Abstract
Background and Purpose
Migraine is a complex neurovascular disorder whose triggers are not entirely understood. Endothelial dysfunction might play a role in migraine, and there have been numerous reports on endothelium dysfunction and migraine pathophysiology, but their reciprocal cause–effect relationship remains unclear. This review reports the current evidence on endothelium dysfunction, its link with migraine, and its possible consequences for cerebral hemodynamics.
Methods
We performed a systematic literature search of PubMed up to March 2020. We included 115 articles in a narrative review.
Results
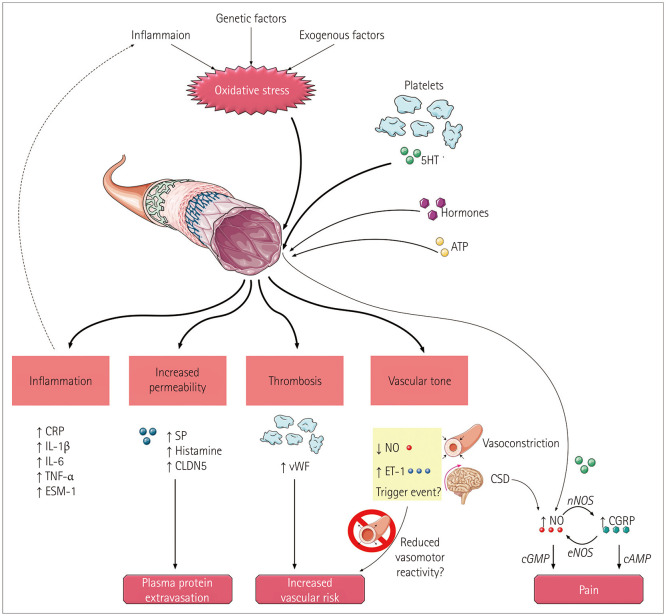
Several studies have demonstrated that endothelium dysfunction may play an important role in migraine. Despite the lack of specific biomarkers, there is evidence of oxidative stress and inflammation—two of the primary causes of endothelial damage—in migraine. The main consequences of endothelial dysfunction are increased vascular tone, thrombosis, inflammation, and increased vascular permeability. As a consequence of oxidative stress, the activity of endothelin-1 is not counterbalanced by nitric oxide (NO), whose levels decrease to lead to vasoconstriction and a possible contribution to cortical spreading depression. NO is involved in pain perception via the cyclic guanosine monophosphate (cGMP) pathway and the induction of calcitonin gene-related peptide. Oxidative stress may induce a hypercoagulable state that mainly affects platelet function through different mechanisms. Endothelial dysfunction seems to be particularly pronounced in migraine with aura (MA). Endothelial dysfunction in migraine particularly involves intracranial vessels, since flow-mediated dilation cannot detect overt peripheral vascular dysfunction.
Conclusions
Endothelial dysfunction is a vascular risk marker. How it impacts migraine, and particularly MA, needs to be understood better by defining its possible role in increasing the stroke risk in migraine patients.
Keywords: hypercoagulability, inflammation, thrombosis, vasoconstriction, vasodilatation
INTRODUCTION
Migraine is a chronic neurological disease characterized by a complex set of symptoms and multifactorial pathophysiology. Although the trigger factors for migraine have not been completely determined, the acknowledged pivotal mechanisms are well defined. Migraine with aura (MA) is the result of a cortical perfusion disturbance defined as cortical spreading depression (CSD), while the head and facial pain and accompanying symptoms result from the activation of the trigeminovascular system.1 Interactions among these different components gave rise to the concept of migraine as a neurovascular disorder.
The vascular involvement in migraine certainly includes the dura vessels, whose dilation and perivascular inflammation generate the typical pulsatile pain. Moreover, a perturbation of the cortical circulation takes place during CSD, when hyperemia precedes the oligemic phase. Substances with vasodilatory effects may trigger migraine attacks, and a recent meta-analysis of susceptibility genes for migraine pointed out that migraine-associated genes are expressed in vascular and smooth-muscle tissues.2 There is increasing evidence for the involvement of intracerebral vessels in migraine. This is of particular interest since it might explain two unclear aspects: 1) the triggers of migraine and 2) the links between migraine and stroke (i.e., reciprocal causality or the expression of a shared pathogenic mechanism).
The endothelium has been linked to migraine, but it is not clear whether 1) endothelial dysfunction is a migraine trigger or a migraine chronicization factor, or 2) endothelial dysfunction is a consequence of migraine. Moreover, it remains to be determined whether endothelial dysfunction increases the stroke risk in migraineurs. Addressing this last point could impact clinical stroke prevention.
This review reports the current evidence of endothelial dysfunction, its implication in migraine, and its consequences for cerebral and systemic hemodynamics.
METHODS
We performed a systematic literature search of PubMed to identify studies published up to March 2020 using the following search terms: “endothelial dysfunction” AND “migraine,” “endothelial function” AND “migraine,” and “endothelium” AND “migraine.” We then selected studies based on their title and Abstract. Reference lists of selected articles were also screened to identify any studies that had been missed in the original search process.
Our preliminary search and subsequent analysis of the reference lists of selected articles revealed 283 relevant studies. We excluded 111 of these articles based on their title and Abstract. The remaining 172 articles comprised 51 reviews and 120 original papers. After reading the full texts, we excluded 28 reviews because their source data were already included in other articles or had been superseded by more-recent reviews, and 29 original articles due to repetition of results already reported elsewhere, or work not primarily involving migraine or endothelial function/dysfunction. The present review finally included 115 articles.
RESULTS
Endothelial dysfunction
The endothelium is the inner layer of blood vessels that acts not only as a barrier between the blood and extravascular space, but also as an active endocrine organ. Its large surface area means that it plays a central role in multiple functions. As an endocrine organ, it produces various paracrine substances mediating vascular permeability, vascular tone, local inflammation, and thrombosis.3 Apart from producing these substances, the endothelium also interacts with and inactivates circulating substances.
The large number of different substances released by the endothelium include nitric oxide (NO), endothelin-1 (ET-1), von Willebrand factor (vWF), plasminogen activator inhibitor-1, angiotensin II, prostacyclin, platelet-activating factor, homocysteine, and adrenomedullin (AM). These substances influence the contraction of smooth-muscle cells (SMC), both pro- and anticoagulation, thrombus lysis or formation, and oxidative stress. The homeostasis of the endothelium is maintained by balanced actions of substances with opposing functions. This balance may be lost when the endothelium is damaged by mechanisms related to vascular risk factors or genetic or exogenous factors, resulting in so-called endothelial dysfunction. Endothelial dysfunction can at last lead to vasoconstriction, increased permeability, inflammation, and a prothrombotic profile (Fig. 1).
Fig. 1. Proposed mechanism of endothelial dysfunction in migraine pathophysiology. Oxidative stress and other endogenous and exogenous factors may lead to endothelium dysfunction, consequently sustaining the induction of pain and possibly increasing the vascular risk via alterations of vascular tone and hypercoagulability. ATP: adenosine triphosphate, cAMP: cyclic adenosine monophosphate, cGMP: cyclic guanosine monophosphate, cGRP: calcitonin-gene-related peptide, CLDN5: claudin-5, CRP: C-reactive protein, CSD: cortical spreading depression, eNOS: endothelial nitric oxide synthase, ESM-1: endocan, ET-1: endothelin-1, IL-1β: interleukin 1β, IL-6: interleukin 6, nNOS: neuronal nitric oxide synthase, NO: nitric oxide, TNF-α: tumor necrosis factor-α, SP: substance P, vWF: von Willebrand factor, 5HT: serotonin.
Causes and detection of endothelial damage
The endothelium of migraine patients, especially those with MA, may be exposed to multiple potentially damaging factors.
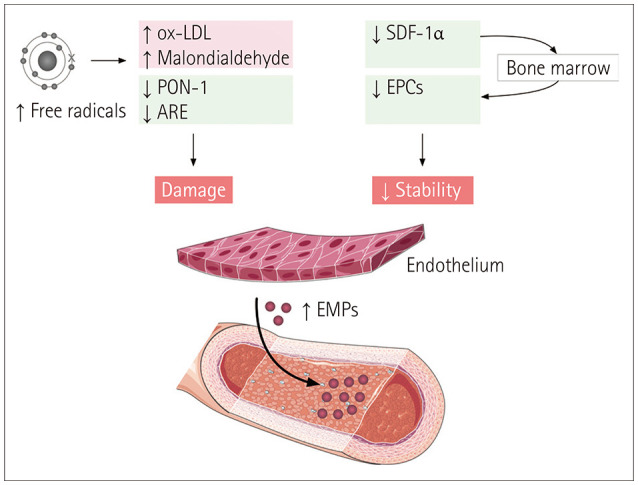
Oxidative stress is the leading cause of endothelial dysfunction. The process of oxidation occurs when a free radical (i.e., a molecule that contains unpaired electrons, and hence is unstable) donates or removes an electron from another molecule, which itself becomes a radical in a chain reaction.4 Oxidative stress results from an imbalance between the production of reactive oxygen species (ROS) and nonradicals. The resultant oxidation of biomolecules and the associated disruption of their standard functioning may lead to tissue damage. Excess levels of free radicals may oxidize low-density lipoprotein (LDL), and the resultant ox-LDL impairs the functioning of the endothelium. Oxidative stress in migraineurs has been demonstrated by measurements of higher levels of ox-LDL and malondialdehyde (the end product of lipid peroxidation, and hence an indicator of oxidative stress) and reduced activity of antioxidant enzymes such as paraoxonase-1 and arylesterase (Fig. 2).5,6 It has even been hypothesized that migraine could be a restorative reaction of the brain to oxidative stress, inducing a complex antioxidizing response.7
Fig. 2. Damage and loss of stability of endothelium lead to the release of endothelial microparticles (EMPs). ARE: arylesterase, EPCs: endothelial progenitor cells, ox-LDL: oxidized low-density lipoprotein, PON-1: paraoxonase-1, SDF-1α: stromal-cell-derived factor-1α.
Inflammation and immunity may also damage the endothelium, acting on it both directly and indirectly. Indeed, inflammation sustains oxidative stress, whereby high levels of reactive species are produced during an inflammatory process.4 Similarly, inflammation is one of the consequences of oxidative stress (both in general and as a result of oxidation-mediated endothelial dysfunction). It is difficult to determine which is the primary process, since oxidative stress and inflammation act simultaneously. Migraine patients may exhibit a genetic susceptibility to a proinflammatory state. Indeed, migraineurs (and particularly female MA patients) showed an association with a polymorphism of tumor necrosis factor (TNF) gene that may enhance the production of TNF, for which the endothelium is a primary target.8 An inflammatory state in migraineurs is also attested by the higher erythrocyte sedimentation rates and C-reactive protein (CRP) levels found in episodic and chronic migraine (CM) patients, which are correlated with the carotid intima-media thickness.9,10 Excessive interactions between T-helper lymphocytes and endothelium, as indicated by the overexpression of integrins, suggests an immunological mechanism of endothelial activation.11 Lymphocytes and endothelium are also targets of activated platelets, whose levels were elevated in migraine patients,12 although the activation of platelets could be a phenomenon secondary to migraine and endothelial dysfunction rather than being their cause.13 There has also been a report of the rate of antibodies directed against endothelium being higher in migraine patients than in controls.14
Another endothelial detrimental factor may be homocysteine. MA patients often present with elevated homocysteine, which is due to the higher frequency of polymorphism of the methylenetetrahydrofolate reductase (MTHFR) gene.15
On the other hand, the endothelium is also the target of protective angiogenic factors such as vascular endothelial growth factor (VEGF) and angiogenin, which are depleted in migraineurs during the interictal period.16 Notably, another study found that the levels of VEGF were higher in migraine patients during the interictal period than in controls.17
This imbalance between protective and detrimental factors may lead to damage to the endothelium. Since endothelial dysfunction is a complex phenomenon involving several factors, it would be useful to find a precise marker of damage (Table 1).
Table 1. Candidate biomarkers of endothelium dysfunction in migraine.
| Marker | Mechanism | Possible validity | References |
|---|---|---|---|
| EPC | Endothelium stability | + | Decreased17,20 |
| CD62E (EPCs/EMPs) | Endothelium activation | + | Increased21,22 |
| SDF-1α | Mobilization of EPC from bone marrow | + | Decreased22 |
| EMPs | Endothelial dysfunction | + | Increased22,24 |
| VEGF | Protective angiogenic factor | – | Decreased,16 increased17 |
| CRP | Inflammation marker | + | Increased,9,10,64,107 unaltered26 |
| TNF | Proinflammatory cytokine | – | Unaltered,26 increased108 |
| Cytokines (IL-1, IL-6) | Proinflammatory | + | Increased 26,108 |
| PTX3 | Proinflammatory | – | Increased26,27 |
| sTWEAK | Endothelial dysfunction, regulates BBB permeability | – | Increased26,27 |
| Endocan (ESM-1) | Endothelial-cell-specific molecule | – | Increased108 |
| Claudin-5 | Regulates BBB permeability | – | Increased108 |
| Urine albumin leakage | Endothelial dysfunction | – | Unaltered28 |
| Homocysteine | Endothelial damage | – | Increased15 |
| ET-1 | Endothelium-dependent vasoconstriction | + | Increased39,40,41,42 |
| NO | Endothelium-dependent vasodilatation | – | Decreased,58 unaltered,59,60 increased65 |
| Urine nitrate/nitrite | Bioavailability of NO | – | Decreased64 |
| ADMA | NOS inhibitor | + | Increased65,66 |
| FMD | Endothelium-dependent vasodilatation | – | Decreased,9,68,71,72 unaltered,17,41,60,70 increased 69,73,74 |
| vWF | Platelet adhesion | + | Increased 10,64,109,110,111,112 |
| Platelet function (different indexes) | Platelet activation | + | Increased aggregates,12 decreased clot time111,113 |
| Fibrinogen | Coagulation | + | Increased107 |
| Thrombin | Coagulation | + | Increased107 |
ADMA: asymmetric dimethylarginine, BBB: blood–brain barrier, CRP: C-reactive protein, EMPs: endothelial microparticles, EPCs: endothelial progenitor cells, ESM-1: endothelial cell-specific molecule 1, ET-1: endothelin-1, FMD: flow-mediated dilation, IL: interleukin, NO: nitric oxide, NOS: NO synthase, PTX3: pentraxin 3, SDF-1α: stromal-cell-derived factor-1α, sTWEAK: soluble TNF weak inducers of apoptosis, TNF: tumor necrosis factor, VEGF: vascular endothelial growth factor, vWF: von Willebrand factor.
Circulating endothelial progenitor cells (EPCs) are a marker of endothelial stability. A decreased number of EPCs indicates the low replacement of damaged endothelial cells and is negatively correlated with the cardiovascular risk,18 and it is also related to inflammatory conditions characterized by higher levels of circulating proinflammatory cytokines.19 A lower number of circulating EPCs has been demonstrated in migraineurs, especially in those with MA.17,20 A more-thorough analysis of EPCs demonstrated that the number of CD62E+EPCs—which is a marker of endothelial activation—was larger in chronic and episodic migraineurs than in controls, hence indicating more mature EPCs that are potentially associated with endothelial damage.21
Stromal-cell-derived factor-1α (SDF-1α) is the most-potent chemoattractant for EPCs, inducing the mobilization of EPCs from bone marrow. A study found reduced levels of SDF-1α in migraine patients, indicating reduced mobilization of bone-marrow-derived EPCs and, as a consequence, endothelial dysfunction.22 That study also demonstrated a negative correlation between SDF-1α and CD62E+ endothelial microparticles (EMPs), which are another marker of endothelial dysfunction. EMPs are vesicles released from the endothelium in response to endothelial activation or injury (i.e., triggered by hypoxia, TNF-α, CRP, and thrombin), with higher circulating levels correlating with higher degrees of dysfunction, mainly due to the impairment of endothelium-dependent NO-mediated vasodilatation23 (Fig. 2). Female MA patients showed higher levels of circulating EMPs compared with controls.24
Other circulating endothelial markers (angiopoietin-1, angiopoietin-2, the tyrosine kinase receptor Tie-2, soluble fmslike tyrosine kinase-1, and N-terminal prohormone of brain natriuretic peptide) have not been found to be correlated with migraine,25 while the serum levels of pentraxin 3 and soluble TNF-like weak inducers of apoptosis were higher in CM patients and showed a correlation with iron deposition in certain regions of the brain.26,27
Flow-mediated dilation (FMD) and tonometry have been used to identify peripheral endothelial dysfunction, as described in the following section.
Urine albumin leakage is considered another marker of peripheral endothelial dysfunction. However, a large study of migraine patients found no evidence of increased urine albumin leakage in migraine patients.28
Endothelial dysfunction and vascular tone in migraine
Vasoconstriction is a typical outcome of endothelial dysfunction.29 Among all of the endothelium products, NO is the leading regulator of vessel tone: it is a potent vasodilator, responsible for endothelium-dependent vasodilatation. Oxidative stress, one of the known mechanisms of endothelial dysfunction, reduces the bioavailability of NO since the latter readily reacts with ROS when the antioxidant system is exhausted. Since this causes an imbalance in vascular tone, the levels of substances such as ET-1 and angiotensin II become excessive so as to lead to vasoconstriction.
NO and ET-1
The production of NO is catalyzed by the NO synthase (NOS) enzyme, oxidating intracellular L-arginine. There are three distinct isoforms of NOS: neuronal NOS (nNOS), endothelial NOS (eNOS), and inducible NOS (iNOS).30 NO synthesized in the endothelium by the action of eNOS mediates endothelium-dependent vasodilatation. The release of NO from the endothelium is stimulated by several substances, such as serotonin (5HT), histamine, bradykinin, ET-1, and substance P (SP), as well as by shear stress.31,32 5HT, in particular, may induce the release of NO from the endothelium by acting on 5HT2B receptors.33 Calcitonin-gene-related peptide (CGRP), whose release from perivascular nerves is induced by NO donors themselves34 and by nNOS-produced NO from the trigeminal ganglion,30 can also sustain NO release from the endothelium, acting on eNOS both directly and indirectly.35 The blockade of eNOS inhibits the CGRP-induced vasodilatation of dural vessels.36 Once released from the endothelium, eNOS-derived NO diffuses to the SMC where it activates the intracellular cGMP pathway, inducing vasodilatation by reducing intracellular Ca2+ levels.
Endothelial NO interacts with its vasoconstrictive counterpart, ET-1, in a complicated manner, with the interplay of these two substances being critical for regulating vascular tone. NO plays the leading role in tone regulation, tonically inhibiting ET-1 activity via several pathways.37 When broken free from direct NO inhibition, ET-1 activity is in any case controlled by a negative feedback mechanism via endothelial ET-1B1 receptors, which induces eNOS activity to increase NO production and prevent excessive ET-1 activity. However, oxidative stress and other conditions that reduce the availability of NO may result in uncontrolled activation of the ET-1 pathway.
ET-1 could play an important role as a migraine trigger.38 Its levels are elevated in MA and migraine without aura (MO) patients during the interictal period39,40,41 and also in the early phase of a migraine attack.39,42 Moreover, ET-1 is directly involved in nociception and induces the release of migraine-provoking substances.38,43
A particularly interesting finding from animal studies is that topical cortical application of ET-1 can induce CSD in rats.44,45 In contrast, intravenous ET-1 infusion in patients with MA did not provoke any aura attack,46 which might have been due to the minimal passage of ET-1 through the blood–brain barrier (BBB). The hypothesis of a CSD-inducing effect of ET-1 therefore remains to be validated by evaluating the concomitant opening of BBB or a more-local effect (paracrine or autocrine).
The potential role in triggering CSD would place ET-1 at an upstream position in the pathological chain of migraine induction. CGRP and the NO donor glyceryl trinitrate seem to act downstream, respectively activating the cAMP and cGMP pathways since they can induce MO attacks in patients with MA.47,48,49 Furthermore, animal studies suggest that NO release can be induced by CSD.50,51 It is worth noting that pretreatment with sumatriptan reduces the CSD-induced release of NO,52 and so NO seems to be mostly involved in pain induction during a migraine attack. A small pilot trial showed the efficacy of a NOS inhibitor in providing significant headache relief during a spontaneous migraine attack.53,54 The action of NO on pain induction is not limited to its effect on vascular tone, but also in activating the trigeminal system.55 eNOS and nNOS are to a greater extent localized in the trigeminal ganglion.30 When administered to migraine patients, exogenous NO donors can induce both immediate and delayed headaches: the immediate headache is probably due to a direct effect on vascular muscular tone (cGMP-mediated vasodilatation), whereas the delayed headache could be due to the trigeminovascular activation, primarily through CGRP56 and pituitary adenylyl-cyclase activating polypeptide (PACAP) release (mainly via nNOS induction30) or mast-cell activation (via iNOS induction30), which in turn induces endothelial cells to release adenosine triphosphate (ATP) that activates perivascular nociceptors.57
Increased levels of oxidative stress and consequential reduced bioavailability of NO have been described during and after migraine attacks.58 Conversely, no baseline alterations of plasmatic NO metabolites were found during the interictal period.59,60 Similarly, no difference was found in the NO-mediated peripheral endothelium-dependent vasodilatation during the interictal period,61,62 also when vascular smooth-muscle cells (VSMC) may lose their sensitivity to the endothelial NO that is normally produced during the interictal period and regain sensitivity during a migraine attack.63 However, a larger study found decreased urinary total nitrate/nitrite levels during the interictal period in female migraine patients.64 This decrease was greater in MA patients and was correlated with headache duration, thus indicating greater endothelial dysfunction in this population.
Another study found that the levels of NO and asymmetric dimethylarginine (ADMA, a NOS inhibitor indicative of oxidative stress) during both a migraine attack and the interictal period were higher in patients with migraine than in a control group.65 Increased ADMA levels during the interictal period in migraine patients were confirmed in another study, where they were also predictive of white-matter lesions (WMLs).66 The migraine patients with WMLs in that study also showed higher symmetric dimethylarginine (SDMA) concentrations, which may reduce NO production from L-arginine; L-arginine levels were higher in all migraine patients than in controls, probably reflecting an increased demand for NO synthesis.66
Hence, despite NO levels failing to serve as a biomarker, the dynamic variations of NO metabolism—particularly during a migraine attack—reflect a pathophysiological mechanism induced by endothelial dysfunction: NOS inhibition and reduced NO availability are counterbalanced by increased levels of L-arginine and the NO sensitivity of VSMC. While a decrease in NO availability may be a triggering factor, the restoration of NO levels (sustained in part by CSD) is crucial for pain induction both directly and via the CGRP pathway.
FMD and arterial tonometry
A functional way to assess NO-mediated endothelium-dependent vasodilatation is using the FMD-based technique, in which the increase in the diameter of the brachial artery is measured after occluding the vessel for 5 minutes. After the occlusion, reactive hyperemia induces the release of NO, with correspondent vasodilatation. A review by Butt et al.67 that excluded studies comprising less than 20% of MA patients and those with CM produced conflicting results. While one study showed reduced FMD in migraine patients,68 another found that FMD was greater in MA patients than in MO patients and controls,69 and four studies did not find any differences between migraine patients and controls.17,41,60,70 Such variability in the findings remains when expanding the analysis to excluded or more-recent studies. The few studies that found a decrease in FMD included one with an exaggerated contextual nitrate-mediated dilation,71 one involving only MO patients,72 and one involving CM patients.9 Conversely, other studies found an increase in FMD in young migraine patients,73 particularly during migraine attacks,74 supporting the role of NO release in the induction of migraine pain. Rajan et al.75 and Larsen et al.76 (in a large population-based study) could not find any differences in FMD between migraineurs and controls. Considering the vast difference in sample size between the last study and the previous ones and the inhomogeneous study samples of MA and MO patients, it can be concluded that measurements of FMD cannot be used to detect overt peripheral vascular dysfunction in migraine.
The use of arterial tonometry to measure arterial stiffness has yielded conflicting results about endothelial dysfunction in peripheral arteries while confirming that arterial stiffness is higher in episodic77,78 and CM79 patients. Arterial stiffness in female MA patients was found to be correlated with circulating EMPs, which is a marker of endothelial dysfunction.24
Other determinants of vascular tone acting on the endothelium implicated in migraine pathogenesis
5HT
5HT is a monoamine derived from tryptophan that is produced in the brainstem and gastrointestinal tract. 5HT released from the brainstem circulates in the vascular system, where it is stored in platelets or metabolized by the liver or the pulmonary endothelium.80 5HT1B, 5HT1D, 5HT1F, and also the 5HT2 receptor subtypes have been well recognized in brain tissue. 5HT1B receptors have been found in brain VSMC and endothelium.81 Triptans act as 5HT1B/1D-selective agonists, with their actions including vasoconstriction, mainly via effects on VSMC receptors.82 Oppositely, endothelial 5HT1B receptors may mediate vasodilatation,81 but triptans should have minimal effects on endothelial receptors. Indeed, triptans did not appear to interfere with the endothelium-dependent FMD.83 However, that finding could have been influenced by triptan-mediated baseline vasoconstriction of the brachial artery. Hence, FMD appears to be a poor indicator of vascular dysfunction in migraine due to the large number of potential confounders.
Apart from its effects on VSMC, 5HT may act directly on the endothelium via the 5HT2B receptors, favoring the induction of a migraine attack. 5HT2B receptors have been found on the meningeal vascular endothelium and possibly also the cerebral vascular endothelium.84 Their activation has been proposed to determine NO release from the endothelium that consequently may induce the sterile inflammation responsible for migraine attack55,85 via the above-mentioned mechanisms mostly involving cGMP-mediated vasodilatation and CGRP release.
ATP
ATP and the purinergic signaling system are involved in both triggering and sustaining migraine attacks. The purinergic system acts as a neurotransmitter and neuromodulator, regulating the relationships among neurons, SMC, and glia in the CNS, with specific roles in mechanisms such as CSD and pain conduction.86 ATP is thought to also play a role in regulating cerebral vascular tone. The following two-phase hypothesis of the role of ATP in influencing vasomotor capability has been proposed: 1) vasoconstriction mediated by ATP that is released from perivascular nerves and damaged endothelial cells, via acting on VSMC P2X receptors, and 2) the vasodilatation phase, during which endothelial and platelet-derived ATP acts on endothelial P2X and P2Y receptors, leading to endothelium-derived vasodilatation.87 This latter phase is associated with pain perception.
AM
AM is a peptide secreted by endothelial cells in response to fluid shear stress, acting on the PIEZO1 mechanosensitive channels on the endothelium. Once released, AM regulates vascular tone by acting on the endothelium in paracrine and autocrine manners, inducing vasodilatation by inducing NOS.88,89 Its structure and function are related to CGRP,90 with AM receptors activating the same CGRP-induced intracellular cAMP pathway, and it is also involved in regulating BBB permeability and pain mediation.88,91 However, the role of AM in migraine induction has not been confirmed.92
Ovarian steroids
Ovarian hormones exert effects on vascular tone by acting on both the endothelium and VSMC.93 Estrogens induce mainly vasodilatation via both endothelium-dependent and -independent mechanisms. Indeed, estradiol receptors are also present on the endothelium, where they act via the classical NO-mediated pathway: the enhancement of NO production seems to be the primary vasodilator mechanism of estradiol. Progesterone may exert different effects on vascular tone, but the most prominent is a vasoconstriction effect, due in part to reducing NO release.94
Cerebrovascular reactivity and autoregulation
The effect of endothelial dysfunction on cerebral vascular tone could potentially affect cerebral hemodynamics. The cerebral circulation is a peculiar vascular system with complex autoregulatory properties that allow a stable perfusion pressure to be maintained under diverse conditions. Cerebrovascular reactivity (CVR) involves cerebral arterioles dilating in response to a vasodilating stimulus, and it can be assessed quantitively using different techniques.95 Endothelial dysfunction might affect CVR, which is impaired or absent in carotid disease and stroke (especially in large-artery occlusion stroke).96 Even though most studies have showed that the interictal CVR is preserved or even higher in the anterior circulation of MA patients,97,98 there are discordant reports of altered CVR in the posterior circulation.
Studies of CVR assessed by breath-holding [quantified as the breath-holding index (BHI)], mainly during transcranial Doppler (TCD) monitoring, have shown a lower cerebral CVR in the posterior circulation of MA patients,99 with a normal BHI in the anterior circulation and in the absence of systemic endothelial dysfunction.75 The lower BHI in the posterior circulation of migraineurs was associated with younger age at the onset of migraine.100 In contrast, another study found that BHI was higher in the posterior circulation in MA patients.101 A particularly interesting observation in that study was that the BHI in the anterior circulation was significant lower in MA patients taking estrogens, which is possibly due to exogenous estrogens inducing a condition of persistent vasodilatation that reduces the ability of vessels to dilate further. In contrast, BHI was higher in MA patients with right-to-left shunts, which questions whether such shunts in MA patients could result from a genetically determined alteration in vascular development, considering the higher familial history of MA in these patients.102
A recent study comparing BHI in migraineurs before and after treatment with erenumab found that CGRP blockade did not influence vasomotor reactivity.103 CVR assessed as reactivity to L-arginine infusion in the posterior circulation has been found to be lower in migraineurs than in healthy controls, while no significant differences in CVR in the middle cerebral artery have been found between migraine patients (both MA and MO) and healthy controls.104 A post-hoc analysis revealed that the CVRs of the posterior and middle cerebral arteries were significantly correlated, and confirmed the absence of a correlation with systemic endothelial dysfunction.70 A recent meta-analysis that included different experimental measurements (BHI, L-arginine infusion, CO2 inhalation, and acetazolamide infusion) confirmed that CVR in the posterior circulation is lower in migraine patients, particularly those with MO,105 while that in the anterior circulation did not differ significantly between migraineurs and controls.
It should be noted that vasodilatory stimuli induced by breath-holding and L-arginine may involve different mechanisms. Breath-holding induces an increase in cerebral blood flow via both a CO2-dependent vasodilatation and increased systemic blood pressure,106 while L-arginine—being the direct precursor of NO—should exert a blood-pressure-independent effect. Hence, studies of CVR adopting L-arginine infusion may provide a better understanding of endothelial dysfunction in migraine (Fig. 3).
Fig. 3. Cerebrovascular reactivity (CVR) studies adopting breath-holding or L-arginine infusion in migraine with aura (MA) patients compared with controls. Data were extracted from the meta-analysis of Dzator et al.105 ADMA: asymmetric dimethylarginine, BP: blood pressure, EtCO2: end-tidal CO2, L-arg: L-arginine, NOS: nitric oxide synthase, RLS: right-to-left shunt, SDMA: symmetric dimethylarginine.
To overcome the limits of breath-holding, it is also possible to evaluate CVR after CO2 inhalation, but this approach has been adopted in only a few studies (which were included in the aforementioned meta-analysis105). In addition to TCD monitoring, CVR has also been assessed using near-infrared spectrometry, with conflicting results.105 To our knowledge, there have been no published studies of MRI evaluations of CVR with CO2 inhalation or other hypercapnic stimuli in migraine patients.
Endothelial dysfunction and inflammation in migraine
As mentioned above, inflammation may be both the cause and consequence of oxidative stress, and hence also endothelial dysfunction. Migraine patients, and especially those with MA, showed higher interictal levels of CRP, with the CRP level being correlated with headache frequency and the number of years of aura attacks.64,107 Higher levels of cytokines confirm the presence of an inflammatory state during a migraine attack; a small study found higher levels of interleukin (IL)-1β, IL-6, TNF-α, and endocan (also called ESM-1), the last of which is produced by the endothelium.108
Endothelial dysfunction and thrombosis in migraine
As mentioned above, platelet activation is increased in migraine patients. A large study of female migraine patients showed a hypercoagulability profile characterized by elevated levels of t-PA antigen during the interictal period, reflecting reduced fibrinolysis, and elevated vWF activity, indicating a platelet-mediated procoagulant effect.64 Moreover, MA patients had a stronger association with elevated vWF levels, and vWF antigen levels were higher in migraineurs with prior stroke than in those without a stroke history.109 vWF was also recognized to increase during a migraine attack.10,110 In migraine patients, higher vWF activity and antigen levels were found along with shortening in all Clot Signature Analyzer measurements (platelet hemostasis time, clot time, and collagen-induced thrombus formation), indicating a hypercoagulability state.111 Moreover, higher vWF levels were found in patients with angiotensin-converting enzyme (ACE) gene polymorphism DD (the deletion genotype that is linked to increased ACE levels, decreased bradykinin levels, and increased vascular tone), especially in carriers of the C677T polymorphism in the MTHFR gene.112 Other hints of hypercoagulability in migraine came from a recent large population-based case–control study that found elevated levels of fibrinogen and factor II in migraine patients (particularly in females with MA) compared with controls.107
A recent pilot study of female MA patients found a hypercoagulable state that confirmed decreases in the platelet clot reaction time and the time to maximum thrombus generation and aberrant fibrin polymerization due to a β-amyloid conformation of fibrin, compared with controls.113 This means that MA patients may produce stronger and larger clots more rapidly, particularly during headache attacks. A cause of this hypercoagulable state may be identified in oxidative stress, since that pilot study also found that erythrocytes in the same MA patients presented with significant variations in size, shape, and distribution, and oxidative stress is one of the main determinants of alterations to erythrocyte membranes.
Endothelial dysfunction and vascular permeability in migraine
Neurogenic inflammation may increase the permeability of the endothelium of cerebral postcapillary venules, allowing plasma protein extravasation (PPE). This is mainly due to the action of SP, a neuropeptide released from trigeminal terminals. Studies of drugs inhibiting SP-induced PPE failed to demonstrate any efficacy on migraine attacks, indicating a marginal role of PPE in migraine.114 Mast-cell-derived histamine can also enhance vascular permeability, in addition to the NO-inducing effect on the endothelium via the activation of the H1 histamine receptor.115
Moreover, the levels of claudin-5 (a membrane protein regulating BBB permeability and endothelial integrity) were higher in migraine patients during migraine attacks and the interictal period than in controls.108
CONCLUSION
Despite the lack of a precise and direct role of endothelial dysfunction in the pathophysiological chain of migraine induction, the available evidence indicates that some endothelial alterations are undoubtedly present in migraine patients. Although it is not clear whether they represent one of the causative factors of migraine attacks or, conversely, are induced by migraine, it is noteworthy that endothelial dysfunction is a marker of vascular risk. More-reliable and precise biomarkers are needed. Studies addressing the role of endothelial dysfunction in migraine are needed to better demonstrate its role and its risks, especially regarding how and what vessels are mostly impaired.
Acknowledgements
We thank Servier Medical Art, where the majority of the basic artwork elements were taken.
Footnotes
- Conceptualization: Matteo Paolucci, Claudia Altamura, Fabrizio Vernieri.
- Data curation: Matteo Paolucci, Claudia Altamura.
- Formal analysis: Matteo Paolucci, Claudia Altamura.
- Investigation: Matteo Paolucci, Claudia Altamura, Fabrizio Vernieri.
- Methodology: Matteo Paolucci, Claudia Altamura, Fabrizio Vernieri.
- Project administration: Fabrizio Vernieri.
- Resources: Matteo Paolucci, Claudia Altamura.
- Software: Matteo Paolucci, Claudia Altamura.
- Supervision: Fabrizio Vernieri.
- Validation: Fabrizio Vernieri.
- Visualization: Matteo Paolucci.
- Writing—original draft: Matteo Paolucci.
- Writing—review & editing: Claudia Altamura, Fabrizio Vernieri.
Conflicts of Interest: MP and CA have no potential conflicts of interest to disclose. FV received travel grants, honoraria for advisory boards, speaker panels or investigation studies from Angelini, Allergan, Eli-Lilly, Novartis, Teva.
References
- 1.Ferrari MD, Klever RR, Terwindt GM, Ayata C, van den Maagdenberg AM. Migraine pathophysiology: lessons from mouse models and human genetics. Lancet Neurol. 2015;14:65–80. doi: 10.1016/S1474-4422(14)70220-0. [DOI] [PubMed] [Google Scholar]
- 2.Gormley P, Anttila V, Winsvold BS, Palta P, Esko T, Pers TH, et al. Meta-analysis of 375,000 individuals identifies 38 susceptibility loci for migraine. Nat Genet. 2016;48:856–866. doi: 10.1038/ng.3598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Roquer J, Segura T, Serena J, Castillo J. Endothelial dysfunction, vascular disease and stroke: the ARTICO study. Cerebrovasc Dis. 2009;27 Suppl 1:25–37. doi: 10.1159/000200439. [DOI] [PubMed] [Google Scholar]
- 4.Biswas SK. Does the interdependence between oxidative stress and inflammation explain the antioxidant paradox? Oxid Med Cell Longev. 2016;2016:5698931. doi: 10.1155/2016/5698931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Yıldırım S, Akar S, Kuyucu M, Yıldırım A, Dane S, Aygül R. Paraoxonase 1 gene polymorphisms, paraoxonase/arylesterase activities and oxidized low-density lipoprotein levels in patients with migraine. Cell Biochem Funct. 2011;29:549–554. doi: 10.1002/cbf.1785. [DOI] [PubMed] [Google Scholar]
- 6.Tuncel D, Tolun FI, Gokce M, Imrek S, Ekerbiçer H. Oxidative stress in migraine with and without aura. Biol Trace Elem Res. 2008;126:92–97. doi: 10.1007/s12011-008-8193-9. [DOI] [PubMed] [Google Scholar]
- 7.Borkum JM. The migraine attack as a homeostatic, neuroprotective response to brain oxidative stress: preliminary evidence for a theory. Headache. 2018;58:118–135. doi: 10.1111/head.13214. [DOI] [PubMed] [Google Scholar]
- 8.Ghosh J, Joshi G, Pradhan S, Mittal B. Investigation of TNFA 308G > A and TNFB 252G > A polymorphisms in genetic susceptibility to migraine. J Neurol. 2010;257:898–904. doi: 10.1007/s00415-009-5430-x. [DOI] [PubMed] [Google Scholar]
- 9.González-Quintanilla V, Toriello M, Palacio E, González-Gay MA, Castillo J, Montes S, et al. Systemic and cerebral endothelial dysfunction in chronic migraine. A case-control study with an active comparator. Cephalalgia. 2016;36:552–560. doi: 10.1177/0333102415607857. [DOI] [PubMed] [Google Scholar]
- 10.Yilmaz Avci A, Akkucuk MH, Torun E, Arikan S, Can U, Tekindal MA. Migraine and subclinical atherosclerosis: endothelial dysfunction biomarkers and carotid intima-media thickness: a case-control study. Neurol Sci. 2019;40:703–711. doi: 10.1007/s10072-019-3710-5. [DOI] [PubMed] [Google Scholar]
- 11.Empl M, Sostak P, Breckner M, Riedel M, Müller N, Gruber R, et al. T-cell subsets and expression of integrins in peripheral blood of patients with migraine. Cephalalgia. 1999;19:713–717. doi: 10.1046/j.1468-2982.1999.019008713.x. [DOI] [PubMed] [Google Scholar]
- 12.Zeller JA, Frahm K, Baron R, Stingele R, Deuschl G. Platelet-leukocyte interaction and platelet activation in migraine: a link to ischemic stroke? J Neurol Neurosurg Psychiatry. 2004;75:984–987. doi: 10.1136/jnnp.2003.019638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Tietjen GE, Khubchandani J. Platelet dysfunction and stroke in the female migraineur. Curr Pain Headache Rep. 2009;13:386–391. doi: 10.1007/s11916-009-0063-4. [DOI] [PubMed] [Google Scholar]
- 14.Gabrielli M, Santarelli L, Addolorato G, Foschi G, Di Gampli C, Gasbarrini A, et al. High prevalence of antiendothelial cell antibodies in migraine. Headache. 2002;42:385–386. doi: 10.1046/j.1526-4610.2002.02114.x. [DOI] [PubMed] [Google Scholar]
- 15.Oterino A, Toriello M, Valle N, Castillo J, Alonso-Arranz A, Bravo Y, et al. The relationship between homocysteine and genes of folate-related enzymes in migraine patients. Headache. 2010;50:99–168. doi: 10.1111/j.1526-4610.2009.01484.x. [DOI] [PubMed] [Google Scholar]
- 16.Michalak S, Kalinowska-Lyszczarz A, Wegrzyn D, Thielemann A, Osztynowicz K, Kozubski W. The levels of circulating proangiogenic factors in migraineurs. Neuromolecular Med. 2017;19:510–517. doi: 10.1007/s12017-017-8465-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Rodríguez-Osorio X, Sobrino T, Brea D, Martínez F, Castillo J, Leira R. Endothelial progenitor cells: a new key for endothelial dysfunction in migraine. Neurology. 2012;79:474–479. doi: 10.1212/WNL.0b013e31826170ce. [DOI] [PubMed] [Google Scholar]
- 18.Hill JM, Zalos G, Halcox JP, Schenke WH, Waclawiw MA, Quyyumi AA, et al. Circulating endothelial progenitor cells, vascular function, and cardiovascular risk. N Engl J Med. 2003;348:593–600. doi: 10.1056/NEJMoa022287. [DOI] [PubMed] [Google Scholar]
- 19.Herbrig K, Haensel S, Oelschlaegel U, Pistrosch F, Foerster S, Passauer J. Endothelial dysfunction in patients with rheumatoid arthritis is associated with a reduced number and impaired function of endothelial progenitor cells. Ann Rheum Dis. 2006;65:157–163. doi: 10.1136/ard.2005.035378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lee ST, Chu K, Jung KH, Kim DH, Kim EH, Choe VN, et al. Decreased number and function of endothelial progenitor cells in patients with migraine. Neurology. 2008;70:1510–1517. doi: 10.1212/01.wnl.0000294329.93565.94. [DOI] [PubMed] [Google Scholar]
- 21.Oterino A, Toriello M, Palacio E, Quintanilla VG, Ruiz-Lavilla N, Montes S, et al. Analysis of endothelial precursor cells in chronic migraine: a case-control study. Cephalalgia. 2013;33:236–244. doi: 10.1177/0333102412469737. [DOI] [PubMed] [Google Scholar]
- 22.Liman TG, Neeb L, Rosinski J, Reuter U, Endres M. Stromal cell-derived factor-1 alpha is decreased in women with migraine with aura. Headache. 2016;56:1274–1279. doi: 10.1111/head.12839. [DOI] [PubMed] [Google Scholar]
- 23.Boulanger CM, Scoazec A, Ebrahimian T, Henry P, Mathieu E, Tedgui A, et al. Circulating microparticles from patients with myocardial infarction cause endothelial dysfunction. Circulation. 2001;104:2649–2652. doi: 10.1161/hc4701.100516. [DOI] [PubMed] [Google Scholar]
- 24.Liman TG, Bachelier-Walenta K, Neeb L, Rosinski J, Reuter U, Böhm M, et al. Circulating endothelial microparticles in female migraineurs with aura. Cephalalgia. 2015;35:88–94. doi: 10.1177/0333102414529671. [DOI] [PubMed] [Google Scholar]
- 25.Fischer M, Gaul C, Shanib H, Holle D, Loacker L, Griesmacher A, et al. Markers of endothelial function in migraine patients: results from a bi-center prospective study. Cephalalgia. 2015;35:877–885. doi: 10.1177/0333102414564890. [DOI] [PubMed] [Google Scholar]
- 26.Domínguez C, López A, Ramos-Cabrer P, Vieites-Prado A, Pérez-Mato M, Villalba C, et al. Iron deposition in periaqueductal gray matter as a potential biomarker for chronic migraine. Neurology. 2019;92:e1076–e1085. doi: 10.1212/WNL.0000000000007047. [DOI] [PubMed] [Google Scholar]
- 27.Domínguez-Vivero C, Leira Y, López-Ferreiro A, Saavedra M, Rodríguez-Osorio X, Sobrino T, et al. Pentraxin 3 (PTX3): a molecular marker of endothelial dysfunction in chronic migraine. J Clin Med. 2020;9:849. doi: 10.3390/jcm9030849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Jacobsen LM, Winsvold BS, Romundstad S, Pripp AH, Holmen J, Zwart JA. Urinary albumin excretion as a marker of endothelial dysfunction in migraine sufferers: the HUNT Study, Norway. BMJ Open. 2013;3:e003268. doi: 10.1136/bmjopen-2013-003268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Tietjen GE. Migraine as a systemic vasculopathy. Cephalalgia. 2009;29:987–996. doi: 10.1111/j.1468-2982.2009.01937.x. [DOI] [PubMed] [Google Scholar]
- 30.Pradhan AA, Bertels Z, Akerman S. Targeted nitric oxide synthase inhibitors for migraine. Neurotherapeutics. 2018;15:391–401. doi: 10.1007/s13311-018-0614-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Thomsen LL, Olesen J. Nitric oxide in primary headaches. Curr Opin Neurol. 2001;14:315–321. doi: 10.1097/00019052-200106000-00009. [DOI] [PubMed] [Google Scholar]
- 32.Lee TJ. Nitric oxide and the cerebral vascular function. J Biomed Sci. 2000;7:16–26. doi: 10.1007/BF02255914. [DOI] [PubMed] [Google Scholar]
- 33.Schmuck K, Ullmer C, Kalkman HO, Probst A, Lubbert H. Activation of meningeal 5-HT2B receptors: an early step in the generation of migraine headache? Eur J Neurosci. 1996;8:959–967. doi: 10.1111/j.1460-9568.1996.tb01583.x. [DOI] [PubMed] [Google Scholar]
- 34.Wei EP, Moskowitz MA, Boccalini P, Kontos HA. Calcitonin gene-related peptide mediates nitroglycerin and sodium nitroprusside-induced vasodilation in feline cerebral arterioles. Circ Res. 1992;70:1313–1319. doi: 10.1161/01.res.70.6.1313. [DOI] [PubMed] [Google Scholar]
- 35.Borkum JM. CGRP and brain functioning: cautions for migraine treatment. Headache. 2019;59:1339–1357. doi: 10.1111/head.13591. [DOI] [PubMed] [Google Scholar]
- 36.Akerman S, Williamson DJ, Kaube H, Goadsby PJ. Nitric oxide synthase inhibitors can antagonize neurogenic and calcitonin gene-related peptide induced dilation of dural meningeal vessels. Br J Pharmacol. 2002;137:62–68. doi: 10.1038/sj.bjp.0704842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Bourque SL, Davidge ST, Adams MA. The interaction between endothelin-1 and nitric oxide in the vasculature: new perspectives. Am J Physiol Regul Integr Comp Physiol. 2011;300:R1288–R1295. doi: 10.1152/ajpregu.00397.2010. [DOI] [PubMed] [Google Scholar]
- 38.Iljazi A, Ayata C, Ashina M, Hougaard A. The role of endothelin in the pathophysiology of migraine-a systematic review. Curr Pain Headache Rep. 2018;22:27. doi: 10.1007/s11916-018-0682-8. [DOI] [PubMed] [Google Scholar]
- 39.Kallela M, Färkkilä M, Saijonmaa O, Fyhrquist F. Endothelin in migraine patients. Cephalalgia. 1998;18:329–332. doi: 10.1046/j.1468-2982.1998.1806329.x. [DOI] [PubMed] [Google Scholar]
- 40.Bianchi A, Pitari G, Amenta V, Giuliano F, Gallina M, Costa R, et al. Endothelial, haemostatic and haemorheological modifications in migraineurs. Artery. 1996;22:93–100. [PubMed] [Google Scholar]
- 41.Hamed SA, Hamed EA, Ezz Eldin AM, Mahmoud NM. Vascular risk factors, endothelial function, and carotid thickness in patients with migraine: relationship to atherosclerosis. J Stroke Cerebrovasc Dis. 2010;19:92–103. doi: 10.1016/j.jstrokecerebrovasdis.2009.04.007. [DOI] [PubMed] [Google Scholar]
- 42.Gallai V, Sarchielli P, Firenze C, Trequattrini A, Paciaroni M, Usai F, et al. Endothelin 1 in migraine and tension-type headache. Acta Neurol Scand. 1994;89:47–55. doi: 10.1111/j.1600-0404.1994.tb01632.x. [DOI] [PubMed] [Google Scholar]
- 43.Joseph EK, Levine JD. Role of endothelial cells in antihyperalgesia induced by a triptan and β-blocker. Neuroscience. 2013;232:83–89. doi: 10.1016/j.neuroscience.2012.12.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Dreier JP, Kleeberg J, Petzold G, Priller J, Windmüller O, Orzechowski HD, et al. Endothelin-1 potently induces Leão's cortical spreading depression in vivo in the rat: a model for an endothelial trigger of migrainous aura? Brain. 2002;125(Pt 1):102–112. doi: 10.1093/brain/awf007. [DOI] [PubMed] [Google Scholar]
- 45.Dreier JP, Kleeberg J, Alam M, Major S, Kohl-Bareis M, Petzold GC, et al. Endothelin-1-induced spreading depression in rats is associated with a microarea of selective neuronal necrosis. Exp Biol Med (Maywood) 2007;232:204–213. [PubMed] [Google Scholar]
- 46.Hougaard A, Younis S, Iljazi A, Sugimoto K, Ayata C, Ashina M. Intravenous endothelin-1 infusion does not induce aura or headache in migraine patients with aura. Headache. 2020;60:724–734. doi: 10.1111/head.13753. [DOI] [PubMed] [Google Scholar]
- 47.Hansen JM, Hauge AW, Olesen J, Ashina M. Calcitonin gene-related peptide triggers migraine-like attacks in patients with migraine with aura. Cephalalgia. 2010;30:1179–1186. doi: 10.1177/0333102410368444. [DOI] [PubMed] [Google Scholar]
- 48.Christiansen I, Thomsen LL, Daugaard D, Ulrich V, Olesen J. Glyceryl trinitrate induces attacks of migraine without aura in sufferers of migraine with aura. Cephalalgia. 1999;19:660–667. doi: 10.1046/j.1468-2982.1999.019007660.x. [DOI] [PubMed] [Google Scholar]
- 49.Butt JH, Rostrup E, Hansen AS, Lambertsen KL, Kruuse C. Induction of migraine-like headache, but not aura, by cilostazol in patients with migraine with aura. Brain. 2018;141:2943–2951. doi: 10.1093/brain/awy228. [DOI] [PubMed] [Google Scholar]
- 50.Read SJ, Smith MI, Hunter AJ, Parsons AA. Enhanced nitric oxide release during cortical spreading depression following infusion of glyceryl trinitrate in the anaesthetized cat. Cephalalgia. 1997;17:159–165. doi: 10.1046/j.1468-2982.1997.1703159.x. [DOI] [PubMed] [Google Scholar]
- 51.Read SJ, Smith MI, Hunter AJ, Upton N, Parsons AA. SB-220453, a potential novel antimigraine agent, inhibits nitric oxide release following induction of cortical spreading depression in the anaesthetized cat. Cephalalgia. 2000;20:92–99. doi: 10.1046/j.1468-2982.2000.00022.x. [DOI] [PubMed] [Google Scholar]
- 52.Read SJ, Parsons AA. Sumatriptan modifies cortical free radical release during cortical spreading depression: a novel antimigraine action for sumatriptan? Brain Res. 2000;870:44–53. doi: 10.1016/s0006-8993(00)02400-8. [DOI] [PubMed] [Google Scholar]
- 53.Lassen LH, Ashina M, Christiansen I, Ulrich V, Olesen J. Nitric oxide synthase inhibition in migraine. Lancet. 1997;349:401–402. doi: 10.1016/s0140-6736(97)80021-9. [DOI] [PubMed] [Google Scholar]
- 54.Lassen LH, Ashina M, Christiansen I, Ulrich V, Grover R, Donaldson J, et al. Nitric oxide synthase inhibition: a new principle in the treatment of migraine attacks. Cephalalgia. 1998;18:27–32. doi: 10.1046/j.1468-2982.1998.1801027.x. [DOI] [PubMed] [Google Scholar]
- 55.Johnson KW, Nelson DL, Dieckman DK, Wainscott DB, Lucaites VL, Audia JE, et al. Neurogenic dural protein extravasation induced by meta-chlorophenylpiperazine (mCPP) involves nitric oxide and 5-HT2B receptor activation. Cephalalgia. 2003;23:117–123. doi: 10.1046/j.1468-2982.2003.00464.x. [DOI] [PubMed] [Google Scholar]
- 56.Bagdy G, Riba P, Kecskeméti V, Chase D, Juhász G. Headache-type adverse effects of NO donors: vasodilation and beyond. Br J Pharmacol. 2010;160:20–35. doi: 10.1111/j.1476-5381.2010.00643.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Ferrari LF, Levine JD, Green PG. Mechanisms mediating nitroglycerin-induced delayed-onset hyperalgesia in the rat. Neuroscience. 2016;317:121–129. doi: 10.1016/j.neuroscience.2016.01.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Ciancarelli I, Tozzi-Ciancarelli MG, Di Massimo C, Marini C, Carolei A. Urinary nitric oxide metabolites and lipid peroxidation byproducts in migraine. Cephalalgia. 2003;23:39–42. doi: 10.1046/j.1468-2982.2003.00447.x. [DOI] [PubMed] [Google Scholar]
- 59.Guldiken B, Demir M, Guldiken S, Turgut N, Ozkan H, Kabayel L, et al. Asymmetric dimethylarginine and nitric oxide levels in migraine during the interictal period. J Clin Neurosci. 2009;16:672–674. doi: 10.1016/j.jocn.2008.08.015. [DOI] [PubMed] [Google Scholar]
- 60.Silva FA, Rueda-Clausen CF, Silva SY, Zarruk JG, Guzmán JC, Morillo CA, et al. Endothelial function in patients with migraine during the interictal period. Headache. 2007;47:45–51. doi: 10.1111/j.1526-4610.2006.00532.x. [DOI] [PubMed] [Google Scholar]
- 61.Napoli R, Guardasole V, Zarra E, Matarazzo M, D'Anna C, Saccà F, et al. Vascular smooth muscle cell dysfunction in patients with migraine. Neurology. 2009;72:2111–2114. doi: 10.1212/WNL.0b013e3181aa53ce. [DOI] [PubMed] [Google Scholar]
- 62.Vanmolkot FH, de Hoon JN. Endothelial function in migraine: a cross-sectional study. BMC Neurol. 2010;10:119. doi: 10.1186/1471-2377-10-119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Napoli R, Guardasole V, Zarra E, Sena AD, Saccà F, Ruvolo A, et al. Migraine attack restores the response of vascular smooth muscle cells to nitric oxide but not to norepinephrine. World J Cardiol. 2013;5:375–381. doi: 10.4330/wjc.v5.i10.375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Tietjen GE, Herial NA, White L, Utley C, Kosmyna JM, Khuder SA. Migraine and biomarkers of endothelial activation in young women. Stroke. 2009;40:2977–2982. doi: 10.1161/STROKEAHA.109.547901. [DOI] [PubMed] [Google Scholar]
- 65.Uzar E, Evliyaoglu O, Toprak G, Acar A, Yucel Y, Calisir T, et al. Increased asymmetric dimethylarginine and nitric oxide levels in patients with migraine. J Headache Pain. 2011;12:239–243. doi: 10.1007/s10194-011-0323-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Erdélyi-Bótor S, Komáromy H, Kamson DO, Kovács N, Perlaki G, Orsi G, et al. Serum L-arginine and dimethylarginine levels in migraine patients with brain white matter lesions. Cephalalgia. 2017;37:571–580. doi: 10.1177/0333102416651454. [DOI] [PubMed] [Google Scholar]
- 67.Butt JH, Franzmann U, Kruuse C. Endothelial function in migraine with aura - a systematic review. Headache. 2015;55:35–54. doi: 10.1111/head.12494. [DOI] [PubMed] [Google Scholar]
- 68.Vanmolkot FH, Van Bortel LM, de Hoon JN. Altered arterial function in migraine of recent onset. Neurology. 2007;68:1563–1570. doi: 10.1212/01.wnl.0000260964.28393.ed. [DOI] [PubMed] [Google Scholar]
- 69.Vernieri F, Moro L, Altamura C, Palazzo P, Antonelli Incalzi R, Rossini PM, et al. Patients with migraine with aura have increased flow mediated dilation. BMC Neurol. 2010;10:18. doi: 10.1186/1471-2377-10-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Perko D, Pretnar-Oblak J, Šabovič M, Zaletel M, Žvan B. Associations between cerebral and systemic endothelial function in migraine patients: a post-hoc study. BMC Neurol. 2011;11:146. doi: 10.1186/1471-2377-11-146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Yetkin E, Ozisik H, Ozcan C, Aksoy Y, Turhan H. Increased dilator response to nitrate and decreased flow-mediated dilatation in migraineurs. Headache. 2007;47:104–110. doi: 10.1111/j.1526-4610.2007.00657.x. [DOI] [PubMed] [Google Scholar]
- 72.Heshmat-Ghahdarijani K, Javanmard SH, Sonbolestan SA, Saadatnia M, Sonbolestan SA. Endothelial function in patients with migraine without aura during the interictal period. Int J Prev Med. 2015;6:2. doi: 10.4103/2008-7802.151432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Sabri MR, Dehghan B, Yaghini O, Nasiri J, Mansourian M, Khalifehsoltani S. Endothelial dysfunction state in migraine headache and neutrally mediated syncope in children and young adults. J Res Med Sci. 2015;20:771–776. doi: 10.4103/1735-1995.168384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Dogru MT, Dilekoz E, Alpua M, Eroglu O, Kandemir H, Alp C, et al. Endothelial and autonomic functions in patients with migraine. Pain Med. 2020;21:e222–e231. doi: 10.1093/pm/pnz223. [DOI] [PubMed] [Google Scholar]
- 75.Rajan R, Khurana D, Lal V. Interictal cerebral and systemic endothelial dysfunction in patients with migraine: a case-control study. J Neurol Neurosurg Psychiatry. 2015;86:1253–1257. doi: 10.1136/jnnp-2014-309571. [DOI] [PubMed] [Google Scholar]
- 76.Larsen JS, Skaug EA, Wisløff U, Ellingsen Ø, Stovner LJ, Linde M, et al. Migraine and endothelial function: the HUNT3 Study. Cephalalgia. 2016;36:1341–1349. doi: 10.1177/0333102416631961. [DOI] [PubMed] [Google Scholar]
- 77.Liman TG, Neeb L, Rosinski J, Wellwood I, Reuter U, Doehner W, et al. Peripheral endothelial function and arterial stiffness in women with migraine with aura: a case-control study. Cephalalgia. 2012;32:459–466. doi: 10.1177/0333102412444014. [DOI] [PubMed] [Google Scholar]
- 78.Dogan A, Orscelik O, Kocyigit M, Elcik D, Baran O, Cerit N, et al. The effect of prophylactic migraine treatment on arterial stiffness. Blood Press. 2015;24:222–229. doi: 10.3109/08037051.2015.1030902. [DOI] [PubMed] [Google Scholar]
- 79.Jiménez Caballero PE, Muñoz Escudero F. Peripheral endothelial function and arterial stiffness in patients with chronic migraine: a case-control study. J Headache Pain. 2013;14:8. doi: 10.1186/1129-2377-14-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Houston DS, Vanhoutte PM. Serotonin and the vascular system. Role in health and disease, and implications for therapy. Drugs. 1986;31:149–163. doi: 10.2165/00003495-198631020-00004. [DOI] [PubMed] [Google Scholar]
- 81.Riad M, Tong XK, el Mestikawy S, Hamon M, Hamel E, Descarries L. Endothelial expression of the 5-hydroxytryptamine1B antimigraine drug receptor in rat and human brain microvessels. Neuroscience. 1998;86:1031–1035. doi: 10.1016/s0306-4522(98)00196-1. [DOI] [PubMed] [Google Scholar]
- 82.Nilsson T, Longmore J, Shaw D, Olesen IJ, Edvinsson L. Contractile 5-HT1B receptors in human cerebral arteries: pharmacological characterization and localization with immunocytochemistry. Br J Pharmacol. 1999;128:1133–1140. doi: 10.1038/sj.bjp.0702773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.de Hoon JN, Willigers JM, Troost J, Struijker-Boudier HA, Van Bortel LM. Vascular effects of 5-HT1B/1D-receptor agonists in patients with migraine headaches. Clin Pharmacol Ther. 2000;68:418–426. doi: 10.1067/mcp.2000.110502. [DOI] [PubMed] [Google Scholar]
- 84.Segelcke D, Messlinger K. Putative role of 5-HT2B receptors in migraine pathophysiology. Cephalalgia. 2017;37:365–371. doi: 10.1177/0333102416646760. [DOI] [PubMed] [Google Scholar]
- 85.Fozard JR. The 5-hydroxytryptamine-nitric oxide connection: the key link in the initiation of migraine? Arch Int Pharmacodyn Ther. 1995;329:111–119. [PubMed] [Google Scholar]
- 86.Cieślak M, Czarnecka J, Roszek K, Komoszyński M. The role of purinergic signaling in the etiology of migraine and novel antimigraine treatment. Purinergic Signal. 2015;11:307–316. doi: 10.1007/s11302-015-9453-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Burnstock G. Purinergic signaling in the cardiovascular system. Circ Res. 2017;120:207–228. doi: 10.1161/CIRCRESAHA.116.309726. [DOI] [PubMed] [Google Scholar]
- 88.Kis B, Kaiya H, Nishi R, Deli MA, Abrahám CS, Yanagita T, et al. Cerebral endothelial cells are a major source of adrenomedullin. J Neuroendocrinol. 2002;14:283–293. doi: 10.1046/j.1365-2826.2002.00778.x. [DOI] [PubMed] [Google Scholar]
- 89.Iring A, Jin YJ, Albarrán-Juárez J, Siragusa M, Wang S, Dancs PT, et al. Shear stress-induced endothelial adrenomedullin signaling regulates vascular tone and blood pressure. J Clin Invest. 2019;129:2775–2791. doi: 10.1172/JCI123825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Lang MG, Paternò R, Faraci FM, Heistad DD. Mechanisms of adrenomedullin-induced dilatation of cerebral arterioles. Stroke. 1997;28:181–185. doi: 10.1161/01.str.28.1.181. [DOI] [PubMed] [Google Scholar]
- 91.Li FJ, Zheng SR, Wang DM. Adrenomedullin: an important participant in neurological diseases. Neural Regen Res. 2020;15:1199–1207. doi: 10.4103/1673-5374.272567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Petersen KA, Birk S, Kitamura K, Olesen J. Effect of adrenomedullin on the cerebral circulation: relevance to primary headache disorders. Cephalalgia. 2009;29:23–30. doi: 10.1111/j.1468-2982.2008.01695.x. [DOI] [PubMed] [Google Scholar]
- 93.Sarrel PM. The differential effects of oestrogens and progestins on vascular tone. Hum Reprod Update. 1999;5:205–209. doi: 10.1093/humupd/5.3.205. [DOI] [PubMed] [Google Scholar]
- 94.Martin VT, Behbehani M. Ovarian hormones and migraine headache: understanding mechanisms and pathogenesis--part I. Headache. 2006;46:3–23. doi: 10.1111/j.1526-4610.2006.00309.x. [DOI] [PubMed] [Google Scholar]
- 95.Wolf ME. Functional TCD: regulation of cerebral hemodynamics--cerebral autoregulation, vasomotor reactivity, and neurovascular coupling. Front Neurol Neurosci. 2015;36:40–56. doi: 10.1159/000366236. [DOI] [PubMed] [Google Scholar]
- 96.Vernieri F, Pasqualetti P, Passarelli F, Rossini PM, Silvestrini M. Outcome of carotid artery occlusion is predicted by cerebrovascular reactivity. Stroke. 1999;30:593–598. doi: 10.1161/01.str.30.3.593. [DOI] [PubMed] [Google Scholar]
- 97.Vernieri F, Tibuzzi F, Pasqualetti P, Altamura C, Palazzo P, Rossini PM, et al. Increased cerebral vasomotor reactivity in migraine with aura: an autoregulation disorder? A transcranial doppler and near-infrared spectroscopy study. Cephalalgia. 2008;28:689–695. doi: 10.1111/j.1468-2982.2008.01579.x. [DOI] [PubMed] [Google Scholar]
- 98.Fiermonte G, Pierelli F, Pauri F, Cosentino FI, Soccorsi R, Giacomini P. Cerebrovascular CO2 reactivity in migraine with aura and without aura. A transcranial Doppler study. Acta Neurol Scand. 1995;92:166–169. doi: 10.1111/j.1600-0404.1995.tb01033.x. [DOI] [PubMed] [Google Scholar]
- 99.Silvestrini M, Baruffaldi R, Bartolini M, Vernieri F, Lanciotti C, Matteis M, et al. Basilar and middle cerebral artery reactivity in patients with migraine. Headache. 2004;44:29–34. doi: 10.1111/j.1526-4610.2004.04006.x. [DOI] [PubMed] [Google Scholar]
- 100.Lee MJ, Cho S, Woo SY, Chung CS. Paradoxical association between age and cerebrovascular reactivity in migraine: a cross-sectional study. J Neurol Sci. 2019;398:204–209. doi: 10.1016/j.jns.2019.01.039. [DOI] [PubMed] [Google Scholar]
- 101.Altamura C, Paolucci M, Brunelli N, Cascio Rizzo A, Cecchi G, Assenza F, et al. Right-to-left shunts and hormonal therapy influence cerebral vasomotor reactivity in patients with migraine with aura. PLoS One. 2019;14:e0220637. doi: 10.1371/journal.pone.0220637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Anzola GP, Meneghetti G, Zanferrari C, Adami A, Dinia L, Del Sette M, et al. Is migraine associated with right-to-left shunt a separate disease? Results of the SAM study. Cephalalgia. 2008;28:360–366. doi: 10.1111/j.1468-2982.2008.01539.x. [DOI] [PubMed] [Google Scholar]
- 103.Altamura C, Viticchi G, Fallacara A, Costa CM, Brunelli N, Fiori C, et al. Erenumab does not alter cerebral hemodynamics and endothelial function in migraine without aura. Cephalalgia. 2021;41:90–98. doi: 10.1177/0333102420956692. [DOI] [PubMed] [Google Scholar]
- 104.Perko D, Pretnar-Oblak J, Sabovič M, Zvan B, Zaletel M. Cerebrovascular reactivity to L-arginine in the anterior and posterior cerebral circulation in migraine patients. Acta Neurol Scand. 2011;124:269–274. doi: 10.1111/j.1600-0404.2010.01468.x. [DOI] [PubMed] [Google Scholar]
- 105.Dzator JS, Howe PR, Wong RH. Profiling cerebrovascular function in migraine: a systematic review and meta-analysis. J Cereb Blood Flow Metab. 2020 Oct 22; doi: 10.1177/0271678X20964344. [Epub]. Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Webb AJS, Paolucci M, Mazzucco S, Li L, Rothwell PM Oxford Vascular Study Phenotyped Cohort. Confounding of cerebral blood flow velocity by blood pressure during breath holding or hyperventilation in transient ischemic attack or stroke. Stroke. 2020;51:468–474. doi: 10.1161/STROKEAHA.119.027829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Tietjen GE, Khubchandani J, Herial N, Palm-Meinders IH, Koppen H, Terwindt GM, et al. Migraine and vascular disease biomarkers: a population-based case-control study. Cephalalgia. 2018;38:511–518. doi: 10.1177/0333102417698936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Yücel M, Kotan D, Gurol Çiftçi G, Çiftçi IH, Cikriklar HI. Serum levels of endocan, claudin-5 and cytokines in migraine. Eur Rev Med Pharmacol Sci. 2016;20:930–936. [PubMed] [Google Scholar]
- 109.Tietjen GE, Al-Qasmi MM, Athanas K, Dafer RM, Khuder SA. Increased von Willebrand factor in migraine. Neurology. 2001;57:334–336. doi: 10.1212/wnl.57.2.334. [DOI] [PubMed] [Google Scholar]
- 110.Cesar JM, García-Avello A, Vecino AM, Sastre JL, Alvarez-Cermeño JC. Increased levels of plasma von Willebrand factor in migraine crisis. Acta Neurol Scand. 1995;91:412–413. doi: 10.1111/j.1600-0404.1995.tb07030.x. [DOI] [PubMed] [Google Scholar]
- 111.Tietjen GE, Al-Qasmi MM, Athanas K, Utley C, Herial NA. Altered hemostasis in migraineurs studied with a dynamic flow system. Thromb Res. 2007;119:217–222. doi: 10.1016/j.thromres.2005.12.020. [DOI] [PubMed] [Google Scholar]
- 112.Tietjen GE, Herial NA, Utley C, White L, Yerga-Woolwine S, Joe B. Association of von Willebrand factor activity with ACE I/D and MTHFR C677T polymorphisms in migraine. Cephalalgia. 2009;29:960–968. doi: 10.1111/j.1468-2982.2008.01824.x. [DOI] [PubMed] [Google Scholar]
- 113.de Villiers S, Bester J, Kell DB, Pretorius E. A possible role of amyloidogenic blood clotting in the evolving haemodynamics of female migraine-with-aura: results from a pilot study. Front Neurol. 2019;10:1262. doi: 10.3389/fneur.2019.01262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Peroutka SJ. Neurogenic inflammation and migraine: implications for the therapeutics. Mol Interv. 2005;5:304–311. doi: 10.1124/mi.5.5.10. [DOI] [PubMed] [Google Scholar]
- 115.Mason BN, Russo AF. Vascular contributions to migraine: time to revisit? Front Cell Neurosci. 2018;12:233. doi: 10.3389/fncel.2018.00233. [DOI] [PMC free article] [PubMed] [Google Scholar]