Abstract
Coronavirus disease 2019 (COVID-19) can reportedly manifest as an acute stroke, with most cases presenting as large vessel ischemic stroke in patients with or without comorbidities. The exact pathomechanism of stroke in COVID-19 remains ambiguous. The findings of previous studies indicate that the most likely underlying mechanisms are cerebrovascular pathological conditions following viral infection, inflammation-induced endothelial dysfunction, and hypercoagulability. Acute endothelial damage due to inflammation triggers a coagulation cascade, thrombosis propagation, and destabilization of atherosclerosis plaques, leading to large-vessel occlusion and plaque ulceration with concomitant thromboemboli, and manifests as ischemic stroke. Another possible mechanism is the downregulation of angiotensin-converting enzyme 2 as the target action of severe acute respiratory syndrome-coronavirus-2 (SARS-CoV-2). Acute stroke management protocols need to be modified during the COVID-19 pandemic in order to adequately manage stroke patients with COVID-19.
Keywords: stroke, COVID-19, hypercoagulability, inflammation, renin-angiotensin system
INTRODUCTION
The World Health Organization declared the coronavirus disease 2019 (COVID-19) pandemic on March 11, 2020 caused by a new strain of coronavirus named severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2), which was first reported in Wuhan, China.1,2 This type of virus has been identified as using the angiotensin-converting enzyme 2 (ACE2) as its main receptor for entering human cells. In addition to respiratory tract infections, there are some reports of COVID-19 also manifesting with symptoms involving the nervous system, cardiovascular, hematology, digestive, and urinary systems.3,4,5
Neurological manifestations of COVID-19 can be related to damage to the central nervous system (CNS) and peripheral nervous system.6 The most common reported CNS symptom found in moderate to severe COVID-19 has been an acute cerebrovascular event or stroke.6 The underlying mechanism of stroke has yet to be established, though activation of coagulation cascade causing thrombus formation has been documented in COVID-19 patients, suggesting the role of inflammatory induced vascular diseases.7,8 ACE2 downregulation is likely to play a role due to the affinity of its receptor to the virus upon entering human cells and causing imbalance of the renin-angiotensin system (RAS). The risk of stroke was reported to be elevated in COVID-19 patients with comorbidities such as hypertension, diabetes, dyslipidemia, and previous history of cerebrovascular disease.6
This article reviews the possible pathomechanisms of stroke in COVID-19 and its management based on recently reported cases of stroke in COVID-19 and pathological findings for the CNS in COVID-19 patients. The in-depth discussion reveals possible mechanisms via which SARS-CoV-2 infection can cause cerebrovascular events and the role of ACE2 as both the entry site and the protector of the vascular system. This review also discusses the latest recommendations for anticoagulant therapy in patients with severe COVID-19 as well as its potential effects and harms stroke outcome.
STROKE IN COVID-19
A retrospective study of 214 COVID-19 patients in Wuhan, China identified 5 patients with concomitant acute stroke, 4 with ischemic strokes and 1 with cerebral hemorrhage. All patients were critically ill with lymphopenia and high D-dimer levels.6 Increasing number of studies of SARS-CoV-2 from different countries have found cerebrovascular events in COVID-19 patients (Table 1).6,9,10,11,12,13,14,15,16,17,18,19,20,21,22
Table 1. Reports of stroke in COVID-19 patients.
| NO | Author | Country | Study design | Number of COVID-19 cases reported | Number of stroke cases reported | Stroke types | ||
|---|---|---|---|---|---|---|---|---|
| Ischemic stroke | Cerebral hemorrhage | SAH | ||||||
| 1 | Mao et al.6 | China | Retrospective study | 214 | 5 | 4 | 1 | - |
| 2 | Oxley et al.9 | USA | Retrospective case series | 5 | 5 | 5 | - | - |
| 3 | Avula et al.10 | USA | Retrospective case series | 4 | 4 | 4 | - | - |
| 4 | Beyrouti et al.11 | UK | Retrospective case series | 6 | 6 | 6 | - | - |
| 5 | Lodigiani et al.12 | Italy | Retrospective study | 388 | 9 | 9 | - | - |
| 6 | Tunç et al.13 | Turkey | Retrospective case series | 4 | 4 | 4 | - | - |
| 7 | Dogra et al.14 | USA | Retrospective study | 33 | 33 | - | 33 | - |
| 8 | Co et al.15 | Philippines | Case report | 1 | 1 | 1 | - | - |
| 9 | Gunasekaran et al.16 | USA | Case report | 1 | 1 | 1 | - | - |
| 10 | Fara et al.17 | USA | Retrospective case series | 3 | 3 | 3 | - | - |
| 11 | Al Saiegh et al.18 | USA | Retrospective case series | 2 | 2 | 1 | - | 1 |
| 12 | Saggese et al.19 | Italy | Case report | 1 | 1 | 1 | - | - |
| 13 | Zhai et al.20 | China | Case report | 1 | 1 | 1 | - | - |
| 14 | Goldberg et al.21 | USA | Case report | 1 | 1 | 1 | - | - |
| 15 | Yaghi et al.22 | USA | Retrospective study | 3,556 | 32 | 32 | - | - |
SAH: subarachnoid hemorrhage.
We covered 11 case reports on stroke in COVID-19 patients from the following 6 countries: the USA, the UK, Italy, the Philippines, Turkey, and China (Table 2).9,10,13,15,16,17,18,19,20,21 There were 29 stroke cases found up to when this review was submitted for publication. All but one of these cases (96.6%), which involved subarachnoid hemorrhage (SAH), were reported as ischemic strokes. Almost all of the ischemic strokes were large vessel stroke that affected the anterior circulation and particularly the middle cerebral artery, with only 3 (10.3%) found to be small vessel stroke. Twenty patients (69.0%) were older than 50 years, with males (17 patients, 58.6%) predominating over females (12 patients, 41.4%). COVID-19 symptoms preceding stroke onset were common (16 patients, 55.2%). Stroke was reported across all severities of COVID-19, but with higher proportions in moderate and severe cases. There were diverse laboratory findings in these case reports. The generalized findings showed that most cases presented with a hypercoagulability state as demonstrated by elevated D-dimer and fibrinogen.
Table 2. Characteristics of stroke in 29 COVID-19 patients described in case reports.
| Variable | Number of cases (%) Total 29 |
|---|---|
| Age | |
| ≤50 years | 9 (31.0) |
| >50 years | 20 (69.0) |
| Sex | |
| Male | 17 (58.6) |
| Female | 12 (41.4) |
| Risk factor for stroke | |
| Identified | 21 (72.4) |
| None | 8 (27.6) |
| Stroke type | |
| Ischemic stroke | 28 (96.6) |
| SAH | 1 (3.4) |
| Vascular territories | |
| Large vessel stroke | |
| ICA | 3 (10.3) |
| MCA | 15 (51.8) |
| PCA | 3 (10.3) |
| Others | 5 (17.2) |
| Small vessel stroke | 3 (10.3) |
| Treatment for stroke | |
| Intravenous t-PA | 5 (17.2) |
| Endovascular treatment | 5 (17.2) |
| Anticoagulant only | 6 (20.7) |
| Antithrombotic only | 7 (24.1) |
| Anticoagulant and antithrombotic | 4 (13.8) |
| Not specified | 2 (6.9) |
| Clinical presentation | |
| Stroke as first presentation | 9 (31.0) |
| COVID-19 as first presentation | 16 (55.2) |
| Not specified | 4 (13.8) |
| COVID-19 severity | |
| No symptoms | 2 (6.9) |
| Mild | 9 (31.0) |
| Moderate | 6 (20.7) |
| Severe/intensive care | 12 (41.4) |
| Laboratory finding | |
| D-dimer: high / normal / not available | 18 (62.1) / 3 (10.3) / 8 (27.6) |
| CRP: high / normal / not available | 14 (48.3) / 2 (6.9) / 13 (44.9) |
| Fibrinogen: high / normal / not available | 10 (34.5) / 1 (3.4) /18 (62.1) |
| Thrombocyte: high / normal / low / not available | 0 / 18 (62.1) / 0 / 11 (37.9) |
| Outcome | |
| Discharged | 24 (82.8) |
| Death | 3 (10.3) |
| Not specified | 2 (6.9) |
Data are n (%) values.
COVID-19: coronavirus disease 2019, CRP: C-reactive protein, ICA: internal carotid artery, MCA: middle cerebral artery, PCA: posterior cerebral artery, SAH: subarachnoid hemorrhage, t-PA: tissue plasminogen activator.
Yaghi et al.22 reported 32 cases of strokes out of 3,556 hospitalized COVID-19 patients in New York. They were all ischemic stroke, with an etiologic distribution of 21 cryptogenic cases, 7 cardioembolic cases, 2 large-artery atherosclerosis, and 2 watershed stroke cases due to hypotension. That study compared the clinical and laboratory aspects of stroke in COVID-19 versus non-COVID-19 stroke cases as control. The cases of stroke with COVID-19 were found to have higher D-dimer levels, more likely to have a cryptogenic stroke subtype, more likely to be treated with anticoagulant, and higher inpatient mortality. Cryptogenic strokes were reported to be associated with higher D-dimer that represents a hypercoagulability state.22
A retrospective study from Italy reported thromboembolic events in 28 out of 388 COVID-19 cases which were divided into 9 patients with stroke, 4 patients with acute ST-elevation myocardial infarction, 5 patients with pulmonary embolism, and 10 patients with venous thromboembolism. The incidence of thromboembolic events after receiving thromboprophylaxis management were 7.7%. The reasoning proposed by the authors was the occurrence of thromboembolic events within the first 24 hours of hospital admission, rendering it unpreventable by the thromboprophylaxis protocols of the hospital.12
A study in New York of intracerebral bleeding in 33 cases COVID-19 patients found that 27 of them had previously given an anticoagulant.14 Twenty-two patients received therapeutic anticoagulant doses during hospitalization, 18 received anticoagulant due to high levels of D-dimer, and 4 received anticoagulant due to suspected thrombus. Unfractionated heparin was administered in most of the cases. A larger proportion of the cases were identified as having punctate hemorrhages, while five patients presenting with large parenchymal bleeding with mass effect and herniation. Mortality occured in 14 (42.4%) patients.14
CHARACTERISTICS AND IMMUNE RESPONSE OF SARS-CoV-2
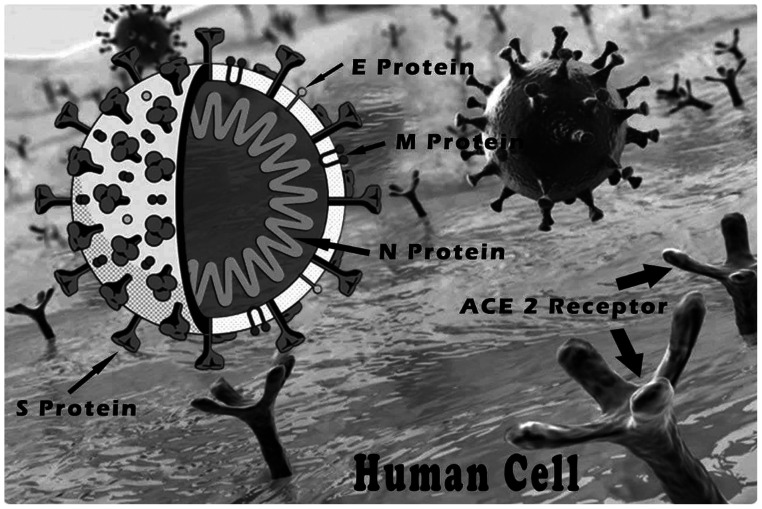
A coronavirus is an RNA virus of the Coronaviridae family.23 SARS-CoV-2 has 79% similarity with severe acute respiratory syndrome coronavirus (SARS-CoV) and 50% similarity with Middle East respiratory syndrome coronavirus (MERS-CoV).24 The basic difference between these two viruses is in the spike protein (S protein), which is much longer in SARS-CoV-2 than in SARS-CoV and MERS-CoV.24,25 The S protein in the coronavirus envelope is the most important structure for viral transmission since it mediates the binding of the virus to the host receptor on the cell surface (Fig. 1).24
Fig. 1. SARS-CoV-2 feature. The virus has 4 main structural proteins: S protein, E protein, M protein, and N protein. ACE2 receptor: angiotensin-converting enzyme 2 receptor, E protein: envelope protein, M protein: membrane protein, N protein: nucleocapside protein, SARS-CoV-2: severe acute respiratory syndrome-coronavirus-2, S protein: spike protein.
ACE2 is the main host receptor infected by this virus.24,25 This receptor has been identified in the epithelial, enterocyte, and macrophage of the respiratory tract, and in the vascular endothelium of all organs.26,27 Several studies have identified the ACE2 receptor in the brain, particularly in regions regulating cardiovascular function, such as the subfornical organ, paraventricular nucleus (PVN), solitary tract nucleus (NTS), and rostral ventrolateral medulla. The ACE2 receptor was also recently found in the motor cortex and raphe neurons.28
A neuropathological study of the brains of 20 COVID-19 patients in the USA performed by Bryce et al.29 found ACE2 to be abundantly expressed in capillaries of the lung, myocardium, and brain parenchymal. Paniz-Mondolfi et al.30 localized viral particles to small vesicles in endothelial cells of intracranial arteries and brain cells in electron microscopy. These findings support the view that the virus takes a hematogenous route to reach the brain. By infecting the ACE2-rich-endothelial cells, the virus spreads to several organs including the brain.30,31
As soon as the virus binds with the ACE2 receptor in the respiratory tract epithelial, the proteolytic domain of S protein induces membrane fusion to enable the virus to invade the host cell.24,27 In the host cell, virus RNA is released into the cytoplasm and a complex process of virus replication starts. The viral load in SARS-CoV-2 infections peaks at 5–6 days after the onset of symptom, compared to after 10 days in SARS-CoV infections.27
Like SARS-CoV and MERS-CoV, it is highly likely that SARS-CoV-2 avoids the normal immune response by interfering with the transcription of interferons, thus facilitating rapid virus replication during the initial stage of the disease.27,32 Rapid replications of the viruses cause massive pyroptosis as well as the release of IL-1β and damage-associated molecular patterns including adenosine triphosphate, nucleic acid, and ASC (apoptosis-associated speck-like protein containing a caspase recruitment domain) oligomer, which further increases the levels of proinflammatory cytokines and chemokines released into the circulation.27,32,33
High level of proinflammatory cytokines and chemokines will subsequently stimulate an abundance of inflammatory cells in the lung tissue, which in turn release very high concentration of proinflammatory cytokines—known as cytokine storms—as well as reactive oxygen species.2,27,33,34 Cytokine storms and the accumulation of the inflammatory cells will destroy the lung and increase vascular permeability,27,33 resulting in these molecules along with virus particles escaping into the circulatory system to cause sepsis, septic shock, and multiorgan damage by inducing diffuse vascular endothelial dysfunction.27
The pathological features identified in the lungs of COVID-19 patients resemble those seen in SARS-CoV and MERS-CoV, thus supporting the aforementioned theory.34,29 Diffuse alveolar damage with interstitial lymphocytic inflammation and vascular lesion resembling capillaritis was observed in the lung. Endothelial injury is evidenced by identification of platelet aggregation, intravascular fibrin thrombi, and associated microhemorrhages in small to medium-sized arteries in several organs including the lung and brain.29
PATHOMECHANISM OF STROKE IN COVID-19
Stroke in COVID-19 occurs as the result of multiple associated mechanisms. A hyperinflammatory state in the form of cytokine storms and hypercoagulability have been identified in patients with severe COVID-19. Several reports on COVID-19 with thromboembolic events including stroke and venous thromboembolism have specifically highlights elevated D-dimer as a marker of the hypercoagulability state in the patients.9,10,11,12,13,14,15,16,17,18,19,20,21,22
Most of the reported cases of stroke following SARS-CoV-2 infections are of large vessel ischemic stroke.9,10,13,15,16,17,18,19,20,21 Hemorrhagic stroke occurred in one out of five cases reported by Mao et al.,6 and one case of SAH due to rupture of aneurism in the posterior inferior cerebellar artery in a young patient with COVID-19.18 Hypercoagulability-induced thrombocytopenia may cause bleeding diathesis.35 Nonetheless, the progression of the majority of critically ill COVID-19 patients leads to death due to multi-organ failure before diathesis takes place.
Damage of the cardiovascular and cerebrovascular system related to SARS-CoV-2 infection may be attributed to the downregulation of ACE2 that follows the binding of the virus to this receptor.27 ACE2 downregulation impairs the balance of the RAS and results in uncontrolled hypertension, and may cause subsequent rupture of microaneurysms and aneurism of cerebral vessels.27 Downregulation of ACE2 also promotes inflammation, coagulation, and endothelial dysfunction.26,35,36,37 There is particularly interesting evidence from an animal study of the downregulation of ACE2 has triggered the development of atrial fibrillation.38 This mechanism could be proposed as the underlying cause of cardiac embolic stroke in COVID-19 patients.
Immunopathology, coagulopathy and endothelial dysfunction
There have been several reports of CNS pathology in COVID-19 patients, which have included vascular congestion, microthrombi infarction, and microhemorrhage as secondary major findings in addition to hypoxic-ischaemic changes (Table 3).29,30,39,40,41,42,43,44,45 Some cases with infarction in large-cerebralartery territories were identified in patients with comorbidities such as diabetes mellitus and hypertension.29,39,42 Systemic inflammatory responses, coagulopathy evidenced by elevated D-dimers, and evidence of disseminated intravascular coagulation increase the risk of stroke among these patients.31 The release of proinflammatory cytokines into the circulation also causes biochemical endothelial dysfunction and increases the risk of thrombogenesis.31 The risk is higher in COVID-19 patients given that the identification of viral particles in endothelial of cerebral arteries suggests the presence of endothelial dysfunction occurring via direct vascular endothelial injury.30
Table 3. Neuropathology findings of COVID-19 patients.
| No | Author | Country | Number of brain autopsy | Findings |
|---|---|---|---|---|
| 1 | Bryce et al.29 | USA | 20 | Microthrombi with small and patchy infarction, and parenchymal microhemorrhages in 6 patients, large infarct in MCA territory in 1 patient minimal inflammation and slight neuronal loss in 14 patients |
| 2 | Hanley et al.39 | UK | Hypoxic-ischaemic changes, moderate to intense microglial activation in 5 patients, and large infarct in MCA territory | |
| 3 | Jaunmuktane et al.40 | UK | 2 | Multifocal brain infarct and microbleeds in cortex and white matter |
| 4 | Kantonen et al.41 | Finland | 1 | Perivascular hemorrhages, parenchymal microhemorrhages, hypoxic-ischaemic changes |
| 5 | Matschke et al.42 | Germany | 43 | Acute infarct in territory PCA/MCA/ACA in 6 patients, inflammation in brainstem and cerebellum (activation of microglia and infiltration of cytotoxic T lymphocytes) |
| 6 | Paniz-Mondolfi et al.30 | USA | 1 | Identification of viral particles in small vesicles in endothelial cells of intracranial arteries and brain cells using electron microscopy |
| 7 | Remmelink et al.43 | Belgium | 17 | Cerebral hemorrhage in 8 patients, hypoxic-ischaemic changes in 3 patients, vascular congestion in 5 patients |
| 8 | Schurink et al.44 | Netherland | 9 | Hypoxic ischaemic changes in cerebrum and cerebellum, inflammation of white and grey matter, most severe in medulla oblongata and olfactory bulb |
| 9 | Solomon et al.45 | USA | 18 | Hypoxic ischaemic changes in all patients, atherosclerosis in 14 patients |
ACA: anterior cerebral artery, COVID-19: coronavirus disease 2019, MCA: middle cerebral artery, PCA: posterior cerebral artery.
An experimental model revealed the septic release of proinflammatory cytokines into the circulation, especially IL-6, inducing tissue-factor release from endothelial cells and hence initiating the coagulation cascade.46,47 The propagation of this process gives rise to systemic vascular occlusion by fibrin deposition. Simultaneously, the immunethrombosis process involving thrombin generation, platelet activation, and the formation of microthrombi occur in the circulations.36 The activation of platelets and endothelial cell release P-selectin that recruits more platelets in the circulation.46 The process is also aggravated by the expression of platelet-activating factor by activated platelet, endothelial cells, and inflammatory cells.47,48
Under normal conditions, the coagulation process remains in balance with natural anticoagulant formation. The vascular endothelium plays a vital role in the formation of the anticoagulants,49 with antithrombin, protein C, and tissue factor pathway inhibitor (TFPI) are being important anticoagulant molecules expressed by the endothelial cell. However, this system fails in immunopathology-related sepsis due to diffuse endothelial dysfunction.49
One experimental model showed that sepsis conditions reduce the level of antithrombin as a natural anticoagulant due to overconsumption.46 Endothelial damage will also decrease the production of protein C in sepsis since the production and activation of protein C depends on the binding of thrombin and thrombomodulin to the endothelial membrane. A low level of protein C in systemic inflammation is related to the suppression of the thrombomodulin expression by proinflammatory cytokines, particularly tumor necrosis factor-α (TNF-α) and IL-1β.46 The third mechanism of natural anticoagulant involves TFPI, which inhibits tissue factor/factor VIIa complex, and the TFPI expression also decreases in sepsis.46
During the initial phase of the coagulation process induced by systemic inflammation, tissue plasminogen activator (t-PA) and urokinase-type plasminogen activator (u-PA) are released by the endothelial cells.46 Both t-PA and u-PA induce plasmin formation, a molecule that degrades fibrin into fibrin degradation products.46 This acute fibrinolytic response is the reason for high-levels of D-dimer in patients with severe COVID-19 patients.9 As the disease progress, the process is inhibited by a slow but sustained increase in the release of plasminogen activator inhibitor type-1 (PAI-1) by the same endothelial cells. TNF-α and IL-1β are the main stimulators of PAI-1 release. The inhibition of fibrin degradation contributes to the worsening of coagulopathy and the thrombotic state.46,50
Downregulation of ACE2
The ACE2 receptor was first identified in 2004.51 Its role in the RAS is to cleave angiotensin II to Ang-(1-7) by acting via the Mas receptor. The ACE2-Ang-(1-7)-Mas receptor-axis balances and attenuates the ACE-angiotensin II-AT1 receptor axis.35,51
The main role of angiotensin II as a vasoconstrictor is well known. Downregulation of ACE2 augments this effect, causing uncontrolled hypertension, and may also induce rupture of cerebral microaneurysm in individuals with chronic hypertension.35 An animal-model study showed that in systemic inflammation, angiotensin II stimulation of AT1 receptor may augment coagulation and immunothrombosis by activating macrophages to release IL-6, TNF-α, and other proinflammatory cytokines, causing damage to the endothelial cells.43,44 Exposing the vascular endothelial and smooth muscle to angiotensin II also inhibits fibrinolysis by increasing PAI-1 production.37
The findings of several animal studies suggest that ACE2 plays a central role in the brain as the cardiovascular center. The action of ACE2 in the NTS may enhance the baroreflex, increase parasympathetic tone, and attenuate sympathetic tone.51 ACE2 also interferes with sympathetic activity via nitrous oxide (NO), with a study of cardiac failure in animal models demonstrating that ACE2 normalized the decrease level of NO in the PVN.51
ACE2 may play two opposing roles in SARS-CoV-2 infection: 1) acting as the main receptor for the virus to enter the host cell, and 2) acting on the ACE2-Ang-(1-7)-Mas receptor axis, which may have a protective role in the cardiovascular and cerebrovascular system. Most of the patients with severe COVID-19 are elderly and have comorbidities such as hypertension, diabetes, and cardiovascular disease.3,4,5,9,10,13,15,16,17,18,19,20,21 In such cases the baseline level of ACE2 is chronically low.35 SARS-CoV-2 infection further undermines the receptor, causing further downregulation of ACE2 and hence the failure of Ang-(1-7) to maintain an adequate balance of angiotensin II activity.35
The dual effects of ACE2 have given rise to controversies regarding the safety of ACE inhibitors and angiotensin receptor blockers (ARBs) in the treatment of hypertension and other cardiovascular diseases during the COVID-19 pandemic. The argument to stop prescribing prescription of these agents originates from the fact that the inhibition of ACE increases ACE2 expression, facilitating virus invasion into the host cell.35 On the other hand, some believe that there is no satisfactory evidence about the deleterious effect of both ACE inhibitors and ARBs in COVID-19.35 Animal model studies have reported ACE inhibitors increasing ANG-(1-7) level due to angiotensin I retention and inhibition of Ang-(1-7) metabolism. The inhibition of the AT1 receptor by ARBs interferes with the angiotensin II effect to the receptor causing inflammation and coagulation process. Studies are needed to unveil the effect and safety of those agents in COVID-19.52
MODIFICATION IN MANAGEMENT OF STROKE IN COVID-19
Screening for COVID-19 has been added to the clinical pathway of acute stroke management. The recommendation to modify code stroke to the protected code stroke is aimed to protect health care professionals from the risk of SARS-CoV-2 infection without impairing timely and precise hyperacute stroke management.53,54 Clinicians should wear the recommended personal protective equipment and comply with a universal precautions protocol whenever they are managing stroke patients.53,54 Patients without suspicion of COVID-19 are managed according to the usual stroke protocol. Suspected COVID-19 patients with fever, cough, or flu-like syndrome must be investigated using a nasopharyngeal swab to confirm the infection status, without interfering with imaging, other diagnostics methods, and therapeutic measures of stroke protocols.53,54,55
Patients with large-vessel ischemic stroke that fulfills the intravenous thrombolysis criteria should receive the procedure according to the applicable protocol.53 Endovascular treatment is recommended for stroke patients who are eligible for the procedure while the neurointerventionist and anesthesia team take specific safety procedures.56,57 Antiplatelet therapy is the main treatment modality recommended for acute-phase stroke in patients who are incompatible with either thrombolysis or endovascular treatment.55
Since the risk of thromboembolism is high in moderate and severe COVID-19, a prophylactic dose of low-molecular-weight heparin (LMWH) is recommended for all hospitalized COVID-19 patients with no identified contraindications.14,58,59 Several studies have found that administering LMWH is associated with a better prognosis and low mortality in COVID-19 patients.58,60
Anticoagulants may be considered for acute large-vessel stroke (particularly severe stenosis of the internal carotid artery) and acute stroke with nonocclusive extracranial intraluminal thrombus, although their effectiveness is still uncertain.55 Anticoagulant therapies including heparin, LMWH, thrombin inhibitor (dabigatran and argatraban), or factor Xa inhibitor (rivaroxaban, apixaban, and edoxaban) are effective in decreasing the risk of stroke in patients with comorbidity. However, their benefits in terms of minimizing disability and mortality in acute stroke have not been well established.61 Administering anticoagulants for acute ischemic stroke increase the risk of intracranial bleeding.61
The benefit of prophylactic-dose subcutaneous LMWH as prophylaxis for deep-vein thrombosis in the acute management of stroke is not well established.55 LMWH has been associated with reduced venous thromboembolism in acute stroke patients, but it has also been found to significantly increase the rate of symptomatic intracranial hemorrhage.55 Extensive studies of the effectiveness and, most importantly, the safety of anticoagulants for acute stroke management in COVID-19 are still required.
Despite published reports on the characteristic of stroke and the identification of large acute infarct in brain pathology studies of COVID-19 patients, the exact pathomechanism of stroke in COVID-19 have yet to be confirmed. Further studies are needed to clarify the exact association between stroke and COVID-19. Most of the existing data show that patients with stroke and COVID-19 have vascular and metabolic comorbidities that increase the risk of stroke.9,10,11 Whether the stroke is directly caused by the inflammatory response to COVID-19 or whether cerebrovascular events merely occur coincidentally with COVID-19 has not been well established. If coagulopathy was found to be the mechanism underlying stroke in COVID-19, future studies will need to determine the benefit and safety of anticoagulants for acute stroke.
An interesting study of statins in the stroke animal model found that in addition to their efficacy in decreasing the effects of cholesterol, statins play roles in antioxidation, anti-inflammation, vasodilatation, antithrombosis, angiogenesis, synaptogenesis, and as neural progenitors of cell migration to the infarct location.62,63,64,65 These findings suggest that statin might be beneficial in improving the outcomes of ischemic stroke, especially in large vessel stroke where inflammation and thrombosis are the underlying mechanisms. A randomized controlled trial of the administration of statins on acute ischemic stroke patient (the ASSORT trial) found that the functional outcome after 90 days of statin administration did not differ significantly between starting the therapy within 24 hours after onset with those who start after one week.66 However, that study did not exclusively include patients with large vessel stroke.66 Given that the most-likely pathophysiology of stroke in COVID-19 is an immune-response-mediated hypercoagulable state and thrombogenesis, administering statins in the acute phase is worth considering.67,68 Nevertheless, just like anticoagulants, further studies are required to evaluate the effectiveness and safety of such therapy.
CONCLUSION
Ischemic stroke is the most reported CNS manifestation in COVID-19 patients. The small amount of available data on stroke characteristics in COVID-19 shows hypercoagulability and prothrombotic state occurring in all patients. An immune response to SARS-CoV-2 infection that triggers a coagulation cascade and endothelial dysfunction is the most convincing explanation for the pathomechanism of stroke in COVID-19. Another possible explanation is downregulation of ACE2. Modification to the acute stroke management protocol is mainly aimed to protect the health-care professionals and patients while simultaneously maintaining rapid, timely and precise acute stroke care.
Administering anticoagulants and statins for acute stroke as well as the discontinuing of ACE inhibitor and ARB prescriptions for patients with cardiovascular disease remain controversial. Further investigations into the characteristics of stroke in COVID-19 and the association of these two conditions as well as other comorbidities are necessary to identify the exact pathomechanism with the aim of developing a rational, effective, and safe management strategy.
Acknowledgements
None
Footnotes
- Conceptualization: Kumara Tini, DPG Purwa Samatra.
- Data curation: Putu Lohita Rahmawati.
- Formal analysis: Putu Lohita Rahmawati, Kumara Tini, Ni Made Susilawathi.
- Funding acquisition: All authors.
- Investigation: Putu Lohita Rahmawati, IA Sri Wijayanti.
- Methodology: Ni Made Susilawathi.
- Project administration: Putu Lohita Rahmawati.
- Resources: Putu Lohita Rahmawati, IA Sri Wijayanti.
- Supervision: Kumara Tini, DPG Purwa Samatra.
- Validation: Ni Made Susilawathi.
- Visualization: Putu Lohita Rahmawati.
- Writing—original draft: Putu Lohita Rahmawati.
- Writing—review & editing: Kumara Tini, IA Sri Wijayanti.
Conflicts of Interest: The authors have no potential conflicts of interest to disclose.
References
- 1.World Health Organization. WHO Timeline - COVID-19. [Internet] Geneva: World Health Organization; [cited 2020 May 6]. Available from: https://www.who.int/news-room/detail/27-04-2020-who-timeline---covid-19. [Google Scholar]
- 2.Li X, Geng M, Peng Y, Meng L, Lu S. Molecular immune pathogenesis and diagnosis of COVID-19. J Pharm Anala. 2020;10:102–108. doi: 10.1016/j.jpha.2020.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395:497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wang D, Hu B, Hu C, Zhu F, Liu X, Zhang J, et al. Clinical characteristics of 138 hospitalized patients with 2019 novel Coronavirus-infected pneumonia in Wuhan, China. JAMA. 2020;323:1061–1069. doi: 10.1001/jama.2020.1585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zhou F, Yu T, Du R, Fan G, Liu Y, Liu Z, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395:1054–1062. doi: 10.1016/S0140-6736(20)30566-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mao L, Jin H, Wang M, Hu Y, Chen S, He Q, et al. Neurologic manifestations of hospitalized patients with Coronavirus Disease 2019 in Wuhan, China. JAMA Neurol. 2020;77:683–690. doi: 10.1001/jamaneurol.2020.1127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wu Y, Xu X, Chen Z, Duan J, Hashimoto K, Yang L, et al. Nervous system involvement after infection with COVID-19 and other coronaviruses. Brain Behav Immun. 2020;87:18–22. doi: 10.1016/j.bbi.2020.03.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Jin H, Hong C, Chen S, Zhou Y, Wang Y, Mao L, et al. Consensus for prevention and management of coronavirus disease (COVID-19) for neurologists. Stroke Vasc Neurol. 2020;5:146–151. doi: 10.1136/svn-2020-000382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Oxley TJ, Mocco J, Majidi S, Kellner CP, Shoirah H, Singh IP, et al. Large-vessel stroke as a presenting feature of COVID-19 in the young. N Engl J Med. 2020;382:e60. doi: 10.1056/NEJMc2009787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Avula A, Nalleballe K, Narula N, Sapozhnikov S, Dandu V, Toom S, et al. COVID-19 presenting as stroke. Brain Behav Immun. 2020;87:115–119. doi: 10.1016/j.bbi.2020.04.077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Beyrouti R, Adams ME, Benjamin L, Cohen H, Farmer SF, Goh YY, et al. Characteristics of ischaemic stroke associated with COVID-19. J Neurol Neurosurg Psychiatry. 2020;91:889–891. doi: 10.1136/jnnp-2020-323586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lodigiani C, Iapichino G, Carenzo L, Cecconi M, Ferrazzi P, Sebastian T, et al. Venous and arterial thromboembolic complications in COVID-19 patients admitted to an academic hospital in Milan, Italy. Thromb Res. 2020;191:9–14. doi: 10.1016/j.thromres.2020.04.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Tunç A, ÜnlübaŞ Y, Alemdar M, Akyüz E. Coexistence of COVID-19 and acute ischemic stroke report of four cases. J Clin Neurosci. 2020;77:227–229. doi: 10.1016/j.jocn.2020.05.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Dogra S, Jain R, Cao M, Bilaloglu S, Zagzag D, Hochman S, et al. Hemorrhagic stroke and anticoagulation in COVID-19. J Stroke Cerebrovasc Dis. 2020;29:104984. doi: 10.1016/j.jstrokecerebrovasdis.2020.104984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Co COC, Yu JRT, Laxamana LC, David-Ona DIA. Intravenous thrombolysis for stroke in a COVID-19 positive Filipino patient, a case report. J Clin Neurosci. 2020;77:234–236. doi: 10.1016/j.jocn.2020.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gunasekaran K, Amoah K, Rajasurya V, Buscher MG. Stroke in a young COVID-19 patient. QJM. 2020;113:573–574. doi: 10.1093/qjmed/hcaa177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Fara MG, Stein LK, Skliut M, Morgello S, Fifi JT, Dhamoon MS. Macrothrombosis and stroke in patients with mild COVID-19 infection. J Thromb Haemost. 2020;18:2031–2033. doi: 10.1111/jth.14938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Al Saiegh F, Ghosh R, Leibold A, Avery MB, Schmidt RF, Theofanis T, et al. Status of SARS-CoV-2 in cerebrospinal fluid of patients with COVID-19 and stroke. J Neurol Neurosurg Psychiatry. 2020;91:846–848. doi: 10.1136/jnnp-2020-323522. [DOI] [PubMed] [Google Scholar]
- 19.Saggese CE, Del Bianco C, Di Ruzza MR, Magarelli M, Gandini R, Plocco M. COVID-19 and stroke: casual or causal role. Cerebrovasc Dis. 2020;49:341–344. doi: 10.1159/000509453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Zhai P, Ding Y, Li Y. The impact of COVID-19 on ischemic stroke. Diagn Pathol. 2020;15:78. doi: 10.1186/s13000-020-00994-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Goldberg MF, Goldberg MF, Cerejo R, Tayal AH. Cerebrovascular disease in COVID-19. AJNR Am J Neuroradiol. 2020;41:1170–1172. doi: 10.3174/ajnr.A6588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Yaghi S, Ishida K, Torres J, Mac Grory B, Raz E, Humbert K, et al. SARS-CoV-2 and stroke in a New York healthcare system. Stroke. 2020;51:2002–2011. doi: 10.1161/STROKEAHA.120.030335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Su S, Wong G, Shi W, Liu J, Lai ACK, Zhou J, et al. Epidemiology, genetic recombination, and pathogenesis of coronaviruses. Trends Microbiol. 2016;24:490–502. doi: 10.1016/j.tim.2016.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lu R, Zhao X, Li J, Niu P, Yang B, Wu H, et al. Genomic characterisation and epidemiology of 2019 novel coronavirus: implications for virus origins and receptor binding. Lancet. 2020;395:565–574. doi: 10.1016/S0140-6736(20)30251-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Rothan HA, Byrareddy SN. The epidemiology and pathogenesis of coronavirus disease (COVID-19) outbreak. J Autoimmun. 2020;109:102433. doi: 10.1016/j.jaut.2020.102433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hamming I, Timens W, Bulthuis ML, Lely AT, Navis G, van Goor H. Tissue distribution of ACE2 protein, the functional receptor for SARS coronavirus. A first step in understanding SARS pathogenesis. J Pathol. 2004;203:631–637. doi: 10.1002/path.1570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Tay MZ, Poh CM, Rénia L, MacAry PA, Ng LFP. The trinity of COVID-19: immunity, inflammation and intervention. Nat Rev Immunol. 2020;20:363–374. doi: 10.1038/s41577-020-0311-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Xia H, Lazartigues E. Angiotensin-converting enzyme 2 in the brain: properties and future directions. J Neurochem. 2008;107:1482–1494. doi: 10.1111/j.1471-4159.2008.05723.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Bryce C, Grimes Z, Pujadas E, Ahuja S, Beasley MB, Albrecht R, et al. Pathophysiology of SARS-CoV-2: targeting of endothelial cells renders a complex disease with thrombotic microangiopathy and aberrant immune response. The Mount Sinai COVID-19 autopsy experience. medRxiv; 2020. May 22, [Preprint]. Available from: [DOI] [Google Scholar]
- 30.Paniz-Mondolfi A, Bryce C, Grimes Z, Gordon RE, Reidy J, Lednicky J, et al. Central nervous system involvement by Severe Acute Respiratory Syndrome Coronavirus-2 (SARS-CoV-2) J Med Virol. 2020;92:699–702. doi: 10.1002/jmv.25915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Al-Sarraj S, Troakes C, Hanley B, Osborn M, Richardson MP, Hotopf M, et al. Invited review: the spectrum of neuropathology in COVID-19. Neuropathol Appl Neurobiol; 2020. Sep 16, [Epub]. Available from: [DOI] [PubMed] [Google Scholar]
- 32.de Wit E, van Doremalen N, Falzarano D, Munster VJ. SARS and MERS: recent insights into emerging coronaviruses. Nat Rev Microbiol. 2016;14:523–534. doi: 10.1038/nrmicro.2016.81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Channappanavar R, Perlman S. Pathogenic human coronavirus infections: causes and consequences of cytokine storm and immunopathology. Semin Immunopathol. 2017;39:529–539. doi: 10.1007/s00281-017-0629-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Xu Z, Shi L, Wang Y, Zhang J, Huang L, Zhang C, et al. Pathological findings of COVID-19 associated with acute respiratory distress syndrome. Lancet Respir Med. 2020;8:420–422. doi: 10.1016/S2213-2600(20)30076-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Verdecchia P, Cavallini C, Spanevello A, Angeli F. The pivotal link between ACE2 deficiency and SARS-CoV-2 infection. Eur J Intern Med. 2020;76:14–20. doi: 10.1016/j.ejim.2020.04.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Bernstein KE, Khan Z, Giani JF, Cao DY, Bernstein EA, Shen XZ. Angiotensin-converting enzyme in innate and adaptive immunity. Nat Rev Nephrol. 2018;14:325–336. doi: 10.1038/nrneph.2018.15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Mehta PK, Griendling KK. Angiotensin II cell signaling: physiological and pathological effects in the cardiovascular system. Am J Physiol Cell Physiol. 2007;292:C82–C97. doi: 10.1152/ajpcell.00287.2006. [DOI] [PubMed] [Google Scholar]
- 38.Pan CH, Lin JL, Lai LP, Chen CL, Stephen Huang SK, Lin CS. Downregulation of angiotensin converting enzyme II is associated with pacing-induced sustained atrial fibrillation. FEBS Lett. 2007;581:526–534. doi: 10.1016/j.febslet.2007.01.014. [DOI] [PubMed] [Google Scholar]
- 39.Hanley B, Naresh KN, Roufosse C, Nicholson AG, Weir J, Cooke GS, et al. Histopathological findings and viral tropism in UK patients with severe fatal COVID-19: a post-mortem study. Lancet Microbe. 2020;1:e245–e253. doi: 10.1016/S2666-5247(20)30115-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Jaunmuktane Z, Mahadeva U, Green A, Sekhawat V, Barrett NA, Childs L, et al. Microvascular injury and hypoxic damage: emerging neuropathological signatures in COVID-19. Acta Neuropathol. 2020;140:397–400. doi: 10.1007/s00401-020-02190-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Kantonen J, Mahzabin S, Mäyränpää MI, Tynninen O, Paetau A, Andersson N, et al. Neuropathologic features of four autopsied COVID-19 patients. Brain Pathol. 2020;30:1012–1016. doi: 10.1111/bpa.12889. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Matschke J, Lütgehetmann M, Hagel C, Sperhake JP, Schröder AS, Edler C, et al. Neuropathology of patients with COVID-19 in Germany: a post-mortem case series. Lancet Neurol. 2020;19:919–929. doi: 10.1016/S1474-4422(20)30308-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Remmelink M, De Mendoca R, D'Haene N, De Clercq S, Verocq C, Lebrun L, et al. Unspecific post-mortem findings despite multiorgan viral spread in COVID-19 patients. medRxiv; 2020. May 28, [Preprint]. Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Schurink B, Roos E, Radonic T, Barbe E, Bouman CSC, de Boer HH, et al. Viral presence and immunopathology in patients with lethal COVID-19: a prospective autopsy cohort study. Lancet Microbe. 2020;1:e290–e299. doi: 10.1016/S2666-5247(20)30144-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Solomon IH, Normandin E, Bhattacharyya S, Mukerji SS, Keller K, Ali AS, et al. Neuropathological features of COVID-19. N Engl J Med. 2020;383:989–992. doi: 10.1056/NEJMc2019373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Levi M, van der Poll T, Büller HR. Bidirectional relation between inflammation and coagulation. Circulation. 2004;109:2698–2704. doi: 10.1161/01.CIR.0000131660.51520.9A. [DOI] [PubMed] [Google Scholar]
- 47.Assinger A, Schrottmaier WC, Salzmann M, Rayes J. Platelets in sepsis: an update on experimental models and clinical data. Front Immunol. 2019;10:1687. doi: 10.3389/fimmu.2019.01687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Cox D, Kerrigan SW, Watson SP. Platelets and the innate immune system: mechanisms of bacterial-induced platelet activation. J Thromb Haemost. 2011;9:1097–1107. doi: 10.1111/j.1538-7836.2011.04264.x. [DOI] [PubMed] [Google Scholar]
- 49.Bazaz R, Marriott HM, Francis SE, Dockrell DH. Mechanistic links between acute respiratory tract infections and acute coronary syndromes. J Infect. 2013;66:1–17. doi: 10.1016/j.jinf.2012.09.009. [DOI] [PubMed] [Google Scholar]
- 50.Schouten M, Wiersinga WJ, Levi M, van der Poll T. Inflammation, endothelium, and coagulation in sepsis. J Leukoc Biol. 2008;83:536–545. doi: 10.1189/jlb.0607373. [DOI] [PubMed] [Google Scholar]
- 51.Xia H, Lazartigues E. Angiotensin-converting enzyme 2: central regulator for cardiovascular function. Curr Hypertens Rep. 2010;12:170–175. doi: 10.1007/s11906-010-0105-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Ferrario CM, Trask AJ, Jessup JA. Advances in biochemical and functional roles of angiotensin-converting enzyme 2 and angiotensin-(1-7) in regulation of cardiovascular function. Am J Physiol Heart Circ Physiol. 2005;289:H2281–H2290. doi: 10.1152/ajpheart.00618.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Khosravani H, Rajendram P, Notario L, Chapman MG, Menon BK. Protected code stroke: hyperacute stroke management during the Coronavirus Disease 2019 (COVID-19) pandemic. Stroke. 2020;51:1891–1895. doi: 10.1161/STROKEAHA.120.029838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Baracchini C, Pieroni A, Viaro F, Cianci V, Cattelan AM, Tiberio I, et al. Acute stroke management pathway during Coronavirus-19 pandemic. Neurol Sci. 2020;41:1003–1005. doi: 10.1007/s10072-020-04375-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Powers WJ, Rabinstein AA, Ackerson T, Adeoye OM, Bambakidis NC, Becker K, et al. Guidelines for the early management of patients with acute ischemic stroke: 2019 update to the 2018 Guidelines for the early management of acute ischemic stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2019;50:e344–e418. doi: 10.1161/STR.0000000000000211. [DOI] [PubMed] [Google Scholar]
- 56.Smith MS, Bonomo J, Knight WA, 4th, Prestigiacomo CJ, Richards CT, Ramser E, et al. Endovascular therapy for patients with acute ischemic stroke during the COVID-19 pandemic: a proposed algorithm. Stroke. 2020;51:1902–1909. doi: 10.1161/STROKEAHA.120.029863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Sharma D, Rasmussen M, Han R, Whalin MK, Davis M, Kofke WA, et al. Anesthetic management of endovascular treatment of acute ischemic stroke during COVID-19 pandemic: consensus statement from Society for Neuroscience in Anesthesiology & Critical Care (SNACC) J Neurosurg Anesthesiol. 2020;32:193–201. doi: 10.1097/ANA.0000000000000688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Thachil J, Tang N, Gando S, Falanga A, Cattaneo M, Levi M, et al. ISTH interim guidance on recognition and management of coagulopathy in COVID-19. J Thromb Haemost. 2020;18:1023–1026. doi: 10.1111/jth.14810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Vivas D, Roldán V, Esteve-Pastor MA, Roldán I, Tello-Montoliu A, Ruiz-Nodar JM, et al. Recommendations on antithrombotic treatment during the COVID-19 pandemic. Position statement of the working group on cardiovascular thrombosis of the Spanish Society of Cardiology. Rev Esp Cardiol. 2020;73:749–757. doi: 10.1016/j.rec.2020.04.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Tang N, Bai H, Chen X, Gong J, Li D, Sun Z. Anticoagulant treatment is associated with decreased mortality in severe coronavirus disease 2019 patients with coagulopathy. J Thromb Haemost. 2020;18:1094–1099. doi: 10.1111/jth.14817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Sandercock PA, Counsell C, Kane EJ. Anticoagulants for acute ischaemic stroke. Cochrane Database Syst Rev. 2015;2015:CD000024. doi: 10.1002/14651858.CD000024.pub4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Amin-Hanjani S, Stagliano NE, Yamada M, Huang PL, Liao JK, Moskowitz MA. Mevastatin, an HMG-CoA reductase inhibitor, reduces stroke damage and upregulates endothelial nitric oxide synthase in mice. Stroke. 2001;32:980–986. doi: 10.1161/01.str.32.4.980. [DOI] [PubMed] [Google Scholar]
- 63.Sironi L, Cimino M, Guerrini U, Calvio AM, Lodetti B, Asdente M, et al. Treatment with statins after induction of focal ischemia in rats reduces the extent of brain damage. Arterioscler Thromb Vasc Biol. 2003;23:322–327. doi: 10.1161/01.atv.0000044458.23905.3b. [DOI] [PubMed] [Google Scholar]
- 64.Kawashima S, Yamashita T, Miwa Y, Ozaki M, Namiki M, Hirase T, et al. HMG-CoA reductase inhibitor has protective effects against stroke events in stroke-prone spontaneously hypertensive rats. Stroke. 2003;34:157–163. doi: 10.1161/01.str.0000048213.18751.52. [DOI] [PubMed] [Google Scholar]
- 65.Berger C, Xia F, Maurer MH, Schwab S. Neuroprotection by pravastatin in acute ischemic stroke in rats. Brain Res Rev. 2008;58:48–56. doi: 10.1016/j.brainresrev.2007.10.010. [DOI] [PubMed] [Google Scholar]
- 66.Yoshimura S, Uchida K, Daimon T, Takashima R, Kimura K, Morimoto T, et al. Randomized controlled trial of early versus delayed statin therapy in patients with acute ischemic stroke: ASSORT trial (administration of statin on acute ischemic stroke patient) Stroke. 2017;48:3057–3063. doi: 10.1161/STROKEAHA.117.017623. [DOI] [PubMed] [Google Scholar]
- 67.Tan WYT, Young BE, Lye DC, Chew DEK, Dalan R. Statin use is associated with lower disease severity in COVID-19 infection. Sci Rep. 2020;10:17458. doi: 10.1038/s41598-020-74492-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Rossi R, Talarico M, Coppi F, Boriani G. Protective role of statins in COVID 19 patients: importance of pharmacokinetic characteristics rather than intensity of action. Intern Emerg Med. 2020;15:1573–1576. doi: 10.1007/s11739-020-02504-y. [DOI] [PMC free article] [PubMed] [Google Scholar]