Abstract
Background and Purpose
Dementia is rapidly becoming more common in the elderly population of South Korea, and there are regional difference in its demographics. This study investigated the trajectories in the prevalence and incidence of dementia based on the Seoul metropolitan area and other areas in South Korea using big data from the National Health Insurance Service (NHIS).
Methods
We examined a population-based elderly cohort obtained from the NHIS Senior Cohort (NHIS-SC) data set that comprises approximately half a million recipients of medical insurance in South Korea during 2003–2015. The age-standardized prevalence and incidence of dementia as well as their trajectories from 2003 were estimated. Regional differences in these rates between Seoul metropolitan area and other areas were also analyzed.
Results
The standardized prevalence of dementia per 100,000 increased significantly from 178.11 in 2003 to 5,319.01 in 2015 (p<0.001). The standardized prevalence of dementia was higher in other areas than in Seoul metropolitan area. The standardized incidence of dementia per 100,000 person-years also increased significantly, from 126.41 in 2003 to 2,218.25 in 2015 (p<0.001). The standardized incidence of dementia was similarly higher in other areas than in Seoul metropolitan area (p<0.001).
Conclusions
This study has shown that the standardized prevalence and incidence of dementia increased steadily from 2003 to 2015 in South Korea based on the NHIS-SC data set, and differed between Seoul metropolitan area and other areas.
Keywords: dementia, prevalence, incidence
INTRODUCTION
Dementia is characterized as cognitive decline resulting in a loss of independence that significantly influences the patients themselves, their caregivers and communities, as well as the national health-care system.1,2,3 The number of dementia patients is predicted to double every 20 years and reach about 40 million worldwide by 2020 because of the increasing aging of the global population.4 Supporting and caring for patients with dementia have broad impacts on the family, health-care system, and society as a whole,5,6,7 and hence the burden of dementia is an important issue in South Korea.8,9,10,11
It is essential to have accurate estimates of changes in the epidemiological trends of dementia in order to formulate effective plans for relieving the associated socioeconomic burden. The Nationwide Survey on Dementia Epidemiology of Korea (NaSDEK) was conducted in 2008, 2012, and 2016.12,13,14 The latest survey estimated that the standardized prevalence of dementia was 6.93% (95% CI=4.48–9.23%) among those older than 60 years and 9.50% (95% CI=6.24–12.76%) among those older than 65 years.14 Along with changes in dementia prevalence, the proportions of dementia subtypes are also changing, with that of Alzheimer's disease increasing (70.7%, 71.3%, and 74.4% in 2008, 2012, and 2016, respectively) and that of vascular dementia decreasing markedly (24.4%, 16.9%, and 8.7%) according to NaSDEK studies.
While the NaSDEK studies conducted every four years since 2008 have provided valuable data for estimating the cross-sectional prevalence of dementia, the longitudinal epidemiological trends were not available. Our hypothesis was that these claims-based data could be a good source for making longitudinal estimations in an epidemiological study of dementia compared with survey-based data such as those from the NaSDEK. Therefore, we conducted the present study to investigate the trajectories of the prevalence and incidence of dementia based on nationwide big data.
METHODS
Data acquisition
The study data set was obtained from the Korean National Health Insurance Service (NHIS), which was founded in 2000 as a single-insurer system. The formation of this system involved integrating more than 366 medical insurance organizations that were present in South Korea, and storing and converting the medical records of individuals into a national database called the National Health Information Database (NHID). This database contains personal information, demographics, and medical treatment data for South Korean citizens who were categorized as insured employees, insured self-employed individuals, or medical aid beneficiaries.
The NHIS Senior Cohort (NHIS-SC) is a research database for the elderly constructed in a cohort format for investigating the risk factors and prognosis of geriatric diseases. The NHIS-SC used a simple randomization method to extract data from 557,195 persons, representing 10% of the 5.5 million population aged ≥60 years who had maintained their health insurance and medical-care status at the end of December 2002.15
The members of the NHIS-SC comprise a 14-year cohort (2002–2015) whose socioeconomic variables (residence area, year and month of death, cause of death, and income level) and medical treatments (health examinations, medical-care history, and medical-care institutions) are tracked. These data enable long-term observations and can be used to investigate causal relationships. The cessation of follow-up for individual subjects in the NHIS-SC data set was determined by their death. The elderly subjects sampled in 2002 for the NIHS-SC continue to drop out as they die, and there is no influx of new cases (Supplementary Table 1 in the online-only Data Supplement).
Diseases are registered in the NHIS-SC based on the sixth edition of the Korean Classification of Disease, which is modified from the 10th revision of the International Classification of Disease (ICD-10) for use in the NHIS and medical-care institutions in South Korea. This study was conducted using NHIS-SC (NHIS-2020-2-133) and approved by the Institutional Review Board of Kangwon National University Hospital (approval no. KNUH-B-2019-07-007).
Study population
This study analyzed a population-based cohort constructed using the NHIS-SC. Dementia was defined based on the ICD-10 classification codes (F00, F01, F02, F03, and G30) used with antidementia drugs (donepezil, galantamine, rivastigmine, or memantine) for the first or second diagnosis for medical-expense claims in 2003 through an outpatient clinic more than three times or for at least one hospital admission. We excluded subjects with dementia registered in 2002 (n=736) in order to identify only newly diagnosed subjects with dementia.
In addition to diagnoses, we extracted other variables including age, sex, and residence area. The residence areas were classified into the following two regions according to their geographical location: 1) Seoul metropolitan area (Seoul, Incheon, and Gyeonggi-do) and 2) other areas (Busan, Daegu, Ulsan, Gangwon-do, Gyeongsangbuk-do, Gyeongsangnam-do, Gwangju, Daejeon, Chungcheongbuk-do, Chungcheongnam-do, Jeollabuk-do, Jeollanam-do, and Jeju Special Self-Governing Province).
Statistical analyses
The crude prevalence of dementia per 100,000 in South Korea according to geographical location was calculated by dividing the number of subjects classified as ICD-10 codes F00, F01, F02, F03, and G30 in each year by the total number of subjects in that year. The standardized prevalence rate of dementia was calculated to compare the prevalence of dementia across years. The crude incidence rates of dementia were calculated per 100,000 South Koreans and for each region. The standardized incidence of dementia corrected for the age and sex of the standard population of South Korea and of the regions was calculated to compare incidence rates of dementia across years.
The following formula was used to calculate the age- and sex-standardized prevalence:16
where Pi is the number of persons in age group i in the standard population; Ei is the expected number of events in age group i in the standard population; ei(f) is the number of events for females in age group i; ei(m) is the number of events for males in age group i; pi(f) is the number of females in age group i in the study population; pi(m) is the number of males in age group i in the study population; Pi(f) is the number of females in age group i in the standard population; Pi(m) is the number of males in age group i in the standard population.
The age- and sex-standardized incidence was calculated using the following formula:16
where ΔTi is the expected number of events in age group i in the standard population during a certain period of time; Ei* is the expected number of new events in age group i in the standard population during a certain period of time; ei(f)* is the number of new events for females in age group i during a certain period of time; ei(m)* is the number of events for males in age group i during a certain period of time; Δti(f) is the person-years at risk females in age group i in the study population during a certain period of time; Δti(m) is the person-years at risk males in age group i in the study population during a certain period of time.
Trend analysis was applied to investigate the trends in the prevalence and incidence of dementia during the study period. The Cochran-Armitage trend test was used to determine whether there were significant linear trends in the prevalence and incidence of dementia.17,18 The statistical analyses were performed using the SAS statistical package (version 7.1, SAS, Cary, NC, USA).
RESULTS
In 2003, the NHIS-SC included 557,195 subjects aged ≥60 years, of whom 1,081 had newly diagnosed dementia (Table 1). The number of subjects in this cohort had decreased to 352,869 in 2015, at which time 23,605 were diagnosed as dementia (Table 2). The number of persons who dropped out due to emigration or death increased as the age of the population in this cohort increased.
Table 1. Numbers of newly diagnosed patients with dementia aged ≥60 years in 2003.
| Variable | Dementia | Total (n=557,195) | |
|---|---|---|---|
| Yes (n=1,081) | No (n=556,114) | ||
| Sex | |||
| Male | 383 (35) | 229,770 (41) | 230,153 |
| Female | 698 (65) | 326,344 (59) | 327,042 |
| Age, years | |||
| 60-64 | 70 (6) | 161,191 (29) | 161,261 |
| 65-69 | 182 (17) | 156,973 (28) | 157,155 |
| 70-74 | 222 (21) | 105,117 (19) | 105,339 |
| 75-79 | 258 (24) | 66,720 (12) | 66,978 |
| 80-84 | 246 (23) | 41,105 (7) | 41,351 |
| ≥85 | 103 (10) | 25,008 (4) | 25,111 |
| Region | |||
| Seoul metropolitan area | 498 (46) | 214,450 (39) | 214,948 |
| Other areas | 583 (54) | 341,664 (61) | 342,247 |
Data are n (%) values.
Table 2. Crude and standardized prevalence and incidence rates of dementia in subjects aged ≥60 years in South Korea from 2003 to 2015.
| Year | Population (n) | Dementia (n) | Prevalence* | De novo (n) | Incidence* | ||
|---|---|---|---|---|---|---|---|
| Crude | Standardized | Crude | Standardized | ||||
| 2003 | 557,195 | 1,081 | 194.01 | 178.11 | 741 | 135.63 | 126.41 |
| 2004 | 539,278 | 1,265 | 234.57 | 201.83 | 849 | 160.21 | 140.06 |
| 2005 | 521,967 | 2,056 | 393.89 | 318.21 | 1,469 | 287.58 | 235.83 |
| 2006 | 504,417 | 3,569 | 707.55 | 535.72 | 2,421 | 491.85 | 379.37 |
| 2007 | 487,460 | 4,933 | 1,011.98 | 980.70 | 3,029 | 637.86 | 628.19 |
| 2008 | 470,005 | 6,707 | 1,427.01 | 1,288.71 | 3,904 | 852.42 | 785.10 |
| 2009 | 452,631 | 9,307 | 2,056.20 | 1,729.22 | 5,399 | 1,232.03 | 1,061.54 |
| 2010 | 436,395 | 11,514 | 2,638.44 | 2,074.79 | 6,244 | 1,482.21 | 1,197.99 |
| 2011 | 422,171 | 14,446 | 3,421.84 | 2,492.09 | 7,352 | 1,812.78 | 1,361.42 |
| 2012 | 405,614 | 16,393 | 4,041.53 | 3,905.28 | 7,599 | 1,950.58 | 1,938.58 |
| 2013 | 388,493 | 18,621 | 4,793.14 | 4,355.67 | 8,266 | 2,227.68 | 2,085.24 |
| 2014 | 369,307 | 20,847 | 5,644.90 | 4,797.89 | 8,622 | 2,447.93 | 2,149.39 |
| 2015 | 352,869 | 23,605 | 6,689.45 | 5,319.01 | 9,043 | 2,696.31 | 2,218.25 |
| p | <0.0001 | <0.0001 | <0.0001 | <0.0001 | |||
p values are from the Cochran-Armitage trend test.
*Prevalence rate per 100,000 persons and incidence rate per 100,000 person-years.
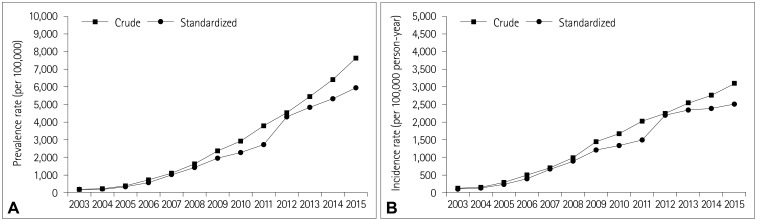
The crude prevalence of dementia per 100,000 subjects aged ≥60 years in South Korea increased gradually from 194.01 in 2003 to 6,689.45 in 2015. The standardized prevalence of dementia per 100,000 increased from 178.11 to 5,319.01 during the same period (Table 2). In the trend analysis, both the crude and standardized prevalence rates of dementia increased in subjects aged ≥60 years (p<0.0001) (Fig. 1A). The crude incidence of dementia per 100,000 South Koreans aged ≥60 years was 135.63 in 2003 and 2,696.31 in 2015; the corresponding standardized rates were 126.41 and 2,218.25, respectively (Table 2). The trend analysis revealed increasing trends in both the crude and standardized incidence rates (p<0.0001) (Fig. 1B).
Fig. 1. Trends in the crude and standardized prevalence (A) and incidence (B) rates of dementia among subjects aged ≥60 years in South Korea from 2003 to 2015.
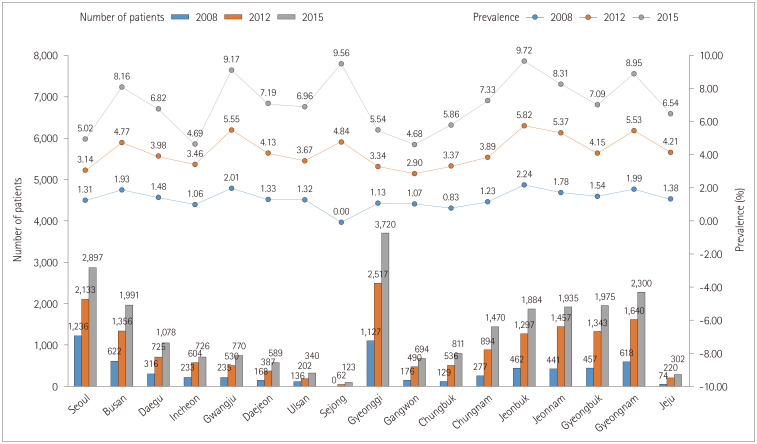
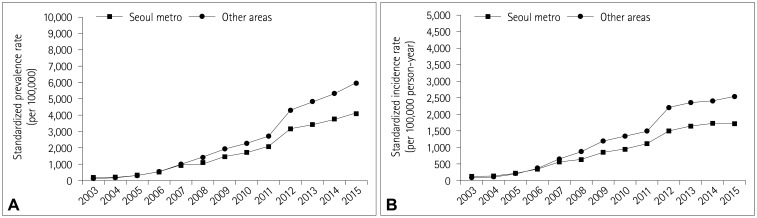
In the regional analysis, the number of patients with dementia exhibited an overall increasing trend regardless of the wide-area unit of the local government across 2008, 2012, and 2015 (Fig. 2), and prevalence rate was largest in Jeollabuk-do in 2015. The standardized prevalence of dementia per 100,000 in 2003 was higher in Seoul metropolitan area (211.24) than the other areas combined (157.08). In the trend analysis, the standardized prevalence of dementia in both regions increased gradually regardless of age group, and the increase was faster in other areas than in Seoul metropolitan area from 2006, with this gap increasing further up to 2015 (Fig. 3A). In the regional analysis, the standardized incidence of dementia per 100,000 person-years in 2003 was higher in Seoul metropolitan area (146.52) than the other areas combined (113.62). In the trend analysis, the standardized incidence rates of dementia in both regions increased gradually regardless of age group, but was higher in other areas than in Seoul metropolitan area from 2006, with this gap increasing further up to 2015 (Fig. 3B).
Fig. 2. Comparison of the numbers of dementia patients according to wide-area units of local government.
Fig. 3. Trends in the standardized prevalence (A) and incidence (B) rates of dementia in South Korea in two regions based on the degree of urbanization from 2003 to 2015.
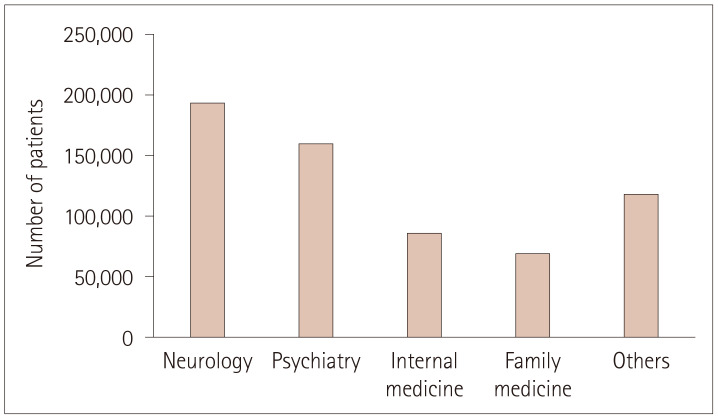
Across the study period, the largest proportion of dementia patients received neurology treatment (30.8%), followed by psychiatry (25.3%), internal medicine (13.79%), and family medicine (11.06%) treatments (Fig. 4).
Fig. 4. Numbers of patients with dementia treated in each department.
DISCUSSION
This study found significant increases in the prevalence and incidence of dementia during all observation periods, with both being higher in other areas than in Seoul metropolitan area from 2006. As far as we know, this is the first study to investigate the prevalence and incidence of dementia using the NHIS-SC cohort.
Many epidemiological studies have investigated dementia among South Korean elderly during 1990–201319,20,21,22,23,24,25,26,27,28,29 based on regional populations using various diagnostic evaluation methods and study designs. A systemic review and meta-analysis of these studies showed that the pooled prevalence estimate of dementia in elderly subjects aged ≥65 years was 9.2% (95% CI=8.2–10.4%), but no significant increasing trend was found.30 This was much higher than the prevalence estimates of dementia in other Asian countries (5.63–7.70%), Europe (5.18–6.80%), and the Americas (5.73–8.41%) according to the World Alzheimer's Report (WAR) in 2015.2 This difference might be due to the pooled prevalence of dementia in the WAR for 2015 being determined for subjects aged ≥60 years while the meta-analysis was performed with subjects aged ≥65 years. As for 2015, the prevalence and incidence rates of dementia from the NIHS-SC data set were 6.69% and 2.56%, respectively, which are within the range of values for other countries in the WAR in 2015.
A previous study of the prevalence and incidence of dementia in Western countries found either stable or declining rates.31 The prevalence of dementia in Western Europe was reported to have reduced by up to 25% in recent decades, suggesting a stabilization in the number of people with dementia in Western Europe despite the presence of population aging.32 In contrast, the prevalence of dementia is increasing in East Asian countries such as Japan, Hong Kong, Taiwan, China, and South Korea.12,33,34,35,36,37 Some of these differences between Eastern and Western countries might be attributable to differences in the selection of the research population, study design, economic status, or social context.31 There are several possible explanations for the increasing prevalence rate of dementia in our study being different from those in other countries. Firstly, among the elderly subjects sampled in 2002 for the NIHS-SC, the deceased continue to drop out without any influx of new cases, and so the number of subjects reduced each year throughout the 14-year observational period, especially among the relatively young elderly. Therefore, the increased annual prevalence rate in our study (in contrast to other countries) might be partly due to the characteristic structure of the sampled data. Secondly, the rate of diagnosing dementia might have increased due to changes in the social/educational conditions, such as the Long-Term Care Insurance program or providing specialized training to dementia physicians supported by the Ministry of Health and Welfare.38,39,40,41 Thirdly, increases in prevalence and incidence can reflect improvements in diagnostic sensitivity and accuracy rather than actual increases in the number of patients with dementia.42
Comparing the NIHS-SC in 2015 and NaSDEK in 2016 revealed that the prevalence rates of dementia in elderly subjects aged ≥60 years were similar, at 6,689 and 6,930 per 100,000, respectively (Table 3).
Table 3. Comparison of crude prevalence of dementia in the NaSDEK in 2016 and the Korean NHIS-SC in 2015.
| NaSDEK | NHIS-SC | |
|---|---|---|
| Male | 4,720 | 4,519 |
| Female | 8,520 | 8,014 |
| Total | 6,930 | 6,689 |
NaSDEK: Nationwide Survey on Dementia Epidemiology of Korea, NHIS-SC: National Health Insurance Service Senior Cohort
The number of patients is constantly higher in other areas than in Seoul metropolitan area and nonspecialist departments such as internal medicine, family medicine, and others were in charge of large proportion of patients with dementia. These findings suggest the need for appropriate regional allocations of resources to support patients or their caregivers as well as the importance of providing education to people who are not experts in dementia.
The present study has demonstrated that national dementia prevalence and incidence rates can be calculated using health insurance statistics such as the NIHS-SC, but there are some limitations. Firstly, it is difficult to ensure data reliability due to different standards for dementia codes being used by different experts and the use of codes sometimes being exaggerated for reimbursements from the fee-for-service payment system.15,43 Standard criteria for calculating prevalence and incidence rates based on patients diagnosed with dementia should be developed using reasonable standards, such as treatment data including drugs combined with ICD-10 codes. Secondly, all patients who receive medication cannot be regarded as having dementia, and dementia drugs are sometimes stopped because of the presence of other medical conditions. Thirdly, the prevalence of mild cognitive impairment and the severity of dementia cannot be obtained from the NIHS-SC. Despite these limitations, the NHIS-SC provides a large sample of 557,195 subjects with a long duration of follow-up from 2002 to 2015 that is representative of the entire elderly population.15
While the cross-sectional prevalence was similar in the NaSDEK and NHIS-SC studies, there are several notable differences. Firstly, the resources and time required for epidemiological investigations are far greater for the NaSDEK than the NHIS-SC. The NaSDEK performed a two-stage study comprising ‘Phase I screening’ that involved applying the Mini Mental State Examination in door-to-door home visits and ‘Phase II diagnostic assessment’ involving a neuropsychological battery.12 However, it is easier to analyze the prevalence and incidence of dementia using the NIHS-SC than the NaSDEK because the former already contains big data on health insurance claims constructed on a yearly basis. The NIHS-SC also has advantages in terms of the duration of data processing and the reliability of data. While the NaSDEK as well as other previous epidemiological studies provide only cross-sectional data, the NIHS-SC provides longitudinal changes during the long-term follow-up of subjects that can show both incidence and prevalence rates. Additionally, the NIHSSC is relatively free from recall bias compared with survey-based data such as the NaSDEK, because the former is based on a nationwide retrospective cohort that includes information from elderly individuals who are randomly sampled by the NHID.15 On top of this, the NIHS-SC also provides information on regional differences as well as medical departments in charge of patients with dementia (Figs. 3 and 4).
In conclusion, the standardized prevalence and incidence rates of dementia increased steadily from 2003 to 2015 in South Korea. There were regional differences in these rates between Seoul metropolitan area and other areas. Big data such as those in the NIHS-SC obtained from health insurance statistics seem to be able to supplement other survey-based national epidemiological studies and also come with their own advantages.
Acknowledgements
This study used National Health Insurance Service-Senior Cohort data (NHIS-2020-2-133), made by National Health Insurance Service. This study was supported by 2021 Kangwon National University Hospital Grant.
Footnotes
- Conceptualization: Jae-Won Jang, Seung-Hwan Lee.
- Data curation: Suk-Hee Lee, Jeong Hoon Park.
- Formal analysis: Suk-Hee Lee, Seongheon Kim.
- Funding acquisition: Jae-Won Jang.
- Investigation: Seung-Hwan Lee.
- Methodology: Young-Ju Kim.
- Project administration: Jae-Won Jang.
- Resources: Seongheon Kim.
- Supervision: Young-Ju Kim.
- Validation: Suk-Hee Lee.
- Visualization: Jae-Won Jang.
- Writing—original draft: Suk-Hee Lee, Jae-Won Jang.
- Writing—review & editing: Young-Ju Kim, Jae-Won Jang.
Conflicts of Interest: The authors have no potential conflicts of interest to disclose.
Supplementary Materials
The online-only Data Supplement is available with this article at https://doi.org/10.3988/jcn.2021.17.2.249
Numbers of total and deceased subjects in each year from 2002 to 2015
References
- 1.Matthews KA, Xu W, Gaglioti AH, Holt JB, Croft JB, Mack D, et al. Racial and ethnic estimates of Alzheimer's disease and related dementias in the United States (2015–2060) in adults aged ≥65 years. Alzheimers Dement. 2019;15:17–24. doi: 10.1016/j.jalz.2018.06.3063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Prince M, Wimo A, Guerchet M, Ali GC, Wu YT, Prina M. World Alzheimer Report 2015. The global impact of dementia: an analysis of prevalence, incidence, cost and trends [Internet] London: Alzheimer's Disease International; 2015. Aug, Available from: https://www.alzint.org/u/WorldAlzheimerReport2015.pdf. [Google Scholar]
- 3.Prince M, Bryce R, Albanese E, Wimo A, Ribeiro W, Ferri CP. The global prevalence of dementia: a systematic review and metaanalysis. Alzheimers Dement. 2013;9:63–75.e2. doi: 10.1016/j.jalz.2012.11.007. [DOI] [PubMed] [Google Scholar]
- 4.Ferri CP, Prince M, Brayne C, Brodaty H, Fratiglioni L, Ganguli M, et al. Global prevalence of dementia: a Delphi consensus study. Lancet. 2005;366:2112–2117. doi: 10.1016/S0140-6736(05)67889-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Etters L, Goodall D, Harrison BE. Caregiver burden among dementia patient caregivers: a review of the literature. J Am Acad Nurse Pract. 2008;20:423–428. doi: 10.1111/j.1745-7599.2008.00342.x. [DOI] [PubMed] [Google Scholar]
- 6.Hughes TB, Black BS, Albert M, Gitlin LN, Johnson DM, Lyketsos CG, et al. Correlates of objective and subjective measures of caregiver burden among dementia caregivers: influence of unmet patient and caregiver dementia-related care needs. Int Psychogeriatr. 2014;26:1875–1883. doi: 10.1017/S1041610214001240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ornstein K, Gaugler JE. The problem with “problem behaviors”: a systematic review of the association between individual patient behavioral and psychological symptoms and caregiver depression and burden within the dementia patient-caregiver dyad. Int Psychogeriatr. 2012;24:1536–1552. doi: 10.1017/S1041610212000737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kim JH, Lee Y. Dementia and death after stroke in older adults during a 10-year follow-up: results from a competing risk model. J Nutr Health Aging. 2018;22:297–301. doi: 10.1007/s12603-017-0914-3. [DOI] [PubMed] [Google Scholar]
- 9.Kim H, Chun HW, Kim S, Coh BY, Kwon OJ, Moon YH. Longitudinal study-based dementia prediction for public health. Int J Environ Res Public Health. 2017;14:983. doi: 10.3390/ijerph14090983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Park JH, Eum JH, Bold B, Cheong HK. Burden of disease due to dementia in the elderly population of Korea: present and future. BMC Public Health. 2013;13:293. doi: 10.1186/1471-2458-13-293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Seo HJ, Lee DY, Sung MR. Public knowledge about dementia in South Korea: a community-based cross-sectional survey. Int Psychogeriatr. 2015;27:463–469. doi: 10.1017/S1041610214001896. [DOI] [PubMed] [Google Scholar]
- 12.Kim KW, Park JH, Kim MH, Kim MD, Kim BJ, Kim SK, et al. A nationwide survey on the prevalence of dementia and mild cognitive impairment in South Korea. J Alzheimers Dis. 2011;23:281–291. doi: 10.3233/JAD-2010-101221. [DOI] [PubMed] [Google Scholar]
- 13.Han J, So Y, Kim TH, Lee DY, Ryu SH, Kim SY, et al. Dementia epidemiology in Korea: comparison of the results from the Nationwide Survey on the Dementia Epidemiology (NaSDEK) 2008 and the NaSDEK 2012. Alzheimers Dement. 2013;9:P687 [Google Scholar]
- 14.Kim KW. A nationwide survey on the prevalence of dementia and mild cognitive impairment in South Korea [Internet] National Institute of Dementia; 2017. Jun, Report No.: NIDR-1603-0015. Available from: https://www.nid.or.kr/info/dataroom_view.aspx?BID=182. [DOI] [PubMed] [Google Scholar]
- 15.Kim YI, Kim YY, Yoon JL, Won CW, Ha S, Cho KD, et al. Cohort profile: National Health Insurance Service-senior (NHIS-senior) cohort in Korea. BMJ Open. 2019;9:e024344. doi: 10.1136/bmjopen-2018-024344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lee SH, Lee SJ, Kim YJ. Region-based analysis of prevalence and incidence of Parkinson’s disease: analysis of the national sample cohort in South Korea. J Clin Neurol. 2018;14:478–486. doi: 10.3988/jcn.2018.14.4.478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Cochran WG. Some methods for strengthening the common χ2 tests. Biometrics. 1954;10:417–451. [Google Scholar]
- 18.Armitage P. Tests for linear trends in proportions and frequencies. Biometrics. 1955;11:375–386. [Google Scholar]
- 19.Suh GH, Kim JK, Cho MJ. Community study of dementia in the older Korean rural population. Aust N Z J Psychiatry. 2003;37:606–612. doi: 10.1046/j.1440-1614.2003.01237.x. [DOI] [PubMed] [Google Scholar]
- 20.Park J, Ko HJ, Park YN, Jung CH. Dementia among the elderly in a rural Korean community. Br J Psychiatry. 1994;164:796–801. doi: 10.1192/bjp.164.6.796. [DOI] [PubMed] [Google Scholar]
- 21.Kwak DI, Choi YK, Jung IK, Lee MS. Epidemiological study of dementia in a Korea urban area. J Korean Geriatr Psychiatry. 1999;3:44–52. [Google Scholar]
- 22.Shin HY, Chung EK, Rhee JA, Yoon JS, Kim JM. Prevalence and related factors of dementia in an urban elderly population using a new screening method. J Prev Med Public Health. 2005;38:351–358. [PubMed] [Google Scholar]
- 23.Woo JI, Lee JH, Yoo KY, Kim CY, Kim YI, Shin YS. Prevalence estimation of dementia in a rural area of Korea. J Am Geriatr Soc. 1998;46:983–987. doi: 10.1111/j.1532-5415.1998.tb02753.x. [DOI] [PubMed] [Google Scholar]
- 24.Choi SJ, Jung SS, You YS, Shin BS, Kim JE, Yoon SW, et al. Prevalence of Alzheimer’s dementia and its risk factors in community-dwelling elderly Koreans. Psychiatry Investig. 2008;5:78–85. doi: 10.4306/pi.2008.5.2.78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Jhoo JH, Kim KW, Huh Y, Lee SB, Park JH, Lee JJ, et al. Prevalence of dementia and its subtypes in an elderly urban Korean population: results from the Korean Longitudinal Study on Health and Aging (KLoSHA) Dement Geriatr Cogn Disord. 2008;26:270–276. doi: 10.1159/000160960. [DOI] [PubMed] [Google Scholar]
- 26.Kim DH, Na DL, Yeon BG, Kang Y, Min KB, Lee SH, et al. Prevalence of dementia in the elderly of an urban community in Korea. Korean J Prev Med. 1999;32:306–316. [Google Scholar]
- 27.Shin IS, Kim JM, Yoon JS, Kim SJ, Yang SJ, Kim WJ, et al. Prevalence rate and risk factors of dementia compared between urban and rural communities of the metropolitan Kwangju area. J Korean Neuropsychiatr Assoc. 2002;41:1165–1173. [Google Scholar]
- 28.Kim J, Jeong I, Chun JH, Lee S. The prevalence of dementia in a metropolitan city of South Korea. Int J Geriatr Psychiatry. 2003;18:617–622. doi: 10.1002/gps.897. [DOI] [PubMed] [Google Scholar]
- 29.Lee DY, Lee JH, Ju YS, Lee KU, Kim KW, Jhoo JH, et al. The prevalence of dementia in older people in an urban population of Korea: the Seoul study. J Am Geriatr Soc. 2002;50:1233–1239. doi: 10.1046/j.1532-5415.2002.50310.x. [DOI] [PubMed] [Google Scholar]
- 30.Kim YJ, Han JW, So YS, Seo JY, Kim KY, Kim KW. Prevalence and trends of dementia in Korea: a systematic review and meta-analysis. J Korean Med Sci. 2014;29:903–912. doi: 10.3346/jkms.2014.29.7.903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Wu YT, Beiser AS, Breteler MMB, Fratiglioni L, Helmer C, Hendrie HC, et al. The changing prevalence and incidence of dementia over time - current evidence. Nat Rev Neurol. 2017;13:327–339. doi: 10.1038/nrneurol.2017.63. [DOI] [PubMed] [Google Scholar]
- 32.Wu YT, Fratiglioni L, Matthews FE, Lobo A, Breteler MM, Skoog I, et al. Dementia in Western Europe: epidemiological evidence and implications for policy making. Lancet Neurol. 2016;15:116–124. doi: 10.1016/S1474-4422(15)00092-7. [DOI] [PubMed] [Google Scholar]
- 33.Dodge HH, Buracchio TJ, Fisher GG, Kiyohara Y, Meguro K, Tanizaki Y, et al. Trends in the prevalence of dementia in Japan. Int J Alzheimers Dis. 2012;2012:956354. doi: 10.1155/2012/956354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Yu R, Chau PH, McGhee SM, Cheung WL, Chan KC, Cheung SH, et al. Trends in prevalence and mortality of dementia in elderly Hong Kong population: projections, disease burden, and implications for long-term care. Int J Alzheimers Dis. 2012;2012:406852. doi: 10.1155/2012/406852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Fuh JL, Wang SJ. Dementia in Taiwan: past, present, and future. Acta Neurol Taiwan. 2008;17:153–161. [PubMed] [Google Scholar]
- 36.Zhang Y, Xu Y, Nie H, Lei T, Wu Y, Zhang L, et al. Prevalence of dementia and major dementia subtypes in the Chinese populations: a meta-analysis of dementia prevalence surveys, 1980–2010. J Clin Neurosci. 2012;19:1333–1337. doi: 10.1016/j.jocn.2012.01.029. [DOI] [PubMed] [Google Scholar]
- 37.Chan KY, Wang W, Wu JJ, Liu L, Theodoratou E, Car J, et al. Epidemiology of Alzheimer's disease and other forms of dementia in China, 1990–2010: a systematic review and analysis. Lancet. 2013;381:2016–2023. doi: 10.1016/S0140-6736(13)60221-4. [DOI] [PubMed] [Google Scholar]
- 38.Jeon B, Kwon S. Health and long-term care systems for older people in the Republic of Korea: policy challenges and lessons. Health Syst Reform. 2017;3:214–223. doi: 10.1080/23288604.2017.1345052. [DOI] [PubMed] [Google Scholar]
- 39.Kang IO, Park CY, Lee Y. Role of healthcare in Korean long-term care insurance. J Korean Med Sci. 2012;27(Suppl):S41–S46. doi: 10.3346/jkms.2012.27.S.S41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Ga H. Long-term care system in Korea. Ann Geriatr Med Res. 2020;24:181–186. doi: 10.4235/agmr.20.0036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Kim SH. Future policy directions for planning of national responsibility for dementia care. J Korean Med Assoc. 2017;60:622–626. [Google Scholar]
- 42.Livingston G, Huntley J, Sommerlad A, Ames D, Ballard C, Banerjee S, et al. Dementia prevention, intervention, and care: 2020 report of the Lancet Commission. Lancet. 2020;396:413–446. doi: 10.1016/S0140-6736(20)30367-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Wilchesky M, Tamblyn RM, Huang A. Validation of diagnostic codes within medical services claims. J Clin Epidemiol. 2004;57:131–141. doi: 10.1016/S0895-4356(03)00246-4. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Numbers of total and deceased subjects in each year from 2002 to 2015