Abstract
In light of recent advances in HIV prevention and treatment, we reviewed the literature to understand how different types of stigma impact HIV risk; access to HIV prevention, care, and treatment services; and related health outcomes among men who have sex with men (MSM) in the US. We conducted a scoping literature review of observational and qualitative studies that examined stigma and HIV-related outcomes among MSM. Our search identified 5794 studies, of which 47 met the eligibility criteria and were included in the final analysis. The review suggests that stigma remains a formidable barrier to engaging in HIV prevention and treatment among both HIV-negative and HIV-positive MSM. Among the studies of HIV-positive MSM, internalized stigma was related to lower levels of treatment engagement. HIV-positive MSM in the Southern part of the US were also more likely to engage in risky sexual behavior. Perceived health care discrimination was negatively associated with PrEP awareness, particularly among HIV-negative Black MSM. Among young MSM of color, intersectional stigma compounded the social structural barriers to PrEP adherence. Findings indicate that stigma reduction interventions should be implemented in diverse MSM communities to address the disproportionate burden of HIV along with critical gap in the care continuum. Further research should examine how individual types of stigma, including intersectional stigma, affect viral suppression and PrEP uptake and adherence, especially among MSM of color.
Supplementary Information
The online version contains supplementary material available at 10.1007/s10461-021-03262-4.
Keywords: Stigma, Discrimination, Intersectionality, HIV, MSM, Scoping review
Introduction
Stigma is a social-psychological construct that manifests in a process by which individuals relegated to a particular social category are subjected to prejudice, discrimination, and unfair treatment because of this category [1, 2]. Stigma has been shown to relate to host of negative health outcomes [1, 2]. Thus, different domains of stigma have been studied to enhance health-related research and develop interventions that specifically target these domains. Enacted stigma refers to the actual experience of prejudice and discrimination that occurs due to one’s social category (e.g., being the victim of a hate crime because one is gay) [3]. Anticipated stigma is the fear or expectation of being rejected due to, for example, one’s social category (e.g., sexual identity, gender identity, race/ethnicity, or HIV serostatus) [4]. Perceived stigma refers to one’s perception about how others might feel about them because they are part of stigmatized group [5]. Internalized stigma is the internalization of negative societal attitudes related to one’s stigmatized identity, typically resulting in diminished self-worth [6]. Marginalized groups such as men who have sex with men (MSM) often contend with these various forms of stigma. Further, because they may also possess more than one minority status (e.g., Black, gay man), they may also experience intersectional stigma [7, 8], which studies have begun to demonstrate negatively impact HIV-related outcomes among MSM [9].
Understanding the impacts of stigma on HIV risk, prevention, and care among MSM warrants immediate attention, as empirical studies continue to show that MSM are disproportionately affected by HIV, despite advances in prevention and treatment [10–12]. In fact, in 2018, 1.1 million people in the US were living with HIV, with MSM accounting for approximately 69% of all the diagnosed HIV infections [13]. The burden that is concentrated among this population has been attributed to a combination of psychosocial factors contributing to syndemics among MSM [14–18]. For example, syndemic factors such as child abuse, substance use, depression, traumatic stress, as well as various forms of stigma interact to increase the vulnerability of these individuals and confer excess risk to HIV infection [15, 16, 19]. One of the suggested mechanisms is through minority stress pathway [20, 21]. In addition to concurrently acting as factors that amplifies the risks for HIV, stigma or marginalization associated with sexual identity, exploration, and race has also been known to act in an additive way through this path [17, 22].
In the absence of a cure for HIV infection, HIV prevention methods and programs that use antiretroviral treatment (ART), also referred to as Treatment as Prevention (TasP) can control and prevent further spread of the virus to uninfected individuals [23]. However, efficacy and effectiveness of TasP can be greatly reduced in MSM who are often stigmatized due to concurrent discriminations acting in unison. Different types of stigma such as internalized stigma, HIV related stigma, stigma experienced in healthcare settings impacts prevention strategies and results in reduced accessibility and decreased quality of care [24, 25]. Thus, stigma may play a significant role in hampering HIV prevention efforts among the MSM population. It can discourage them from seeking information, prevent them from getting tested, seeking care or support, and hinder access to biomedical interventions such as TasP and PrEP [26]. This has resulted in significant challenges when conducing biobehavioral HIV surveillance studies as well as understanding of the social structural factors contributing to HIV risk. In order to strengthen efforts to characterize and to reduce stigma and discrimination and further improve health outcomes, an improved understanding of how stigma impacts HIV risk and access to prevention and care among MSM is needed. Studies have assessed stigma in different ways, some examine it by using a scale while others adopted a more qualitative or a mixed method approach [20, 27, 28]. This paper presents a critical scoping review by summarizing the largely fragmented literature on stigma among MSM in the United States as it pertains to risk of HIV infection, access to prevention, care and treatment services, and other health outcomes. The review is guided by the following research questions:
How did the studies conceptualize and measure individual types of stigma as well as intersectional stigma?
How did different types of stigma affect HIV risks, in particular syndemic conditions?
What types of stigma negatively impact prevention (e.g., PrEP) and care continuum outcomes?
Our objectives were to summarize research on the associations between stigma and these different measures of HIV cascade by systematically reviewing peer-reviewed literature. In line with the broad coverage of our topic, a scoping review was chosen as the most appropriate methodology to inform the way research has been conducted [29].
Methods
Search Strategy
Original peer-reviewed articles published in English language journals from early 1980’s to October 2019 were obtained from systematic searches of five electronic bibliographic databases: PubMed, CINAHL, Psych Info, Scopus, and Web Science. The search was implemented in November 2019. The search query consisted of terms such as stigma, discrimination, stereotype, gay, HIV, AIDS, MSM or other associated terms (supplementary file), and this was tailored to the specific requirements of each database. Grey literature, commentaries, or other document types such as reports, and essays were excluded since they were not peer reviewed. All identified articles from the searches were transferred to a bibliographic management system software program (EndNote, Rayyan). Duplicates were excluded by automatic duplication removal process in EndNote’s default one step auto-deduplication process. The articles were further checked and then removed manually if they had not already been identified by the reference manager software. This was carried out independently by two reviewers (RAB, PW).
Eligibility Criteria
In order to be included in this scoping review, original peer-reviewed articles had to meet three inclusion criteria. First, the study had to be conducted in the United States among the adult MSM population. This criterion was not limited to behavior only; we have included gay and bisexual men in this review. Second, the study had to examine at least one type of stigma and discrimination and have at least one HIV-related outcomes as the dependent variable (e.g., risk of HIV acquisition, HIV medication or treatment adherence, suppression of viral load, linkage to care, and HIV prevention measures such as HIV testing and PrEP use). Third, only peer-reviewed articles written in English that presented original quantitative, qualitative, or mixed methods research were considered. Studies were excluded if any of the above criteria were missing.
Data Charting and Synthesis
Applying the eligibility criteria, the two independent reviewers screened and assessed the articles using a two-step process. In the first step, the reviewers selected the articles based on title and abstract and in the second step they screened the full text of the articles that had been included in the first step. In circumstances where the title/abstract was deemed to not provide sufficient information, the full article was retrieved and examined before a final decision was made. All conflicts and disagreements generated through the screening stages between the two reviewers were discussed until consensus was reached. Furthermore, when needed, a third opinion from the senior author (CY) was consulted to reach unanimity. After the articles were selected, the following data was recorded in a spreadsheet for data extraction and charting: author(s), year, city/region, study purpose, study design (e.g., quantitative, qualitative, or mixed methods), exposure, outcomes measured, and key findings. To ensure accuracy, the same reviewers abstracted the data. We did not perform an assessment of the quality of included studies in align with the methodology of scoping reviews.
Results
Search Results
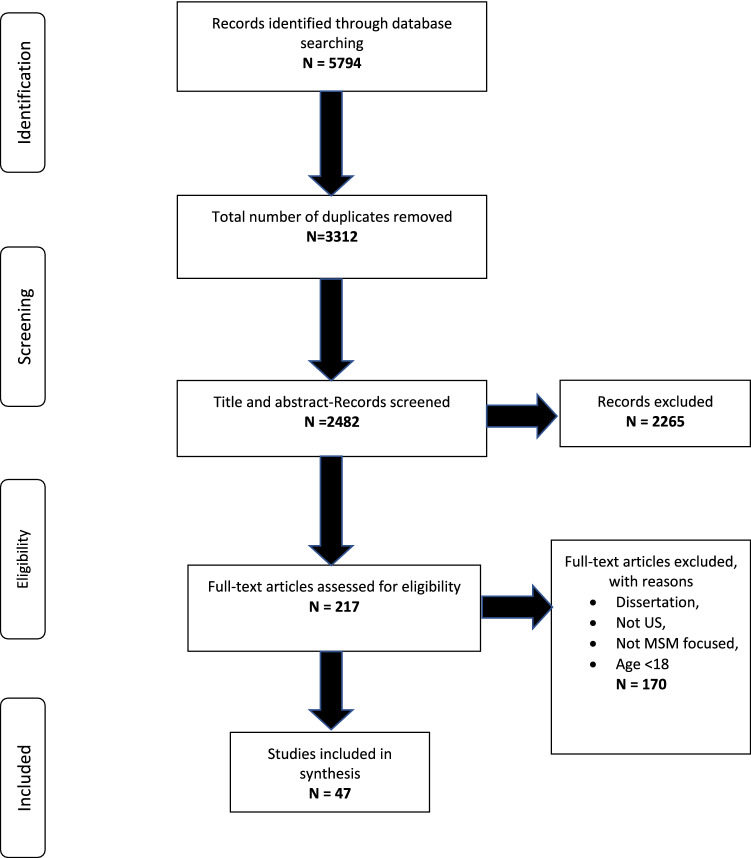
The initial literature search resulted in a total of 5,794 citations from the five electronic databases (PubMed: 1356, CINAHL: 921, Psych Info: 1346, Scopus: 392, and Web Science: 1779). After removing the duplicates, a total of 2,482 records were potentially eligible and were hence screened for title and abstract. Subsequent to this, a full text assessment of 217 articles were performed. The full-text screening led to 47 eligible articles relevant to our scoping review that were included in the final data extraction and further analysis. Figure 1 shows the flow chart of articles examined for this scoping review.
Fig. 1.
Scoping review flow diagram
The results begin with an overall summary of the studies included in the scoping review and then describe the findings related to different types of stigma and its measurements, as well as its association with syndemic conditions, PrEP use, and the HIV care continuum.
Characteristics of Studies
The majority of studies were quantitative (n = 30) [20, 24, 28, 30–56] with the remaining being qualitative studies (n = 16) [25, 57–71]. There was only one study that applied a mixed method study design [27]. Five studies spanned the larger geographical area of the United States, thereby including the 50 states [31, 36, 38, 39, 52]. Most frequently, the studies were conducted in New York City (n = 15) [27, 32, 33, 37, 40, 43, 47, 49, 51, 54, 59, 63, 66, 68, 70], followed by Chicago (n = 6) [35, 37, 48, 57, 58, 69], Los Angeles (n = 6) [25, 30, 34, 37, 51, 61], Boston (n = 5) [20, 37, 46, 51, 56], and San Francisco (n = 4) [27, 28, 37, 51]. Twenty-seven of the quantitative investigations were cross-sectional surveys [24, 28, 30, 31, 33–41, 43–56], and the remaining three were longitudinal studies [20, 32, 42]. Of the seventeen qualitative and mixed method studies [25, 27, 57–71], seven were conducted using focus group discussions [25, 61–64, 67, 68] and the remaining were either in-depth or semi-structured interviews [27, 57–60, 65, 66, 69–71]. Approximately, 85% (n = 40) of all included studies were published in 2010 or later [20, 24, 25, 28, 30–43, 45–54, 56–62, 64, 65, 67, 70, 71].
Fewer studies (n = 14) [20, 27, 30–35, 57–60, 70, 71] were conducted among HIV-positive MSM as compared to HIV-negative MSM (n = 33) [24, 25, 28, 36–56, 61–69]. Only one quantitative [35] and three qualitative studies [58–60] focused exclusively on the effects of stigma among HIV-positive African American MSM. In contrast, one qualitative study [71] focused on HIV-negative Hispanic MSM, while three other studies were conducted on both Hispanic and Black MSM populations [30, 34, 70]. Furthermore, among HIV-negative Black MSM, five quantitative [43, 45, 48, 49, 51] and six qualitative [25, 61, 63, 67–69] studies were conducted, whereas one qualitative study [62] was among Hispanic MSM. Lastly, there was only one quantitative study [41] that included both Black and Hispanic MSM.
Types of Stigma
Both quantitative and qualitative studies of MSM living with HIV showed that internalized, perceived and experienced HIV stigma was associated with increased prevalence of HIV-transmission risk behaviors and poorer self-reported health [20, 27, 30–35, 57–60, 70, 71] (Table 1). Among HIV-negative MSM, the most frequently measured stigma was experienced stigma due to sexual or racial prejudice [37, 38, 40, 41, 43, 48, 53, 55, 56]. Internalized and perceived stigma were less frequently assessed [24, 36, 39, 51], as were structural and healthcare discrimination [42, 44, 45, 47]. These various forms of stigma and discrimination have been shown to be negatively associated with willingness and awareness to use PrEP and engage in HIV testing but positively associated with engagement in high-risk sexual behavior [24, 25, 28, 36–56, 61–69] (Table 2).
Table 1.
Characteristics of studies (HIV positive MSM)
| Author(s) | Year of publication | Location | Aims/purpose | Sample size | Methodology | Exposure (s) | Outcome (s) | Key findings |
|---|---|---|---|---|---|---|---|---|
| Quantitative studies | ||||||||
|
Laura M. Bogart, et al. [30] |
2013 | Los Angeles | 1. To develop a Multiple Discrimination Scale (MDS) for assessment of perceived interpersonal, institutional, and violent forms of discrimination; 2. To explore health correlates of perceived discrimination due to HIV-status, race/ethnicity, and sexual orientation among Black and Latino men who have sex with men (MSM) living with HIV using MDS | 181 Black MSM; 167 Latino MSM | Cross-sectional; audio computer assisted self-interview | MDS: race/ethnicity, sexual orientation, HIV-serostatus | CD4, Viral Load, AIDS-related symptoms, medication side effects, emergency department use | 1. All three discrimination types were significantly correlated with worse physical health outcomes; 2. For Black, racial discrimination has more effects, while for Latino all three are not different; 3. No interaction effects among the different types of discrimination |
|
Mark Hatzenbuehler, et al. [20] |
2011 | Boston | To examine the prospective relationships between experiencing HIV-related stigma and symptoms of anxiety and depression, as well as sexual transmission risk behavior | 314 MSM | Survey, longitudinal follow-up | Perceived HIV stigma | HIV transmission risk behaviors | 1. Perceived HIV stigma led to sexual risk behaviors where perceived fear was uniquely associated with depressive and anxious symptoms and perceived shame was uniquely predictive of HIV risk behaviors |
|
Luke D. Mitzel, et al. [31] |
2015 | USA | To examine the association of HIV related stigma and medication adherence | 66 MSM | Cross-sectional survey | HIV related stigma | Medication adherence | 1. Depressive symptoms mediated the association of HIV-related stigma to medication adherence |
|
H. Jonathon Rendina, et al. [33] |
2012 | NYC | To examine sexual behavior, internalized homonegativity, internalized HIV stigma, and interpersonal HIV stigma in their associations with SC | 127 GBM | Cross-sectional | Number of sexual partners, Internalized homonegativity, Interpersonal and internalized HIV stigma | Sexual compulsivity (SC) | 1. The number of recent male sexual partners and internalized HIV stigma significantly predicted SC symptomology, 2. race was associated with SC symptomology and Black higher |
|
H. Jonathon Rendina, et al. [32] |
2017 | NYC | Explore the role of HIV-related stress within a minority stress model of mental health and condom less anal sex | 136 GBM | Longitudinal study |
Internalized homonegativity, Gay-related rejection sensitivity, Internalized HIV stigma and HIV-related rejection sensitivity |
Condom less anal sex | 1. For both sexual minority and HIV-related stressors, internalized stigma (i.e., internalized homonegativity, internalized HIV stigma) was significantly associated with poorer mental health and increased sexual transmission risk behavior while rejection sensitivity was not |
|
Amy Rock Wohl, et al. [34] |
2011 | LA | To examine the impact of social support, stress, stigma, HIV disclosure on HIV care of African Americans and Latinos | 198 Black and Latino MSM | Cross-sectional | Social support, stigma, stress, HIV disclosure | Retention in HIV care | 1. Stress was associated with retention in HIV care for Black MSM who disclosed their status, but not for Latino MSM; 2. Latino MSM with higher MSM stigma are less likely to be retained in HIV care |
|
Katherine Quinn, et al. [35] |
2017 | Chicago | To examine the association between multiple domains of HIV-related stigma and health-related correlates including viral load and medication adherence | 92 Black YMSM | Baseline survey of RCT | HIV stigma | Medication adherence and viral load; psychological distress; sexual risk; | 1. Total stigma and personalized stigma were significantly negatively associated with viral suppression; 2. Stronger perceptions that people will react negatively to people living with HIV was associated with a higher likelihood of achieving optimal medication adherence |
| Qualitative studies | ||||||||
|
Clare Barrington, et al. [71] |
2019 | North Carolina | To explore the experiences of Latino gay men living with HIV in NC to improve understanding of the factors that shape their HIV care and treatment outcomes, including timely linkage to HIV care, retention in care, and adherence to ART | 14 Latino MSM | Semi-structured interview | Internalized HIV stigma | HIV care and treatment outcomes: Linkage to HIV care, retention in care, and adherence to ART | 1. It is hard for subjects to disclose their HIV status to families; the structures of institutionalized homophobia and clinic policy impede HIV care; 2. HIV care in the US is still a major time and logistical burden for people living with HIV, especially among those who are undocumented |
|
Jason D. P. Bird, et al. [57] |
2017 | Chicago | To identify and explore the potential role of parental rejection on high-risk sexual behaviors among a sample of young, self-identified gay and bisexual men who acquired HIV during adolescence | 21 YGBM | In-depth interviews | Parental rejection | High risk behaviors | 1. The decreased instrumental and emotional support that accompanied parental rejection was related to housing instability, homelessness, poverty, lack of guidance and support, and emotional isolation, and these factors seemed to be potentially linked to their engaging in survival sex or having riskier sexual partnerships |
|
Jason D. P. Bird, et al. [58] |
2013 | Chicago | To better understand how beliefs about and experiences with HIV-related stigma among Black MSM influence HIV disclosure to sexual partners, family, and friends | 20 Black MSM | Semi-structured open-ended interview | HIV stigma | Disclosure | 1. HIV-related stigma is a significant barrier to their discussions with family and friends; 2. Gay communities are not so tolerant to HIV Positive people |
|
Rahwa Haile, et al. [59] |
2011 | NYC | Focusing on the life history narratives on what it means to live with the stigmas of race/ethnicity, HIV status, sexual nonnormativity, and poverty | 10 Black GBM | In-depth interview | Stigmas of race/ethnicity, HIV status, sexual non- normativity, and poverty | Ability to survive with HIV | 1. Stigma were multiple and ubiquitous participants in this study described stigma as an intractable social force that has impeded their ability to survive with HIV and that they needed to subordinate to the broader structure |
|
John B. Jemmott 3rd, et al. [60] |
2019 | Philadelphia | To identify modifiable factors potentially affecting Black MSM's low rates of engagement in HIV care continuum | 27 Black MSM | One-on-one interview | Stigma, concerns about HCP, social support | Low rates of engagement in HIV care continuum | 1. Stigma is the biggest barrier to HIV care continuum; 2. concerns about HCP were most evident in seeking care; 3. social support helps the engagement |
|
Robert H. Remien, et al. [70] |
2015 | NYC | Explore system, social, and individual barriers to and facilitators of engagement in HIV care among HIV-positive African immigrants, previously incarcerated adults, YMSM, and TGW | 20 Black and Latino YMSM | Face to-Face interview | Barriers and Facilitators to Engagement (housing, CBOs, immigration status, healthcare provider, stigma, social support, individual) | Engagement in HIV care | 1. Stigma was a powerful deterrent to entering and staying in HIV care across populations; 2. They wanted providers to make them feel comfortable in sharing their sexual and gender identity and practices and to be knowledgeable to explain treatment options thoroughly and address their concerns |
| Mixed study | ||||||||
|
Cari Courtenay-Quirk, et al. [27] |
2006 | NYC and SF | To describe perceptions of HIV/AIDS stigma among a diverse sample of HIV-positive MSM and to examine whether perceived stigma is related to increased HIV transmission risk behavior, increased substance use, decreased serostatus disclosure, and poorer mental health | 456 MSM | Cross-sectional; semi-structured interview and quantitative survey; | Perceived HIV/AIDS stigma | Sexual risk behaviors, substance use, disclosure of HIV serostatus, mental health | 1. Perceived HIV/AIDS stigma is related to mental health and unrelated to sexual risk behavior; 2. HIV-related stigma was not associated with awareness of HIV serostatus; 3. Those who perceived higher levels of HIV/AIDS stigma in the gay community were more likely to seek partners in settings that facilitate anonymous sex |
Table 2.
Characteristics of studies (HIV negative MSM)
| Author(s) | Year of publication | Location | Aims/purpose | Sample size | Methodology | Exposure (s) | Outcome (s) | Key findings |
|---|---|---|---|---|---|---|---|---|
| Quantitative studies | ||||||||
|
Kaston D. Anderson-Carpenter, et al. [36] |
2019 | All 50 US states, Washington, DC, and Puerto Rico | To examine associations between perceived homophobia, community connectedness, and having a health care provider among men who have sex with men (MSM) | 2281 MSM | Cross-sectional | Perceived Homophobia | Having a regular health care provider | 1. Greater level of perceived community level homophobia were associated with a lower likelihood of having a health care provider |
|
Alexandra B. Balaji, et al. [37] |
2017 | Atlanta, Georgia; Baltimore, Maryland; Boston, Massachusetts; Chicago, Illinois; Dallas, Texas; Denver, Colorado; Detroit, Michigan; Houston, Texas; Los Angeles, California; Miami, Florida; Nassau, New York; Newark, New Jersey; New Orleans, Louisiana; New York City, New York; Philadelphia, Pennsylvania; San Diego, California; San Francisco, California; San Juan, Puerto Rico; Seattle, Washington; and Washington, District of Columbia | To examine the association between measures of enacted stigma (related to sexual minority) and HIV-related risk behaviors | 9819 MSM | Cross-sectional; NHBS | Enacted Stigma: verbal harassment, discrimination, physical assault | HIV-related risk behaviors: CAI at last sex with a male partner of HIV discordant or unknown status and the past 12-month measures of CAI with a male partner, four or more male sexual partners, and exchange sex | 1. A sizable proportion of participants had experienced some form of enacted stigma related to sexual minority status in the past 12 months; 2. Age was strongly related to the risk of victimization (more for younger ones); 3. No association between self-reported HIV status and any of the enacted stigma measures |
|
Abigail W. Batcheldera, et al. [56] |
2020 | Boston, Massachusetts | To examine sexual orientation discrimination and HIV stigma in relation to condom less anal sex among MSM | 382 MSM | Cross-sectional; NHBS | Sexual orientation discrimination, HIV related stigma | Sexual risk (number of condom less anal sex male partners in the past 12 months) | 1. Substance use was associated with health care discrimination and physical assault; 2. Substance use and both forms of discrimination were associated with more condom less anal sex; 3. Hispanic MSM reported more workplace discrimination |
|
Adolph Joseph Delgado, et al. [38] |
2016 | USA | To increase the body of knowledge on the sexual and behavioral health among gay and bisexual servicemen while investigating whether heteronormative roles and expectations led to discrimination and psychological stress. Further analyses were conducted to determine if stress and discrimination that negatively impacted negative health behaviors (i.e., using tobacco, drinking alcohol) and risky sexual behavior (i.e., having casual sex partners) | 85 GB service men | Cross-sectional | Discrimination and psychological stress | Negative health behaviors (i.e., drugs, tobacco, and alcohol) and risky sexual behaviors | 1. Gay and Bi servicemen reported experiencing discrimination more often than straight; 2. Sexual orientation is a significant predictor of tobacco use, alcohol use, and casual sex |
|
Susan A. Fallon, et al. [24] |
2017 | Baltimore | To examine correlates of PrEP awareness and willingness to use PrEP | 399 MSM | Cross-sectional | Discrimination and stigma | PrEP awareness and PrEP use | 1. Black was associated with decreased awareness of PrEP; 2. People who perceived discrimination against HIV were less likely to hear of PrEP but more likely to take it; 3. Perception of HIV intolerance is a barrier for MSM to accessing HIV prevention; 4. HIV-related stigma influence PrEP use |
|
Catherine Finneran, et al. [39] |
2014 | USA | To explore the associations between minority stress and both intimate partner violence and sexual risk-taking | 1575 MSM | Cross-sectional | Internalized homophobia index, homophobic discrimination index, racist discrimination index | Experienced Physical Violence, experienced sexual violence, perpetrated physical violence, perpetrated sexual violence, unprotected anal sex | 1. Minority stress has significant associations with sexual violence; 2. Non-white race, low education, HIV Positive have significant associations with violence and sexual risk; 3. The bidirectional association between perpetration of sexual intimate partner violence and unprotected anal intercourse at last sex; 4. No association of homophobia and HIV risk |
|
Victoria Frye, et al. [40] |
2015 | NYC | To assess the relationship between sexual orientation and race-based experiences of discrimination and sexual HIV risk behavior | 1369 MSM | Cross-sectional | Experience of race- and sexual orientation-based discrimination | HIV acquisition risk behavior, HIV transmission risk behavior | 1. self-reported experience of sexual orientation-based discrimination only within the past 3 months that was significantly associated with sexual HIV acquisition risk behavior; 2. Psychological distress and alcohol and/or drug use before/during last sex, were associated with the outcome, but not internalized homophobia |
|
Tamar Goldenberg, et al. [41] |
2018 | Detroit | To understand and address the social and structural factors influencing HIV/AIDS among Black and Latino YMSM | 334 YMSM | Cross-sectional survey | Perceived community prejudice, internalized homonegativity (IH), experience of sexuality-related discrimination | Three outcomes for HIV testing were examined: testing for HIV in 2012; previously testing for HIV, but not in 2012; and never testing for HIV | 1. Higher perceived sexuality prejudice with higher odds of HIV testing, but not associated with timing since last test; 2. IH was negatively associated with likelihood of testing for HIV; 3. No association between stigma and recency of HIV testing among YMSM who had tested in the past |
|
Michael A. Hoyt, et al. [42] |
2012 | Central Arizona | To investigate relationships between institutional mistrust, HIV risk behaviors, and HIV testing | 394 MSM | Longitudinal study | Institutional Mistrust (systematic discrimination, organizational suspicion, conspiracy beliefs), perceived susceptibility to HIV | Sexual risk behaviors | 1. Perceptions of systematic discrimination were related to lower likelihood of having received HIV testing; 2. Among minority, conspiracy beliefs impact HIV risk behaviors; 3. Higher levels of mistrust are more detrimental to minority MSM, resulting in increased risk-taking behavior, less testing |
|
William L. Jeffries 4th, et al. [43] |
2013 | NYC and Philadelphia | To examine the association of the experience of homophobic and whether social integration level affects the association | 1140 Black MSM | Cross-sectional | Homophobia; social integration | Sexual risk behaviors such as unprotected anal sex | 1. People experienced homophobic events are more likely to have UAI than people did not; 2. For people not diagnosed of HIV positive before, being bullied increases their UAI; 3. For people diagnosed of HIV positive before, all type of homophobic events increase their HIV transmission; 4. Social integration cannot mitigate the association of homophobia and UAI |
|
Leslie E. Kooyman [44] |
2008 |
South USA-Charlotte, North Carolina; Columbia, South Carolina; and, Nashville, Tennessee |
To examine the predictive value of peer norms, self-efficacy, stigma, social support, age, and recreational drug use on high-risk sexual behavior | 576 gay and MSM | Cross-sectional | Stigma | High-risk sexual behaviors | 1. Low peers’ norms for safer sex, low self-efficacy, greater family, and community stigma, being younger in age, and greater drug use do predict higher risk sexual behavior; 2. Predictors might be interrelated |
|
Jessica L. Maksut, et al. [45] |
2018 | Southeast USA |
1. To determine the extent of PrEP awareness among BMSM; 2. to examine whether perceived healthcare-related discrimination, disclosure of same-sex sex behavior to a healthcare provider, and participants’ age were related to PrEP awareness among BMSM; and whether age moderated the relationship between perceived healthcare-related discrimination and PrEP awareness |
147 BMSM | Cross-sectional | Perceived healthcare related discrimination, disclosure of same-sex behavior | PrEP awareness | 1. Perceived healthcare related discrimination was significantly negatively associated with PrEP awareness; 2. Same sex behavior disclosure was significantly positively associated with PrEP awareness; 3. Older BMSM were significantly less aware of PrEP as an HIV prevention strategy than were their younger counterparts; 4. Age moderated the relationship between perceived healthcare related discrimination and PrEP awareness |
|
Henry F Raymond, et al. [28] |
2011 | San Francisco | To examine the association of negative life factors during adolescence and adult HIV status | 521 MSM | Cross-sectional | Adolescent life course negative factors: disconnected, discriminated, harassed, uncomfortable | Adult HIV status | 1. There were high level of ever being harassed, ever being discriminated, and ever feeling disconnected from community and being uncomfortable with sexuality [12-18yrs]; 2. Higher harassment experiences, higher discrimination, and higher discomfort at ages 12–18 are associated with HIV Neg status as adult; 3. Black MSM do not experience more negative life course factors that others |
|
John E. Pachankis, et al. [47] |
2016 | NYC | To investigate migration-related motivations, experiences, health risks | 273 YGBM | Cross-sectional | Hometown characteristics (size, USA or not, structural stigma, discrimination), experiences upon arrival (income, gay density, knew no one in NYC, recently arrived), migration motivations (escape, opportunity, work/school) | HIV transmission risk behavior; heavy drug use; alcohol use; mental health problems | 1. Hometown interpersonal discrimination was strongly related to all assessed health risks, including HIV transmission risk, heavy substance use, alcohol use problems, and mental health problems, although hometown structural stigma climate was associated with lower odds of heavy drug use; 2. There is an inverse association between hometown structural stigma and substance use |
|
Catherine E. Oldenburg, et al. [46] |
2016 | Boston | To assess PrEP awareness, use, and intent to use among those who reported engaging in condom less anal intercourse in the context of stimulant and/or alcohol use | 254 MSM | Cross-sectional | Substance use | PrEP awareness and use | 1. Stimulant-using MSM reported engaging in higher risk sex more often than alcohol-using MSM; 2. For alcohol users, HIV stigma is a limiting factor in PrEP use; 3. Significant association between type of substance used and concern about HIV stigma; 5. Black MSM are more concerned of HIV stigma |
|
Kellie Schueler, et al. [48] |
2019 | Chicago |
1. To characterize HIV-positive index participants and the members of their potential transmission networks; 2. To understand how behavioral factors, PrEP use within networks, and experiences of stigma and community support are associated with awareness and use of PrEP among transmission network members |
218 MSM | Cross-sectional | Stigma, support, HIV status, HIV test, HIV knowledge | PrEP awareness and PrEP use | 1. Individuals who were aware of PrEP were more likely to identify as gay, be highly educated, engaged in health care, and have HIV-related social support; 2. PrEP users were more likely to know other PrEP users |
|
Ja’Nina J. Walker, et al. [49] |
2015 | NYC | To understand the ways in which racial and sexual identities may serve as buffers to risky sexual behavior | 120 Black GBM | Cross-sectional | Racial identities, sexual identities | Risky sexual behavior | 1. Racial identity was associated with sexual risk behavior; 2. There is no association of sexual identity and sexual risk behavior |
|
Jennifer L. Walsh [50] |
2019 | Midwestern US | To explore factors associated with PrEP intentions and use | 476 MSM | Cross-sectional | PrEP knowledge, PrEP attitudes, PrEP stigma, PrEP descriptive norms, PrEP subjective norms, PrEP self-efficacy | PrEP intention and use | 1. Information (PrEP knowledge); motivation (PrEP attitudes, PrEP stigma, and PrEP descriptive norms); and behavioral skills (PrEP self-efficacy) all had associations with PrEP use; 2. PrEP knowledge was directly associated with PrEP use; 3. Latino MSM were less knowledgeable about PrEP than White and Black MSM; 4. Self-efficacy for PrEP use was positively associated with PrEP use and PrEP intention |
|
Sari L Reisner, et al. [52] |
2019 | US | To assess PrEP indication and uptake as a means of primary HIV prevention | 857 trans MSM | Cross-sectional | PrEP awareness, uptake, and persistence | PrEP indications | 1. Majority heard of PrEP, but PrEP uptake was low and PrEP indications were high; 2. Higher perceived HIV risk was found to be associated with increased odds of PrEP indication; 3. Higher partner stigma was associated with increased odds of PrEP indications |
|
Katie Wang, et al. [54] |
2016 | NYC | To investigate associations among gay-related rejection sensitivity, condom use self-efficacy, and condom less anal sex | 63 MSM | Cross-sectional | Gay-related rejection sensitivity, safer sex self-efficacy | Condom less anal sex | 1. Gay related rejection were positively associated with the number of condom less anal sex acts with casual partners; 2. Gay-related rejection sensitivity was associated with lower self-efficacy for condom use, which in turn predicted a higher number of condom less anal sex acts |
|
Erik D. Storholm, et al. [53] |
2019 | Dallas and Houston |
To assess the mediating effects of gay pride/self-esteem, resilience, and social support on the relationship between stressful experiences of racism and homophobia, stimulant use, and sexual risk behavior |
1817 YBMSM | Cross-sectional | Minority stress (experienced homophobia, experienced racism, internalized homophobia) | Sexual risk behavior | 1. Minority stress was significantly and directly associated with sexual risk behavior; 2. Stimulant use was associated with sexual risk behavior; 3. There is no association between minority stress and stimulant use; 4. Minority stress was found to be negatively associated with sources of resilience |
|
Hirokazu Yoshikawa, et al. [55] |
2004 | Northeastern city, USA | To examine the influence of experiences of racism, homophobia, and anti-immigrant discrimination on depressive symptoms and HIV risk | 192 Asian and Pacific Islander MSM | Cross-sectional | Experience of discrimination (racism, homophobia, anti-immigrant discrimination) | Depressive symptoms, HIV risk (UAI) | 1. Experiences of discrimination and conversations about discrimination with family members were somewhat associated with both depression and HIV risk; 2. Conversations with gay friends and with family members about discrimination were associated with lower levels of UAI with primary partners; 3. High levels of discrimination + low levels of conversations with family about discrimination was associated with the highest levels of UAI; 4. Low levels of racism + low levels of family discussions was related to highest levels of secondary-partner UAI |
|
Sharon Mannheimer, et al. [51] |
2014 | Atlanta, GA; Boston, MA; New York, NY; Los Angeles, CA; San Francisco, CA; and Washington, D.C | To assess frequency and correlates of infrequent HIV testing and late diagnosis | 1301 Black MSM | Cross-sectional | Internalized HIV stigma, employment status, housing status, seeing a health care provider | Late HIV diagnosis | 1. Infrequent testing was associated with higher frequency of newly diagnosed HIV infection compared to that among BMSM tested in the prior 12 months and was not associated with lower CD4 or late diagnosis; 2. Unemployment, not seeing health care provider, high internalized HIV stigma are independently associated with infrequent testing |
| Qualitative studies | ||||||||
|
Derek T. Dangerfield li, et al. [61] |
2018 | LA | To inform the development of an intervention for promoting HIV and STI testing, prevention, and treatment | 24 Black MSM | 5 Focus groups | Barriers and facilitators | HIV testing | 1. Fear, stigma and drug use are barriers to HIV testing; 2. Symptoms, new relationships, perceptions of risk, community HIV prevalence and peer navigators are motivations to HIV testing |
|
Joseph P. De Santis, et al. [62] |
2014 | Florida | To describe the relationship of risky sexual behavior, substance abuse, and violence within the cultural context | 20 Latino MSM | Focus group | Roots of risk: acculturation, culture, discrimination, economics, immigration issues, peer influences, unstable intimate relationships | Burden of violence, substance abusers as a buffer, negation of sexual risk | 1. Acculturation to mainstream U.S. culture could be both a risk and protective factor for the acquisition of HIV infection; 2. Internal and external sources of discrimination resulted in stress that was mitigated by high-risk sexual behaviors and substance abuse, and sometimes IPV; 3. Economic factors, unstable intimate relationships and access to psychological support contributed to high-risk sex, substance abuse, and violence |
|
Maria Knight Lapinski, et al. [67] |
2010 | Michigan | To addresses the functional role of stigma in human social systems and the nature of the Down Low phenomenon | 32 for Interviews, Black MSM, 24 for focus group, BMSM, | Interview, focus groups | Stigma | Down low (closet), sexual risk | 1. Organized religion was viewed as a source of expressing stigma around sex and sexuality; 2. Stigma and discrimination are linked to sexual risk behaviors, mainly in health information and information seeking |
|
David J. Malebranche, et al. [68] |
2004 | NY State; Atlanta | To assess healthcare experiences of BMSM and the perceived influence of their race and sexuality on these experiences; (2) perceived barriers to healthcare utilization and (3) factors affecting adherence in this population | 81 BMSM | 8 Focus groups | Racial and sexual prejudice; external barriers (money, insurance, lack confidentiality, impersonal medical system); internal barriers (distrust, fear, discrimination) | Access to medical care | 1. Experiences with societal and institutional racism, and the subsequent expectation of medical racism, impacts how open BMSM are with providers about their sexuality; 2. Internalized displacement makes healthcare access difficult |
|
José Nanín, et al. [63] |
2009 | NYC | To identify participants’ experiences with and attitudes and other factors toward HIV testing | 29 BMSM | Focus group | Fear, stigma, universality of messages, responsibility, sexuality, religion, race and class, knowledge, media influences | HIV Testing | 1. How to overcome barriers to HIV testing: hiring and retention of competent testing personnel, use of more focused, competent, community relevant messages in HIV testing |
|
Jennifer R. Pharr, et al. [64] |
2015 | Nevada | To identify barriers as well as facilitators to HIV testing so as to inform future interventions to increase testing among this group | 11 YMSM | Semi-structured focus group | Barriers: lack of awareness and knowledge, fear, lack of self-esteem, access problems, stigma, unfriendly environment; Facilitators: fear about having HIV, access, friendly environment | HIV Testing | 1. The greatest barrier is lack of awareness and knowledge and the perception of stigma is a major barrier; 2. Friendly environment is important facilitator |
|
Whitney S. Rice, et al. [65] |
2019 | Birmingham, Alabama | To explore perceptions of PrEP access among current and potential PrEP users; to assess the effects of stigma on PrEP uptake an adherence | 44 MSM | Semi-structured interviews | Barriers and facilitators (approachability, acceptability, availability and accommodation, affordability, appropriateness) | PrEP use | 1. Barriers: lack of awareness particularly within communities of color; 2. Facilitators: PrEP-related information gathering and sharing, making PrEP more approachable, social support networks, cost assistance programs, and clinical support staff |
|
Karolynn Siegel, et al. [66] |
1989 | NYC | To explore the motives of gay men for taking or not taking HIV test | 120 MSM | Unstructured focused interviews | Motives | HIV Testing |
To test: 1. To enable medical treatment for HIV infection and to inform sexual decision making; 2. to relieve the psychological distress associated with not knowing HIV status; To not test: 1. To avoid the adverse psychological impact of being positive and to avoid social discrimination |
|
Thomas Alex Washington, et al. [25] |
2015 | LA | To explore the barriers and challenges to HIV testing uptake behavior | 36 Black YMSM | Focus group | Barriers to HIV testing (lack of knowledge for HIV testing; anxiety and substance use; lack of peer support; stigma; perceptions about HIV testing and treatment facilities | HIV testing | 1. Young BMSM are drinking alcohol before and during sex, and as a result having condom less sex; thus, increasing their risk for HIV |
|
Joseph P. Stokes, et al. [69] |
1998 | Atlanta and Chicago | To examine the relationship of negative attitudes toward homosexuality, self-esteem, and risk for HIV | 76 Black MSM | Interview | Homophobia | HIV risk | 1. Fear of being perceived as gay or bisexual can lead some men to avoid showing interest in information about HIV and AIDS or to avoid discussing using condoms |
Intersectional Stigma
Of all the studies reviewed, the theory of intersectionality was explicitly investigated in just one qualitative study [71]. Individual, community and structural determinants among MSM was informed by intersectional stigma in this particular study, which included Hispanic MSM living with HIV. This qualitative study assessed the salient intersections of identities among participants and how their multiple identities shaped HIV testing and treatment experiences. Findings from this study demonstrated that Hispanic MSM who are HIV-positive may find it easier to disclose their sexual orientation to family, friends, and sexual partners than their HIV status, due to both internalized and perceived HIV stigma [71]. Intersecting identities are even discriminated against within gay communities, leading to more social isolation and lesser support. Even though not explicitly investigating intersectional stigma, one of the significant findings of this particular study among HIV negative MSM is worth mentioning. It reported the interaction between enacted stigma and healthcare discrimination resulting in increased substance use and thus resulting in more risky behaviors such as condom less sex [56].
Stigma and Syndemic Conditions
Of the literature available on the interaction of syndemic conditions, six studies examined the relationships between stigma and syndemic conditions [20, 32, 35, 40, 46, 62]. The greater likelihood of sexual risk behavior among MSM can be explained by higher co-occurrence of psychosocial health problems, resulting in increased HIV infection. In a study of HIV negative Hispanic MSM, it was reported that various sexual behaviors and health and social conditions (sexual risk, substance abuse, and violence), which were compounded by heath disparities and social inequalities, increased their risk of HIV exposure [62]. This phenomenon is further intensified among African Americans, where co-occurring conditions like racism, HIV stigma, and substance use increase their risk of infection by acting as a barrier for PrEP adherence [46]. This was supplemented by another study, that reported substance abuse and mental health distress as consequences of sexual orientation-based discrimination, resulting in higher observed sexual risk [40]. Among HIV positive MSM, the stress associated with HIV stigma was one of the fundamental hypothesized and examined syndemic relationships that was considered to drive the HIV epidemic [20, 35]. This was strengthened by findings from a longitudinal study that reported that, internalized HIV stigma along with sexual minority stressor was significantly related with adverse mental health, which ultimately led to an increased risk of transmission [32].
Stigma and PrEP, Care Continuum Outcomes
Among HIV negative MSM, there were a total of 11 studies that assessed the association between stigma and PrEP awareness and use [24, 25, 45, 48, 50, 52, 61, 63–66]. In particular among Black and Hispanic MSM, perceived intolerance against someone with HIV resulted in the knowledge, awareness, and intention to take PrEP among them as being low. This was due to the cultural norms of belonging to a particular race, resulting in reduced visibility and availability of services [24, 50, 65]. In addition, among Black MSM, perceived health-care discrimination as result of race and sexual orientation led to negative awareness about PrEP, thereby, restricting information. However, disclosure of same-sex behavior to healthcare providers (HCP) was positively related to PrEP awareness [45]. Among trans-MSM, although knowledge about PrEP was high, its use was nevertheless low, due to internalized stigma as a result of sexual orientation [52]. Moreover, merely being cognizant about PrEP is not sufficient, its usage is increased if you know other PrEP users or individuals with recent infections in your network, thereby, bridging the gap between them [48]. Besides, major barriers have been noted pertaining to this high-risk population. As compared to young MSM (YMSM, ages 18–29), the awareness about PrEP was lower in older MSM [45]. In YMSM, the perception of HIV related stigma was identified as a formidable barrier to HIV testing [64]. In addition to this, among YMSM of color, other factors that contributed to not getting tested was unfriendly environment at the testing centers attributable to one’s race and lack of support within community [25, 63]. Moreover, lack of knowledge among both MSM and some HCP as they are not comfortable in prescribing PrEP, low awareness about testing, and the psychological impact that the fear of a positive test result might also act as a barrier to HIV prevention measures [61, 66].
Among MSM with HIV, a total of eight studies addressed relationship between stigma and care continuum. Specifically, among older Black MSM in the South or elsewhere, medical care settings that are considered to be a safety net, were themselves a source of stigmatization [58–60]. The ability to manage their illness was impeded if individuals were structurally marginalized by the healthcare organizations. This was predominantly due to lower linkage to care, retention in care, adherence to antiretroviral therapy (ART), and inability to achieve viral suppression. Consequently, individuals usually weaken the care continuum by either missing the stages completely or by exiting the continuum altogether for a period of time. As a result, they revert back to an earlier stage in the HIV treatment cascade due to the fear of stigma and discrimination associated with HIV diagnosis. Since YMSM of color are disproportionately affected by HIV [35, 70], various domains of HIV stigma act differently in relation to care continuum outcomes, for example, internalized HIV stigma was negatively associated with viral load suppression [35] whereas perceived HIV stigma was a deterrent to engagement in care [70]. However, another form of HIV related stigma, disclosure of HIV status, was not found to be associated with either viral load suppression or medication adherence [35]. Depression was found to mediate the association between enacted and anticipated HIV related stigma and adherence to medications, but not between perceived HIV stigma and sexual risk behaviors [20, 31]. As compared to Hispanics, the persistence of discrimination due to race was higher specifically among Blacks, leading to an exacerbation of AIDS-related symptoms [30].
Discussion
The purpose of this review was to examine different types of stigma and how they affect HIV prevention, care, and treatment services among MSM in the United States. As evidenced by this review, HIV vulnerability generated through structural inequalities among MSM is fueled by social stigma and discrimination that influences their behaviors and health outcomes. Thus, the interplay between multiple stigmatized identities can severely intensify the negative detrimental health effects among MSM. Several important factors stood out during this review. First, since the advent of HAART is considered one of the historic achievements, we chose to examine this larger time frame within the context of stigma. While the treatment has definitely improved the prognosis for HIV positive individuals, we wanted to understand whether there were any studies concerning stigma and HIV risks or syndemic conditions in the pre-treatment era. However, we did not find any studies that had been conducted in this regard. Second, the other significant gap that were reported in the literature was the lack of research among YMSM of color. These individuals experience disparities across the HIV care continuum and it has further been demonstrated that stigma impacts the willingness to use PrEP among YMSM regardless of where they live in the US [72]. Perceptions about PrEP use were challenged and determined by societal stigmas such as racism, homophobia, healthcare access along with individual factors such as age and employment. Thus, the disparities in HIV incidence among men of color are further increased due to their inability to discuss PrEP with a healthcare provider and lack of health coverage [73, 74]. As already established in the literature, knowledge about PrEP is directly related to its use and therefore the campaign by CDC about PrEP is very crucial, especially, within the non-White communities. However, while education raises awareness and improve knowledge, it is often not the primary factor in changing behavior. Structural interventions such as increasing access to PrEP and decreasing stigma associated with PrEP uptake/use is far more crucial by decreasing provider-patient stigma, increasing access to easy and free PrEP, and ensuring that those on PrEP are able to stay on PrEP. Therefore, to increase the PrEP care continuum among MSM, multilevel interventions, increased dialogue concerning sexuality and visibility with social groups and community groups are needed.
Third, Southern states have reported disproportionate number of new infections among MSM, however, few studies conducted in this region were focused on stigma. This is surprising, since it has already been established that transmission of HIV is mainly dependent on individual sexual networks and social conditions such as poverty, prejudice, and inequality. Studies have shown that within African American MSM communities, sexual networks are mostly closed and interconnected due to racism such that, if HIV is introduced, it is more likely to be transmitted to a large proportion of other African Americans than to outside groups [75–77]. Our review also revealed that none of these studies included MSM in rural areas, where stigma may be higher than urban areas [78]. In addition, the scant number of studies that have been carried out specifically among Hispanics may not be generalizable because many were conducted using qualitative research methodology. Furthermore, due to a lack of longitudinal studies, our ability to account for temporal ordering; that is, that stigma led to the inability to access components of HIV prevention or treatment services is limited. As most of these quantitative studies were cross-sectional in nature, any associations that have been observed, cannot be considered causal. A mixed-method approach should be employed among this population where participant’s experiences would be grounded in quantitative findings.
Fourth, empirical findings from this study emphasize the need for future research and intervention studies to better understand and address intersectional stigma. Intersectional stigma continues to be a barrier to the uptake of HIV testing and evidence-based prevention interventions. The need to address intersectional stigma has been corroborated by the fact that these already marginalized groups due to one stigma are yet further stigmatized by membership in another stigmatized group based on their serostatus thus further exacerbating negative health outcomes. There is very limited research that has been conducted to understand and analyze intersectional stigma that may drive HIV vulnerability among MSM. Furthermore, interventions designed to address intersectional stigma in order to improve HIV prevention outcomes are notably absent from the literature. There is an urgent need to integrate an intersectionality lens by addressing the multi-level factors that frequently play a role in the experiences of marginalized populations. Science-based dissemination of measurement of intersectional stigma, along with HIV prevention and treatment strategies, would be crucial in mitigating this type of stigma. Future studies should focus more on the intricate co-existence and interactions between different types of stigma and concurrent health conditions.
Finally, the impact of syndemics among MSM on the increased risk for HIV infection have been clearly established as seen in the studies above. While prior work has established the deleterious impact on mental health, stigma not only increases their risk of infection but also has an additive impact on poor antiretroviral uptake, lower medication adherence and viral suppression [19, 79]. Thus, these synergistically acting syndemic factors should not be treated in isolation and instead they should be regularly screened for and treated as an essential step in HIV care continuum. Hence, applying a holistically integrated approach to HIV care among MSM is suggested.
There are several limitations to our scoping review. The scope of the review was restricted to only English peer reviewed based articles, thereby introducing a potential bias by not accounting for relevant studies that would have been published in other languages. We noted the individual study designs as described in the literature, however, as is typical for scoping reviews, we did not intend to assess the quality of the information analyzed. Thus, the conclusions of this review are based on the existence of studies rather than their quality. Due to the limited number of studies, our study was not able to measure the strength of association between one particular type of stigma and one type of HIV outcome. By conducting a scoping review, we intended to answer broader research questions. Our hope is that findings from our review will provide a blueprint for future research on this important topic such as conducing meta-analyses to answer more nuanced and specific research questions while the literature continues to grow. Furthermore, this review provides a comprehensive overview of the existing research on stigma and its associated health outcomes suggesting that research attention to stigma is a field with more attention among MSM in the United States.
Therefore, to address the health disparities among this highly stigmatized populations, an ideal combination of stigma reduction interventions along with TasP would be required. Moreover, interventions will have to be tailored to be culturally specific, suitable, and appropriate to address the critical gap in the care continuum in this population. Finally, existing laws, programs and policies should be evaluated, and evidence-based intervention and policy changes should be made.
Conclusions
Although significant progress has been made in the field of HIV/AIDS, the greatest public health challenge in the fight against the HIV epidemic may still be stigma and discrimination. It is essential to disentangle the stigma associated with risk of acquisition of HIV and prevention efforts. MSM often hold multiple intersecting identities, and the stigma and discrimination they face related to these identities, can impact their health outcomes. Stigmatizing beliefs can severely influence an individual’s decision to seek care and act as a barrier to testing, numerous intervention programs, healthcare access, and treatment adherence. This can lead to severe public health ramifications. There is an urgent need to bridge the gap in programmatic knowledge regarding stigma and the vulnerable risk categories. The integration of different measures of stigma approaches along with psychological and social supports should be incorporated into the national HIV response.
Supplementary Information
Below is the link to the electronic supplementary material.
Acknowledgements
The authors acknowledge the helpful guidance of Yingting Zhang, a research services librarian at the Robert Wood Johnson Library of the Health Sciences for her guidance during the implementation of the search.
Abbreviations
- MSM
Men who have sex with men
- PrEP
Pre-exposure prophylaxis
- TasP
Treatment as prevention
- HIV
Human immunodeficiency virus
- CDC
Centers for disease control and prevention
Author contributions
CY and RAB conceived the paper and developed the search strategy. RAB drafted the manuscript. RAB implemented the search strategy, led the title, abstract, full-text review and data abstraction processes of this article. PW contributed to the title, abstract, and full-text reviews and the data abstraction. All authors (RAB, PW, EJA, HR, CY) critically revised and approved the final version of manuscript.
Declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Crocker J, Major B. Social stigma and self-esteem: the self-protective properties of stigma. Psychol Rev. 1989;96(4):608–630. doi: 10.1037/0033-295X.96.4.608. [DOI] [Google Scholar]
- 2.Crocker J, Major B. The self-protective properties of stigma: evolution of a modern classic. Psychol Inq. 2003;14(3/4):232–237. doi: 10.1207/S15327965PLI1403&4_9. [DOI] [Google Scholar]
- 3.Van Brakel WH. Measuring health-related stigma: a literature review. Psychol Health Med. 2006;11(3):307–334. doi: 10.1080/13548500600595160. [DOI] [PubMed] [Google Scholar]
- 4.Earnshaw VA, Smith LR, Chaudoir SR, Amico KR, Copenhaver MM. HIV stigma mechanisms and well-being among PLWH: a test of the HIV stigma framework. AIDS Behav. 2013;17(5):1785–1795. doi: 10.1007/s10461-013-0437-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Logie C, Gadalla TM. Meta-analysis of health and demographic correlates of stigma towards people living with HIV. AIDS Care. 2009;21(6):742–753. doi: 10.1080/09540120802511877. [DOI] [PubMed] [Google Scholar]
- 6.Phillips KD, Moneyham L, Tavakoli A. Development of an instrument to measure internalized stigma in those with HIV/AIDS. Issues Ment Health Nurs. 2011;32(6):359–366. doi: 10.3109/01612840.2011.575533. [DOI] [PubMed] [Google Scholar]
- 7.Crenshaw K. Demarginalizing the intersection of race and sex: a black feminist critique of antidiscrimination doctrine, feminist theory and antiracist politics. Univ Chic Leg Forum. 1989;140:139–167. [Google Scholar]
- 8.Bowleg L. When Black + Lesbian + Woman ≠ Black Lesbian Woman: the methodological challenges of qualitative and quantitative intersectionality research. Sex Roles. 2008;59(5):312–325. doi: 10.1007/s11199-008-9400-z. [DOI] [Google Scholar]
- 9.Turan JM, Elafros MA, Logie CH, et al. Challenges and opportunities in examining and addressing intersectional stigma and health. BMC Med. 2019;17(1):7. doi: 10.1186/s12916-018-1246-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mahendra VS, Gilborn L, Bharat S, et al. Understanding and measuring AIDS-related stigma in health care settings: a developing country perspective. SAHARA J. 2007;4(2):616–625. doi: 10.1080/17290376.2007.9724883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mahajan AP, Sayles JN, Patel VA, et al. Stigma in the HIV/AIDS epidemic: a review of the literature and recommendations for the way forward. AIDS. 2008;22(Suppl 2):S67–79. doi: 10.1097/01.aids.0000327438.13291.62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ha H, Ross MW, Risser JMH, Nguyen HTM. Measurement of stigma in men who have sex with men in Hanoi, Vietnam: assessment of a homosexuality-related stigma scale. J Sex Transm Dis. 2013;2013:174506. doi: 10.1155/2013/174506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.CDC. Estimated HIV incidence and prevalence in the United States, 2014–2018. HIV Surveillance Supplemental Report 2020.25 (No. 1).
- 14.Dyer TP, Shoptaw S, Guadamuz TE, et al. Application of syndemic theory to black men who have sex with men in the Multicenter AIDS Cohort Study. J Urban Health. 2012;89(4):697–708. doi: 10.1007/s11524-012-9674-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Stall R, Mills TC, Williamson J, et al. Association of co-occurring psychosocial health problems and increased vulnerability to HIV/AIDS among urban men who have sex with men. Am J Public Health. 2003;93(6):939–942. doi: 10.2105/AJPH.93.6.939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Santos G-M, Do T, Beck J, et al. Syndemic conditions associated with increased HIV risk in a global sample of men who have sex with men. Sex Transm Infect. 2014;90(3):250–253. doi: 10.1136/sextrans-2013-051318. [DOI] [PubMed] [Google Scholar]
- 17.Stall R, Friedman M, Catania J. Interacting epidemics and gay men's health: a theory of syndemic production among urban gay men. Unequal Opportunity: Health Disparities Affecting Gay and Bisexual Men in the United States; 2007. pp. 251–274. [Google Scholar]
- 18.Singer M, Clair S. Syndemics and public health: reconceptualizing disease in bio-social context. Med Anthropol Q. 2003;17(4):423–441. doi: 10.1525/maq.2003.17.4.423. [DOI] [PubMed] [Google Scholar]
- 19.Friedman MR, Stall R, Silvestre AJ, et al. Effects of syndemics on HIV viral load and medication adherence in the multicentre AIDS cohort study. AIDS. 2015;29(9):1087–1096. doi: 10.1097/QAD.0000000000000657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hatzenbuehler ML, O'Cleirigh C, Mayer KH, Mimiaga MJ, Safren SA. Prospective associations between HIV-related stigma, transmission risk behaviors, and adverse mental health outcomes in men who have sex with men. Ann Behav Med. 2011;42(2):227–234. doi: 10.1007/s12160-011-9275-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Pachankis JE. A transdiagnostic minority stress treatment approach for gay and bisexual men's syndemic health conditions. Arch Sex Behav. 2015;44(7):1843–1860. doi: 10.1007/s10508-015-0480-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Egan JE, Frye V, Kurtz SP, et al. Migration, neighborhoods, and networks: approaches to understanding how urban environmental conditions affect syndemic adverse health outcomes among gay, bisexual and other men who have sex with men. AIDS Behav. 2011;15(Suppl 1):S35–50. doi: 10.1007/s10461-011-9902-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Granich RM, Gilks CF, Dye C, De Cock KM, Williams BG. Universal voluntary HIV testing with immediate antiretroviral therapy as a strategy for elimination of HIV transmission: a mathematical model. Lancet. 2009;373(9657):48–57. doi: 10.1016/S0140-6736(08)61697-9. [DOI] [PubMed] [Google Scholar]
- 24.Fallon S, Park J, Ogbue C, Flynn C, German D. Awareness and acceptability of pre-exposure HIV prophylaxis among men who have sex with men in Baltimore. AIDS Behav. 2017;21(5):1268–1277. doi: 10.1007/s10461-016-1619-z. [DOI] [PubMed] [Google Scholar]
- 25.Washington TA, D'Anna L, Meyer-Adams N, Malotte CK. From their voices: barriers to HIV testing among black men who have sex with men remain. Healthcare. 2015;3(4):933–947. doi: 10.3390/healthcare3040933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.WHO. Programmatic update: antiretroviral treatment as prevention (TasP) of HIV and TB. 2012.
- 27.Courtenay-Quirk C, Wolitski RJ, Parsons JT, Gomez CA. Is HIV/AIDS stigma dividing the gay community? Perceptions of HIV-positive men who have sex with men. AIDS Educ Prev. 2006;18(1):56–67. doi: 10.1521/aeap.2006.18.1.56. [DOI] [PubMed] [Google Scholar]
- 28.Raymond HF, Chen YH, Stall RD, McFarland W. Adolescent experiences of discrimination, harassment, connectedness to community and comfort with sexual orientation reported by adult men who have sex with men as a predictor of adult HIV status. AIDS Behav. 2011;15(3):550–556. doi: 10.1007/s10461-009-9634-y. [DOI] [PubMed] [Google Scholar]
- 29.Arksey H, O'Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol. 2005;8(1):19–32. doi: 10.1080/1364557032000119616. [DOI] [Google Scholar]
- 30.Bogart LM, Landrine H, Galvan FH, Wagner GJ, Klein DJ. Perceived discrimination and physical health among HIV-positive Black and Latino men who have sex with men. AIDS Behav. 2013;17(4):1431–1441. doi: 10.1007/s10461-012-0397-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Mitzel LD, Vanable PA, Brown JL, Bostwick RA, Sweeney SM, Carey MP. Depressive symptoms mediate the effect of HIV-related stigmatization on medication adherence among HIV-infected men who have sex with men. AIDS Behav. 2015;19(8):1454–1459. doi: 10.1007/s10461-015-1038-6. [DOI] [PubMed] [Google Scholar]
- 32.Rendina HJ, Gamarel KE, Pachankis JE, Ventuneac A, Grov C, Parsons JT. Extending the minority stress model to incorporate HIV-positive gay and bisexual men's experiences: a longitudinal examination of mental health and sexual risk behavior. Ann Behav Med. 2017;51(2):147–158. doi: 10.1007/s12160-016-9822-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Rendina HJ, Golub SA, Grov C, Parsons JT. Stigma and sexual compulsivity in a community-based sample of HIV-positive gay and bisexual men. AIDS Behav. 2012;16(3):741–750. doi: 10.1007/s10461-011-0048-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Wohl AR, Galvan FH, Myers HF, et al. Do social support, stress, disclosure and stigma influence retention in HIV care for Latino and African American men who have sex with men and women? AIDS Behav. 2011;15(6):1098–1110. doi: 10.1007/s10461-010-9833-6. [DOI] [PubMed] [Google Scholar]
- 35.Quinn K, Voisin DR, Bouris A, et al. Multiple dimensions of stigma and health related factors among young black men who have sex with men. AIDS Behav. 2017;21(1):207–216. doi: 10.1007/s10461-016-1439-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Anderson-Carpenter KD, Sauter HM, Luiggi-Hernández JG, Haight PE. Associations between perceived homophobia, community connectedness, and having a primary care provider among gay and bisexual men. Sex Res Social Policy. 2019;16(3):309–316. doi: 10.1007/s13178-018-0347-8. [DOI] [Google Scholar]
- 37.Balaji AB, Bowles KE, Hess KL, Smith JC, Paz-Bailey G. Association between enacted stigma and HIV-related risk behavior among MSM, National HIV behavioral surveillance system, 2011. AIDS Behav. 2017;21(1):227–237. doi: 10.1007/s10461-016-1599-z. [DOI] [PubMed] [Google Scholar]
- 38.Delgado AJ, Gordon D, Schnarrs P. The effect of discrimination and stress on sexual and behavioral health among sexual minority servicemen. J Gay Lesbian Ment Health. 2016;20(3):258–279. doi: 10.1080/19359705.2016.1141344. [DOI] [Google Scholar]
- 39.Finneran C, Stephenson R. Intimate partner violence, minority stress, and sexual risk-taking among US men who have sex with men. J Homosex. 2014;61(2):288–306. doi: 10.1080/00918369.2013.839911. [DOI] [PubMed] [Google Scholar]
- 40.Frye V, Nandi V, Egan J, et al. Sexual orientation- and race-based discrimination and sexual HIV risk behavior among urban MSM. AIDS Behav. 2015;19(2):257–269. doi: 10.1007/s10461-014-0937-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Goldenberg T, Stephenson R, Bauermeister J. Community stigma, internalized homonegativity, enacted stigma, and HIV testing among young men who have sex with men. J Community Psychol. 2018;46(4):515–528. doi: 10.1002/jcop.21957. [DOI] [Google Scholar]
- 42.Hoyt MA, Rubin LR, Nemeroff CJ, Lee J, Huebner DM, Proeschold-Bell RJ. HIV/AIDS-related institutional mistrust among multiethnic men who have sex with men: effects on HIV testing and risk behaviors. J Health Psychol. 2012;31(3):269–277. doi: 10.1037/a0025953. [DOI] [PubMed] [Google Scholar]
- 43.Jeffries W, Marks G, Lauby J, Murrill CS, Millett GA. Homophobia is associated with sexual behavior that increases risk of acquiring and transmitting HIV infection among black men who have sex with men. AIDS Behav. 2013;17(4):1442–1453. doi: 10.1007/s10461-012-0189-y. [DOI] [PubMed] [Google Scholar]
- 44.Kooyman LE. Predictors of high-risk sexual behavior among gay men and men who have sex with men. J LGBT Issues Couns. 2008;2(4):285–307. doi: 10.1080/15538600802501979. [DOI] [Google Scholar]
- 45.Maksut JL, Eaton LA, Siembida EJ, Fabius CD, Bradley AM. Health care discrimination, sex behavior disclosure, and awareness of pre-exposure prophylaxis among Black men who have sex with men. Stigma Health. 2018;3(4):330–337. doi: 10.1037/sah0000102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Oldenburg CE, Mitty JA, Biello KB, et al. Differences in attitudes about HIV pre-exposure prophylaxis use among stimulant versus alcohol using men who have sex with men. AIDS Behav. 2016;20(7):1451–1460. doi: 10.1007/s10461-015-1226-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Pachankis JE, Eldahan AI, Golub SA. New to New York: ecological and psychological predictors of health among recently arrived young adult gay and bisexual urban migrants. Ann Behav Med. 2016;50(5):692–703. doi: 10.1007/s12160-016-9794-8. [DOI] [PubMed] [Google Scholar]
- 48.Schueler K, Ferreira M, Nikolopoulos G, et al. Pre-exposure prophylaxis (PrEP) awareness and use within high HIV transmission networks. AIDS Behav. 2019;23(7):1893–1903. doi: 10.1007/s10461-019-02411-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Walker JJ, Longmire-Avital B, Golub S. Racial and sexual identities as potential buffers to risky sexual behavior for black gay and bisexual emerging adult men. Health Psychol. 2015;34(8):841–846. doi: 10.1037/hea0000187. [DOI] [PubMed] [Google Scholar]
- 50.Walsh JL. Applying the information–motivation–behavioral skills model to understand PrEP intentions and use among men who have sex with men. AIDS Behav. 2019;23(7):1904–1916. doi: 10.1007/s10461-018-2371-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Mannheimer SB, Wang L, Wilton L, et al. Infrequent HIV testing and late HIV diagnosis are common among a cohort of black men who have sex with men in 6 US cities. J Acquir Immune Defic Syndr. 2014;67(4):438–445. doi: 10.1097/QAI.0000000000000334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Reisner SL, Moore CS, Asquith A, et al. High risk and low uptake of pre-exposure prophylaxis to prevent HIV acquisition in a national online sample of transgender men who have sex with men in the United States. J Int AIDS Soc. 2019;22(9):e25391. doi: 10.1002/jia2.25391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Storholm ED, Huang W, Siconolfi DE, et al. Sources of resilience as mediators of the effect of minority stress on stimulant use and sexual risk behavior among young black men who have sex with men. AIDS Behav. 2019;23(12):3384–3395. doi: 10.1007/s10461-019-02572-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Wang K, Pachankis JE. Gay-related rejection sensitivity as a risk factor for condomless sex. AIDS Behav. 2016;20(4):763–767. doi: 10.1007/s10461-015-1224-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Yoshikawa H, Wilson PA, Chae DH, Cheng JF. Do family and friendship networks protect against the influence of discrimination on mental health and HIV risk among Asian and Pacific Islander gay men? AIDS Educ Prev. 2004;16(1):84–100. doi: 10.1521/aeap.16.1.84.27719. [DOI] [PubMed] [Google Scholar]
- 56.Batchelder AW, Klevens M, Fitch C, McKetchnie SM, Mayer KH, O'Cleirigh C. Stigma, discrimination, and substance use among an urban sample men who have sex with men in Massachusetts. AIDS Care. 2020;32(3):370–378. doi: 10.1080/09540121.2019.1683807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Bird JD, LaSala MC, Hidalgo MA, Kuhns LM, Garofalo R. "I had to go to the streets to get love": pathways from parental rejection to HIV risk among young gay and bisexual men. J Homosex. 2017;64(3):321–342. doi: 10.1080/00918369.2016.1179039. [DOI] [PubMed] [Google Scholar]
- 58.Bird JD, Voisin DR. "You're an open target to be abused": a qualitative study of stigma and HIV self-disclosure among Black men who have sex with men. Am J Public Health. 2013;103(12):2193–2199. doi: 10.2105/AJPH.2013.301437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Haile R, Padilla MB, Parker EA. 'Stuck in the quagmire of an HIV ghetto': the meaning of stigma in the lives of older black gay and bisexual men living with HIV in New York City. Cult Health Sex. 2011;13(4):429–442. doi: 10.1080/13691058.2010.537769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Jemmott JB, Zhang JW, Croom M, Icard LD, Rutledge SE, O'Leary A. Barriers and facilitators to engaging african american men who have sex with men in the HIV care continuum: a theory-based qualitative study. J Assoc Nurses AIDS Care. 2019;30(3):352–361. doi: 10.1097/JNC.0000000000000087. [DOI] [PubMed] [Google Scholar]
- 61.Dangerfield Ii DT, Harawa NT, McWells C, Hilliard C, Bluthenthal RN. Exploring the preferences of a culturally congruent, peer-based HIV prevention intervention for black men who have sex with men. Sex Health. 2018;15(5):424–430. doi: 10.1071/SH18057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.De Santis JP, Gonzalez-Guarda R, Provencio-Vasquez E, Deleon DA. The tangled branches (Las Ramas Enredadas): sexual risk, substance abuse, and intimate partner violence among hispanic men who have sex with men. J Transcult Nurs. 2014;25(1):23–32. doi: 10.1177/1043659613504110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Nanin J, Osubu T, Walker J, Powell B, Powell D, Parsons J. "HIV is still real": perceptions of HIV testing and HIV prevention among black men who have sex with men in New York City. Am J Mens Health. 2009;3(2):150–164. doi: 10.1177/1557988308315154. [DOI] [PubMed] [Google Scholar]
- 64.Pharr JR, Lough NL, Ezeanolue EE. Barriers to HIV testing among young men who have sex with men (MSM): experiences from Clark county. Nevada Glob J Health Sci. 2015;8(7):9–17. doi: 10.5539/gjhs.v8n7p9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Rice WS, Stringer KL, Sohail M, et al. Accessing pre-exposure prophylaxis (PrEP): perceptions of current and potential PrEP users in Birmingham, Alabama. AIDS Behav. 2019;23(11):2966–2979. doi: 10.1007/s10461-019-02591-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Siegel K, Levine MP, Brooks C, Kern R. The motives of gay men for taking or not taking the HIV antibody test. Soc Probl. 1989;36(4):368–383. doi: 10.2307/800821. [DOI] [Google Scholar]
- 67.Lapinski MK, Braz ME, Maloney EK. The down low, social stigma, and risky sexual behaviors: insights from African-American men who have sex with men. J Homosex. 2010;57(5):610–633. doi: 10.1080/00918361003712020. [DOI] [PubMed] [Google Scholar]
- 68.Malebranche DJ, Peterson JL, Fullilove RE, Stackhouse RW. Race and sexual identity: perceptions about medical culture and healthcare among black men who have sex with men. J Natl Med Assoc. 2004;96(1):97–107. [PMC free article] [PubMed] [Google Scholar]
- 69.Stokes JP, Peterson JL. Homophobia, self-esteem, and risk for HIV among African American men who have sex with men. AIDS Educ Prev. 1998;10(3):278–292. [PubMed] [Google Scholar]
- 70.Remien RH, Bauman LJ, Mantell JE, et al. Barriers and facilitators to engagement of vulnerable populations in HIV primary care in New York City. J Acquir Immune Defic Syndr. 2015;69(Suppl 1):S16–S24. doi: 10.1097/QAI.0000000000000577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Barrington C, Davis DA, Villa-Torres L, Carcano J, Hightow-Weidman L. Intersectionalities and the HIV continuum of care among gay Latino men living with HIV in North Carolina. Ethn Health. 2019;2019:1–16. doi: 10.1080/13557858.2019.1620177. [DOI] [PubMed] [Google Scholar]
- 72.Quinn K, Bowleg L, Dickson-Gomez J. "The fear of being Black plus the fear of being gay": the effects of intersectional stigma on PrEP use among young Black gay, bisexual, and other men who have sex with men. Soc Sci Med. 2019;232:86–93. doi: 10.1016/j.socscimed.2019.04.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Finlayson T, Cha S, Xia M, et al. Changes in HIV preexposure prophylaxis awareness and use among men who have sex with men - 20 urban areas, 2014 and 2017. MMWR Morb Mortal Wkly Rep. 2019;68(27):597–603. doi: 10.15585/mmwr.mm6827a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Mayer KH, Hosek S, Cohen S, et al. Antiretroviral pre-exposure prophylaxis implementation in the United States: a work in progress. J Int AIDS Soc. 2015;18(4 Suppl 3):19980. doi: 10.7448/IAS.18.4.19980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Friedman SR, Cooper HL, Osborne AH. Structural and social contexts of HIV risk among African Americans. Am J Public Health. 2009;99(6):1002–1008. doi: 10.2105/AJPH.2008.140327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Raymond HF, McFarland W. Racial mixing and HIV risk among men who have sex with men. AIDS Behav. 2009;13(4):630–637. doi: 10.1007/s10461-009-9574-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Bingham TA, Harawa NT, Johnson DF, Secura GM, MacKellar DA, Valleroy LA. The effect of partner characteristics on HIV infection among African American men who have sex with men in the Young Men's Survey, Los Angeles, 1999–2000. AIDS Educ Prev. 2003;15(Suppl 1):39–52. doi: 10.1521/aeap.15.1.5.39.23613. [DOI] [PubMed] [Google Scholar]
- 78.Preston DB, D'Augelli AR, Kassab CD, Starks MT. The relationship of stigma to the sexual risk behavior of rural men who have sex with men. AIDS Educ Prev. 2007;19(3):218–230. doi: 10.1521/aeap.2007.19.3.218. [DOI] [PubMed] [Google Scholar]
- 79.Blashill AJ, Bedoya CA, Mayer KH, et al. Psychosocial syndemics are additively associated with worse ART adherence in HIV-infected individuals. AIDS Behav. 2015;19(6):981–986. doi: 10.1007/s10461-014-0925-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.