRP) ≤ 3.2 and higher DAS28(CRP) < 2.6 response rates compared with adalimumab + methotrexate at week 12 [19, 26].
Similar to bDMARDs, JAK inhibitors, including tofacitinib 5 mg or 10 mg BID as monotherapy [27], baricitinib 4 mg once daily + methotrexate [17, 28], upadacitinib 15 mg once daily either with methotrexate or as monotherapy [18, 25, 29], and filgotinib 200 mg once daily either with methotrexate or as monotherapy [19, 26, 30, 31], demonstrated significant inhibition of structural progression compared with placebo and/or methotrexate. Unlike the majority of bDMARDs, all of the approved JAK inhibitors are indicated for use either as monotherapy or in combination with methotrexate [16–19]. JAK inhibitors have other potential advantages over bDMARDs, including oral administration, no immunogenicity, and a shorter half-life than bDMARDs.
Long-term safety evaluations are ongoing to assess potential latency events of JAK inhibitors such as malignancies and major adverse cardiovascular events (MACE). Safety signals emerging from phase III studies and limited observational real-world evidence of JAK inhibitors include infections, comprising serious and opportunistic infections and, notably, an increased incidence of herpes zoster [32]. A post-marketing study reported an increased risk of serious infection with fatal outcome associated with tofacitinib 5 mg BID; this has led to label restrictions in EU countries for patients aged > 65 years [16, 33]. Changes in laboratory parameters (e.g., creatine phosphokinase [CPK]) have also been observed in JAK inhibitor studies, and dose reductions are required in patients with moderate or severe renal impairment for tofacitinib, baricitinib, and filgotinib [16, 17, 19, 32]. A potential risk of venous thromboembolic events (VTEs), including pulmonary embolism (PE) and deep vein thrombosis (DVT), has also been identified from phase III clinical trials (baricitinib) and has been observed in the post-marketing setting (tofacitinib) [33, 34].
Upadacitinib
In this benefit–risk report, we focus on upadacitinib, an oral JAK inhibitor with preferential activity toward JAK1 over JAK2, JAK3, and tyrosine kinase 2 [35, 36]. Upadacitinib 15 mg once daily has been approved for the treatment of moderately to severely active RA in adults who are IRs or have an intolerance to methotrexate, either as monotherapy or in combination with methotrexate or other non-bDMARDs, depending on local labeling [18, 37]. A dose of 7.5 mg once daily is also approved in Japan.
Upadacitinib Phase III Clinical Program for Rheumatoid Arthritis
The SELECT phase III clinical development program evaluated the efficacy and safety of upadacitinib with background csDMARDs in both csDMARD-IR and bDMARD-IR patient populations and as a monotherapy in patients who were naïve to methotrexate or methotrexate-IR across five pivotal randomized, multicenter, double-blind, parallel-group, placebo or active comparator-controlled studies (Table 1 in the Electronic Supplementary Material [ESM]). Two additional studies were included in the SELECT program: SELECT-CHOICE, which evaluated the safety and efficacy of upadacitinib versus abatacept in bDMARD-IR patients [38], and SELECT-SUNRISE, which evaluated upadacitinib in Japanese patients [39]. Each phase III study had separate primary endpoints to meet different requirements from the European Medicines Agency (EMA), the US Food and Drug Administration (FDA), and the Japan Pharmaceuticals and Medical Devices Agency (Table 1). Further details of study-specific assessments are outlined in the ESM.
Table 1.
Summary of primary endpoints across pivotal upadacitinib clinical trialsa
| Study | Patient population | Primary endpoint(s) % patients, unless otherwise stated |
||||
|---|---|---|---|---|---|---|
| SELECT-EARLY [29, 76] | MTX-naïve | MTX (n = 314) | UPA 15 mg (n = 317) | |||
| ACR50 at week 12b | 28.3 | 52.1*** | ||||
| DAS28(CRP) < 2.6 at week 24c | 18.5 | 48.3*** | ||||
| ACR20 at week 12d | 54.1 | 75.7‡‡‡ | ||||
| mTSS change from BL at week 24d | 0.7 (n = 264) | 0.1** (n = 279) | ||||
| SELECT-NEXT [48] | csDMARD-IR | PBO + csDMARDs (n = 221) | UPA 15 mg + csDMARDs (n = 221) | |||
| ACR20 at week 12b | 35.7 | 63.8†††† | ||||
| DAS28(CRP) ≤ 3.2 at week 12c | 17.2 | 48.4†††† | ||||
|
SELECT-COMPARE |
MTX-IR |
PBO + MTX (n = 651) |
UPA 15 mg + MTX (n = 651) |
ADA 40 mg + MTX (n = 327) |
||
| ACR20 at week 12b | 36 | 71†††, § | 63 | |||
| DAS28(CRP) < 2.6 at week 12c | 6 | 29†††, §§§ | 18 | |||
| SELECT-MONOTHERAPY [53] | MTX-IR | cMTX (n = 216) | UPA 15 mg (n = 217) | |||
| ACR20 at week 14b | 41.2 | 67.7**** | ||||
| DAS28(CRP) ≤ 3.2 at week 14c | 19.4 | 44.7**** | ||||
| SELECT-BEYOND [49] | bDMARD-IR | PBO + csDMARDs (n = 169) | UPA 15 mg + csDMARDs (n = 164) | |||
| ACR20 at week 12b | 28.4 | 64.6†††† | ||||
| DAS28(CRP) ≤ 3.2 at week 12c | 14.2 | 43.3†††† | ||||
ACR20/50 20/50% improvement in American College of Rheumatology criteria, ADA adalimumab, bDMARD biologic disease-modifying antirheumatic drug, BL baseline, csDMARD conventional synthetic disease-modifying antirheumatic drug, cMTX continued methotrexate, DAS28(CRP) Disease Activity Score of 28 joints with C-reactive protein, EMA European Medicines Agency, IR inadequate responder, mTSS modified Total Sharp Score, MTX methotrexate, NRI non-responder imputation, PBO placebo, UPA upadacitinib
aMissing data were imputed using NRI for binary non-radiographic outcomes and linear extrapolation for radiographic outcomes unless otherwise stated
bPrimary endpoint for the US FDA
cPrimary endpoint for the EU EMA
dPrimary endpoint for the Japan Pharmaceuticals and Medical Devices Agency
Comparisons adjusted for multiplicity: **p ≤ 0.01, ***p ≤ 0.001, ****p ≤ 0.0001 vs. MTX; †††p ≤ 0.001, ††††p ≤ 0.0001 vs. PBO
Comparisons unadjusted for multiplicity: nominal ‡‡‡p ≤ 0.001 vs. MTX; §p ≤ 0.05, §§§p ≤ 0.001 vs. ADA
Efficacy Assessments
Efficacy outcomes assessed across studies included signs and symptoms of RA (ACR response rates and change from baseline in DAS28[CRP]), remission and LDA rates, physical function (Health Assessment Questionnaire-Disability Index [HAQ-DI]) [40, 41], and patient-reported outcomes, including pain and fatigue. Radiographic progression, as assessed by the van der Heijde modified Total Sharp Score (mTSS) [42], was included in two studies: SELECT-EARLY (methotrexate-naïve patients) and SELECT-COMPARE (methotrexate-IR patients).
Safety Assessments
AEs, physical examinations, vital signs, electrocardiograms, and laboratory tests were collected and assessed as previously described [43]. In brief, AEs were identified using the standardized Medical Dictionary for Regulatory Activities (MedDRA) query or company MedDRA query search criteria. Treatment-emergent AEs (TEAEs: AE onset on or after the first dose and ≤ 30 days after the last dose of placebo, methotrexate, or upadacitinib, or ≤ 70 days after the last dose of adalimumab) were summarized. AEs of special interest included AEs with increased prevalence in patients with RA and labeled or emerging risks for immunomodulators and/or other JAK inhibitors. All potential cardiovascular events, including thromboembolic events, were blindly adjudicated by an independent cardiovascular adjudication committee. MACE included cardiovascular death, non-fatal myocardial infarction, and non-fatal stroke. VTEs included DVT and PE.
Methodology
This study reports the benefits and risks of upadacitinib 15 mg once daily (the approved dose for RA in the USA and the EU) as monotherapy and in combination with csDMARDs, compared with placebo, methotrexate, and adalimumab, based on pooled data from five pivotal upadacitinib phase III clinical trials (SELECT-BEYOND, SELECT-COMPARE, SELECT-NEXT, SELECT-MONOTHERAPY, and SELECT-EARLY). Selected benefits and risks of upadacitinib (Sect. 4.1) were assessed up to the time of regulatory submission (Sect. 4.2) and the long-term integrated safety profile of upadacitinib (Sect. 4.3) was reviewed as a supplement to the benefit–risk analysis.
Assessed Benefits and Risks
Efficacy outcomes analyzed to assess the benefits of upadacitinib were ACR20/50/70, achievement of LDA, and remission defined by CDAI ≤ 10 or ≤ 2.8, respectively, DAS28(CRP) < 2.6 or ≤ 3.2, and minimal clinically important difference (MCID) in HAQ-DI (reduction from baseline ≥ 0.22) [40, 41]. These represent either primary endpoints of the upadacitinib phase III studies or secondary endpoints commonly recognized by regulatory authorities (US FDA and/or EMA) to demonstrate efficacy in RA required for drug approval. Radiographic and patient-reported outcomes were also assessed.
Safety outcomes analyzed to assess the risks of upadacitinib were serious infection, herpes zoster, malignancies excluding non-melanoma skin cancer (NMSC), MACE, and VTE. These represent labeled warnings for upadacitinib and other JAK inhibitors that are potentially serious or life threatening and can result in severe outcomes such as hospitalization or death.
Upadacitinib Benefit–Risk Analysis Up to Regulatory Submission
Three integrated analyses of upadacitinib 15 mg once daily versus placebo, methotrexate, and adalimumab 40 mg EOW were conducted based on phase III data up to regulatory submission. The placebo-controlled analysis set (upadacitinib 15 mg vs. placebo, both with background methotrexate/csDMARDs) was based on short-term (week 12/14) data from SELECT-BEYOND, SELECT-NEXT, and SELECT-COMPARE. The methotrexate-controlled monotherapy analysis set compared upadacitinib 15 mg monotherapy with methotrexate monotherapy in methotrexate-naïve and methotrexate-IR patients using week 12/14 efficacy data and week 24/14 safety data from SELECT-EARLY/SELECT-MONOTHERAPY, respectively. A comparison of upadacitinib 15 mg + methotrexate versus adalimumab + methotrexate was conducted using short-term (week 12/14) and long-term (week 48) data from SELECT-COMPARE (adalimumab-controlled upadacitinib 15 mg analysis set).
The differences between the proportion of patients achieving efficacy outcomes and experiencing safety events with the pooled upadacitinib 15 mg versus comparator analysis sets were calculated: (proportion of patients treated with upadacitinib 15 mg reporting outcome) − (proportion of patients treated with comparator group reporting outcome). In the risk analysis comparing upadacitinib 15 mg with adalimumab in methotrexate-IR patients, the differences between the events per 100 patient-years (E/100PY) of AEs were used instead of the incidence of AEs. Ninety-five percent confidence intervals (CIs) were calculated based on Mantel–Haenszel estimation and adjusted for the study as a stratification factor.
Overall, a positive value indicates that a greater proportion of patients treated with upadacitinib reported the outcome of interest. Therefore, when considering benefits, positive values indicate that upadacitinib 15 mg is more favorable than its comparators. However, when considering risks, negative values indicate that upadacitinib 15 mg is more favorable than its comparators.
Long-Term Integrated Safety Analysis of Upadacitinib
An integrated safety assessment with long-term follow-up across the five pivotal SELECT phase III studies has been previously described [43–47]. Here, we reviewed these data up to the cut-off date of June 30, 2019 for pooled upadacitinib 15 mg (five trials; median exposure 101.9 weeks), methotrexate (one trial; median exposure 92.6 weeks), and adalimumab (one trial; median exposure 78.6 weeks). AEs of special interest were reported as exposure-adjusted event rates (EAERs) defined as the total number of E/100PY, including multiple events that occurred in the same patient.
Benefit Assessment
Improvement of Disease Status
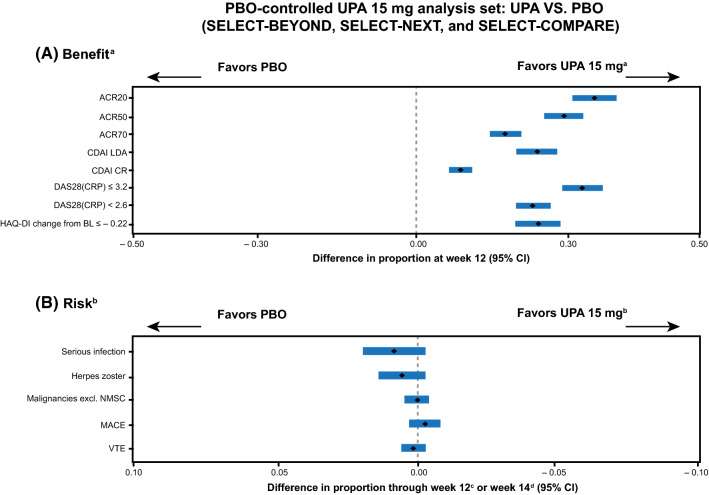
Upadacitinib 15 mg + background csDMARDs/methotrexate in patients who were either csDMARD/methotrexate-IR or bDMARD-IR was superior to placebo at week 12 across composite indices for measures of clinical response and overall disease status (SELECT-NEXT, SELECT-COMPARE, and SELECT-BEYOND) (Fig. 1 and Table 1 [25, 48, 49]). Compared with placebo, significantly higher proportions of patients achieved ACR responses (with the exception of ACR70 at week 12 in SELECT-BEYOND) as well as remission and LDA by all definitions. Responses improved through week 48 and continued through week 60 (SELECT-NEXT and SELECT-BEYOND [50, 51]).
Fig. 1.
Integrated analysis of the a benefits and b risks of upadacitinib 15 mg once daily compared with placebo with background csDMARDs/MTX in csDMARD/MTX-IR and bDMARD-IR patients. aA positive value indicates more favorable efficacy with upadacitinib 15 mg than with placebo. bA negative value indicates more favorable safety with upadacitinib 15 mg than with placebo. cSELECT-BEYOND and SELECT-NEXT. dSELECT-COMPARE. ACR20/50/70 20/50/70% improvement in American College of Rheumatology criteria, bDMARD biologic disease-modifying antirheumatic drug, BL baseline, CDAI Clinical Disease Activity Index, CI confidence interval, CR clinical remission, csDMARD conventional synthetic disease-modifying antirheumatic drug, DAS28(CRP) Disease Activity Score of 28 joints with C-reactive protein, excl. excluding, HAQ-DI Health Assessment Questionnaire-Disability Index, IR inadequate responder, LDA low disease activity, MACE major adverse cardiovascular event, MTX methotrexate, NMSC non-melanoma skin cancer, PBO placebo, UPA upadacitinib, VTE venous thromboembolic event
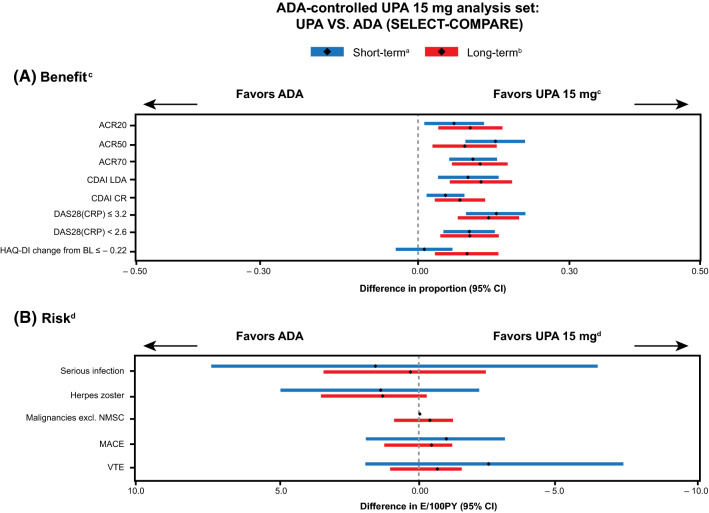
In a direct head-to-head comparison with adalimumab + methotrexate in methotrexate-IR patients (SELECT-COMPARE), upadacitinib + methotrexate demonstrated superior efficacy based on ACR50 at week 12, which was maintained to week 48 [25, 52]. Significantly greater proportions of patients treated with upadacitinib also achieved ACR20/ACR70 responses, DAS28(CRP) < 2.6, CDAI remission, and Boolean remission compared with those treated with adalimumab at week 12, which were also maintained at weeks 24 and 48 [25, 52] (Fig. 2).
Fig. 2.
Integrated analysis of the a benefits and b risks of upadacitinib 15 mg once daily + MTX compared with adalimumab + MTX in MTX-IR patients. aShort term efficacy is measured at week 12 and short term safety is measured through week 14. bLong term efficacy and safety are measured at/through week 48. Long term safety is based on any UPA 15 mg once daily and any adalimumab 40 mg EOW patient populations. cA positive value indicates more favorable efficacy with upadacitinib 15 mg than with adalimumab. dA negative value indicates more favorable safety with upadacitinib 15 mg than with adalimumab. ACR20/50/70 20/50/70% improvement in American College of Rheumatology criteria, ADA adalimumab, BL baseline, CDAI Clinical Disease Activity Index, CI confidence interval, CR clinical remission, DAS28(CRP) Disease Activity Score of 28 joints with C-reactive protein, E/100PY events per 100 patient-years, EOW every other week, excl. excluding, HAQ-DI Health Assessment Questionnaire-Disability Index, IR inadequate responder, LDA low disease activity, MACE major adverse cardiovascular event, MTX methotrexate, NMSC non-melanoma skin cancer, UPA upadacitinib, VTE venous thromboembolic event
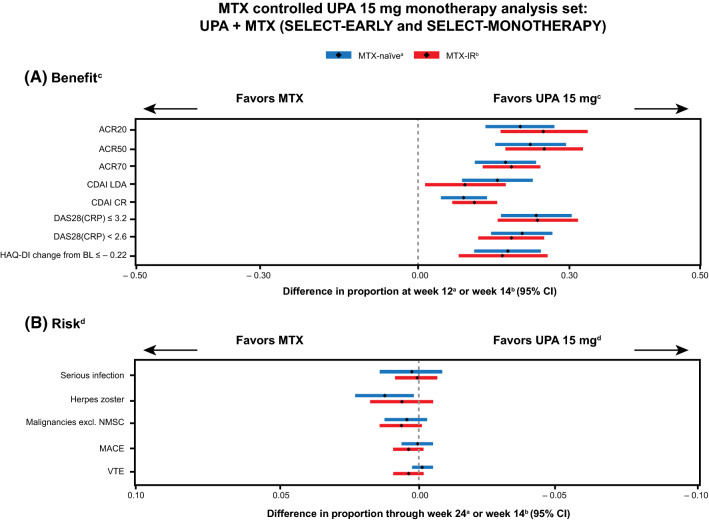
Upadacitinib monotherapy was superior to methotrexate at week 12 or 14, respectively, across multiple measures of clinical response and disease states, in patients who were methotrexate-naïve (SELECT-EARLY) or methotrexate-IR (SELECT-MONOTHERAPY) [29, 53] (Fig. 3, Table 1). This was maintained to week 48 in both studies [54, 55].
Fig. 3.
Integrated analysis of the a benefits and b risks of upadacitinib 15 mg once daily as monotherapy compared with cMTX/MTX in MTX-IR and MTX-naïve patients. aSELECT-EARLY. bSELECT-MONOTHERAPY. cA positive value indicates more favorable efficacy with upadacitinib 15 mg than with MTX. dA negative value indicates more favorable safety with upadacitinib 15 mg than with MTX. ACR20/50/70 20/50/70% improvement in American College of Rheumatology criteria, BL baseline, CDAI Clinical Disease Activity Index, CI confidence interval, cMTX continuing methotrexate, CR clinical remission, DAS28(CRP) Disease Activity Score of 28 joints with C-reactive protein, excl. excluding, HAQ-DI Health Assessment Questionnaire-Disability Index, IR inadequate responder, LDA low disease activity, MACE major adverse cardiovascular event, MTX methotrexate, NMSC non-melanoma skin cancer, UPA upadacitinib, VTE venous thromboembolic event
Of note, upadacitinib as combination therapy or monotherapy demonstrated a rapid onset of action, with statistically significant responses as early as week 2 compared with placebo or methotrexate, respectively.
Inhibition of Progression of Structural Joint Damage
According to EULAR recommendations, treatment decisions should be based on progression of structural damage in addition to disease activity and safety, with the inhibition of structural damage highlighted as an important differentiator of DMARDs from strictly symptomatic antirheumatic agents, such as non-steroidal anti-inflammatory drugs [6].
In the upadacitinib development program, radiographic progression was assessed in both methotrexate-naïve and methotrexate-IR populations (SELECT-EARLY and SELECT-COMPARE). Upadacitinib + methotrexate in methotrexate-IR patients showed a statistically significant reduction in the progression of structural joint damage compared with placebo + methotrexate at week 26, with a significantly greater proportion of patients having no radiographic progression [25]. Inhibition of structural joint damage was maintained through week 48 [52]. Similarly, upadacitinib monotherapy in methotrexate-naïve patients showed a statistically significant reduction in the progression of structural joint damage compared with methotrexate monotherapy, as well as a significantly greater percentage of patients with no radiographic progression at week 24 (Table 1 and van Vollenhoven et al. [29]), with inhibition of progression maintained through week 48 [55].
Improved Function
Upadacitinib + background csDMARDs/methotrexate was superior to placebo at week 12 for both improvement in HAQ-DI and for the percentage of patients achieving MCID in HAQ-DI (reduction from baseline ≥ 0.22) (Fig. 1; Table 2 in the ESM). Upadacitinib + methotrexate demonstrated superior improvement in HAQ-DI compared with adalimumab + methotrexate at week 12, with significant differences from week 8 that were maintained through week 48 [25, 52] (Fig. 2). The percentage of patients receiving upadacitinib + methotrexate who achieved MCID for HAQ-DI in the upadacitinib group was significantly greater than that of those receiving adalimumab + methotrexate at week 48.
Similar to combination therapy with csDMARDs, upadacitinib monotherapy was superior to methotrexate at week 12 or 14 for both improvement in HAQ-DI and for the percentage of patients achieving the MCID (Fig. 3; Table 2 in the ESM). These responses were maintained through week 48.
Additional Patient-Reported Outcomes
Other patient-reported outcomes included morning stiffness duration, health-related QoL (Short Form-36 physical component summary), fatigue (Functional Assessment of Chronic Illness Therapy-Fatigue), and pain. Upadacitinib 15 mg with or without background csDMARDs/methotrexate showed statistically significant improvements across all of these outcome measures in patients who were methotrexate-naïve, csDMARD-IR/methotrexate-IR, or bDMARD-IR (fatigue and pain were not assessed in patients who were bDMARD-IR or csDMARD-IR, respectively) compared with the placebo and active comparator groups (Table 2 in the ESM). Of note, improvement of pain with upadacitinib + methotrexate was superior to adalimumab + methotrexate at week 12 and was maintained to week 48 in SELECT-COMPARE [25, 52].
Risk Assessment
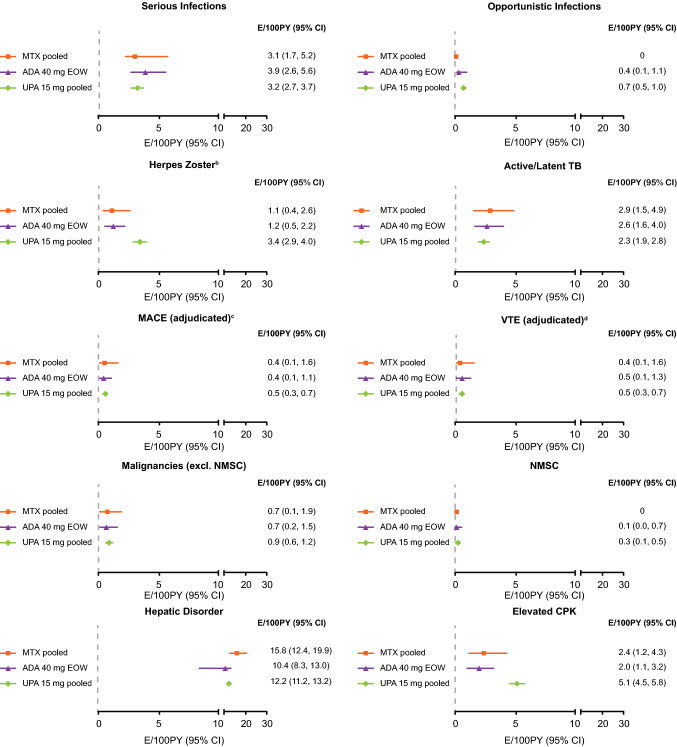
In this review, risks associated with upadacitinib were assessed using short-term integrated risk analyses based on phase III clinical data (week 12 for SELECT-BEYOND, SELECT-NEXT, and SELECT-EARLY; week 14 for SELECT-MONOTHERAPY; and weeks 14/48 for SELECT-COMPARE; Figs. 1, 2 and 3) and a long-term integrated safety analysis (Fig. 4), which included 2629 patients who received at least one dose of upadacitinib 15 mg (4565.8 patient-years (PY); median exposure: 101.9 weeks), 314 patients who received methotrexate (456.0 PY; median exposure: 92.6 weeks), and 579 patients who received adalimumab (768.6 PY; median exposure: 78.6 weeks).
Fig. 4.
Event rates for TEAEs of special interest for upadacitinib 15 mg once daily and active comparators (adapted from Cohen et al. [44])a. MTX pooled: n = 314, PY = 456.0, median exposure = 92.6 weeks; ADA 40 mg EOW: n = 579, PY = 768.6, median exposure = 78.6 weeks; UPA 15 mg pooled: n = 2629, PY = 4565.8, median exposure = 101.9 weeks. aPatients who switched from PBO, ADA, or MTX to UPA were included in the UPA analysis set from the start of UPA, whereas those who switched from UPA to ADA were included in the ADA dataset from the start of ADA. bMost herpes zoster cases were non-serious (95%) and involved a single dermatome (71%). cMACE was defined as CV death, non-fatal MI, and non-fatal stroke. dVTE was defined as DVT and PE. ADA adalimumab, CI confidence interval, CPK creatine phosphokinase, CV cardiovascular, DVT deep vein thrombosis, E/100PY events per 100 patient-years, EOW every other week, excl. excluding, MACE major adverse CV event, MI myocardial infarction, MTX methotrexate, NMSC non-melanoma skin cancer, PE pulmonary embolism, TB tuberculosis, TEAE treatment-emergent adverse event, UPA upadacitinib, VTE venous thromboembolic event
A detailed description of the integrated safety profile of upadacitinib 15 mg from an earlier data cut (2655 PY; median exposure: 53.6 weeks) has been previously reported [43]. Cox regression analyses from this report suggested that upadacitinib 15 mg treatment was associated with an increased risk of herpes zoster and CPK elevations compared with placebo, methotrexate, and adalimumab. A summary of TEAEs and laboratory abnormalities observed with upadacitinib 15 mg and its comparators was also described.
Serious Infections
In the short-term risk analyses, numerically greater proportions of patients treated with upadacitinib 15 mg experienced serious infections compared with placebo in combination with background csDMARDs (Fig. 1), but similar proportions of patients receiving upadacitinib 15 mg and methotrexate monotherapy reported serious infections (Fig. 3). In the SELET-COMPARE study, numerically higher rates of serious infections with upadacitinib 15 mg versus adalimumab were also observed at week 14 but not at week 48 (Fig. 2).
In the long-term integrated analysis, the EAER of serious infection among any patient receiving upadacitinib 15 mg across all five phase III studies was 3.2 E/100PY (95% CI 2.7–3.7 [46]; Fig. 4). This was consistent with that observed in patients treated with adalimumab (3.9 E/100PY [95% CI 2.6–5.6]) and methotrexate (3.1 E/100PY [95% CI 1.7–5.2]). Comparisons of rates or incidence of events across different clinical programs conducted in different patient populations should be interpreted with caution; however, the EAER of serious infection reported with upadacitinib 15 mg was within the range reported for the RA clinical development programs of tofacitinib, tocilizumab, and sarilumab [56–58]. According to Cox regression analyses from an earlier data cut, upadacitinib 15 mg was not associated with higher risk of serious infections compared with adalimumab (hazard ratio 0.8 [95% CI 0.5–1.4]) or methotrexate (hazard ratio 1.6 [95% CI 0.7–3.4]) [43]. The EAER of upadacitinib 15 mg did not increase over time. The types of serious infections reported in patients treated with upadacitinib were generally consistent with those anticipated in patients with RA, with pneumonia being most common. Among patients receiving upadacitinib 15 mg, those who were aged ≥ 75 years and smoked, but not those who were receiving concomitant methotrexate or glucocorticoids, had an increased risk of serious infections [46].
Opportunistic infections in patients treated with upadacitinib 15 mg were reported at a rate of 0.7 E/100PY (95% CI 0.5–1.0) and were comparable with those observed in patients treated with adalimumab (Fig. 4). The majority of opportunistic infections were non-serious oral candidiasis [46]. Rates of latent/active tuberculosis were similar across upadacitinib 15 mg, methotrexate, and adalimumab.
Herpes Zoster
Herpes zoster was more commonly observed with upadacitinib 15 mg than comparators across phase III studies in the short term (Figs. 1, 2 and 3). A total of 142 patients receiving upadacitinib 15 mg with an EAER of 3.4 E/100PY (95% CI 2.9–4.0) experienced herpes zoster across the five pivotal phase III trials with up to 3 years of follow-up [44, 45] (Fig. 4). The rate of herpes zoster was higher in patients treated with upadacitinib than in those receiving placebo, methotrexate, or adalimumab. In patients who received upadacitinib 15 mg, the majority of herpes zoster events involved a single dermatome (71%) and were non-serious (95%). Seven events of disseminated herpes zoster, six events of ophthalmic herpes zoster (periorbital involvement), and six events of post-herpetic neuralgia were reported in patients receiving upadacitinib 15 mg. No patient experienced central nervous system involvement in the 15 mg group.
Using multivariate analysis, prior herpes zoster and age ≥ 65 years were identified as risk factors for the development of herpes zoster while receiving upadacitinib 15 mg, and a higher rate of herpes zoster was seen in the Asian region than in other geographic regions (Table 3 in the ESM), as observed with other JAK inhibitors [59, 60]. Within Asia, the highest rate of herpes zoster was observed in Japan (12.2 E/100PY [95% CI 7.0–19.9]), and the increased risk of herpes zoster in the Japanese versus global populations treated with upadacitinib 15 mg has been previously reported [61, 62]. There was no apparent association between the use of methotrexate and/or concomitant corticosteroids at baseline with the development of herpes zoster [45].
Malignancy
Upadacitinib 15 mg had similar rates of malignancy excluding NMSC compared with placebo, methotrexate, and adalimumab across patient populations in the short-term risk analyses (Figs. 1, 2 and 3). In the long-term analysis, the EAER for malignancy excluding NMSC in the upadacitinib 15 mg group was 0.9 E/100PY (95% CI 0.6–1.2), which was comparable with adalimumab and methotrexate (Fig. 4). A standardized incidence ratio (SIR) analysis for malignancy excluding NMSC, adjusted for age and sex from the Surveillance, Epidemiology, and End Results 18 Registry Data 2000–2015 for the general population, yielded an SIR estimate of 1.05 (95% CI 0.66–1.60) for the upadacitinib 15 mg group in an earlier data cut [43], which suggests that the number of malignancies excluding NMSC in patients exposed to upadacitinib was not significantly higher than expected. As mentioned, comparisons between different clinical trial programs should be interpreted with caution; however, the EAER for malignancy excluding NMSC reported with upadacitinib 15 mg was within the range reported for the RA clinical development programs of tofacitinib, baricitinib, tocilizumab, and sarilumab [56–58, 63].
The types of malignancies observed reflected those expected in patients with moderately to severely active RA [64], and no notable pattern was observed for the types of malignancies reported. Rates of NMSC were similar across upadacitinib 15 mg, methotrexate, and adalimumab.
Major Adverse Cardiovascular Events
In the short-term risk analyses, similar rates of MACE were observed with upadacitinib and placebo, methotrexate, and adalimumab (Figs. 1, 2 and 3). In the long-term integrated analysis, the EAER for MACE in the upadacitinib 15 mg group was 0.5 E/100PY (95% CI 0.3–0.7) [44]. Rates of MACE were comparable between the upadacitinib, adalimumab, and methotrexate groups (Fig. 4). While comparisons between clinical trial programs should be interpreted with caution, the rate for MACE reported with upadacitinib 15 mg was within the range of that reported for the clinical RA development programs of tofacitinib, baricitinib, and sarilumab [56, 58, 63]. The incidence rates for MACE did not increase over time, and there was no pattern in the time to onset for MACE. All patients who experienced MACE during upadacitinib therapy had at least one cardiovascular risk factor.
While reducing chronic inflammation with effective therapies may reduce cardiovascular disease risk in patients with RA [65], JAK inhibitors, including upadacitinib, are also associated with an increase in serum lipid levels. Although treatment with upadacitinib led to increased levels of low-density lipoprotein cholesterol (LDL-C) and high-density lipoprotein cholesterol, their ratio remained constant over time and there was no association between elevated LDL-C and the occurrence of MACE [66].
Venous Thromboembolic Events
Similar rates of VTEs were observed with upadacitinib 15 mg and its comparators in the short-term risk analyses (Figs. 1, 2 and 3) and long-term integrated analysis (Fig. 4). The EAER for VTEs reported with upadacitinib 15 mg was 0.5 E/100PY (95% CI 0.3–0.7), which was comparable with the rates with adalimumab or methotrexate (Fig. 4) and also similar to that observed in the general RA population (~ 0.6 n/100PY) [67]. In total, 21 VTEs were observed in 20 patients receiving upadacitinib 15 mg, of which 11 events were PE only, five events were DVT only, and four events were PE + DVT [47]. There was no pattern in the timing of VTEs in patients receiving upadacitinib 15 mg, and the accumulative probability of VTE in this treatment group over 3 years was ≤ 1%. All patients who experienced a VTE had at least one known risk factor. Subsequent analysis suggested prior VTE, age ≥ 65 years, non-steroidal anti-inflammatory drug or statin use, and—to a lesser extent—higher body mass index (BMI), were risk factors for the development of VTE in patients receiving upadacitinib 15 mg [47]. These factors are known to increase the risk of VTE in the general population [68].
Other Treatment-Emergent Adverse Events of Special Interest
Similar to other JAK inhibitors [16, 17, 19, 32], treatment with upadacitinib has been associated with an increased incidence of CPK elevations compared with placebo, methotrexate, and adalimumab (Fig. 4). Most cases of CPK elevations were asymptomatic, and no cases of rhabdomyolysis were observed with upadacitinib 15 mg. CPK elevations > 5 × the upper limit of normal were transient and did not require treatment discontinuation, with mean CPK levels increasing through 12 weeks of treatment and remaining stable at an increased value thereafter.
Although a higher incidence of hepatic transaminase elevations was observed with upadacitinib 15 mg than with placebo during the short-term placebo-controlled period [18], similar rates of hepatic disorders (most of which were transaminase elevations) were observed across upadacitinib 15 mg, methotrexate, and adalimumab in the long-term integrated analysis (Fig. 4). Most cases of hepatic transaminase elevations with upadacitinib were asymptomatic and transient. If elevated hepatic transaminase levels are observed during routine patient management, and drug-induced liver injury is suspected, interruption of upadacitinib treatment is recommended until this diagnosis is excluded.
Benefit–Risk Evaluation
Summary of Benefits
Upadacitinib 15 mg in combination with background csDMARDs/methotrexate demonstrated superior efficacy based on clinical response and overall disease status, including achievement of LDA or remission and improvement in physical function compared with placebo at week 12 (Fig. 1). Similarly, upadacitinib 15 mg as monotherapy in methotrexate-naïve or methotrexate-IR patients demonstrated superior efficacy across multiple disease outcome measures compared with methotrexate at week 12 (Fig. 3). Treatment with upadacitinib 15 mg was associated with a rapid onset of action with statistically significant responses versus comparators as early as week 2. Upadacitinib demonstrated inhibition of structural joint damage both in combination with methotrexate (in methotrexate-IR patients) and as monotherapy (in methotrexate-naïve patients) [25, 29, 52] (Table 1).
Upadacitinib also demonstrated superiority compared with two established biologic therapies. Upadacitinib had significantly greater efficacy versus adalimumab in methotrexate-IR patients, for all clinical (including remission) and patient-reported outcomes assessed in this analysis [25] (Fig. 2). Similarly, upadacitinib 15 mg demonstrated superior improvement in disease activity and remission compared with abatacept in bDMARD-IR patients [38].
Summary of Risks
In the short-term placebo-controlled period, upadacitinib 15 mg + csDMARDs had an increased incidence of serious infections and herpes zoster compared with placebo (Fig. 1). There was no notable difference in the incidence of MACE, malignancies, or VTEs between upadacitinib and placebo. With the exception of herpes zoster, all safety events reported in the short-term risk analyses occurred at a similar incidence with upadacitinib 15 mg monotherapy versus methotrexate (Fig. 3) or upadacitinib 15 mg + methotrexate versus adalimumab + methotrexate (Fig. 2). No new safety risks were observed in the long-term integrated safety analysis of upadacitinib 15 mg, and—compared with methotrexate or adalimumab—higher EAERs were only observed for herpes zoster and elevated CPK (Fig. 4). While not included in this integrated analysis, the safety profile of upadacitinib reported in SELECT-CHOICE was consistent with that from the five pivotal trials, with no new risks identified [38].
While the rate of VTEs with upadacitinib was similar to that with placebo and adalimumab, concerns around VTEs have been raised for other JAK inhibitors, which have led to cautionary use in certain patient populations [16]. In addition to pre-existing RA, all upadacitinib-treated patients who experienced VTEs had at least one known risk factor: prior VTE, age ≥ 65 years, non-steroidal anti-inflammatory drug or statin use, and high BMI [47]. Major surgery and prolonged immobilization are also listed as risk factors for VTE in the upadacitinib label [18]. Therefore, it is recommended that the risks and benefits be considered prior to initiating treatment with upadacitinib in patients who have known risk factors for VTE [18].
Summary of Benefit–Risk Assessment
Upadacitinib 15 mg, as monotherapy or in combination with csDMARDs/methotrexate, met all primary and ranked secondary efficacy endpoints and achieved significantly higher remission and LDA rates than placebo, methotrexate, and adalimumab across all five pivotal phase III trials in the SELECT clinical program [25, 29, 48, 49, 54].
Consistent with a previous integrated safety analysis [47], upadacitinib 15 mg was associated with higher rates of herpes zoster and CPK elevations but otherwise had a safety profile similar to that of methotrexate and adalimumab based on short- and long-term analyses. Risks observed with upadacitinib 15 mg were similar to those reported for other JAK inhibitors (tofacitinib and baricitinib) and other RA treatments (tocilizumab and sarilumab). No new safety risks were found with upadacitinib 15 mg compared with other JAK inhibitors.
An increased risk for herpes zoster was observed with upadacitinib 15 mg in this analysis. However, the numbers needed to treat (based on achieving CDAI remission) and the numbers needed to harm (based on an event of herpes zoster) compared with adalimumab over 26 weeks’ treatment in SELECT-COMPARE were 11 and 216, respectively. This suggests that, for every additional case of herpes zoster reported with upadacitinib over that reported with adalimumab, approximately 20 additional patients would achieve CDAI remission. The risk of herpes zoster is consistent with that observed with other JAK inhibitors, is familiar to healthcare professionals who treat patients with RA, and is considered manageable with standard clinical practice. However, the increased risk of herpes zoster observed in patients from Asia (particularly those in Japan), patients aged ≥65 years, and/or those with prior herpes zoster [45] should be considered by rheumatologists and discussed with patients prior to prescribing upadacitinib.
Increased rates of CPK elevations were also reported with upadacitinib compared with active comparators. CPK elevations reported with upadacitinib were mostly asymptomatic and transient and did not require treatment discontinuation. These elevations may be due to the restoration of myoblast differentiation mediated by JAK inhibition [69], and the current consensus is that CPK testing is not required in patients receiving JAK inhibitors, including upadacitinib [70].
None of the covariates assessed (body weight, sex, race, ethnicity, age, renal/hepatic impairment) in the population pharmacokinetic analysis based on phase I–III clinical trials had a clinically relevant effect on upadacitinib exposure [71, 72]. Therefore, the pharmacokinetics of upadacitinib are not expected to have a clinically meaningful effect on the efficacy or safety of upadacitinib. No dose adjustment is required in patients with mild or moderate renal or hepatic impairment [18].
The safety and efficacy of upadacitinib 15 mg was generally consistent with that of regional subpopulations, including Central and Eastern European patients in a subgroup analysis of SELECT-COMPARE [73], Japanese patients in the SELECT-SUNRISE study [39], and a subgroup analysis of SELECT-EARLY [74]; and in Chinese, Brazilian, and South Korean patients in an independent phase III study [75]. The only notable difference was a higher incidence of herpes zoster in Japanese versus global patients [39, 74].
Overall, these data suggest that upadacitinib 15 mg has a favorable benefit–risk profile for the treatment of RA. However, rheumatologists should ensure any potential risks are communicated prior to prescribing upadacitinib to patients, especially those who have relevant risk factors. As with all RA treatments, patients should also be monitored by a specialist while receiving upadacitinib.
Uncertainties Related to Benefits and Risks
Although the upadacitinib clinical development program was robust, uncertainties remain regarding the characterization of risks of upadacitinib and its use in certain populations who were under-represented in clinical trials. For example, clinical trials exclude patients with significant underlying conditions in whom safety risks may be different. Uncertainties also exist for risks requiring long-term observation to understand whether there is an association with upadacitinib use. Due to clinical trial exclusion criteria, there is limited exposure of upadacitinib in patients with severe renal or hepatic impairment and in patients aged ≥ 75 years, and upadacitinib has not yet been evaluated in children and will not be indicated for use in pediatric patients aged < 18 years at this time. However, these are generic limitations associated with phase III clinical data, which may be rectified when long-term post-marketing data become available.
Planned/Ongoing Pharmacovigilance Activities
Long-term observation of the safety and efficacy of upadacitinib will continue through ongoing long-term extensions for clinical trials and planned pharmacoepidemiologic studies. These include long-term database studies (in the USA and the EU), which will provide evidence in support of the safety profile of upadacitinib in real-world populations, especially those that were under-represented during clinical trials. Upadacitinib studies in children with juvenile idiopathic arthritis are also planned.
Conclusions
Upadacitinib is an oral, once-daily selective JAK inhibitor that has been evaluated in a phase III clinical development program. With over 2600 patients and 4500 PY of exposure, upadacitinib 15 mg demonstrated a favorable benefit–risk profile, both in combination with csDMARDs/methotrexate or as a monotherapy across a range of patients with moderately to severely active RA, including those who were naïve to methotrexate, and those who were IRs or had intolerance to csDMARDs or bDMARDs. Upadacitinib fills an unmet medical need for patients with RA, providing significantly greater rates of disease outcomes (remission and LDA) compared with established therapies (methotrexate, adalimumab, and abatacept), and inhibits structural joint damage. While labeled risks of upadacitinib include serious infection, herpes zoster, malignancies excluding NMSC, MACE, and VTE, with the exception of herpes zoster and CPK elevations, the safety profile of upadacitinib was similar to that observed with adalimumab.
Supplementary Information
Below is the link to the electronic supplementary material.
Acknowledgements
AbbVie and the authors thank the patients, study sites, and investigators who participated in the clinical trials. Philip G. Conaghan is supported in part by the UK National Institute for Health Research (NIHR) Leeds Biomedical Research Centre. The views expressed are those of the authors and not necessarily those of the UK national health service, the NIHR, or the Department of Health. Medical writing assistance was provided by Siddharth Mukherjee, PhD, CMPP™, of AbbVie and Frances Smith, PhD, of 2 the Nth (Cheshire, UK), and was funded by AbbVie.
Declarations
Funding
AbbVie Inc. funded this study and participated in the study design, research, analysis, data collection, interpretation of data, review, and approval of the publication. All authors had access to relevant data and participated in the drafting, review, and approval of this publication. No honoraria or payments were made for authorship.
Conflicts of interest
Philip G. Conaghan has received consultancy or speakers’ bureau fees from AbbVie, AstraZeneca, Bristol-Myers Squibb, Eli Lilly, Flexion Therapeutics, Galapagos, Gilead, Janssen, Novartis, and Pfizer. Eduardo Mysler has received research grants and/or consulting fees from AbbVie, Amgen, AstraZeneca, Bristol-Myers Squibb, Eli Lilly, GlaxoSmithKline, Janssen, Pfizer, Roche, and Sandoz. Yoshiya Tanaka has received speaking fees and/or honoraria from AbbVie GK, Astellas Pharma Inc., Bristol-Myers Squibb, Chugai Pharmaceutical, Daiichi Sankyo, Eisai, Eli Lilly Japan KK, Janssen Pharmaceutical KK, Mitsubishi-Tanabe Pharma, Novartis, Pfizer Japan Inc., Takeda, Teijin, and YL Biologics and research grants from Asahi-Kasei Pharma, Bristol-Myers Squibb, Chugai Pharmaceutical, Daiichi Sankyo, Eisai, Mitsubishi-Tanabe Pharma, Ono Pharmaceutical, Sanofi KK, Takeda, and UCB Japan. Barbara Da Silva-Tillmann, Tim Shaw, John Liu, Ryan Ferguson, and Jeffrey V. Enejosa are employees of AbbVie and may own AbbVie stock or options. Stanley Cohen has received grant money/research support from, and has acted as consultant to, Amgen, AbbVie, Boehringer Ingelheim, Pfizer, and Sandoz. Peter Nash has received funding for clinical trials, research grants, and honoraria for lectures and advice from AbbVie, Boehringer Ingelheim, Bristol-Myers Squibb, Celgene, Eli Lilly, Gilead, Janssen, Novartis, Pfizer, Roche, Sandoz, Sanofi-Aventis, and UCB. William Rigby has received grant/research support from, and has acted as a consultant for, AbbVie, Bristol-Myers Squibb, Eli Lilly, Pfizer, Roche, and Sun Pharma. Gerd Burmester has acted as consultant and participated in speakers’ bureaus for AbbVie, Eli Lilly, Gilead, and Pfizer.
Ethics approval
Studies were conducted in compliance with the Declaration of Helsinki, International Conference on Harmonisation of Technical Regulations for Pharmaceuticals for Human Use guidelines, and applicable local country regulations. All study-related documents were approved by independent ethics committees and institutional review boards.
Consent to participate
All patients provided written informed consent to participate in the trials.
Consent for publication
Not applicable.
Availability of data and material
AbbVie is committed to responsible data sharing regarding the clinical trials we sponsor. This includes access to anonymized, individual, and trial-level data (analysis data sets), as well as other information (e.g., protocols and clinical study reports), provided the trials are not part of an ongoing or planned regulatory submission. This includes requests for clinical trial data for unlicensed products and indications. These clinical trial data can be requested by any qualified researchers who engage in rigorous, independent scientific research and will be provided following review and approval of a research proposal and statistical analysis plan and execution of a data sharing agreement. Data requests can be submitted at any time, and the data will be accessible for 12 months, with possible extensions considered. For more information on the process, or to submit a request, visit https://www.abbvie.com/ourscience/clinicaltrials/clinicaltrialsdataandinformationsharing/dataandinformationsharingwithqualifiedresearchers.html.
Code availability
Not applicable.
Authors’ contributions
All authors contributed to the study concept/design, data acquisition, analysis, and interpretation, as well as writing and critical review of the manuscript. All authors provided final approval of the submitted version.
References
- 1.Smolen JS, Aletaha D, Barton A, et al. Rheumatoid arthritis. Nat Rev Dis Primers. 2018;4:18001. doi: 10.1038/nrdp.2018.1. [DOI] [PubMed] [Google Scholar]
- 2.McInnes IB, Schett G. Pathogenetic insights from the treatment of rheumatoid arthritis. Lancet. 2017;389:2328–2337. doi: 10.1016/S0140-6736(17)31472-1. [DOI] [PubMed] [Google Scholar]
- 3.Alamanos Y, Voulgari PV, Drosos AA. Incidence and prevalence of rheumatoid arthritis, based on the 1987 American College of Rheumatology criteria: a systematic review. Semin Arthritis Rheum. 2006;36:182–188. doi: 10.1016/j.semarthrit.2006.08.006. [DOI] [PubMed] [Google Scholar]
- 4.Yamanaka H, Sugiyama N, Inoue E, et al. Estimates of the prevalence of and current treatment practices for rheumatoid arthritis in Japan using reimbursement data from health insurance societies and the IORRA cohort (I) Mod Rheumatol. 2013;24:33–40. doi: 10.3109/14397595.2013.854059. [DOI] [PubMed] [Google Scholar]
- 5.Sengul I, Akcay-Yalbuzdag S, Ince B, et al. Comparison of the DAS28-CRP and DAS28-ESR in patients with rheumatoid arthritis. Int J Rheum Dis. 2015;18:640–645. doi: 10.1111/1756-185X.12695. [DOI] [PubMed] [Google Scholar]
- 6.Smolen JS, Landewé R, Bijlsma J, et al. EULAR recommendations for the management of rheumatoid arthritis with synthetic and biological disease-modifying antirheumatic drugs: 2019 update. Ann Rheum Dis. 2020;79:685–699. doi: 10.1136/annrheumdis-2019-216655. [DOI] [PubMed] [Google Scholar]
- 7.Singh JA, Saag KG, Bridges SL, Jr, et al. 2015 American College of Rheumatology guideline for the treatment of rheumatoid arthritis. Arthritis Care Res (Hoboken). 2016;68:1–25. doi: 10.1002/acr.22783. [DOI] [PubMed] [Google Scholar]
- 8.Wang W, Zhou H, Liu L. Side effects of methotrexate therapy for rheumatoid arthritis: a systematic review. Eur J Med Chem. 2018;158:502–516. doi: 10.1016/j.ejmech.2018.09.027. [DOI] [PubMed] [Google Scholar]
- 9.Bello AE, Perkins EL, Jay R, et al. Recommendations for optimizing methotrexate treatment for patients with rheumatoid arthritis. Open Access Rheumatol. 2017;9:67–79. doi: 10.2147/OARRR.S131668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Smolen JS, Breedveld FC, Burmester GR, et al. Treating rheumatoid arthritis to target: 2014 update of the recommendations of an international task force. Ann Rheum Dis. 2016;75:3–15. doi: 10.1136/annrheumdis-2015-207524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Yu C, Jin S, Wang Y, et al. Remission rate and predictors of remission in patients with rheumatoid arthritis under treat-to-target strategy in real-world studies: a systematic review and meta-analysis. Clin Rheumatol. 2019;38:727–738. doi: 10.1007/s10067-018-4340-7. [DOI] [PubMed] [Google Scholar]
- 12.Combe B, Lula S, Boone C, et al. Effects of biologic disease-modifying anti-rheumatic drugs on the radiographic progression of rheumatoid arthritis: a systematic literature review. Clin Exp Rheumatol. 2018;36:658–667. [PubMed] [Google Scholar]
- 13.Nam JL, Ramiro S, Gaujoux-Viala C, et al. Efficacy of biological disease-modifying antirheumatic drugs: a systematic literature review informing the 2013 update of the EULAR recommendations for the management of rheumatoid arthritis. Ann Rheum Dis. 2014;73:516–528. doi: 10.1136/annrheumdis-2013-204577. [DOI] [PubMed] [Google Scholar]
- 14.Kalden JR, Schulze-Koops H. Immunogenicity and loss of response to TNF inhibitors: implications for rheumatoid arthritis treatment. Nat Rev Rheumatol. 2017;13:707–718. doi: 10.1038/nrrheum.2017.187. [DOI] [PubMed] [Google Scholar]
- 15.Rubbert-Roth A, Finckh A. Treatment options in patients with rheumatoid arthritis failing initial TNF inhibitor therapy: a critical review. Arthritis Res Ther. 2009;11:S1. doi: 10.1186/ar2666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.EMA. Xeljanz (tofacitinib): Summary of product characteristics 2017. https://www.ema.europa.eu/en/documents/product-information/xeljanz-epar-product-information_en.pdf. Accessed 1 Dec 2020.
- 17.EMA. Olumiant (baricitinib): Summary of product characteristics 2017. https://www.ema.europa.eu/en/documents/product-information/olumiant-epar-product-information_en.pdf. Accessed 1 Dec 2020.
- 18.EMA. RINVOQ (upadacitinib). Summary of product characteristics. 2019. https://www.emaeuropaeu/en/documents/product-information/rinvoq-epar-product-information_enpdf. Accessed 1 Dec 2020.
- 19.EMA. Jyseleca (filgotinib): Summary of product characteristics 2020. https://www.ema.europa.eu/en/documents/product-information/jyseleca-epar-product-information_en.pdf. Accessed 1 Dec 2020.
- 20.Gilead. Gilead receives complete response letter for filgotinib for the treatment of moderately to severely active rheumatoid arthritis 2020. https://www.gilead.com/news-and-press/press-room/press-releases/2020/8/gilead-receives-complete-response-letter-for-filgotinib-for-the-treatment-of-moderately-to-severely-active-rheumatoid-arthritis. Accessed 1 Dec 2020.
- 21.Burmester GR, Pope JE. Novel treatment strategies in rheumatoid arthritis. Lancet. 2017;389:2338–2348. doi: 10.1016/S0140-6736(17)31491-5. [DOI] [PubMed] [Google Scholar]
- 22.Fleischmann R, Mysler E, Hall S, et al. Efficacy and safety of tofacitinib monotherapy, tofacitinib with methotrexate, and adalimumab with methotrexate in patients with rheumatoid arthritis (ORAL strategy): a phase 3b/4, double-blind, head-to-head, randomised controlled trial. Lancet. 2017;390:457–468. doi: 10.1016/S0140-6736(17)31618-5. [DOI] [PubMed] [Google Scholar]
- 23.Taylor PC, Keystone EC, van der Heijde D, et al. Baricitinib versus placebo or adalimumab in rheumatoid arthritis. N Engl J Med. 2017;376:652–662. doi: 10.1056/NEJMoa1608345. [DOI] [PubMed] [Google Scholar]
- 24.A study in moderate to severe rheumatoid arthritis (RA-BEAM). https://clinicaltrials.gov/ct2/show/results/NCT01710358?view=results. Accessed 1 Dec 2020.
- 25.Fleischmann R, Pangan AL, Song IH, et al. Upadacitinib versus placebo or adalimumab in patients with rheumatoid arthritis and an inadequate response to methotrexate: results of a phase III, double-blind, randomized controlled trial. Arthritis Rheumatol. 2019;71:1788–1800. doi: 10.1002/art.41032. [DOI] [PubMed] [Google Scholar]
- 26.Combe B, Kivitz A, Tanaka Y, et al. LB0001 Efficacy and safety of filgotinib for patients with rheumatoid arthritis with inadequate response to methotrexate: FINCH1 primary outcome results. Ann Rheum Dis. 2019;78(S2):77–78. [Google Scholar]
- 27.Lee EB, Fleischmann R, Hall S, et al. Tofacitinib versus methotrexate in rheumatoid arthritis. N Engl J Med. 2014;370:2377–2386. doi: 10.1056/NEJMoa1310476. [DOI] [PubMed] [Google Scholar]
- 28.Fleischmann R, Schiff M, van der Heijde D, et al. Baricitinib, methotrexate, or combination in patients with rheumatoid arthritis and no or limited prior disease-modifying antirheumatic drug treatment. Arthritis Rheumatol. 2017;69:506–517. doi: 10.1002/art.39953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.van Vollenhoven R, Takeuchi T, Pangan A, et al. Efficacy and safety of upadacitinib monotherapy in methotrexate-naïve patients with moderately to severely active rheumatoid arthritis (SELECT-EARLY): a randomized, double-blind, active-comparator, multi-center, multi-country trial. Arthritis Rheumatol. 2020;72:1607–1620. doi: 10.1002/art.41384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Westhovens R, Rigby W, van der Heijde D, et al. LB0003 EFficacy and safety of filgotinib for patients with rheumatoid arthritis naïve to methotrexate therapy: FINCH3 primary outcome results. Ann Rheum Dis. 2019;78(S2):259–261. [Google Scholar]
- 31.Genovese MC, Kalunian K, Gottenberg JE, et al. Effect of filgotinib vs. placebo on clinical response in patients with moderate to severe rheumatoid arthritis refractory to disease-modifying antirheumatic drug therapy: The FINCH 2 randomized clinical trial. JAMA. 2019;322:315–325. doi: 10.1001/jama.2019.9055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Winthrop KL. The emerging safety profile of JAK inhibitors in rheumatic disease. Nat Rev Rheumatol. 2017;13:234. doi: 10.1038/nrrheum.2017.23. [DOI] [PubMed] [Google Scholar]
- 33.EMA. EMA confirms Xeljanz to be used with caution in patients at high risk of blood clots 2019. https://www.ema.europa.eu/en/medicines/human/referrals/xeljanz. Accessed 1 Dec 2020.
- 34.Taylor PC, Weinblatt ME, Burmester GR, et al. Cardiovascular safety during treatment with baricitinib in rheumatoid arthritis. Arthritis Rheumatol. 2019;71:1042–1055. doi: 10.1002/art.40841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Parmentier JM, Voss J, Graff C, et al. In vitro and in vivo characterization of the JAK1 selectivity of upadacitinib (ABT-494) BMC Rheumatol. 2018;2:23. doi: 10.1186/s41927-018-0031-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Tanaka Y. A review of upadacitinib in rheumatoid arthritis. Mod Rheumatol. 2020;30:1–9. doi: 10.1080/14397595.2020.1782049. [DOI] [PubMed] [Google Scholar]
- 37.FDA. RINVOQ (upadacitinib) Prescribing Information. https://www.accessdata.fda.gov/drugsatfda_docs/label/2019/211675s000lbl.pdf2019. Accessed 1 Dec 2020.
- 38.Rubbert-Roth A, Enejosa J, Pangan A, et al. Efficacy and safety of upadacitinib versus abatacept in patients with active rheumatoid arthritis and prior inadequate response or intolerance to biologic disease-modifying anti-rheumatic drugs (SELECT-CHOICE): a double-blind, rnadomized controlled Phase 3 trial [Abstract] Ann Rheum Dis. 2020;79:1011. [Google Scholar]
- 39.Kameda H, Takeuchi T, Yamaoka K, et al. Efficacy and safety of upadacitinib in Japanese patients with rheumatoid arthritis (SELECT-SUNRISE): a placebo-controlled phase IIb/III study. Rheumatology (Oxford) 2020;59:3303–3313. doi: 10.1093/rheumatology/keaa084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Fries JF, Spitz P, Kraines G, et al. Measurement of patient outcome in arthritis. Arthritis Rheum. 1980;23:137–145. doi: 10.1002/art.1780230202. [DOI] [PubMed] [Google Scholar]
- 41.Orbai AM, Bingham CO., 3rd Patient reported outcomes in rheumatoid arthritis clinical trials. Curr Rheumatol Rep. 2015;17:28. doi: 10.1007/s11926-015-0501-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.van der Heijde D. How to read radiographs according to the Sharp/van der Heijde method. J Rheumatol. 2000;27:261–263. [PubMed] [Google Scholar]
- 43.Cohen SB, van Vollenhoven R, Winthrop KL, et al. Safety profile of upadacitinib in rheumatoid arthritis: integrated analysis from the SELECT phase III clinical programme. Ann Rheum Dis. 2020 doi: 10.1136/annrheumdis-2020-218510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Cohen SB, van Vollenhoven R, Curtis JR, et al. Safety profile of upadacitinib up to 3 years of exposure in patients with rheumatoid arthritis [THU0197] Ann Rheum Dis. 2020;79:315. [Google Scholar]
- 45.Winthrop K, Nash P, Yamaoka K, et al. Incidence and risk factors for herpes zoster in rheumatoid arthritis patients receiving upadacitinib [THU0218] Ann Rheum Dis. 2020;79:331. doi: 10.1136/annrheumdis-2021-220822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Winthrop K, Calabrese LH, Van den Bosch F, et al. Characterization of serious infections with upadacitinib in patients with rheumatoid arthritis [FRI0141] Ann Rheum Dis. 2020;79:650. [Google Scholar]
- 47.Choy E, McInnes I, Cush J, et al. Incidence and risk of venous thromboembolic events among patients with rheumatoid arthritis enrolled in the upadacitinib SELECT clinical trial program [THU0195] Ann Rheum Dis. 2020;79:313. [Google Scholar]
- 48.Burmester GR, Kremer JM, Van den Bosch F, et al. Safety and efficacy of upadacitinib in patients with rheumatoid arthritis and inadequate response to conventional synthetic disease-modifying anti-rheumatic drugs (SELECT-NEXT): a randomised, double-blind, placebo-controlled phase 3 trial. Lancet. 2018;391:2503–2512. doi: 10.1016/S0140-6736(18)31115-2. [DOI] [PubMed] [Google Scholar]
- 49.Genovese MC, Fleischmann R, Combe B, et al. Safety and efficacy of upadacitinib in patients with active rheumatoid arthritis refractory to biologic disease-modifying anti-rheumatic drugs (SELECT-BEYOND): a double-blind, randomised controlled phase 3 trial. Lancet. 2018;391:2513–2524. doi: 10.1016/S0140-6736(18)31116-4. [DOI] [PubMed] [Google Scholar]
- 50.Burmester G, van den Bosch F, Bassette L, et al. Long-term safety and efficacy of upadacitinib in patients with rheumatoid arthritis and an inadequate response to csDMARDs: results at 60 weeks from the SELECT-NEXT study. Ann Rheum Dis. 2019;78:735–736. [Google Scholar]
- 51.Genovese MC, Combe B, Hall S, et al. Upadacitinib in patients with rheumatoid arthritis and inadequate response or intolerance to biological DMARDs: results at 60 weeks from the SELECT-BEYOND study. Ann Rheum Dis. 2019;78:360–361. [Google Scholar]
- 52.Fleischmann RM, Genovese MC, Enejosa JV, et al. Safety and effectiveness of upadacitinib or adalimumab plus methotrexate in patients with rheumatoid arthritis over 48 weeks with switch to alternate therapy in patients with insufficient response. Ann Rheum Dis. 2019;78:1454–1462. doi: 10.1136/annrheumdis-2019-215764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Smolen JS, Pangan AL, Emery P, et al. Upadacitinib as monotherapy in patients with active rheumatoid arthritis and inadequate response to methotrexate (SELECT-MONOTHERAPY): a randomised, placebo-controlled, double-blind phase 3 study. Lancet. 2019;393:2303–2311. doi: 10.1016/S0140-6736(19)30419-2. [DOI] [PubMed] [Google Scholar]
- 54.Smolen J, Emery P, Rigby W, et al. Upadacitinib as monotherapy in patients with rheumatoid arthritis: results at 48 weeks [abstract]. Arthritis Rheumatol. 2019;71(suppl 10).
- 55.van Vollenhoven R, Takeuchi T, Pangan A, et al. Monotherapy with upadacitinib in MTX-naive patients with rheumatod arthritis: results at 48 weeks from the SELECT-EARLY study. Ann Rheum Dis. 2019;78:376–377. [Google Scholar]
- 56.FDA. Tofacitinib Medical Review. Application Number 203214Orig1s000 2012. https://www.accessdata.fda.gov/drugsatfda_docs/nda/2012/203214Orig1s000MedR.pdf. Accessed 1 Dec 2020.
- 57.FDA. Tocilizumab Medical Review. Application Number 125276. 2009. https://www.accessdata.fda.gov/drugsatfda_docs/nda/2010/125276s000MedR.pdf. Accessed 1 Dec 2020.
- 58.FDA. Sarilumab Medical Review. Application Number 761037Orig1s000 2017. https://www.accessdata.fda.gov/drugsatfda_docs/nda/2017/761037Orig1s000MedR.pdf. Accessed 1 Dec 2020.
- 59.Tanaka Y, Ishii T, Cai Z, et al. Efficacy and safety of baricitinib in Japanese patients with active rheumatoid arthritis: a 52-week, randomized, single-blind, extension study. Mod Rheumatol. 2018;28:20–29. doi: 10.1080/14397595.2017.1307899. [DOI] [PubMed] [Google Scholar]
- 60.Winthrop KL, Yamanaka H, Valdez H, et al. Herpes zoster and tofacitinib therapy in patients with rheumatoid arthritis. Arthritis Rheumatol. 2014;66:2675–2684. doi: 10.1002/art.38745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Harigai M, Imafuku S, Sasaki N, et al. Incidence and risk factors for herpes zoster (HZ) in Japanese and global rheumatoid arthritis (RA) populations receiving upadacitinib (UPA). In: The 64th Annual Meeting of the Japanese Society of Rheumatology, 2020.
- 62.Yamaoka K, Tanaka Y, Kameda H, et al. Safety profile of upadacitinib (UPA) in Japanese patients (pts) with rheumatoid arthritis (RA). In: The 64th Annual Meeting of the Japanese Society of Rheumatology, 2020;20(Suppl).
- 63.FDA. Baricitinib, a JAK inhibitor for RA. Briefing Information for the April 23, 2018 Meeting of the Arthritis Advisory Committee (AAC). https://www.fda.gov/media/112372/download. Accessed 1 Dec 2020.
- 64.Simon TA, Thompson A, Gandhi KK, et al. Incidence of malignancy in adult patients with rheumatoid arthritis: a meta-analysis. Arthritis Res Ther. 2015;17:212. doi: 10.1186/s13075-015-0728-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Roubille C, Richer V, Starnino T, et al. The effects of tumour necrosis factor inhibitors, methotrexate, non-steroidal anti-inflammatory drugs and corticosteroids on cardiovascular events in rheumatoid arthritis, psoriasis and psoriatic arthritis: a systematic review and meta-analysis. Ann Rheum Dis. 2015;74:480–489. doi: 10.1136/annrheumdis-2014-206624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Choy E, McInnes I, Cush J, et al. MACE and VTE across multiple upadacitinib studies in rheumatoid arthritis: integrated analysis from the SELECT phase 3 clinical program [abstract]. Arthritis Rheumatol. 2019;71(suppl 10).
- 67.Kim SC, Schneeweiss S, Liu J, et al. Risk of venous thromboembolism in patients with rheumatoid arthritis. Arthritis Care Res (Hoboken). 2013;65:1600–1607. doi: 10.1002/acr.22039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Kroegel C, Reissig A. Principle mechanisms underlying venous thromboembolism: epidemiology, risk factors, pathophysiology and pathogenesis. Respiration. 2003;70:7–30. doi: 10.1159/000068427. [DOI] [PubMed] [Google Scholar]
- 69.Queeney K, Housley W, Sokolov J, et al. FRI0131 Elucidating the mechanism underlying creatine phosphokinase upregulation with upadacitinib. Ann Reum Dis. 2019;78(S2):734–735. [Google Scholar]
- 70.Nash P, Kerschbaumer A, Dörner T, et al. Points to consider for the treatment of immune-mediated inflammatory diseases with Janus kinase inhibitors: a consensus statement. Ann Rheum Dis. 2020;80:71–87. doi: 10.1136/annrheumdis-2020-218398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Mohamed MF, Klünder B, Othman AA. Clinical pharmacokinetics of upadacitinib: review of data relevant to the rheumatoid arthritis indication. Clin Pharmacokinet. 2020;59:531–544. doi: 10.1007/s40262-019-00855-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Klünder B, Mittapalli RK, Mohamed MF, et al. Population pharmacokinetics of upadacitinib using the immediate-release and extended-release formulations in healthy subjects and subjects with rheumatoid arthritis: analyses of phase I-III cinical trials. Clin Pharmacokinet. 2019;58:1045–1058. doi: 10.1007/s40262-019-00739-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Pavelka K, Szekanecz Z, Damjanov N, et al. Upadacitinib versus placebo or adalimumab with background methotrexate in patients with rheumatoid arthritis and an inadequate response to methotrexate: a subgroup analysis of a phase III randomized controlled trial in Central and Eastern European patients. Drugs Context. 2020;9:2020-7-5. doi: 10.7573/dic.2020-7-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Takeuchi T, Rischmueller M, Blanco R, et al. Upadacitinib monotherapy versus methotrexate monotherapy in methotrexate-naïve Japanese patients with rheumatoid arthritis: a sub-analysis of the Phase 3 SELECT-EARLY study. Mod Rheumatol. 2020:1–22. [DOI] [PubMed]
- 75.Zeng X, Zhao D, Radominski S, et al. SAT0160 Efficacy and safety of upadacitinib in patients from China, Brazil, and South Korea with rheumatoid arthritis who have had inadequate response to conventional synthetic disease-modifying antirheumatic drugs. Ann Rheum Dis. 2020;79(S1):1020–1021. [Google Scholar]
- 76.A study to compare upadacitinib (ABT-494) monotherapy to methotrexate (MTX) monotherapy in adults with rheumatoid arthritis (RA) who have not previously taken methotrexate (SELECT-EARLY) https://clinicaltrials.gov/ct2/show/NCT02706873. Accessed 1 Dec 2020.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.