Abstract
Background
Ramifications of coronavirus disease 2019 (COVID-19) on the re-structuring of healthcare are widespread, including delivery of surgical services across all specialties, including plastic surgery. Re-deployment of personnel and cessation of elective services are commonplace. However, there is a continued need for both emergency and oncological surgery. A national review of practice was conducted during the COVID-19 pandemic, to assess impact on services, staffing and training.
Methods
Key aspects of current plastic surgery practice in the United Kingdom were examined in this cross-sectional study; operating capacity, location of theatre lists (national health service or outsourced private institutions (PIs)), differences across sub-specialties, change in anaesthesia practices, staffing, re-deployment, on-call provision and impact on training.
Results
Three-hundred and forty-four plastic surgeons in the United Kingdom provided practice data across 51 units. Theatre capacity and outpatient services were markedly reduced. Outsourcing of operating lists to PIs was widely utilised. Increased use of local anaesthetic hand procedures, the prioritisation of shorter operations with reduced microsurgery in both head and neck/lower limb and almost complete cessation of breast reconstruction were noted, together with marked regional variations. Re-deployment occurred at all staffing levels, whilst telemedicine played a critical role in both patient management and training.
Conclusions
COVID-19 has enforced unprecedented changes to surgical care delivery and training, as identified by examination of plastic surgery nationally in the United Kingdom. Novel means to support continued elective and emergency services, including oncology have been identified. Lessons learned will allow phased return of services and improved preparation for the future.
Background
At the time of writing, severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) has been responsible for 105,394,301 confirmed cases of coronavirus disease 2019 (COVID-19).1 Of these, 3929,839 have been confirmed in the United Kingdom alone2. Entering into the realm of a pandemic3 has had global consequences for healthcare delivery. An immediate need for equipment and personnel on the frontline4 has directly impacted on the delivery of previously established surgical services. Plastic surgery is not unique in this domain. Re-deployment of surgical staff5 (of any grade), reduction or cessation of elective services and novel provisions for time-critical surgery (including cancer or trauma) are widespread.6
The impact on patients and healthcare professionals must be ascertained. The reasons for this are numerous and include the need to provide a unified speciality response during the current pandemic (including potential re-introduction of services), the effects on staffing and training, but perhaps most importantly, planning the future of the speciality including its preparation for global events.
Plastic surgery is unique in being surgically broad. However, during this time, many units have been forced to re-evaluate services, separating essential from desirable activity. Where surgery cannot be delayed, logistical challenges may exist with respect to theatre and staff availability. Combined with national guidance towards shorter operations, the gold-standard of microvascular free flap reconstructions across all sub-specialties may have been directly impacted.
To further delineate the effect on plastic surgery in the United Kingdom, a novel questionnaire was distributed in association with BAPRAS (British Association of Plastic Reconstructive and Aesthetic Surgeons) to all members within the United Kingdom. Furthermore, we reviewed updated COVID-19 guidelines across all sub-specialties, comparing this to current practice.
Methods
An electronic questionnaire was designed to specifically focus on key areas of plastic surgery service delivery. This survey was conducted over a 3-week period in May 2020. Basic demographic data were collated to include grade of responder and base unit.
Current number and location of operating lists (across both National Health Service(NHS)/private hospitals and specifically for sub-specialties including hand, skin, breast, lower limb, head and neck), type of anaesthesia, theatre utilisation, changes in reconstructive options utilised, management of outpatients, re-deployment of staffing, changes in emergency service provision, use of information technology services and teaching were all evaluated. Any clinician reporting themselves to be shielding at this time was recorded.
Data were collated and statistical analysis performed using Stata 15.1 (Timberlake Consultants Limited, London, UK). Descriptive statistics were used to report patterns across units and sub-specialties. We assumed the rates within regions to have a Poisson distribution and used a test for overdispersion (heterogeneity) to examine whether regional differences were statistically significant. Updated guidelines from national plastic surgery bodies and sub-specialties were accessed for comparison against results.
Results
In total, 344 individuals responded across the United Kingdom. From these, 124 responses were removed for inadequate completion (81), no unit information15 and shielding (28). Of the remaining 220 responses, these represented a total of 63 plastic surgery units. A further 35 questionnaires contained information only on hand trauma and once removed the final data set represented 185 responses from 51 units. Of the 185 included responses, 142 were consultant (attending) level and 43 were trainee level (Specialist Registrar/resident or equivalent)."?>
Theatre capacity
From 51 units, 46 (90%) reported reduced capacity and 5 (10%) no capacity. Reasons for reduced capacity (from 41 responses) included conversion to COVID-19 theatre (15 units, 37%), anaesthetic capacity (10 units, 24%) and theatre staffing capacity (8 units, 20%) and combinations of all (8 units, 20%).
Outpatient clinics
Elective clinics were reported as normal,4 restricted (37), not running7 with the nature of these clinics either face-to-face,6 telephone (30), virtual15 or a combination of all.5 Hand clinics were reported as restricted,15 normal,27 not running,8 with clinic frequency per week of 1–5,22 7(12), >8.7
COVID-19 staffing levels
Staff were re-deployed in 38 of 51 units. This was reported as senior house officer (SHO) (6 units, 12%), SHO and nursing staff only (13 units, 25%), resident Registrars, SHO and nursing (7 units, 14%), all levels of staff (5 units, 10%) and other (7 units, 14%). Only 13 units (25%) reported no re-deployment. Location of re-deployment was equally distributed between urgent care centres, COVID-19 wards, medical wards, intensive care unit staffing and proning teams.
On-call service provision was as follows: none (4 units, 8%), consultant Attending only (5 units, 10%), Attending and Resident consultant and registrar (17 units, 33%), Attending, Resident consultant, registrar and SHO (16 units, 31%) and no change (9 units, 18%). Whilst some inter-unit variability exists, on-call-services were defined as on-site shift-pattern SHO (day and night) supported by non-resident registrar and consultant out of hours.
Information technology support
All units reported benefit from IT support during the time of COVID-19. This was relatively equally distributed between telemedicine (42), teaching (41), Microsoft teams (35) and a combination of all these.25
Trainee responses
Of the 43 trainees who responded, 31 provided meaningful data, 22.5% had been re-deployed whilst the remainder had not. Concerns over training issues were expressed by 81%, in particular indicative logbook numbers alone (32%) and also combined with work-based assessments (48%). Only 10% reported having no concerns.
Sub-speciality data across the United Kingdom
Hand trauma
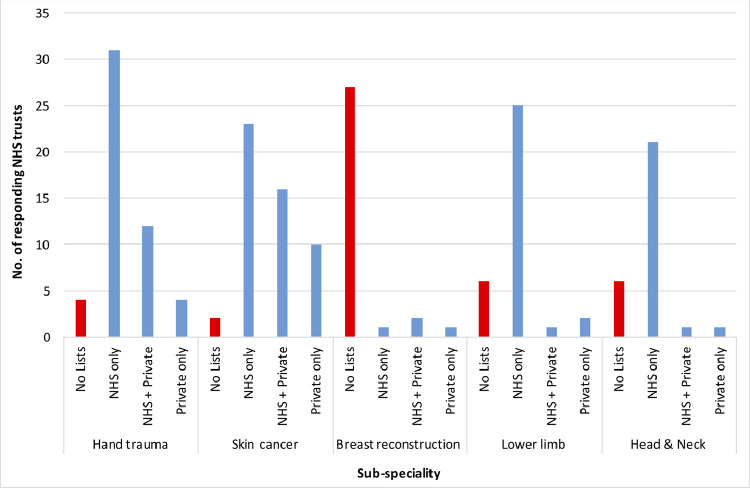
Forty-seven of 51 units continued provision of a hand trauma service. The location of these lists was split between NHS (31 units, 66%), NHS and private institution (PI) (12 units, 26%) and PI only (4 units, 9%) across units (Graph 1 ).
Graph 1.
Location of operating lists across NHS hospitals and PIs.
The majority of units (43/50) confirmed paediatric trauma was still taking place, although a significant shift was seen in the location of these lists to adult emergency theatres (59 and 41% in adult and paediatric theatres, respectively).
Seventy-four percent of units reported local anaesthetic or WALANT techniques were the most common anaesthetic type used, versus regional and general anaesthesia (15% and 11% of units, respectively).
Hand trauma theatres were the most commonly reported location for cases (13 units, 30%), followed by local procedure rooms (12 units, 28%), emergency departments (9 units, 21%) and CEPOD (9 units, 21%).
Skin cancer
Of 51 responding units, all but two reported continued provision of a skin cancer service. The location of these lists was split between NHS (23 units, 47%), NHS and PI (16 units, 33%) and PI only (10 units, 20%; Graph 1). As a relative proportion of work undertaken, a larger volume of skin cancer operating was completed in PIs relative to other sub-specialties, although predominantly still being performed by NHS teams. With regards to management of nodal basins, 25 units (50%) were still performing sentinel node biopsy and 37 (74%) were still carrying out axillary dissections. Of those who felt able to comment, 88% reported meeting the 2-week wait cancer pathway criteria.
Microsurgical sub-specialties
Breast reconstruction
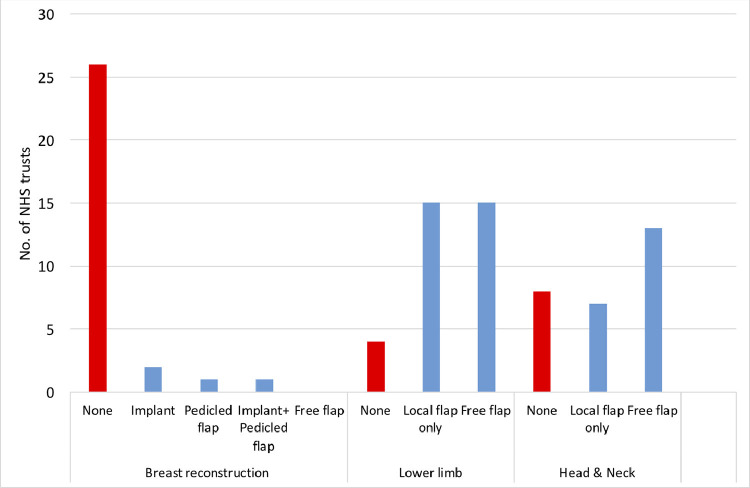
Of the 34 units usually performing breast reconstruction, only 4 units in the United Kingdom provided any form of reconstruction during COVID-19, with single figure cases of implant only, pedicled flap only and a combination of both (Graph 2 ). Most units did not offer reconstruction (none, n = 26), with patients undergoing mastectomy only or stabilising patients on endocrine treatment. Operating lists were equally distributed across the NHS and PI sector (Graph 1).
Graph 2.
Reconstruction types by sub-speciality.
Lower limb reconstruction
Of the 34 units that normally perform lower limb reconstruction, 4 (12%) reported no available lists, 15 (44%) performed vacuum-assisted closure (VAC)/local flaps only and 15 (44%) a variety of reconstructive options including free flaps (Graph 2). Within the free flap cohort, 14 units reported 1–2 flaps a week and a single unit 3–4 a week. Almost all reconstructions were carried out in NHS hospitals (89%, Graph 1). A significant majority (81%) accepted that during COVID, shorter operations had been prioritised with potentially lesser outcomes (22 v 5 units).
Head and neck reconstruction
Of the 29 units that normally perform head and neck reconstruction, 8 (28%) were not performing reconstructions, 7 (24%) performed only local flaps and 13 units (38%) carried out free flaps (45%, all reporting 1–2 a week) (Graph 2). Almost all reconstructions were performed in NHS hospitals (91%). A significant majority (72%) accepted that during COVID, shorter operations had been prioritised with potentially lesser outcomes (13 v 5 units).
Comparison of regional data across the United Kingdom
No correlation was noted between the unit size (represented by the number of consultants) and the mean number of lists per week at the time of this study, representing the effect of COVID-19 on unit capacity.
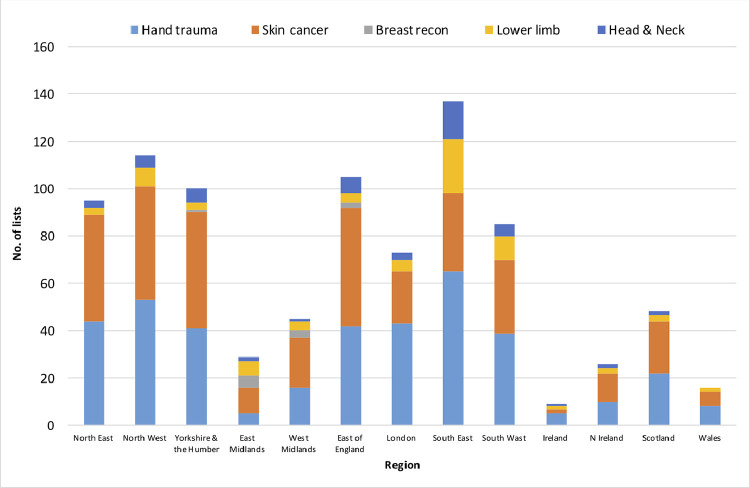
A breakdown of caseload by sub-speciality across UK regions is shown (Graph 3 ), emphasising bulk of operating capacity across hand trauma and skin cancer, with lower numbers for head and neck, lower limb reconstruction and extremely limited breast reconstruction.
Graph 3.
Sub-speciality regional variation across UK regions.
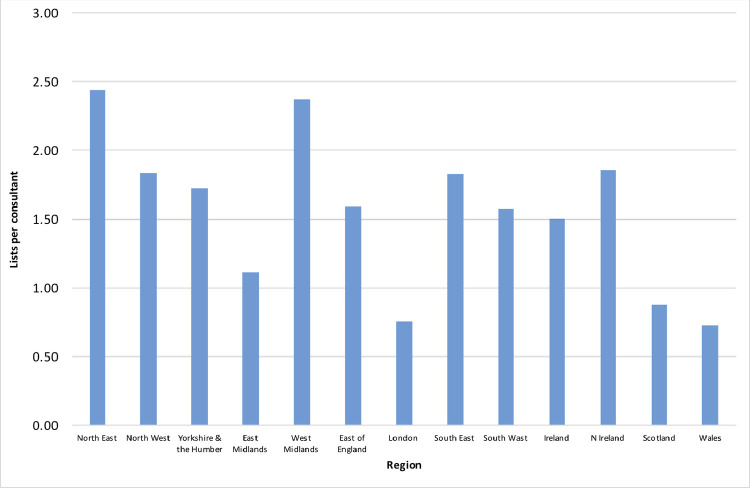
To further compare regional data, the mean number of lists per consultant was extracted based on the total number of lists and consultants per unit across the region. This information is shown in Graph 4 and reveals differences between regions were statistically significant (test for overdispersion, p < 0.001).
Graph 4.
Mean number of lists per consultant per week, across UK regions.
Review of current guidance across the United Kingdom
At the time of this study, the most up to date national COVID-19 guidelines across all plastic surgery sub-specialties were reviewed. A summary of this is presented in Table 1 .
Table 1.
National body COVID-19 guidance in plastic surgery. Published national guidelines for surgical management during COVID-19.
| Sub-speciality | National body | Advice |
|---|---|---|
| Hand trauma7 | BOA, OTS, BSSH, BAPRAS, BAHT, BSCOS | Non-operative management wherever possible, local anaesthetic surgery and use of outpatient or procedure room facilities |
| Skin cancer8, 9, 10 | BAPRAS, BAD | -Defer excision of low-risk lesions (basal cell carcinoma (BCC), melanoma in-situ and some squamous cell carcinoma (SCC)) -Standard excision of high risk SCC and melanoma -Individual decisions on sentinel lymph node biopsy acknowledging capacity for this may reduce |
| Head and neck cancer11 | BAHNO | -Day case surgery where feasible -Reduce procedures requiring HDU/ITU -Reduce length of surgery (local flaps versus free flaps) |
| Lower limb (BOAST)7 | BOA, OTS, BSSH, BAPRAS, BAHT, BSCOS | -Consider alternative reconstruction to avoid multiple operations and critical care input -Consider early amputation if limb salvage uncertain |
| Breast12 | ABS | -No immediate breast reconstruction. Consider local flaps/oncoplastic techniques. |
BOA – British Orthopaedic Association; OTS – Orthopaedic Trauma Society; BSSH – The British Society for Surgery of the Hand; British Association of Plastic, Reconstructive and Aesthetic Surgeons; BAHT – The British Association of Hand Therapists; BSCOS – British Society for Children's Orthopaedic Surgery; BAD – British Association of Dermatologists; BAHNO – British Association of Head and Neck Oncologists; ABS – Association of Breast Surgery.
Discussion
Exponential rise in worldwide community and hospital infections secondary to COVID-193 , 13 , 14 has resulted in unprecedented challenges for healthcare service delivery. Plastic surgery services, in line with many other surgical specialties, have been significantly affected.
This study has examined the national effect on an entire speciality and demonstrated severe restrictions in operating capacity, cross-level re-deployment, modified outpatient services and marked changes in reconstructive practices across all sub-specialties. Novel strategies to combat this have included outsourcing of lists to PIs, most significantly in day-case surgery such as hand trauma and skin cancer. Outpatient management has been largely telephone or virtual-based. Absence of clinical examination may limit decisions on future management. However, it appears patients requiring immediate treatment (oncology or acute trauma) have continued to be seen. A testament to this is the high proportion (88%) who reported meeting the 2-week wait targets in skin cancer. Considering specific sub-specialties, significant logistical and intra-operative changes were implemented to allow continuation of urgent work.
Hand trauma and skin cancer
In hand trauma, a huge shift to local anaesthetic/wide awake local anaesthesia no tourniquet (WALANT) was demonstrated (74% of all cases), in parallel to increased procedure-room (versus formal theatre) operating. Injuries traditionally deemed to require theatre utilisation have been safely treated in this manner. Advocates of WALANT15 , 16 would suggest this to be best practice even in non-pandemic times. However, long-term data on patient outcomes are required with comparison of non-COVID-matched cohorts.
Within this study, only 50% of UK units were currently performing sentinel node biopsy for cutaneous malignancy. Given the extensive published trial data17 , 18 showing prognostic benefit, outcomes from this time period will provide opportunity to re-evaluate the importance of these adjunctive procedures. The relatively high number of units performing ongoing nodal dissection (74%) may represent small cohorts with advanced disease and the need for local surgical control.
Microsurgical sub-specialties and free flap reconstruction
Of the microsurgical sub-specialties, breast reconstruction was most impacted during the COVID-19 outbreak. A total number of lists were nationally low, with only single cases of implant-based reconstruction and pedicled flaps, the majority being treated by mastectomy only. No free flap reconstructions were being performed.
Globally, increasing numbers of patients have been stabilised on endocrine treatment, with a view to carrying out mastectomy with or without reconstruction at a later date.19 This will generate expanding waiting lists for both immediate and delayed reconstruction, with associated logistical and financial implications. These concerns are not unique to plastic surgery and many healthcare institutions globally will be met with similar dilemmas.
Considering other microsurgical sub-specialties, lower limb and head and neck practices appear to be continuing, albeit at reduced capacity. The modal response was for 1–2 operating lists per week across both sub-specialties, with the majority in NHS institutions. However, reconstructive practices favoured increased use of local options (including pedicled flaps and grafts), with a majority prioritising shorter operations. In total, 15 (of 34) units were still performing free flaps in lower limb and 13 (of 29) units for head and neck. The net result of this in terms of functional and (to a lesser extent) aesthetic outcomes remains to be seen; high numbers requiring revisional surgery or late spikes in extremity deep infections may be of concern.
Regional data in the United Kingdom
Regional comparisons identified numerous key factors. Large centres did not necessarily have more theatre capacity, perhaps a reflection on increased conversion of these units to COVID-19 medical hubs. There was significant regional variation in the numbers of lists and sub-speciality activity (Figure 3). A large proportion of lists were devoted to hand trauma and skin cancer, a reflection on both volume of work, access to lists (including at PIs) and the ability for local anaesthetic operating. Standardising regions by number of lists per consultant per week demonstrated that high population areas (such as London; with correspondingly high incidence of COVID-19 infections) were most affected in terms of operating capacity (Figure 4).
Staffing, re-deployment and training
Almost all units experienced re-deployment of personnel at all grades. This directly impacted trainees in particular, who expressed concern regarding indicative numbers required for progression and the ability to complete work-based assessments. This may also be a reflection on increased consultant-led operating during this time period combined with reduced operative exposure.
With the likelihood of ongoing waves in the current pandemic, the imminent return to ‘normal’ levels of surgical activity is doubtful. Furthermore, the need to prioritise patient and staff health may result in further paired Consultant operating. Net results are likely to be negative for training within not only plastic surgery but across all specialities. This may necessitate re-evaluation of required competencies for completion of training and perhaps also extension of training time.
Information technology clearly has a critical role to play during a pandemic; both in-patient care and for training healthcare professionals where usual clinical bedside or operative opportunities are lacking. Many institutions have reported on the use of telemedicine for triage (emergency and surgical)20 , 21 and outpatient services whilst online webinars have proved critical for ongoing education at all staff levels across a multitude of specialties.22 Our own data confirmed widespread use of IT support (>80% of units), including telemedicine, Microsoft Teams or combinations of these.
Conclusion
A clear need has been identified for future proofing in the event of ongoing or new global healthcare crises. Increased staff training, preparation of pandemic response plans and dedicated theatres or hospitals for infected individuals have been suggested as potential strategies.6 , 23 Protocols for parallel continuation of clean surgery may be critical for maintaining standards of care in elective work,24 including the potential use of ambulatory surgical centres.25 These are likely to be fundamental to the reintroduction of elective surgery after an initial blanket ban proposed by national organisations.26 Regular review of outcomes is required, particularly given early data suggesting higher post-operative pulmonary complications and mortality in COVID-positive patients.27
This study has identified the response of plastic surgery as a speciality in the United Kingdom to a pandemic, which is likely to readily translate to other specialities and countries worldwide. It remains to be seen whether the delivery of plastic surgery services in the United Kingdom, or indeed globally, will return to pre COVID-19 levels. Microsurgical reconstruction, particularly the use of free flaps across all sub-specialties but especially breast reconstruction, has been greatly impacted. However, resilience has been demonstrated by the adaptation of limited resources to continue to care for the acute needs of our patients. Despite a pandemic, services for urgent oncology and acute trauma have continued to operate.
Ongoing re-evaluation of surgical systems and patient outcomes is critical across all specialties at numerous time-points both during and post-crisis, as data such as our own provides only a single temporal window of the impact of COVID-19.
Perhaps as a speciality, profession and a nation, we will feel better prepared for a future global health crisis. For now, the situation is fluid and we must continue to adapt to ensure we can continue to meet the needs of our patients and staff alike.
Ethical approval
Not required.
Declaration of Competing Interest
None.
Acknowledgements
We thank Ms J Medina and Prof D Cromwell of the Clinical Effectiveness Unit, Royal College of Surgeons of England for their support with analysing the survey results. We would also like to thank the British Association of Plastic Reconstructive and Aesthetic Surgeons (BAPRAS) for distribution of the survey and collection of data, in particular Gemma Adlington (secretariat), Mr Mark Henley (President) and the BAPRAS council.
Footnotes
Presented: Not previously presented.
Funding: none.
References
- 1.World Health Organisation. WHO Coronavirus Disease (COVID-19) Dashboard [Internet]. 2020. Available from: https://covid19.who.int
- 2.World Health Organisation. COVID-19 [Internet]. 2020. Available from: https://covid19.who.int/region/euro/country/gb
- 3.Callaway E. Time to use the p-word? Coronavirus enters a dangerous new phase. Nature. 2020;579(12):10. doi: 10.1038/d41586-020-00551-1. 10o/ [DOI] [PubMed] [Google Scholar]
- 4.Taub P.J. Plastic Surgeons in the Time of a Pandemicmic a dangerous new phase. Nature. 2020;579(12):10–38. country/g. [Google Scholar]
- 5.Sarpong N., Forrester L., Levine W.N. Whathat Pandemicmic a dangerous new phase.opaedic surgeon during the COVID-19 pandemic: perspectives from the trenches. J Bone Jt Surg Am. 2020;102(12) doi: 10.2106/JBJS.20.00574. 1010010nu. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Brindle M., Gawande A. Managing COVIDVIDhat Pandemicmic a dangerous new phase.opaedic surg
- 7.British Orthopaedic Association Standards for Trauma and Orthopaedics. Management of patients with urgent orthopaedic conditions and trauma during the coronavirus pandemic [Internet]. 2020 [cited 2020 Jun 22]. Available from: https://www.boa.ac.uk/uploads/assets/ee39d8a8-9457-4533-9774e973c835246d/4e3170c2-d85f-4162-a32500f54b1e3b1f/COVID-19-BOASTs-Combined-FINAL.pdf
- 8.British Association of Plastic, Reconstructive and Aesthetic Surgeons. Advice for managing BCC & SCC patients during Coronavirus pandemic [Internet]. 2020 [cited 2020 Jun 22]. Available from: http://www.bapras.org.uk/docs/default-source/covid-19-docs/coronavirus-bcc-scc-revision.pdf?sfvrsn=2
- 9.British Association of Plastic, Reconstructive and Aesthetic Surgeons. Advice for managing Melanoma patients during Coronavirus pandemic. [Internet]. 2020 [cited 2020 Jun 22]. Available from: http://www.bapras.org.uk/docs/default-source/covid-19-docs/corona-virus-melanoma-final-version-2.pdf?sfvrsn=2
- 10.British Association of Dermatologists and British Society for Dermatological Surgery. COVID-19 - Skin cancer surgery guidance [Internet]. 2020 [cited 2020 Jun 22]. Available from: https://www.bad.org.uk/shared/get-file.ashx?itemtype=document&id=6670
- 11.British Association of Head and Neck Oncologists. BAHNO Statement on Covid-19 [Internet]. 2020 [cited 2020 Jun 22]. Available from: https://www.bahno.org.uk/bahno_statement_on_covid-19.aspx
- 12.Association of Breast Surgery. Statement from the Association of Breast Surgery [Internet]. 2020 [cited 2020 Jun 22]. Available from: https://associationofbreastsurgery.org.uk/media/252009/abs-statement-150320-v2.pdf
- 13.Zhu N., Zhang D., Wang W., Li X., Yang B., Song J., et al. A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med. 2020;382(8):727. doi: 10.1056/NEJMoa2001017. 727a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Guan W., Ni Z., Hu Y., Liang W., Ou C., He J., et al. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020;382(18):1708–1720. doi: 10.1056/NEJMoa2002032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lalonde D. Wide-awake flexor tendon repair. Plast Reconstr Surg. 2009;123(2):623. doi: 10.1097/PRS.0b013e318195664c. 623. [DOI] [PubMed] [Google Scholar]
- 16.Lalonde D., Tang J. How the wide awake tourniquet-free approach is changing hand surgery in most countries of the world. Hand Clin. 2020;35(1):xiii–xxiv. doi: 10.1016/j.hcl.2018.10.001. [DOI] [PubMed] [Google Scholar]
- 17.Morton D.L., Elashoff R., Hoekstra H.J., Coventry B.J. Sentinel-node biopsy or nodal observation in melanoma. N Engl J Med. 2006;35(13) doi: 10.1056/NEJMoa060992. [DOI] [PubMed] [Google Scholar]
- 18.Ribero S., Osella-Abate S., Sanlorenzo M., Balagna E., Senetta R., Fierro M.T., et al. Sentinel lymph node biopsy in thick-melanoma patients (N=350): what is its prognostic role? Ann Surg Oncol. 2015;22(6) doi: 10.1245/s10434-014-4211-7. [DOI] [PubMed] [Google Scholar]
- 19.Spring L., Specht M., Jiminez R., Isakoff S., Wang G.X., Ly A., et al. Case 22-2020: a 62-year-old woman with early breast cancer during the Covid-19 pandemic. N Engl J Med. 2020 doi: 10.1056/NEJMcpc2002422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Argenziano M., Fischkoff K., Smith C. Surgery scheduling in a crisis. N Engl J Med. 2020;382(23):e87. doi: 10.1056/NEJMc2017424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hollander J., Carr B. Virtually perfect? Telemedicine for COVID-19. N Engl J Med. 2020;382(18) doi: 10.1056/NEJMp2003539. [DOI] [PubMed] [Google Scholar]
- 22.Ali S., Dobbs T., Whitaker I. Webinars in plastic and reconstructive surgery training-a review of the current landscape during the COVID-19 pandemic. J Plast Reconstr Aesthet Surg. 2020;73(7) doi: 10.1016/j.bjps.2020.05.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.COVIDSurg Collaborative. Global guidance for surgical care during the COVIDOVIDning-a review of the curren
- 24.Myles P.S., Maswime S. Mitigating the risks of surgery during the COVID-19 pandemic. Lancet. 2020;396(10243):23. doi: 10.1016/S0140-6736(20)31256-3. 2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Squitieri L., Chung K. Surviving the Covid-19 pandemic: surge capacity planning for non-emergent surgery. Plast Reconstr Surg. 2020 doi: 10.1097/PRS.0000000000007075. PRS Online First. [DOI] [PubMed] [Google Scholar]
- 26.Iacobucci G. Covid-19: all non-urgent elective surgery is suspended for at least three months in England. BMJ. 2020:m1106. doi: 10.1136/bmj.m1106. [DOI] [PubMed] [Google Scholar]
- 27.COVIDSurg Collaborative Mortality and pulmonary complications in patients undergoing surgery with perioperative SARS-CoV-2 infection: an international cohort study. Lancet. 2020;396(10243):27–38. doi: 10.1016/S0140-6736(20)31182-X. [DOI] [PMC free article] [PubMed] [Google Scholar]