Abstract
Background:
Spinal hemangioblastomas account for 1–3% of all spinal cord tumors and are mostly intramedullary in location. Here, we report an intradural extramedullary hemangioblastoma of the thoracic spine, occurring in in a patient without von Hippel-Lindau disease.
Case Description:
A 58-year-old female had a 5-year history of progressive left lower extremity weakness. When the MR demonstrated an intradural/extramedullary lesion with a syrinx at the T2-3 level, she successfully underwent gross total tumor excision following which she neurologically improved.
Conclusion:
Here, we report a rare case of an intradural/extramedullary thoracic hemangioblastoma successfully excised at the T 2-3 level in a patient without von Hippel-Lindau disease.
Keywords: Cyst, Extramedullary spinal tumor, Hemangioblastoma

INTRODUCTION
Spinal hemangioblastomas account for 1–3% of all spinal cord tumors and are typically intramedullary in location.[1-5] Here, we report a patient with a T2-T3 thoracic intradural/ extramedullary hemangioblastoma in the absence of von Hippel-Lindau disease. Following gross total tumor excision, the patient neurologically improved.
CASE REPORT
Clinical presentation
A 58-year-old female presented with a 5-year history of progressive left lower extremity weakness. On examination, she exhibited hypesthesia and hypalgesia in both lower extremities accompanied by diffuse hyperreflexia and bilateral Babinski signs. The accompanying laboratory and radiographic studies rule out the presence of von Hippel-Lindau disease.
MR documentation
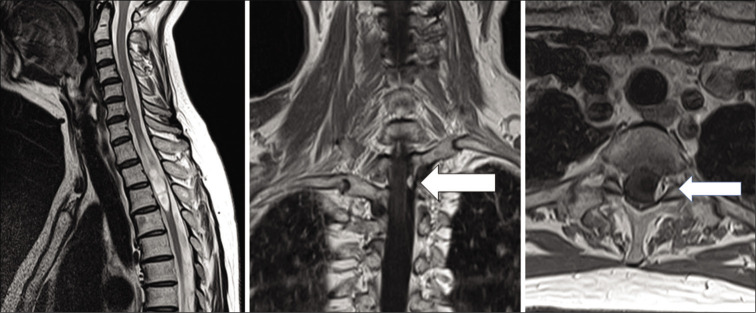
The MR demonstrated a homogenously, contrast enhancing intradural/extramedullary tumor accompanied by edema and a syrinx at the T2-T3 level [Figure 1]. The lesion appeared to be on the surface of the cord and occupied the left posterolateral canal; the syrinxes were located both above and below the lesion. No other lesions were identified on preoperative neuraxis MR studies.
Figure 1:
MRI of the thoracic spine. Left – T2-weighted MR images revealed a syrinx with edema. Center, right – T1-weighted Gd-enhanced image coronal and axial image revealing an extramedullary intradural isodense mass (arrow) at the Th2–3 level. Center, coronal view. Right, axial view.
Surgery
Under MEP and SEP monitoring, the patient underwent gross total excision of the intradural/extramedullary mass. On opening the dura and arachnoid, a triangular, small, orange mass could be seen located between the thoracic roots [Figure 2]. A temporary clip was placed on the vascular feeder to the tumor; it was then “avascularly” detached from the surrounding tissues. Although the tumor was slightly adherent to the dorsal cord, it was still removed “en block,” further, the thin wall of the caudal syrinxes was partially opened. Although transient repeated episodes of SEP and MEP deterioration occurred, the operation was paused every time and was resumed after confirming recovery.
Figure 2:

Left – Intraoperative photograph. A triangle small orange tumor between the thoracic roots. The thin wall of cyst is also seen at caudal side. Right – feeder (left side red) and drainer (right side green) identified by intraoperative indocyanine green.
Five days postoperatively, the patient was discharged with only slight residual left lower extremity weakness. No residual tumor mass was observed on follow-up MR studies. The final histologic diagnosis was consistent with a hemangioblastoma.
DISCUSSION
Spinal hemangioblastomas are rare tumors and mostly occur with von Hippel-Lindau disease.[3,4] As they typically derive from medullary tissues under the pia matter, most are intramedullary in location (41–84% intramedullary, 11–37% intramedullary+extramedullary, and 3–22% extramedullary, respectively).[3-5] Of interest, Yasuda et al. reported that extramedullary hemangioblastomas had smaller syrinxes versus intramedullary and intramedullary+extramedullary lesions,[6] this finding might help distinguish between extramedullary hemangioblastomas versus meningioma and other tumors.
Ideal treatment
The ideal treatment for these lesions is gross total surgical excision.[4] Microsurgical removal under continuous SEP and MEP monitoring is recommended to prevent the onset of new postoperative neurological deficits. Further, identification of and temporary occlusion of vascular feeding vessels using intraoperative indocyanine green readily facilitate hemostasis and less “bloody” tumor removal.
Footnotes
How to cite this article: Kawanishi M, Tanaka H, Itoh Y, Yokoyama K, Yamada M, Sugie A, et al. Intradural extramedullary hemangioblastoma of the thoracic cord: A case report. Surg Neurol Int 2021;12:126.
Contributor Information
Masahiro Kawanishi, Email: mkawanis@takedahp.or.jp.
Hidekazu Tanaka, Email: bozu.hidekazu@nifty.com.
Yutaka Itoh, Email: yutaka_727@yahoo.co.jp.
Kunio Yokoyama, Email: neu100@osaka-med.ac.jp.
Makoto Yamada, Email: neu090@osaka-med.ac.jp.
Akira Sugie, Email: neu055@osaka-med.ac.jp.
Akari Miyake, Email: mkawanistakedahp@yahoo.co.jp.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Deng X, Wang K, Wu L, Yang C, Yang T, Zhao L, et al. Intraspinal hemangioblastomas: Analysis of 92 cases in a single institution: Clinical article. J Neurosurg Spine. 2014;21:260–9. doi: 10.3171/2014.1.SPINE13866. [DOI] [PubMed] [Google Scholar]
- 2.Imagama S, Ito Z, Wakao N, Sakai Y, Kato F, Yukawa Y, et al. Differentiation of localization of spinal hemangioblastomas based on imaging and pathological findings. Eur Spine J. 2011;20:1377–84. doi: 10.1007/s00586-011-1814-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Taniguchi S, Ogikubo O, Nakamura T, Yamagishi I, Hayakawa K, Otsuka T, et al. A rare case of extramedullaryintradural hemangioblastoma in the thoracic spine. Spine (Phila Pa 1976) 2009;34:E969–72. doi: 10.1097/BRS.0b013e3181b8e4f4. [DOI] [PubMed] [Google Scholar]
- 4.Toyoda H, Seki M, Nakamura H, Inoue Y, Yamamoto Y, Takaoka K. Intradural extramedullary hemangioblastoma differentiated by MR images in the cervical spine: A case report and review of the literature. J Spinal Disord Tech. 2004;17:343–7. doi: 10.1097/01.bsd.0000083630.91606.af. [DOI] [PubMed] [Google Scholar]
- 5.Yasargil MG, Antic J, Laciga R, de Preux J, Fideler RW, Boone SC. The microsurgical removal of intramedullary spinal hemangioblastomas. Report of twelve cases and a review of the literature. Surg Neurol. 1976;3:141–8. [PubMed] [Google Scholar]
- 6.Yasuda T, Hasegawa T, Yamato Y, Kobayashi S, Togawa D, Banno T, et al. Relationship between spinal hemangioblastoma location and age. Asian Spine J. 2016;10:309–13. doi: 10.4184/asj.2016.10.2.309. [DOI] [PMC free article] [PubMed] [Google Scholar]