Abstract
Background
Wide necked bifurcation aneurysms (WNBA) are among the most difficult aneurysms to treat. Very low dome-to-neck (DTN) and aspect ratios provide an even greater challenge in the management of WNBAs. We present the safety and efficacy profile for endovascular clip system (eCLIPs) device in the treatment of this subset of WNBAs with very unfavorable morphologies.
Methods
In our case series, 24 patients treated at 12 international centers were taken from a larger prospective voluntary post-marketing registry of 65 patients treated with the eCLIPs device and coiling. Those who had WNBAs at either the carotid or basilar terminus with a DTN ratio <1.6 and aspect ratio <1.2 were included. Radiologic and clinical outcomes were assessed immediately after the procedure and at the latest follow-up.
Results
The eCLIPs device was successfully deployed in 23 cases (96%). One patient (4.2%) died due to guidewire perforation distal to the implant site. No other complications were documented. After a mean follow-up of 15.8 months (range 3–40 months), good radiologic outcomes (modified Raymond–Roy classification (MRRC) scores of 1 or 2) were documented in 20 of 21 patients (95%) with follow-up data. The lone patient with an MRRC score of 3 showed coiled compaction after incomplete neck coverage with the device.
Conclusion
Our series of patients with aneurysms having adverse DTN and aspect ratios demonstrated that the eCLIPs device has a safety and efficacy profile comparable with currently available devices in the treatment of WNBAs.
Keywords: aneurysm, device
Introduction
Wide necked bifurcation aneurysms (WNBAs) present a unique challenge to endovascular repair. The wide neck predisposes to coil herniation into the parent artery while having the aneurysm at the bifurcation makes the use of more conventional maneuvers, such as stenting and flow diversion, technically difficult. A review of the treatment outcomes of WNBAs without stent assistance showed less than ideal complete or near complete occlusion rates (54.4% initial and 73.0% long term).1 Wide necked aneurysms have traditionally been defined as those having a neck measuring 4 mm or more.2 Aneurysm metrics, such as the dome-to-neck ratio (DTN, dome width/neck width) and aspect ratios (dome height/neck width), have also contributed to the varying definitions of a 'wide neck'. These adverse metrics create a challenge for successful delivery of intrasaccular contents into the aneurysm. A single center series has demonstrated that 25% of aneurysms with a DTN ratio of <1.6% and 89% of those with an aspect ratio of <1.2 needed an adjunctive device for endovascular repair.3 These aneurysms that are both wide and short present an even greater challenge when located in a bifurcation with arteries frequently arising from or adjacent to the aneurysm neck.
The endovascular clip system (eCLIPs) is a novel device that bridges the neck of the aneurysm and acts as a scaffold for coil retention. Furthermore, it has flow diversion properties that contributes to aneurysm closure.4 Having both of these characteristics makes eCLIPs different from other neck bridging devices, such as stents, pCONus, and PulseRider.5 In contrast with traditional stent type flow diverters, the device can also be 'coiled through' in cases of aneurysm persistence. The device has been previously demonstrated to be a viable treatment option for bifurcation aneurysms.6
Our aim was to determine the efficacy and safety of the eCLIPS device for WNBAs involving the internal carotid and basilar terminus with unfavorable aneurysm metrics (DTN <1.6 and aspect ratio <1.2).
Methods
Patient population
A prospective anonymized registry of all patients treated with eCLIPs was reviewed. Sixty-five patients were identified from registry inception in 2014 until May 2019 as having WNBAs at the carotid or basilar terminus. The registry is a post-marketing surveillance initiative supported by the manufacturer. Twelve clinical sites contributed, 11 in Europe after CE Mark approval, and one in Canada under its Special Access Program. Twenty-four patients fulfilled our inclusion criteria for this study: (1) wide neck; (2) located in a bifurcation of either the basilar or carotid terminus; (3) DTN <1.6; and (4) aspect ratio <1.2. Both untreated and previously repaired aneurysms with recurrence were included in the study. There were no patients with acutely ruptured aneurysms. The study focused on aneurysms with unfavorable metrics (DTN <1.6 and aspect ratio <1.2); thus aneurysms that did not fulfill these criteria were not included in the study. Local institutional review board approval was obtained.
Measurements of aneurysm characteristics to determine eligibility were obtained by application of standard angiographic measuring software to digital two-dimensional angiographic or three-dimensional reconstructed images of the pre-procedure angiogram performed by the site investigator. In recurrent aneurysms, the height was measured from the aneurysm neck to the bottom of the intrasaccular device (coils or Woven EndoBridge (WEB)).
eCLIPs treatment
The initial imaging of each patient was reviewed prior to acceptance for eCLIPs treatment by a three member clinical advisory board. All initial cases at new sites were mentored by someone from the clinical advisory board. All patients were pretreated with a regimen of dual antiplatelets, aspirin, and either clopidogrel or ticagrelor. The antiplatelets were kept on for 6 months after treatment.
The eCLIPs (Evasc Medical Systems Corp, Vancouver, British Columbia, Canada) is a device that has two distinct limbs: an anchoring limb that secures the device in one of the post-bifurcation vessels, and a second limb with higher density ribs that covers the aneurysm neck (see online supplementary figure 1). The latter limb, known as the 'leaf', functions to retain coils, diverts blood flow away from the aneurysm, and serves as a scaffold for neointimal growth across the neck. The non-circumferential design of the device allows it to function with no metal in the main branch (basilar trunk or terminal carotid) and unimpeded access to side branches. The porosity of the device is approximately 65% (range 58–77%) depending on vessel diameter, similar to that of conventional flow diverters.4 6 The device is recommended for aneurysms having necks with lengths <6 mm and aneurysm neck breadth (perpendicular diameter to length) <4.75 mm.
neurintsurg-2020-016354supp001.pdf (547.7KB, pdf)
All patients underwent a neuroendovascular procedure with a quadriaxial technique. After obtaining percutaneous transfemoral access, intravenous heparin was administered. Through a short 8 F sheath, a long sheath was placed in either the left or right subclavian artery or common carotid artery. Afterwards, a 6 F Navien distal access catheter (Medtronic, Minneapolis, Minnesota, USA) was advanced into the vertebral artery or internal carotid artery. A 4.2 F Fargo mini-catheter (Balt, Montmorency, France) and a Prowler Select Plus microcatheter (Johnson & Johnson, New Brunswick, New Jersey, USA) over a 0.014 inch microwire were placed in the P1 segment of the posterior cerebral artery in the case of a basilar terminus aneurysm, or in the A1 segment of the anterior cerebral artery or the M1 segment of the middle cerebral artery in the case of a carotid terminus aneurysm.
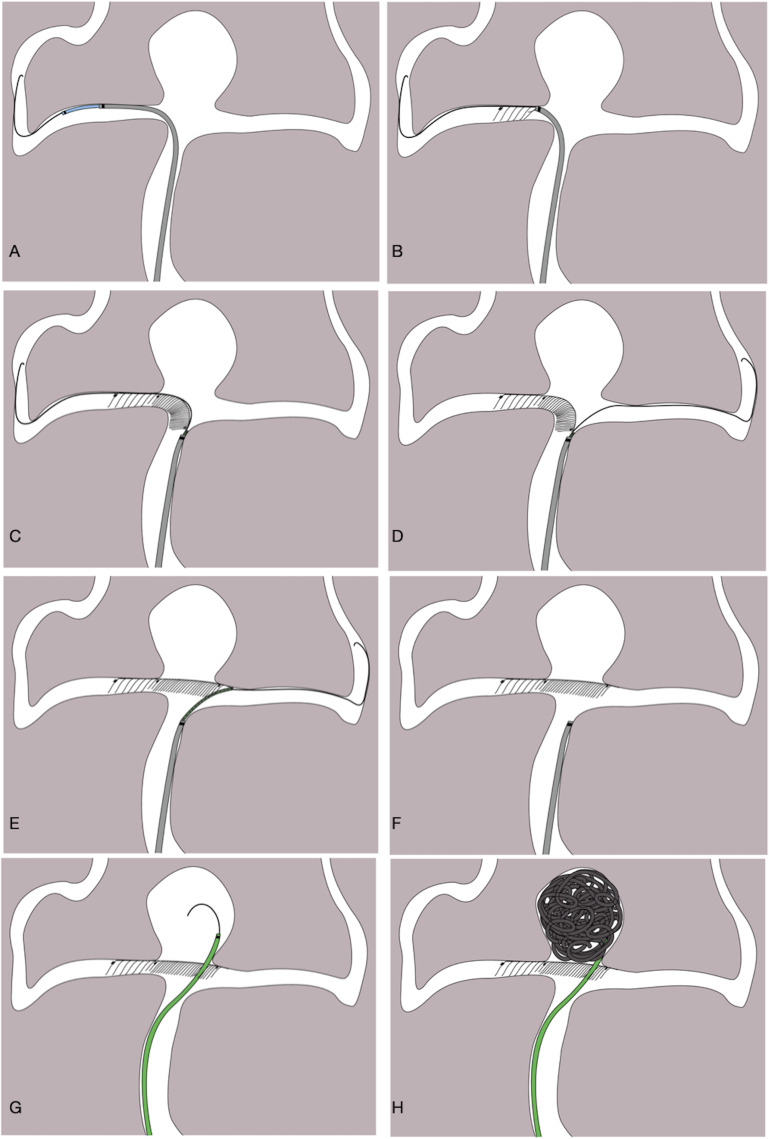
The 0.014 inch wire and the Prowler Select Plus microcatheter were removed and the eCLIPs system was advanced through the Fargo mini over a 0.014 inch wire and deployed by pulling the Fargo mini back. After complete unsheathing of the eCLIPs, the wire was retracted proximally and subsequently advanced into the contralateral branch. Afterwards, the eCLIPs was advanced over this wire until complete neck coverage was achieved. Once the operator was satisfied with the position of the device, the device was mechanically detached from its pusher. After complete deployment of the eCLIPs, the device was crossed with a microcatheter and the aneurysm coiled (figure 1). A video of device deployment is available at https://vimeo.com/191976808.6
Figure 1.
Endovascular repair of a basilar artery terminus aneurysm with the endovascular clip system (eCLIPs) and coiling. (A) A microwire (thin black line), microcatheter (blue), and intermediate microcatheter (gray) are taken into a P1 segment. (B) After being brought up to the treatment site through the intermediate microcatheter, the device is carefully unsheathed to secure the anchoring limb in the proximal P1. (C)The device is further unsheathed to reveal the 'leaf' with higher density of ribs. (D)After complete unsheathing of the eCLIPs, the microwire is retracted proximally and subsequently advanced into the contralateral P1 segment. (E)The device is advanced over the wire until the leaf attains complete coverage of the aneurysm neck. (F)Complete deployment of the device after detachment. (G, H) The device is crossed with a coiling microcatheter (green) and the aneurysm is filled with coils in the standard manner.
Outcomes
The outcomes of the study included: radiologic outcomes immediately after the procedure and on the most recent follow-up, technical success, periprocedural complications, retreatment, and clinical outcomes. Technical success was defined as successful deployment of the device across the neck of the aneurysm and subsequent coiling. Radiologic outcomes were assessed in terms of the modified Raymond–Roy classification (MRRC).7 A good radiologic outcome was defined as an MRRC score of 1 (complete obliteration) or 2 (residual neck). Follow-up imaging was done with either catheter angiography or MR angiography (MRA). Periprocedural complications included wire perforations, arterial dissections, side branch stenosis, and aneurysm rupture. Side branch stenosis was defined as a decrease of >50% in the size of the vessel lumen. Clinical outcomes included neurologic events and mortality. Neurologic events included persistent deterioration in the sensorium and focal deficits.
The follow-up protocol implemented was according to the site’s usual practice. Neurovascular imaging was repeated at 6 months, 12 months, and annually thereafter to monitor the status of the aneurysm. Evaluation of radiologic outcomes was performed by an independent core laboratory. Clinical outcomes were assessed by physicians at the participating sites.
Results
Baseline characteristics
This case series reports 24 patients with a mean age of 57 years. Eleven patients (46%) had a prior embolization procedure: one was initially treated with a WEB device and the others were initially treated with coils, eCLIPs treatment occurring at variable time intervals after the initial treatment. Three (13%) patients had more than one previous endovascular repair procedure. None of the patients had prior treatment with stents, flow diverters, or other neck bridging devices, such as the PulseRider or the pCONus. The majority of the aneurysms (92%) were located at the basilar terminus. Mean neck width was 5.5 mm. Mean DTN ratio and aspect ratio were 1.20 and 0.82, respectively (see online supplementary table 1).
Outcomes
The eCLIPs effectively bridged the neck in 23 of 24 (96%) patients. In one patient with a carotid terminus aneurysm, access to the contralateral branch (A1) with the leaf could not be achieved despite multiple attempts; thus only partial neck coverage was achieved. Despite this, coiling was still accomplished. In one patient, a small thrombus developed during implantation but resolved completely with more heparin. One patient had a small dissection in the vertebral artery during vessel access. A stent was placed over the dissection and the aneurysm repair was carried out without incident. There were no clinical sequelae documented from these events.
One patient died from a subarachnoid hemorrhage a few hours after an apparently uneventful procedure. After the death of this patient a careful analysis of the intraprocedural angiography was performed and a guidewire perforation of a vessel distal to the aneurysm treatment site could be seen. The rest of the patients had no neurologic deficit at discharge or at the most recent follow-up.
Radiologic outcomes in terms of MRRC scores were determined by a core laboratory based on imaging obtained at the end of the procedure and at each follow-up. Immediately after endovascular repair, 20 (83%) of the aneurysms had good radiologic outcomes. The remaining three patients had MRRC scores of 3a (n=1) and 3b (n=2). In one case, the core laboratory was not able to determine the MRRC score because the image quality was judged to be poor.
Because the registry was voluntary, follow-up data were obtained at different follow-up times depending on the local site’s usual practice. Mean follow-up was 15.8 months (range 3–40). Twenty-one of 24 (88%) patients had follow-up imaging data. Six patients had follow-up with MRA only. Seven patients had initial follow-up with DSA and then subsequent follow-up with MRA. Eight patients had DSA follow-up imaging only. Three patients did not have imaging follow-up data: two patients refused any follow-up imaging and one patient, as described above, died. The two patients without follow-up imaging were doing well clinically at their latest follow-up.
At the most recent follow-up, 20 of 21 (95%) patients with available data had good radiologic outcomes. The degree of occlusion (MRRC) was stable in 14 patients, improved in 4 patients, and regressed in 2 patients (MRRC scores from 1 to 2). The lone patient with only partial neck coverage described above was the only documented retreatment. Repeat coiling was done 3.5 months later because of coil compaction resulting in a significant residual. Radiologic outcomes are summarized in table 1. Assuming that the three patients without imaging follow-up data had poor radiologic outcomes, 83.3% (20/24) of all patients would still have good radiologic outcomes.8 9
Table 1.
Radiologic outcomes
| Post repair (n=24)* | Latest follow-up (n=21) | |
| MRRC 1 (n (%)) | 14 (58.3) | 13 (61.9) |
| MRRC 2 (n (%)) | 6 (25) | 7 (33.3) |
| MRRC 3a (n (%)) | 1 (4.2) | – |
| MRRC 3b (n (%)) | 2 (8.3) | 1 (4.8) |
| Image quality too poor for MRRC grading (n (%)) | 1 (4.2) | – |
*One image post-repair was deemed too poor for MRRC grading.
MRRC, modified Raymond–Roy classification.
Discussion
In our cohort of WNBAs with unfavorable aneurysm metrics, the eCLIPs (1) was successfully deployed in 23/24 (96%) patients; (2) had good radiologic outcomes at follow-up in 20/21 (95%) cases; and (3) had a low retreatment (1/24, 4.2%) and mortality rate (1/24, 4.2%) that was comparable with other devices used to treat WNBAs.8 9
Radiologic outcomes compared with other endovascular treatment strategies for WNBAs
Despite the complex aneurysms included in our series (WNBAs, unfavorable metrics, 92% located at the basilar terminus, and 46% recurrent aneurysms with previous treatment), the radiologic outcomes of the eCLIPS device were comparatively better than other adjunct devices. A recent meta-analysis of treatment results of WNBAs revealed that only 40% were completely occluded after endovascular treatment.10 A subset of patients with wide necked aneurysms in the Matrix and Platinum Science trial were treated with stent assisted coiling which resulted in 45.7% complete occlusion.11 In the BRANCH (wide neck bifurcation aneurysms of the middle cerebral artery and basilar apex treated by endovascular techniques) study that utilized only balloon and stents for WNBAs (DTN ratio <2 and neck >4 mm), only 63% of aneurysms achieved good radiologic outcomes at follow-up. Pooled data from three prospective multicenter series using the WEB system, an intrasaccular device for flow diversion, for bifurcation aneurysms showed that 242/306 (79.1%) patients attained good radiologic outcomes (complete occlusion or neck remnant) at follow-up.12 In the Adjunctive Neurovascular Support of Wide neck aneurysm Embolization and Reconstruction (ANSWER) trial, with the PulseRider, a neck bridging device, 87.9% of aneurysms attained good radiologic outcomes at follow-up.13 However, a recent meta-analysis of the pCONus that collected data from eight clinical retrospective series showed a long term complete occlusion rate of 60%.14
A detailed breakdown of the aneurysm metrics and outcomes in studies utilizing adjunctive devices for WNBAs is shown in table 2. Both the mean aspect ratio (0.82 vs 1.1-1.5) and the DTN ratio (1.2 vs 1.34-1.8) were substantially less in our series compared with the other studies (1.1–1.5). These results imply that our series had more unfavorable aneurysm metrics—that is, shorter and wider aneurysms with a greater tendency for suboptimal treatment of coil herniation.
Table 2.
Aneurysm metrics and outcomes in contemporary trials describing devices to treat wide necked aneurysms
| Author (No of patients) |
De Vries (current study) (24) | De Leacy25
(115) |
Gawlitza18
(17) |
Khalid8
(16) |
Piotin26
(63) |
Sourour27
(12) |
Spiotta13
(34) |
Fischer9
(25) |
| Adjunctive device | eCLIPs | Balloon and stent | WEB | WEB | Luna | Medina | PulseRider | pCONus |
| Mechanism | Neck bridging and extrasaccular flow diversion | Neck bridging | Intrasaccular flow diversion | Intrasaccular flow diversion | Intrasaccular flow diversion | Intrasaccular flow diversion | Neck bridging | Neck briding |
| Aneurysms included | Wide necked bifurcation: BA, ICA | Wide necked: BA, MCA | Recurrent: BA, ICA, MCA, PComA | Large: BA, MCA, AcomA | Wide necked bifurcation or side wall: BA, ACA, ICA, MCA, AComA, PcomA, PICA | Wide necked bifurcation: MCA, BA | Wide necked bifurcation: ICA, BA | Wide necked bifurcation: ICA, BA, MCA, AComA |
| Aneurysm metrics | ||||||||
| Neck width (mm) | 5.5 | 4.85 | 5.3 | 6.2 | 3.9 | 4.4 | 5.2 | 6 |
| Dome width (mm) | 6.7 | 7.66 | 7.5 | 10.5 | 5.7 | 7.5 | 7 | 9 |
| Aneurysm height (mm) | 4.8 | – | 6 | 9 | – | – | 7.2 | – |
| Dome-to-neck ratio | 1.20 | 1.42 | 1.4 | 1.8 | 1.46 | 1.4 | 1.34 | 1.5 |
| Aspect ratio | 0.82 | – | 1.1 | 1.5 | – | – | 1.38 | – |
| Outcomes | ||||||||
| Good radiologic outcomes at follow-up (%) | 95 | 63 | 73.3 | 80 | 80 | 83 | 87.9 | 81 |
| Retreatment (%) | 0 | 8.7 | 11.8 | 46.7 | 6.3 | 8.3 | 2.9 | 0 |
| Average follow-up (months) | 15.8 | 12.2 | 12.1 | 36 | 36 | 5.2 | 6 | 9.5 |
ACA, anterior cerebral artery; AComA, anterior communicating artery; BA, basilar artery; ICA, internal carotid artery; MCA, middle cerebral artery; PComA, posterior communicating artery; PICA, posterior inferior cerebellary artery; WEB, Woven EndoBridge.
eCLIPs has some technical limitations. The device is recommended only when one of the arteries past the bifurcation measures 1.5–3.25 mm. In addition, a very acute take off angle and tortuous morphology of the post bifurcation arteries makes the placement of the device more difficult. In these situations, other measures, such as intrasaccular flow diversion with the WEB device15 and other neck bridging devices such as the pCONus,16 may be considered. Only basilar and carotid terminus aneurysms were included in this study based on the size of the current device and the local anatomy at these two sites. Another smaller version of the device has been recently developed for bifurcation configurations at the anterior communicating artery and middle cerebral artery, each of which have smaller branches into which the anchoring segment of the device will land.
Recurrent aneurysms
Eleven (46%) of the patients in our series had recurrent aneurysms, having already undergone a previous endovascular repair. All of these patients had good radiologic outcomes at follow-up and none underwent retreatment. A large review for repeat coiling in aneurysms found a need for adjunctive devices in nearly 30% of cases and a complete occlusion rate of <50%.17 A series of WEB treated recurrent aneurysms demonstrated a good radiologic outcome of 73.3%. However, 11.8% of these patients underwent retreatment after a mean follow-up of 12.1 months18 (table 2). Unlike intrasaccular devices, eCLIPs is agnostic to aneurysm metrics. These data would suggest that eCLIPs is particularly suited to recurrent aneurysms due to compaction of intrasaccular contents where the aspect ratio is very low. We present two of our cases with a recurrent basilar tip aneurysm treated with eCLIPs (see online supplementary figures 2 and 3).
The single case in our series with incomplete neck coverage and subsequent retreatment 3 months later remained an MRRC 3b, 7 months after the initial procedure. This demonstrates the importance of full neck coverage for optimal flow diversion.
Safety
The safety profile of eCLIPS compares favorably with several other reported treatment modalities of these complex lesions.13 14 19–21 Fargen et al, in the largest case series on Y stenting, reported an 8.9% post-treatment ischemic event rate.19 In the PulseRider trial, 8.8% of patients had permanent neurological sequelae.13 The meta-analysis of the pCONus documented a perioperative morbidity and mortality rate of 7%.14 WEB treatment in more challenging aneurysms, as reported in the separate series of Gawlizta and Khalid, demonstrated 23% and 18.8% complication rates, respectively.8 18 Apart from the single case of distal vessel perforation resulting in subsequent subarachnoid hemorrhage and death, no other hemorrhagic or thromboembolic complications causing lasting neurologic sequelae were encountered in our series.
eCLIPs flow diversion
Intrasaccular devices such as coils and the WEB, while disrupting flow within the aneurysm and promoting thrombosis, do not block the water hammer jet of blood entering the aneurysm neck. Thus they may still be subject to long term compaction.22–24 Figure 2 illustrates the distinction between the flow disrupting effect of a true neck bridging device and an intrasaccular device. The leaf segment placed across the neck mitigates this water hammer effect and is possibly the factor preventing deterioration of radiologic outcomes at follow-up. A series on the use of WEB devices in large complex aneurysms reported a 46.7% retreatment rate for increasing shortening of the device and distal dislocation.8 The coils inside other neck bridging devices, such as the PulseRider and pCONus, that do not have flow diverting properties, will also be subject to the same force and subsequent compaction. The extra-aneurysmal leaf segment of the eCLIPs device also serves as a platform for endothelial growth in the long term.4
Figure 2.
The difference between the endovascular clip system (eCLIPs) and an intrasaccular device (Woven EndoBridge or coils). (A) Basilar terminus aneurysm with the jets of blood (broken arrows) going into the aneurysm. (B) With an intrasaccular device, such as coils (black oval), and a neck bridging device, such as the eCLIPs device, the leaf (thick semi-solid line) absorbs the water hammer jet of blood (broken arrows) and diverts flow away from the aneurysm (black arrows). (C) With an intrasaccular device only (black oval), the water hammer jet of blood (broken arrows) still enters the aneurysm neck and predisposes to device compaction in the long term.
Limitations
The major limitations of this study include the lack of uniformity in the imaging modalities and follow-up schedule/clinical outcome assessment, and the limited number of patients.
Conclusion
The eCLIPs has demonstrated comparable radiologic outcomes and safety profile for our subset of WNBAs with unfavorable aneurysm metrics. The data presented in this case series suggest the need for a more robust prospective clinical study of this complex patient population. A separate prospective independently monitored European clinical trial, European ECLIPs Efficacy and Safety Investigation (EESIS), is currently ongoing (https://clinicaltrials.gov/ct2/show/NCT02607501).
Acknowledgments
The authors acknowledge the contributions of Dr Donald Ricci (post-marketing registry) and Dr Anton Meijer (core laboratory). Dr Ricci provided the data from a post-marketing registry that addresses such a cohort of patients. Dr Ricci is a principal of eVasc Neurovascular, manufacturers of the eCLIPs. Dr Meijer conducted the independent review of images to assess the MRRC score for this case series.
Footnotes
Contributors: JDV and LS identified the gap in knowledge about management of highly complex WNBAs. Collectively the remaining authors confirmed a lack of consensus, either in clinical practice or in the literature, in the management of these lesions. All other authors reviewed the manuscript and provided feedback for the final draft. JDV, as guarantor, accepts full responsibility for the work and/or the conduct of the study, having had access to the data, and controlling the decision to publish.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial, or not-for-profit sectors.
Competing interests: JDV is a consultant for Evasc; honoraria is paid to his institution. LS is a consultant for, and receives honoraria from, Evasc. TRM is a principal of eVasc Neurovascular, manufacturers of the eCLIPs.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement
Data are available upon reasonable request.
Ethics statements
Patient consent for publication
Not required.
Ethics approval
Local institutional review board approval was obtained.
References
- 1. Zhao B, Yin R, Lanzino G, et al. Endovascular coiling of wide-neck and wide-neck bifurcation aneurysms: a systematic review and meta-analysis. AJNR Am J Neuroradiol 2016;37:1700–5. 10.3174/ajnr.A4834 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Hendricks BK, Yoon JS, Yaeger K, et al. Wide-neck aneurysms: systematic review of the neurosurgical literature with a focus on definition and clinical implications. J Neurosurg 2019:159–65. 10.3171/2019.3.JNS183160 [DOI] [PubMed] [Google Scholar]
- 3. Brinjikji W, Cloft HJ, Kallmes DF. Difficult aneurysms for endovascular treatment: overwide or undertall? AJNR Am J Neuroradiol 2009;30:1513–7. 10.3174/ajnr.A1633 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Marotta TR, Riina HA, McDougall I, et al. Physiological remodeling of bifurcation aneurysms: preclinical results of the eCLIPs device. J Neurosurg 2018;128:475–81. 10.3171/2016.10.JNS162024 [DOI] [PubMed] [Google Scholar]
- 5. Peach TW, Ricci D, Ventikos Y. A virtual comparison of the eCLIPs device and conventional flow-diverters as treatment for cerebral bifurcation aneurysms. Cardiovasc Eng Technol 2019;10:508–19. 10.1007/s13239-019-00424-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Chiu AH, De Vries J, O'Kelly CJ, et al. The second-generation eCLIPs endovascular clip system: initial experience. J Neurosurg 2018;128:482–9. 10.3171/2016.10.JNS161731 [DOI] [PubMed] [Google Scholar]
- 7. Mascitelli JR, Moyle H, Oermann EK, et al. An update to the Raymond-Roy occlusion classification of intracranial aneurysms treated with coil embolization. J Neurointerv Surg 2015;7:496–502. 10.1136/neurintsurg-2014-011258 [DOI] [PubMed] [Google Scholar]
- 8. Khalid Z, Sorteberg W, Nedregaard B, et al. Efficiency and complications of Woven EndoBridge (web) devices for treatment of larger, complex intracranial aneurysms-a single-center experience. Acta Neurochir 2019;161:393–401. 10.1007/s00701-018-3752-0 [DOI] [PubMed] [Google Scholar]
- 9. Fischer S, Weber A, Titschert A, et al. Single-center experience in the endovascular treatment of wide-necked intracranial aneurysms with a bridging intra-/extra-aneurysm implant (pCONus). J Neurointerv Surg 2016;8:1186–91. 10.1136/neurintsurg-2015-012004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Fiorella D, Arthur AS, Chiacchierini R, et al. How safe and effective are existing treatments for wide-necked bifurcation aneurysms? Literature-based objective performance criteria for safety and effectiveness. J Neurointerv Surg 2017;9:1197–201. 10.1136/neurintsurg-2017-013223 [DOI] [PubMed] [Google Scholar]
- 11. Hetts SW, Turk A, English JD, et al. Stent-assisted coiling versus coiling alone in unruptured intracranial aneurysms in the matrix and platinum science trial: safety, efficacy, and mid-term outcomes. AJNR Am J Neuroradiol 2014;35:698–705. 10.3174/ajnr.A3755 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Pierot L, Moret J, Barreau X, et al. Safety and efficacy of aneurysm treatment with WEB in the cumulative population of three prospective, multicenter series. J Neurointerv Surg 2018;10:553–9. 10.1136/neurintsurg-2017-013448 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Spiotta AM, Derdeyn CP, Tateshima S, et al. Results of the ANSWER trial using the PulseRider for the treatment of broad-necked, bifurcation aneurysms. Neurosurgery 2017;81:56–65. 10.1093/neuros/nyx085 [DOI] [PubMed] [Google Scholar]
- 14. Sorenson TJ, Iacobucci M, Murad MH, et al. The pCONUS bifurcation aneurysm implants for endovascular treatment of adults with intracranial aneurysms: a systematic review and meta-analysis. Surg Neurol Int 2019;10:24. 10.4103/sni.sni_297_18 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Arthur AS, Molyneux A, Coon AL, et al. The safety and effectiveness of the Woven EndoBridge (web) system for the treatment of wide-necked bifurcation aneurysms: final 12-month results of the pivotal web intrasaccular therapy (web-it) study. J Neurointerv Surg 2019;11:924–30. 10.1136/neurintsurg-2019-014815 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Aguilar Perez M, AlMatter M, Hellstern V, et al. Use of the pCONus HPC as an adjunct to coil occlusion of acutely ruptured aneurysms: early clinical experience using single antiplatelet therapy. J Neurointerv Surg 2020. 10.1136/neurintsurg-2019-015746. [Epub ahead of print: 26 Feb 2020]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Henkes H, Fischer S, Liebig T, et al. Repeated endovascular coil occlusion in 350 of 2759 intracranial aneurysms: safety and effectiveness aspects. Neurosurgery 2006;58:224–32. 10.1227/01.NEU.0000194831.54183.3F [DOI] [PubMed] [Google Scholar]
- 18. Gawlitza M, Soize S, Januel A-C, et al. Treatment of recurrent aneurysms using the Woven EndoBridge (WEB): anatomical and clinical results. J Neurointerv Surg 2018;10:629–33. 10.1136/neurintsurg-2017-013287 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Fargen KM, Mocco J, Neal D, et al. A multicenter study of stent-assisted coiling of cerebral aneurysms with a y configuration. Neurosurgery 2013;73:466–72. 10.1227/NEU.0000000000000015 [DOI] [PubMed] [Google Scholar]
- 20. Pierot L, Spelle L, Molyneux A, et al. Clinical and anatomical follow-up in patients with aneurysms treated with the WEB device: 1-year follow-up report in the cumulated population of 2 prospective, multicenter series (WEBCAST and French Observatory). Neurosurgery 2015;78:133–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Pierot L, Gubucz I, Buhk JH, et al. Safety and efficacy of aneurysm treatment with the WEB: results of the WEBCAST 2 study. AJNR Am J Neuroradiol 2017;38:1151–5. 10.3174/ajnr.A5178 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Henkes H, Fischer S, Mariushi W, et al. Angiographic and clinical results in 316 coil-treated basilar artery bifurcation aneurysms. J Neurosurg 2005;103:990–9. 10.3171/jns.2005.103.6.0990 [DOI] [PubMed] [Google Scholar]
- 23. Crobeddu E, Lanzino G, Kallmes DF, et al. Review of 2 decades of aneurysm-recurrence literature, part 1: reducing recurrence after endovascular coiling. AJNR Am J Neuroradiol 2013;34:266–70. 10.3174/ajnr.A3032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Cognard C, Januel AC. Remnants and recurrences after the use of the WEB intrasaccular device in large-neck bifurcation aneurysms. Neurosurgery 2015;76:522–30. 10.1227/NEU.0000000000000669 [DOI] [PubMed] [Google Scholar]
- 25. De Leacy RA, Fargen KM, Mascitelli JR, et al. Wide-neck bifurcation aneurysms of the middle cerebral artery and basilar apex treated by endovascular techniques: a multicentre, core lab adjudicated study evaluating safety and durability of occlusion (BRANCH). J Neurointerv Surg 2019;11:31–6. 10.1136/neurintsurg-2018-013771 [DOI] [PubMed] [Google Scholar]
- 26. Piotin M, Biondi A, Sourour N, et al. The LUNA aneurysm embolization system for intracranial aneurysm treatment: short-term, mid-term and long-term clinical and angiographic results. J Neurointerv Surg 2018;10:E34. 10.1136/neurintsurg-2018-013767 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Sourour N-A, Vande Perre S, Maria FD, et al. Medina® embolization device for the treatment of intracranial aneurysms: safety and angiographic effectiveness at 6 months. Neurosurgery 2018;82:155–62. 10.1093/neuros/nyx161 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
neurintsurg-2020-016354supp001.pdf (547.7KB, pdf)
Data Availability Statement
Data are available upon reasonable request.