Abstract
The Coronavirus disease 19 (COVID-19) pandemic has increased the burden of stress on the global healthcare system in 2020. Point of care ultrasound (PoCUS) is used effectively in the management of pulmonary, cardiac and vascular pathologies. POCUS is the use of traditional ultrasound imaging techniques in a focused binary manner to answer a specific set of clinical questions. This is an imaging technique that delivers no radiation, is inexpensive, ultraportable and provides results instantaneously to the physician operator at the bedside. In regard to the pandemic, PoCUS has played a significant adjunctive role in the diagnosis and management of co-morbidities associated with COVID-19. PoCUS also offers an alternative method to image obstetric patients and the pediatric population safely in accordance with the ALARA principle. Finally, there have been numerous PoCUS protocols describing the effective use of this technology during the COVID-19 pandemic.
Keywords: PoCUS, Ultrasound, COVID-19, Coronavirus
Introduction
COVID-19 is a novel virus from the coronavirus family. It has a mean incubation period of 4–5 days however, [1, 2] COVID-19 spreads via respiratory droplets from person-to-person and causes an acute respiratory illness [3]. While the information on the pathogenesis and pathology of the disease is quickly evolving and vast with large variations on the severity of disease, the major symptoms include fever, fatigue, dry cough, dyspnea and anosmia [4]. Since notification of the first instances of a cluster of pneumonias with an unknown cause in Wuhan, China on the 31st of December 2019, COVID-19 has spread quickly throughout 216 countries globally [4]. Declared a pandemic by the WHO on March 11th, 2020, the disease has led to 35 million infections and 1 million deaths [5]. The rise of COVID-19 globally has placed significant pressure on healthcare and its resources.
The current gold standard diagnostic method is reverse transcription-PCR (RT-PCR) testing of a nasopharyngeal swab [6, 7]. Alternatively, chest X-ray (CXR) and chest computed tomography (CT) are commonly used imaging modalities. A CXR is less sensitive than a chest CT and they both subject the patient to varying degrees of radiation [8, 9]. PoCUS refers to the act of using ultrasound during a standard clinical assessment as an adjuvant diagnostic tool. Ultrasonography has proven to be an alternative solution in offering a safe and quick first-line bedside diagnostic exam for COVID-19 lung, cardiac and venous thromboembolic manifestations [10–12]. In this review, the implications of PoCUS in the management of COVID-19 patients will be explored.
Methods
To complete this literary review, articles from PubMed.org database were reviewed for eligibility. No language, date or age restrictions were applied. A search string was designed using the following terms: COVID-19, coronavirus, point of care ultrasound, and PoCUS with the following filters applied: clinical trial, meta-analysis, randomized controlled trial, review, systematic review. Papers deemed eligible based on abstract review were accessed as full-length articles for analysis.
PoCUS advantages and limitations
Nanotechnological advancements in technology have enabled ultrasound to become an affordable and portable imaging modality. Whether it is a cart-based ultrasound machine or a handheld device, a scan can be conducted at the bedside quickly and affordably while providing physicians with results in real time [13, 14]. In regard to COVID-19, PoCUS offers a non-invasive option to screen and trend patients safely. Disinfection protocols include sheathing and disinfection of the ultrasound transducer [10]. Although an ultrasound device may act as a fomite for COVID-19, following a simple checklist can assist physicians in the disinfection process to safely reduce contamination (Table 1) [11, 15–18].
Table 1.
Modified PoCUS machine disinfection checklist: COVID-19 point-of-view
| Pre-Scan | Minimize the amount of additional equipment on the ultrasound cart and if possible designate certain devices as COVID-19-specific |
| If possible, cover the machine and probe in a protective plastic sheath | |
| Use single-use gel packets rather than a reusable bottle | |
| Post-Scan | Inspect the probe and thoroughly sanitize the machine/reusable plastic sheath using approved-disinfectant wipes while wearing personal protective equipment (PPE)a |
| Remove the machine from the patient’s room followed by doffing PPE | |
| Reinspect the machine; re-apply new gloves and disinfect the machine once again |
a Disinfecting hand-held PoCUS device can be less strenuous with the use of smaller disposable plastic sheaths
Additionally, the portability of PoCUS reduces the risk of transmission to staff and equipment exposure, which in turn conserves valuable personal protective equipment (PPE) and supplies [11]. Rather than transporting a patient through the hospital to the radiology department, a dedicated ultrasound machine in a COVID-19 unit may be brought to the patient’s bedside. A single physician can interact with the patient minimizing staff exposure while performing an exam.
In comparison to CT imaging, PoCUS is a non-ionizing imaging modality which offers comparable sensitivity and accuracy in the diagnosis of COVID-19 lung involvement [19]. In comparison to a portable X-ray which correlated to CT lung findings by 62%, PoCUS paralleled CT lung findings of COVID-19 by 87% [20]. Another study concluded that while comparing ultrasound to CT images of alveolar-interstitial patterns in the same COVID-19 patients, PoCUS had a sensitivity of 60% compared to only 39% in CT images [21]. Additionally, PoCUS is extremely beneficial in monitoring the progression of cardiac and venous abnormalities associated with COVID-19 [11].
Although PoCUS is a useful tool, it does carry limitations. To acquire clinically useful images, the operator must have sufficient experience using an ultrasound machine [11, 13]. Patients with an elevated body habitus or compromised status may impair the operator’s ability to obtain a clear visual [22]. In addition, PoCUS images may be difficult to interpret, which may lead to missed findings or require further investigations using alternative imaging modalities [11].
PoCUS for COVID-19 lung involvement
The organ system most commonly involved by the coronavirus is the respiratory tract. It can manifest as a mild viral pneumonia or acute respiratory distress syndrome [23, 24]. Lung ultrasound (LUS) has proven to be an invaluable first-line diagnostic tool when it comes to COVID-19 patients. It has an overall diagnostic sensitivity and specificity of 90.2% (67.6–99.3%) and 88.8% (81.8–94.4%) in COVID-19 pneumonia when compared to CXR, CT and clinical exam [25]. Additionally, while COVID-19 has a preference to affect the posterior-basal lung zones, ultrasound provides effective visualization of the lung’s peripheries [10, 26–30]. LUS is not capable of visualising central lung lesions—these are best seen on cross-sectional CT imaging.
Common pathologies visualized using LUS during COVID-19 are multifocal B lines, sub-pleural/lobar consolidations with decreased doppler signal, bilateral alveolar-interstitial pattern, pleural irregularities, air bronchograms and less commonly pleural effusions [9, 11, 18, 30–33]. B-lines are defined as reverberation artifacts that are represented as smooth vertical lines that extend from the pleural line to the far field while obliterating A-lines [34, 35]. Particularly in COVID-19, B-lines are commonly visualized in the posterior-lateral lung zones in the early phases of the disease [33]. In addition to pleuropathies, consolidations are pathological and can be identified peripherally and inferior to or disrupting the pleural line [9, 18, 30, 31]. Air bronchograms are visualized as bright opacities distal to a consolidation when the ultrasound wave reflects off of an air-filled bronchus [9, 18, 31]. As previously stated, pleural effusions are uncommon in COVID-19 but can be seen clearly as anechoic regions found cephalad to the diaphragm [9, 18, 30, 31].
PoCUS for COVID-19 cardiac involvement
PoCUS has played a pivotal role in monitoring patients’ cardiac function, especially those with pre-existing cardiovascular co-morbidities [10, 12]. A point-of-care echocardiogram may be useful to evaluate patient status when they become hemodynamically unstable or have elevated cardiac biomarkers [12]. Cardiac involvement in COVID-19 presents in a large proportion of patients and as a multitude of pathologies. Cardiac involvement of the disease is very common amongst patients and the process can be either via primary viral infection or secondary activation of the immune cascade [14, 23]. These processes directly affect cardiac function from resultant myocarditis and pulmonary embolisms (PE) [17, 23].
PoCUS has high accuracy when used to evaluate left and right ventricular function, valvular dysfunction, pericardial effusion and to calculate stroke volume [10, 36]. In monitoring PE occurrence, PoCUS has been used to assess right ventricular function and resulting pulmonary hypertension. The ability to identify these findings using cardiac PoCUS provides information for whether or not additional management is required [37].
PoCUS for COVID-19 vascular involvement
Fluid status changes and vascular abnormalities are commonly associated with COVID-19. It has been suggested that inflammation caused by COVID-19 may increase vascular permeability, thus reducing intravascular volume [38]. The hepatic, portal and intra-renal veins can be visualized using PoCUS to accurately assess fluid status in hospitalized COVID-19 patients [36]. If PoCUS is conducted serially, it is extremely beneficial in monitoring the effect of fluid administration in hemodynamically unstable patients [14].
Similarly, to other critically ill patients, COVID-19 has been associated with an increased risk for thromboembolic events [11]. A two-point compression PoCUS ultrasound examination may be utilized to assess for deep vein thrombosis (DVT) in the femoral and popliteal veins [11, 36]. Given the difficulties in diagnosing a PE with superimposed lung involvement using CT pulmonary angiography, venous doppler studies are essential in guiding appropriate management [14].
Ultrasound-guided venous access provides physicians with an abundance of advantages. PoCUS can be utilized to assess for vessel thrombi prior to intravenous puncture, it may also help distinguish a vein from the artery [12]. It can also assess lung sliding pre- and post-procedural during central line placement to diagnose iatrogenic pneumothorax [12]. Particularly in COVID-19 patients, these parameters are very important to account for to prevent precipitating a thromboembolic event or worsening of concomitant lung involvement.
PoCUS for COVID-19 in pregnancy
PoCUS is particularly useful in pregnant women and monitoring disease progression of COVID-19 [39–42]. Accessibility at the bedside and elimination of radiation exposure enables ultrasound to be used to serially track COVID-19 manifestations while pregnant [40]. Although CT imaging is used to diagnose and monitor pulmonary disease progression in many COVID-19 patients, the downsides of radiation exposure outweigh the benefits. In theory, reducing the amount of radiation used would be the solution, however, CT with reduced radiation levels has been found to be insensitive in the early and/or mild COVID-19 cases [43].LUS is proven to correlate with CT images and is therefore feasible during pregnancy [3, 44].
In addition, obstetricians and gynecologists may be adequately trained to perform a fetal ultrasound followed by a LUS examination in pregnant patients with a suspected or known COVID-19 diagnosis [45, 46]. This minimizes the need for various ultrasound operators and equipment, reducing the exposure to potential infection. Moreover, the severity of the disease seen on LUS may influence treatment decisions and subsequently the outcome of the pregnancy [43].
PoCUS for COVID-19 in neonates and children
Ultrasonography is a safe and effective tool to monitor neonatal lung and cardiac diseases. Its neonatal application in COVID-19 has been used to assess the progression of lung involvement [47–50]. Interestingly, some neonates with COVID-19 were found to have signs of lung involvement on LUS, that did not coincide with any respiratory decompensation, commonly seen in adults [51]. Similarly to adults, B-lines, pleural irregularities, and consolidations were noted in neonates [51].
Although much of the discussion around COVID-19 and ultrasound refers to its use in adults, it is also a practical tool when it comes to assessing infection in children. A majority of children are asymptomatic, yet those who present with symptoms commonly have a fever, cough or both [52]. It has been suggested that in early disease, not all children display characteristic COVID-19 LUS findings [53]. However, when they do, ultrasound findings include pleural irregularities, sub-pleural consolidations and B lines [54]. Therefore, in addition to the use of LUS in other viral pneumonias, there is compelling evidence suggesting LUS should be used at the bedside in children [54].
Less frequently, children have been reported to develop multi-system inflammatory syndrome (MIS); a syndrome which closely mimics Kawasaki disease [55]. This can present as a rash, bilateral conjunctivitis, myocardial dysfunction, shock, coagulopathy or acute gastrointestinal distress [55]. A large majority of these children with MIS present with cardiac manifestations including arrhythmias, ventricular dysfunction and coronary dilatation, primarily caused by focal necrosis and fibrosis of the myocardium [33]. Furthermore, to prevent the overuse of CT on children, ultrasound may be a useful modality in the evaluation of cardiac dysfunction, fluid status and vascular abnormalities in the COVID-19 pediatric population [54–56].
PoCUS scanning protocol options in COVID-19
As a result of COVID-19, numerous PoCUS scanning protocols have been introduced to best assess patient status. (Table 2) Each protocol was designed to quickly assess COVID-19 patients in the emergency department or the intensive care unit. This not only minimizes exposure to potential respiratory droplets but also gives the physicians a more well-rounded clinical picture of the patient’s current condition.
Table 2.
Summaries of PoCUS Protocols
| Date Introduced for COVID19 | Authors | Pulmonary assessment | Lung zones | Cardiac assessment | Vascular assessment | Details (Position, transducer, system examined, time required) | Population studied | ||
|---|---|---|---|---|---|---|---|---|---|
| End SBT Protocol [59] | March 12th, 2020 | Peng et al. | ✓ | 12 |
Originally for patients with postextubation distress Upper and lower posterior zones Upper and lower axillary zones Upper and lower anterior zones |
20 adult patients at Xiangya Hospital [60] | |||
| LUSCOVID Protocol [33] | March 30th, 2020 | Soldati et al. | ✓ | 14 |
10 s per zone Linear/convex transducer Basal, middle and upper paravertebral line Basal and upper midaxillary line Basal and upper midclavicular line |
1462 COVID-19 patients across 20 USA/European hospitals [25] 1 pregnant woman with COVID-19 at a tertiary hospital in Rome [40 10 children with COVID-19 at 2 tertiary hospitals in Rome [54] 88 adult COVID-19 patients from 3 Italian hospitals [28] |
|||
| ASE Protocol [11] | April 15th, 2020 | Johri et al. | ✓ | 8–10 | ✓ | ✓ |
Assess ventricles, pericardium and valves Perform an 8–12 zone lung scan Assess the jugular venous pressure (JVP), subcostal inferior vena cava (IVC) and leg veins |
77 COVID-19 patients in the Adan General Hospital ICU [28] | |
| DLETE Protocol [61] | April 18th, 2020 | Fox et al. | ✓ | 8 | ✓ | ✓ |
10-min examination Linear/phased array transducer Perform a focused ECHO Perform an 8-zone lung scan Assess the IVC and leg veins for DVTs |
– | |
|
CLUE Protocol [6] |
May 9th, 2020 | Manivel et al. | ✓ | 12 |
Upright position Linear/convex transducer Upper and lower posterior zones Upper and lower lateral zones Upper and lower anterior zones |
– | |||
| BLUEa Protocol [57] | May 15th, 2020 | Karagöz et al. | ✓ | 12 |
Upright position Upper and lower posterior zones Upper and lower axillary zones Upper and lower anterior zones |
20 adult patients at Xi’an Chest Hospital [58] | |||
| Six Zone Protocol [30] | June 12th, 2020 | Antúnez-Montes et al. | ✓ | 6 |
Upright/prone position Linear/curvilinear transducer Bilateral posterior, lateral superior, and lateral inferior zones |
38 COVID-19 patients in Tongji Hospital, Wuhan [29] | |||
The ‘under 2-min’ Six Zone LUS Protocol [29, 30] proposes that the operator situates themselves posterior to the patient sitting upright, and three scans are conducted bilaterally: posterior zone of the chest wall, lateral superior and inferior zones of the axilla (Fig. 1). The CLUE Protocol [6], BLUE Protocol [57, 58] and the end spontaneous breathing trial (SBT) Protocol [59, 60] involve a more comprehensive twelve-zone LUS assessment. The CLUE Protocol produces a score of 0–3 per zone, with 3 representing more severe disease. The BLUE Protocol offers insight into what the underlying pulmonary pathology may be depending on the specific LUS findings observed. In regard to COVID-19, the presence of multiple diffuse B-lines indicates pulmonary edema, whereas consolidations indicate pneumonia [57]. The end SBT LUS protocol provides a score of 0 for a normal LUS, 1 or 2 for the presence of B-lines and 3 for consolidation [59]. The LUSCOVID Protocol [25, 28, 33, 39, 54, 61, 62] assesses 14-zones thus it is the most extensive LUS protocol.
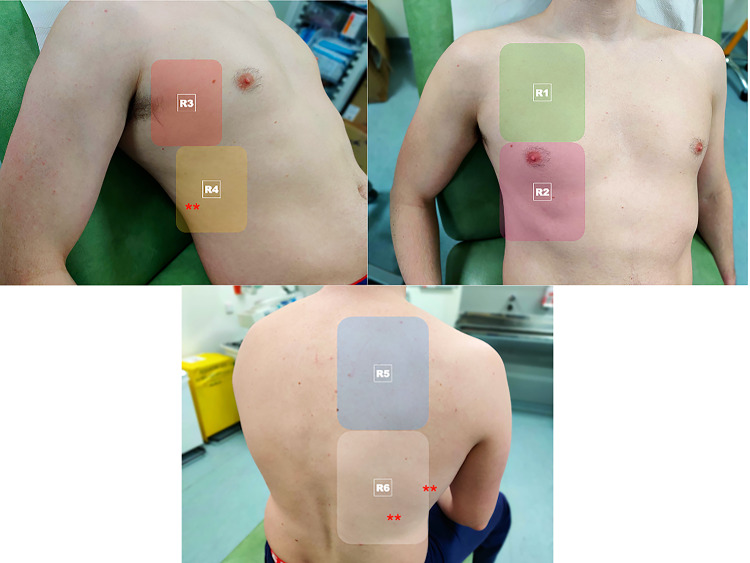
Fig. 1.
12 zone scanning protocol showing 2 anterior zones, 2 lateral zones and 2 posterior zones. Asterisks (*) indicate the posterobasal areas where COVID19 changes occur most frequently
The ASE Protocol [11, 63] and DLETE [64] are the most comprehensive and are comprised of cardiac, lung and venous assessment which encompasses the main manifestations of COVID-19.
Conclusion
PoCUS’ usefulness as an adjunctive tool in the management of COVID-19 is strong. The portability, availability and the real-time nature of ultrasound provides physicians with a safe imaging modality for pulmonary, cardiac and vascular COVID-19 manifestations. With no risk of radiation exposure, ultrasonography is beneficial when used to assess lung involvement in pregnant women. Additionally, ultrasound is practical and effective for use in pediatric COVID-19 patients.
Funding
Open Access funding provided by the IReL Consortium. No funding was received during the creation of this review article.
Declarations
Competing interests
There are no conflicts of interest.
Ethical approval
If human beings have participated in the research (**) All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. If human beings have NOT participated in the research. This article does not contain any studies with human participants or animals performed by any of the authors.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
John Karp, Email: johnkarp@rcsi.com.
Karina Burke, Email: karinaburke@rcsi.com.
Sarah-Marie Daubaras, Email: sarahdaubaras@rcsi.com.
Cian McDermott, Email: cianmcdermott@gmail.com.
References
- 1.Guan W, Ni Z, Hu Y, Liang W, Ou C, He J, et al. Clinical Characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020;382(18):1708–1720. doi: 10.1056/NEJMoa2002032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Li Q, Guan X, Wu P, Wang X, Zhou L, Tong Y, et al. Early Transmission dynamics in Wuhan, China, of novel coronavirus-infected pneumonia. N Engl J Med. 2020;382(13):1199–1207. doi: 10.1056/NEJMoa2001316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Meyerowitz E, Richterman A, Gandhi R, Sax P. Transmission of SARS-CoV-2: a review of viral, host, and environmental factors. Annals Int Med. 2020;21:771. doi: 10.7326/M20-5008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Stokes E, Zambrano L, Anderson K, Marder E, Raz K, El Burai FS, et al. Coronavirus disease 2019 case surveillance—United States, January 22–May 30, 2020. MMWR Morb Mortal Wkly Rep. 2020;69(24):759–765. doi: 10.15585/mmwr.mm6924e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Timeline: WHO's COVID-19 response [Internet]. Who.int. 2020. https://www.who.int/emergencies/diseases/novel-coronavirus-2019/interactive-timeline#event-0. Accessed 24 Sept 2020
- 6.Manivel V, Lesnewski A, Shamim S, Carbonatto G, Govindan T. CLUE: COVID-19 lung ultrasound in emergency department. Emerg Med Australas. 2020;32(4):694–696. doi: 10.1111/1742-6723.13546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rafiee M, Parsaei F, RahimiPordanjani S, Amiri V, Sabour S. A review on applicable and available paraclinical methods for diagnosis of coronavirus disease-19. Arch Iran Med. 2020;23(11):794–800. doi: 10.34172/aim.2020.106. [DOI] [PubMed] [Google Scholar]
- 8.Pare J, Camelo I, Mayo K, Leo M, Dugas J, Nelson K, et al. Point-of-care lung ultrasound is more sensitive than chest radiograph for evaluation of COVID-19. Western J Emerg Med. 2020;21(4):771. doi: 10.5811/westjem.2020.5.47743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Moore S, Gardiner E. Point of care and intensive care lung ultrasound: a reference guide for practitioners during COVID-19. Radiography. 2020;26(4):e297–e302. doi: 10.1016/j.radi.2020.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Khanji M, Ricci F, Patel R, Chahal A, Bhattacharyya S, Galusko V, et al. The role of hand-held ultrasound for cardiopulmonary assessment during a pandemic. Progress Cardiovasc Dis. 2020;63:690–695. doi: 10.1016/j.pcad.2020.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Johri A, Galen B, Kirkpatrick J, Lanspa M, Mulvagh S, Thamman R. ASE statement on point-of-care ultrasound during the 2019 novel coronavirus pandemic. J Am SocEchocardiogr. 2020;33(6):670–673. doi: 10.1016/j.echo.2020.04.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mathews B, Koenig S, Kurian L, Galen B, Mints G, Liu G, et al. Clinical progress note: point-of-care ultrasound applications in COVID-19. J Hosp Med. 2020;15(6):353–355. doi: 10.12788/jhm.3454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Rubulotta F, Soliman-Aboumarie H, Filbey K, Geldner G, Kuck K, Ganau M, et al. Technologies to optimize the care of severe COVID-19 patients for health care providers challenged by limited resources. AnesthAnalg. 2020;131(2):351–364. doi: 10.1213/ANE.0000000000004985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Chiem A, Shibata J, Lim G, Liu Y. Pick Up Your Probes. J Ultrasound Med. 2020. [DOI] [PMC free article] [PubMed]
- 15.Kim D, Jelic T, Woo M, Heslop C, Olszynski P. Just the Facts: Recommendations on point-of-care ultrasound use and machine infection control during the coronavirus disease 2019 pandemic. CJEM. 2020;22(4):445–449. doi: 10.1017/cem.2020.364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gogna A, Yogendra P, Lee S, Aziz A, Cheong E, Chan L, et al. Diagnostic ultrasound services during the coronavirus disease (COVID-19) pandemic. Am J Roentgenol. 2020;215:1–6. doi: 10.2214/AJR.20.23167. [DOI] [PubMed] [Google Scholar]
- 17.Abrams E, Rose G, Fields J, Esener D. Point-of-Care ultrasound in the evaluation of COVID-19. J Emerg Med. 2020;59:403–408. doi: 10.1016/j.jemermed.2020.06.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.McDermott C, Daly J, Carley S. Combatting COVID-19: is ultrasound an important piece in the diagnostic puzzle? Emerg Med J. 2020;37(10):644–649. doi: 10.1136/emermed-2020-209721. [DOI] [PubMed] [Google Scholar]
- 19.Smallwood N, Walden A, Parulekar P, Dachsel M. Should point-of-care ultrasound become part of healthcare worker testing for COVID? Clin Med. 2020;20(5):486–487. doi: 10.7861/clinmed.2020-0442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Tierney D, Huelster J, Overgaard J, Plunkett M, Boland L, St. Hill C, et al. Comparative performance of pulmonary ultrasound, chest radiograph, and CT among patients with acute respiratory failure*. Crit Care Med. 2020;48(2):151–157. doi: 10.1097/CCM.0000000000004124. [DOI] [PubMed] [Google Scholar]
- 21.Yang Y, Huang Y, Gao F, Yuan L, Wang Z. Lung ultrasonography versus chest CT in COVID-19 pneumonia: a two-centered retrospective comparison study from China. Intensive Care Med. 2020;46(9):1761–1763. doi: 10.1007/s00134-020-06096-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Huang G, Vengerovsky A, Morris A, Town J, Carlbom D, Kwon Y. Development of a COVID-19 point-of-care ultrasound protocol. J Am SocEchocardiogr. 2020;33(7):903–905. doi: 10.1016/j.echo.2020.04.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Agricola E, Beneduce A, Esposito A, Ingallina G, Palumbo D, Palmisano A, et al. Heart and lung multimodality imaging in COVID-19. JACC Cardiovascular Imag. 2020;13(8):1792–1808. doi: 10.1016/j.jcmg.2020.05.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Xu J, Ma X, Bai L, Wang M, Deng W, Ning N. A systematic review of etiology, epidemiology, clinical manifestations, image findings, and medication of 2019 Corona Virus Disease-19 in Wuhan, China. Medicine. 2020;99(42):e22688. doi: 10.1097/MD.0000000000022688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Volpicelli G, Gargani L, Perlini S, Spinelli S, Barbieri G, Lanotte A, et al. Lung ultrasound for the early diagnosis of COVID-19 pneumonia: an international multicenter study. Intens Care Med. 2021 doi: 10.1093/ehjci/jeaa163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Duggan N, Shokoohi H, Liteplo A, Huang C, Goldsmith A. Best practice recommendations for point-of-care lung ultrasound in patients with suspected COVID-19. J Emerg Med. 2020;59:515–520. doi: 10.1016/j.jemermed.2020.06.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Smargiassi A, Soldati G, Torri E, Mento F, Milardi D, Giacomo P, et al. Lung ultrasound for COVID-19 patchy pneumonia: extended or limited evaluations? J Ultrasound Med. 2020;40:521–528. doi: 10.1002/jum.15428. [DOI] [PubMed] [Google Scholar]
- 28.Mento F, Perrone T, Macioce V, Tursi F, Buonsenso D, Torri E, et al. On the impact of different lung ultrasound imaging protocols in the evaluation of patients affected by coronavirus disease 2019. J Ultrasound Med. 2020 doi: 10.1002/jum.15580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Zhu F, Zhao X, Wang T, Wang Z, Guo F, Xue H, et al. Ultrasonic characteristics and severity assessment of lung ultrasound in COVID-19 pneumonia in Wuhan, China: a retrospective Observational Study. Engineering. 2020 doi: 10.1016/j.eng.2020.09.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Antúnez-Montes O, Buonsenso D. Routine use of point-of-care lung ultrasound during the COVID-19 pandemic. Med Intensiva. 2020 doi: 10.1016/j.medin.2020.04.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Smith M, Hayward S, Innes S, Miller A. Point-of-care lung ultrasound in patients with COVID-19–a narrative review. Anaesthesia. 2020;75(8):1096–1104. doi: 10.1111/anae.15082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Smargiassi A, Soldati G, Borghetti A, Scoppettuolo G, Tamburrini E, Testa A, et al. Lung ultrasonography for early management of patients with respiratory symptoms during COVID-19 pandemic. J Ultrasound. 2020;23(4):449–456. doi: 10.1007/s40477-020-00501-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Soldati G, Smargiassi A, Inchingolo R, Buonsenso D, Perrone T, Briganti D, et al. Proposal for international standardization of the use of lung ultrasound for patients with COVID -19. J Ultrasound Med. 2020;39(7):1413–1419. doi: 10.1002/jum.15285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Soldati G, Demi M, Inchingolo R, Smargiassi A, Demi L. On the physical basis of pulmonary sonographic interstitial syndrome. J Ultrasound Med. 2016;35(10):2075–2086. doi: 10.7863/ultra.15.08023. [DOI] [PubMed] [Google Scholar]
- 35.Demi L, Demi M, Smargiassi A, Inchingolo R, Faita F, Soldati G. Ultrasonography in lung pathologies: new perspectives. MultidisciplinRespirat Med. 2014;9(1):27. doi: 10.1186/2049-6958-9-27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Koratala A, Ronco C, Kazory A. Need for objective assessment of volume status in critically Ill patients with COVID-19: The Tri-POCUS approach. Cardiorenal Med. 2020;10(4):209–216. doi: 10.1159/000508544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Zhang L, Wang B, Zhou J, Kirkpatrick J, Xie M, Johri A. Bedside focused cardiac ultrasound in COVID-19 from the Wuhan Epicenter: The role of cardiac point-of-care ultrasound, limited transthoracic echocardiography, and critical care echocardiography. J Am SocEchocardiogr. 2020;33(6):676–682. doi: 10.1016/j.echo.2020.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Thalappillil R, White R, Tam C. POCUS to guide fluid therapy in COVID-19. J CardiothoracVascAnesth. 2020;34(10):2854–2856. doi: 10.1053/j.jvca.2020.04.049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Inchingolo R, Smargiassi A, Moro F, Buonsenso D, Salvi S, Del Giacomo P, et al. The diagnosis of pneumonia in a pregnant woman with coronavirus disease 2019 using maternal lung ultrasound. Am J ObstetGynecol. 2020;223(1):9–11. doi: 10.1016/j.ajog.2020.04.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Buonsenso D, Raffaelli F, Tamburrini E, Biasucci D, Salvi S, Smargiassi A, et al. Clinical role of lung ultrasound for diagnosis and monitoring of COVID-19 pneumonia in pregnant women. Ultrasound ObstetGynecol. 2020;56(1):106–109. doi: 10.1002/uog.22055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Yassa M, Mutlu M, Kalafat E, Birol P, Yirmibeş C, Tekin A, et al. How to perform and interpret the lung ultrasound by the obstetricians in pregnant women during the SARS-CoV-2 pandemic. J Turkish Soc Obstetric Gynecol. 2020;17(3):225–232. doi: 10.4274/tjod.galenos.2020.93902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Yassa M, Mutlu M, Birol P, Kuzan T, Kalafat E, Usta C, et al. Lung ultrasonography in pregnant women during the COVID-19 pandemic: an interobserver agreement study among obstetricians. Ultrasonography. 2020;39(4):340–349. doi: 10.14366/usg.20084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Yassa M, Birol P, Mutlu A, Tekin A, Sandal K, Tug N. Lung Ultrasound can influence the clinical treatment of pregnant women with COVID -19. J Ultrasound Med. 2020;40(1):191–203. doi: 10.1002/jum.15367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Kalafat E, Yaprak E, Cinar G, Varli B, Ozisik S, Uzun C, et al. Lung ultrasound and computed tomographic findings in pregnant woman with COVID-19. Ultrasound ObstetGynecol. 2020;55(6):835–837. doi: 10.1002/uog.22034. [DOI] [PubMed] [Google Scholar]
- 45.Moro F, Buonsenso D, Merwe J, Bourne T, Deprest J, Froyman W et al. A Prospective international lung ultrasound analysis study in tertiary maternity wards during the severe acute respiratory syndrome coronavirus 2 pandemic. J Ultrasound Med. 2020. [DOI] [PMC free article] [PubMed]
- 46.Buonsenso D, Moro F, Inchingolo R, Smargiassi A, Demi L, Soldati G, et al. Effectiveness of rapid lung ultrasound training program for gynecologists and obstetricians managing pregnant women with suspected COVID-19. Ultrasound ObstetGynecol. 2020;56(1):110–111. doi: 10.1002/uog.22066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Tsankov B, Allaire J, Irvine M, Lopez A, Sauvé L, Vallance B, et al. Severe COVID-19 infection and pediatric comorbidities: a systematic review and meta-analysis. Int J Infect Dis. 2020;103:246–256. doi: 10.1016/j.ijid.2020.11.163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Zhang C, Gu J, Chen Q, Deng N, Li J, Huang L, et al. Clinical and epidemiological characteristics of pediatric SARS-CoV-2 infections in China: a multicenter case series. PLoS Med. 2020;17(6):e1003130. doi: 10.1371/journal.pmed.1003130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Guo C, He L, Yin J, Meng X, Tan W, Yang G, et al. Epidemiological and clinical features of pediatric COVID-19. BMC Med. 2020;18(1):1–7. doi: 10.1186/s12916-019-1443-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Parri N, Lenge M, Cantoni B, Arrighini A, Romanengo M, Urbino A, et al. COVID-19 in 17 Italian Pediatric Emergency Departments. Pediatrics. 2020;146:e20201235. doi: 10.1542/peds.2020-1235. [DOI] [PubMed] [Google Scholar]
- 51.Gregorio-Hernández R, Escobar-Izquierdo A, Cobas-Pazos J, Martínez-Gimeno A. Point-of-care lung ultrasound in three neonates with COVID-19. Eur J Pediatr. 2020;179(8):1279–1285. doi: 10.1007/s00431-020-03706-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Wang Z, Zhou Q, Wang C, Shi Q, Lu S, Ma Y, et al. Clinical characteristics of children with COVID-19: a rapid review and meta-analysis. Annals Translat Med. 2020;8(10):620–620. doi: 10.21037/atm-20-3302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Scheier E, Guri A, Balla U. Lung ultrasound cannot be used to screen for Covid-19 in children. Eur Rev PharmacolSci. 2020;9:4623–4624. doi: 10.26355/eurrev_202005_21145. [DOI] [PubMed] [Google Scholar]
- 54.Musolino A, Supino M, Buonsenso D, Ferro V, Valentini P, Magistrelli A, et al. Lung ultrasound in children with COVID-19: PREliminary findings. Ultrasound Med Biol. 2020;46(8):2094–2098. doi: 10.1016/j.ultrasmedbio.2020.04.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Jiang L, Tang K, Levin M, Irfan O, Morris S, Wilson K, et al. COVID-19 and multisystem inflammatory syndrome in children and adolescents. Lancet Infect Dis. 2020;20(11):e276–e288. doi: 10.1016/S1473-3099(20)30651-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Liu E, Smyth R, Luo Z, Qaseem A, Mathew J, Lu Q, et al. Rapid advice guidelines for management of children with COVID-19. Annals Translat Med. 2020;8(10):617–617. doi: 10.21037/atm-20-3754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Karagöz A, Sağlam C, Demirbaş H, Korkut S, Ünlüer E. Accuracy of bedside lung ultrasound as a rapid triage tool for suspected Covid-19 Cases. Ultrasound Q. 2020;36(4):339–344. doi: 10.1097/RUQ.0000000000000530. [DOI] [PubMed] [Google Scholar]
- 58.Huang Y, Wang S, Liu Y, Zhang Y, Zheng C, Zheng Y, et al. A Preliminary study on the ultrasonic manifestations of peripulmonary lesions of non-critical novel coronavirus pneumonia (COVID-19) SSRN Electron J. 2020;46:2908–2917. [Google Scholar]
- 59.Soummer A, Perbet S, Brisson H, Arbelot C, Constantin J, Lu Q, et al. Ultrasound assessment of lung aeration loss during a successful weaning trial predicts postextubation distress*. Crit Care Med. 2012;40(7):2064–2072. doi: 10.1097/CCM.0b013e31824e68ae. [DOI] [PubMed] [Google Scholar]
- 60.Peng Q, Wang X, Zhang L. Findings of lung ultrasonography of novel corona virus pneumonia during the 2019–2020 epidemic. Intensive Care Med. 2020;46(5):849–850. doi: 10.1007/s00134-020-05996-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Perrone T, Soldati G, Padovini L, Fiengo A, Lettieri G, Sabatini U, et al. A new lung ultrasound protocol able to predict worsening in patients affected by severe acute respiratory syndrome coronavirus 2 pneumonia. J Ultrasound Med. 2020 doi: 10.1002/jum.15548. [DOI] [PubMed] [Google Scholar]
- 62.Smargiassi A, Soldati G, Torri E, Mento F, Milardi D, Del Giacomo P, et al. Lung ultrasound for COVID -19 patchy pneumonia. J Ultrasound Med. 2020;40(3):521–528. doi: 10.1002/jum.15428. [DOI] [PubMed] [Google Scholar]
- 63.Bitar Z, Shamsah M, Bamasood O, Maadarani O, Alfoudri H. Point-of-Care ultrasound for COVID-19 pneumonia patients in the ICU. J CardiovascImag. 2021;29(1):60. doi: 10.4250/jcvi.2020.0138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Fox S, Dugar S. Point-of-care ultrasound and COVID-19. Cleveland Clin J Med. 2020 doi: 10.3949/ccjm.87a.ccc019. [DOI] [PubMed] [Google Scholar]
- 65.Lichtenstein D. Lung ultrasound in the critically ill. Ann Intensive Care. 2014;4(1):1. doi: 10.1186/2110-5820-4-1. [DOI] [PMC free article] [PubMed] [Google Scholar]