Abstract
Purpose
This study aimed to assess the efficacy of vaginally versus orally administered estradiol (E2) and dydrogesterone (DG) on the proliferative and secretory transformation of endometrium in patients with premature ovarian failure (POF) and preparing for assisted reproductive technology.
Methods
Twenty patients with POF who were awaiting oocyte donation were included in the study; they were randomly assigned to two groups to receive E2 and DG either orally or vaginally. Treatment efficacy was compared between the two groups regarding blood E2 concentrations, endometrial thickness, histology using hematoxylin and eosin staining, immunohistochemical analysis of ER expression, and PR and pinopodes morphology using scanning electron microscopy.
Results
E2 concentrations differed significantly between oral and vaginal E2 and DG administration for 14 days (82.3 vs 1015.6 pg/mL; P < 0.001) and 21 days (85.0 vs 809.8 pg/mL; P < 0.001). Endometrial thickening was more pronounced in the vaginal treatment group, and also ER staining was stronger on days 14 and 21 in the vaginal treatment group. PR staining in the endometrium appeared more intense in the oral treatment group, which was, however, not significant. The abundance of developing pinopodes was higher in the vaginal treatment group (P = 0.04).
Conclusion
Vaginal administration of E2 and DG is more effective than oral administration regarding proliferative and secretory transformation of the endometrium in POF patients and preparing for assisted reproductive technology.
Keywords: micronized estradiol, vaginal administration, oral administration, pinopodes, premature ovarian failure
Introduction
Hormonal supplementation is crucial for preparation of the endometrium for frozen-thawed embryo transfer (FET) to produce adequate endometrial conditions during the implantation window. Numerous drugs and various administration routes have been tested previously in order to optimize implantation pregnancy rates.1 Oral administration elicits endometrial proliferation in the majority of cases during FET cycles and in routine endometrial transformation in patients with premature ovarian failure (POF), and this route of administration is considered convenient; however, when this method is ineffective,2 eg, in patients with a still thin endometrium or recurrent implantation failure,3 vaginal administration may be favorable. Strict comprehensive and individual therapy is used for patients with recurrent implantation failure, which includes improving endometrial receptivity, ameliorating immune responses, and transplanting high-quality embryos only, among others, thus, vaginal administration is a relevant option for some patients.
The vagina is a target organ and an effective systemic entry point for sex steroids, and vaginal administration may result in direct vagina-to-uterus transportation which circumvents the liver first-pass effect that occurs in the gastrointestinal tract.4 Absorption of steroids via the vaginal route may thus help achieve systemic drug delivery.5
Previous studies showed that serum estradiol (E2) levels are distinctly higher after vaginal administration of micronized E2,2,6 which is of concern for clinical doctors. The molecular structure and pharmacologic effects of dydrogesterone (DG), a retro-progesterone, closely resemble those of endogenous progesterone (P), with stable and effective bioavailability after oral administration.7 Vaginal P administration is considered more convenient and efficient than intramuscular or oral administration, according to several clinical trials;8,9 however, there is only a limited number of studies on usage and availability of vaginal DG administration.
Menopausal patients are most suitable for investigating endometrial proliferative and secretory transformation,10,11 as their lack of endogenous E2 and P production facilitates testing bioavailability and effectiveness of different administration routes of hormonal supplementation. In this study, 20 volunteer POF patients who were awaiting oocyte donation were included.
Previous research predominantly focused on comparing clinical efficacy between oral and vaginal administration of E2 regarding factors such as clinical pregnancy rates; however, systematic efficacy and endometrial histological changes were rarely assessed. The aim of this study was to compare oral versus vaginal administration of E2 and DG regarding conventional histology of the endometrium, immunohistochemical changes of ER and PR, and pinopodes development in POF patients awaiting oocyte donation. Furthermore, serum hormone measurements and ultrasound examination of the uterus were performed.
Participants and Methods
Participants
This study was conducted in accordance with the principles of the Declaration of Helsinki. It was reviewed by the Chinese Clinical Trial Register (clinical trial registration number: ChiCTR1900026410) and was approved by the Medical Ethics Committee of Qilu Hospital of Shandong University, China. Written informed consent was obtained from each patient.
Subjects: Twenty married POF patients aged 20–35 years who were awaiting oocyte donation were included, with the inclusion criteria of diagnosed POF with 4–6 months of amenorrhea,12,13 follicle-stimulating hormone (FSH) concentrations > 40 mIU/mL at least twice at an internal of 4–6 weeks, E2 concentrations < 20 pg/mL, endometrium double-wall thicknesses < 5 mm, normal uterine cavity, and no steroid replacement drug treatment in the previous three months. Exclusion criteria were metabolic disorders, a history of thromboembolism, a family history of thrombosis or cardiovascular disease, and a history of blood system disorders.
Treatment protocol: The patients were randomly assigned to an oral and a vaginal treatment group (n = 10, each) using a randomized block design. Patients in the oral group received femoston 2/10 (Abbott Biologicals B.V, Weesp, Netherlands) sequentially by oral administration, which comprised 14 red pills containing 2 mg E2 and 14 yellow pills containing 2 mg E2 and 10 mg DG. The vaginal group received femoston 1/10 vaginally, which comprised 14 white pills containing 1 mg E2 and 14 gray pills containing 1 mg E2 and 10 mg DG. Before treatment, uterine volume and endometrial thickness were measured using transvaginal ultrasound scanning, and hormone measurements were performed regarding E2, P, FSH, and luteinizing hormone (LH) concentrations to assess basal levels. The patients were not subjected to embryo transfer during the study.
In addition, 10 volunteers with normal menstrual cycles were recruited as the control whose serum E2, P, FSH, LH, SHBG, and endometrial thickness in menstrual phase, ovulatory phase and mid-luteal phase were recorded (Supplementary Table 1).
Serum Assays
After 14 and 21 days of treatment, blood samples were collected 12 hours after the last dose. Serum E2, P, FSH, LH, and sex hormone-binding globulin (SHBG) concentrations were measured using an automated electrochemiluminescence immunoassay system (ECLIA; Roche Diagnostics, Mannheim, Germany).
Ultrasonic Examination
After 14 days of treatment, endometrial thickness and endometrial–subendometrial blood flow distribution patterns were examined.14 These patterns were defined as follows: pattern A, vessels penetrating the internal zone of the endometrium; pattern B, vessels entering the hyperechogenic outer margin of the endometrium; and pattern C, vessels penetrating the superficial hypoechogenic area surrounding the endometrium.15 Color Doppler evaluation using a vaginal probe was performed to assess endometrial vascularity. All Doppler evaluations were carried out by one investigator who was blind with respect to treatment groups to prevent bias and interobserver variation.
Histology
After 14 and 21 days (DG administration for 7 days) of treatment, endometrial biopsy was performed, respectively, by the same surgeon using an endometrial pipelle. All specimens were rinsed using saline, and a portion of the specimen was fixed in 4% neutral-buffered formalin for hematoxylin and eosin staining and immunohistochemical (IHC) analyses. The remaining part of samples collected on day 21 was immersed in a 2.5% glutaraldehyde phosphate-buffered solution to examine pinopodes development using scanning electron microscopy.
Common Morphology of the Endometrium
Slices were examined using a Nikon inverted microscope (Nikon, Tokyo, Japan), and observations were recorded using NIS-Elements F software (Ver4.60.00 for 64bit edition, Nikon) at high magnification (100-fold). NIS-Elements F software was used to calculate the cross-sectional area, perimeter, and diameter of each gland and glandular lumen; from these data, the whole area and constituent ratio of glands, glandular lumens, and epithelia were calculated, according to the following equations: the whole glandular epithelial area of each field (%)={(the sum of each glandular area-the sum of each glandular lumens area)÷the whole field’s area}×100%; the whole stroma area of each field (%)={(the whole field’s area-the sum of each glandular area)÷the whole field’s area}×100%.
IHC Staining for Assessing ER and PR
Sections of 4 mm thickness were cut and were placed in a stove at 37 °C overnight. Tissue slices were deparaffinized and rehydrated using an ethanol concentration series, after which antigen retrieval was performed using citrate buffer, and endogenous peroxidase action was blocked by incubating the slices with 3% hydrogen peroxide. The slices were then incubated at 4 °C overnight with polyclonal anti-human ER antibody (PB0188; Boster, Wuhan, China) and PR antibody (PB0077; Boster) at a dilution of 1:100. On the next day, the slices were incubated with a biotinylated secondary antibody. To assess protein expression, a chromogenic reaction was performed using a 3, 30ʹ-diaminobenzidine color reagent kit (DAB: AB1022; Boster). For negative controls, phosphate-buffered saline was used instead of the primary antibody.16
Intensity and distribution of specific IHC staining reactions were evaluated using a semi-quantitative method according to the following equation: HSCORE:∑pi(i+1), where i = the intensity of staining with a value of 1, 2, or 3 (weak, positive, or strong, respectively), and pi = the proportion of stained epithelial cells, ranging from 0% to 100%. Slices were assessed separately by two senior pathologists who were blind with respect to treatment groups.
Evaluation of Pinopodes Development
Slices were washed several times using phosphate buffer, were fixed in 4% osmium phosphate-buffered solution, dehydrated in an acetone solution containing distilled water in a concentration series (from 20% to 100%), and were preserved in 100% acetone. After this, the slices were dried in a critical-point drier using carbon dioxide, were mounted and coated with gold (150–200 Å), and were examined using a scanning electron microscope (SIGMA 300; Zeiss, Oberkochen, Germany) at 3,000-fold magnification.
Two observers who were blind with respect to treatment groups independently examined all biopsies. The period of pinopodes development was assessed according to Nikas et al,17 who differentiated between developing, fully developed, and regressing pinopodes.
Statistical Analyses
All statistical analyses were performed using SPSS 20.0 (IBM Corp., Armonk, NY, USA). Continuous data are shown as Median (Min-Max). Differences in continuous variables between groups were compared using Mann–Whitney U-test, and Chi‑square tests were used to test differences in categorical variables. Statistical significance is reported at P < 0.05.
Results
Demographics
Demographic characteristics of 20 subjects are compared. The mean age and body mass index (BMI) of the patients were similar between the groups {26(23–33) versus 26(22–29) years, 22.10(18.52–25.93) versus 22.03(18.22–24.91) kg/m2, respectively} (P>0.05, Supplementary Table 2).
Serum Assays
After 14 and 21 days, serum E2 levels were significantly higher in the vaginal treatment group (P < 0.001, each), whereas serum P and SHBG concentrations did not differ significantly between groups (Table 1). Serum FSH and LH concentrations decreased more in the vaginal treatment than in the oral treatment group on days 14 and 21 (P < 0.05, each; Table 2).
Table 1.
Clinical Characteristics of POF Patients Between Orally and Vaginally Administering Estradiol and DG for 14 and 21 Days
| Variables | Before | 14 Days | 21 Days | |||
|---|---|---|---|---|---|---|
| OR | VR | OR | VR | OR | VR | |
| FSH(mIU/mL) | 93.0(58.5–156.6) | 105.0(67.5–183.1) c | 50.7(10.9–93.6) | 20.5(11–49) b | 46.4(8.9–87.6) | 12.3(2.9–38.9) a |
| LH(mIU/mL) | 50.9(39.9–105.4) | 49.4(44.6–121.3) c | 35.3(16.1–87.8) | 20.8(10.5–56.3) c | 30.8(17.5–82.1) | 6.4(2.3–42.3) a |
| E2(pg/mL) | 5(5–5) | 5.5(4.6–9.7) c | 82.3(62.4–94.7) | 1015.6(781–1292) a | 85(57.6–122.2) | 809.8(740.3–1278) a |
| P(ng/mL) | 0.44(0.26–0.69) | 0.57(0.34–0.94) c | 0.39(0.05–0.7) | 0.46(0.12–0.67) c | 0.33(0.19–0.7) | 0.41(0.11–0.51) c |
| SHBG (nmol/L) | 62.8(38.9–90.5) | 53.2(36.5–86.5) c | 83.8(33.7–165) | 67.2(34.4–123) c | 89.1(39.4–215) | 82.8(42–110) c |
| ET(mm) | 3 | 3c | 7.5(5–9) | 10.3(9.2–11.6) a | 7.9(6–9) | 9.4(7.2–12.4) a |
| UV(cm3) | 23.7(10.5–44.5) | 27.1(10.1–43.7) c | 49.4(30.9–59.5) | 56.1(44–102.6) c | 53.6(35.6–72.9) | 56.7(45.7–100.3) c |
Notes: Values are showed as median (Min-Max); P values are for Mann–Whitney U-test; aP<0.001; bP <0.05; cP >0.05.
Abbreviations: OR, oral route; VR, vaginal route; SHBG, sex hormone-binding globulin; ET, endometrial thickness; UV, uterine volume.
Table 2.
FSH and LH Decrease of POF Patients Between Orally and Vaginally Administering Estradiol and DG for 14 and 21 Days
| Variables | 14 Days | 21 Days | ||
|---|---|---|---|---|
| OR | VR | OR | VR | |
| FSH decrease (mIU/mL) | 57(8.5–68.2) | 81.1(52.5–134.1) a | 58.5(13–71.7) | 85.1(57.5–147.5) a |
| LH decrease (mIU/mL) | 17.6(12.9–26.6) | 27.6(5.4–78.9) b | 23.6(14.4–30.7) | 43.2(30.7–79) a |
Notes: Values are showed as median (Min-Max); P values are for Mann–Whitney U-test; aP <0.001; bP <0.05.
Abbreviations: OR, oral route; VR, vaginal route.
Ultrasonic Examination
Endometrial thickness increase was significantly higher in the vaginal treatment group than in the oral treatment group after 14 and 21 days of E2 (Table 1, Supplementary Figure 1). On day 14, endometrial and sub-endometrial blood patterns in the vaginal treatment group showed more patterns of category A, which was, however, mot statistically significant (P = 0.472; Table 3).
Table 3.
Endometrial Blood Patterns Between Orally and Vaginally Administering Estradiol and DG for 14 Days
| Variables | Pattern A | Pattern B | Pattern C | P value |
|---|---|---|---|---|
| Oral route(n) | 3 | 4 | 3 | 0.472 |
| Vaginal route(n) | 5 | 4 | 1 |
Notes: Pattern A, vessels entering the hypoechogenic inner area; Pattern B, vessels penetrating the hyperechogenic outer margin of the endometrium; Pattern C, vessels penetrating the outer hypoechogenic area surrounding the endometrium; P values are x2 test.
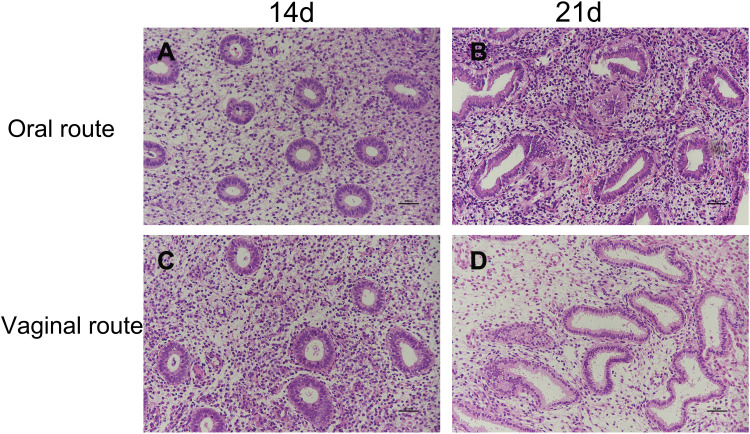
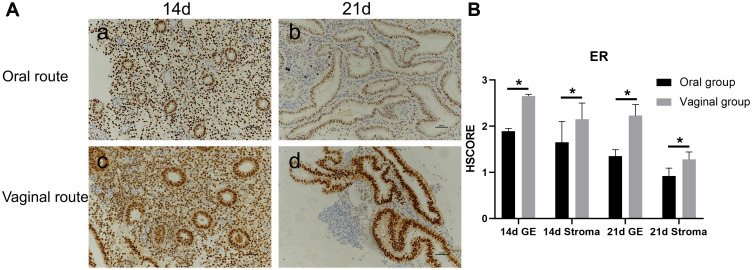
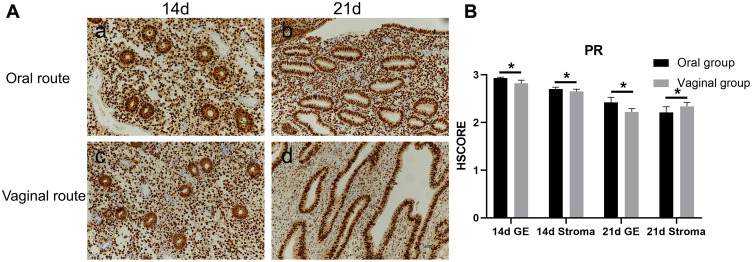
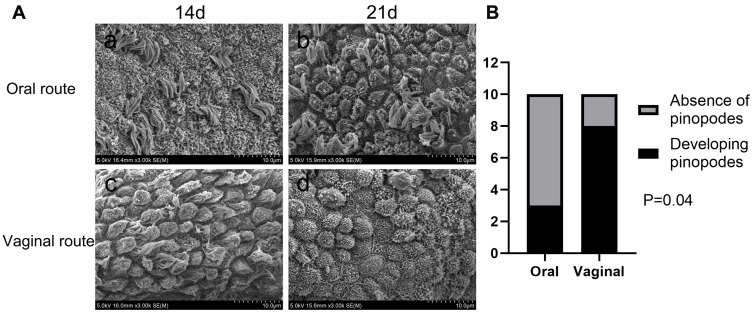
Histology
Proliferative and secretory transformation of endometrium in the vaginal and oral treatment groups are shown in Table 4 and Figure 1. Immunohistochemical localization of ER and PR in the endometrium are shown in Figures 2 and 3, respectively. Pinopode development in both treatment groups is shown in Figure 4.
Table 4.
The Conventional Histology of Endometrium Between Orally and Vaginally Administering Estradiol and DG
| Variables | 14 Days | 21 Days | ||
|---|---|---|---|---|
| OR | VR | OR | VR | |
| Glands area, μm2 | 12659(8903–17982) | 18418(11098–24887) a | 26957(25432–28934) | 49035(44091–53875) a |
| Glands circumference, μm | 425(385–510) | 520(435–626) a | 668(619–690) | 879(832–934) a |
| Glandular lumen area, μm2 | 1730(1297–2980) | 2820(1158–4932) a | 6345(3689–12930) | 15385(10632–16875) a |
| Glandular lumen circumference, μm | 177(140–208) | 229(132–298) b | 435(320–538) | 516(310–601) a |
| Glandular epithelium area, μm2 | 10556(7498–16,252) | 15613(6996–20670) a | 20345(12502–23130) | 34027(32844–37000) a |
| Glandular epithelium mean height, μm | 38.6(34.7–44.9) | 46.8(37.6–52.7) a | 39.9(35.8–46,9) | 35.1(24.3–41.5) a |
| PCT of glands, % | 14.5(12.6–17.1) | 22.1(15.5–26.4) a | 33.7(32.3–37.3) | 34.9(32.3–37.9) b |
| PCT of glandular lumen, % | 2.4(1.8–2.8) | 4.1(1.7–7.6) a | 7.3(6.76–8.1) | 13.1(10.1–15.7) a |
| PCT of glandular epithelium, % | 12.2(10.8–14.2) | 18.0(13.8–19.9) a | 26.4(25.7–29.6) | 21.7(21.2–23.1) a |
| PCT of stroma, % | 85.5(83.7–87.4) | 77.9(73.7–84.5) a | 66.3(62.7–67.7) | 65.2(62.1–67.7) b |
Notes: Values are showed as median (Min-Max); P values are for Mann–Whitney U-test; aP <0.05; bP >0.05.
Abbreviations: OR, oral route; VR, vaginal route; PCT, percentage.
Figure 1.
Proliferative and secretory transformation of endometrium via the vaginal and oral route of estradiol and dydrogesterone (DG). Photomicrographs (×200) showing the amounts of glands in the vaginal group (C, D) were more than the oral (A, B). After 14 days of therapy, the vaginal group had pseudostratified columnar epithelium, curved glands, intercellular substance edema and spindle-shaped cells (C). On day 21 the vaginal group had bigger, curved, serrate glands, active apocrine secretion, large and round interstitial cells, apparent edema and glandular lumens existed secretions. After 21 days of therapy, the vaginal group had bigger, curved, serrate glands, active apocrine secretion, large and round interstitial cells, apparent edema and glandular lumens existed secretions.
Figure 2.
Photomicrographs (×200) showing immunohistochemical localization of ER in endometrium from oral and vaginal women. Both glandular epithelial and stromal compartments demonstrated more intense nuclear immunoreactivity for ER on day 14 (the proliferative phase) (a, c, (A)) than on day 21 (the secretory phase) (b, d, (A)) and more intense in the vaginal versus oral group (*P<0.05, (B)). GE= glandular epithelium. P values are for Mann–Whitney U-test. HSCORE:∑pi(i+1), where i = the intensity of staining, with a value of 1, 2, or 3 (weak, positive, or strong, respectively), and pi = the proportion of stained epithelial cells, varying from 0 to 100%.
Figure 3.
Photomicrographs (×200) showing immunohistochemical localization of PR in endometrium from oral and vaginal women. Both glandular epithelial and stromal compartments demonstrated more intense nuclear immunoreactivity for PR on day 14 (a, c, (A)) than on day 21 (b, d, (A)) and more intense in the oral (a, b, (A)) versus vaginal group (c, d, (A)), but there were no significant differences(*P>0.05, (B)). P values are for Mann–Whitney U-test.
Abbreviation: GE, glandular epithelium.
Figure 4.
(A) Scanning electron micrograph showing the apical surface of the luminal uterine epithelium in endometrial samples obtained on day 21. Note the absence of pinopodes (a) and the presence of the developing pinopodes (b, c, d). Scale bars = 10μm. (B) Only 3 of the oral group patients showed developing pinopodes on day 21, while 8 patients in the vaginal group were observed (P=0.04). None of them showed fully developed pinopodes. P values are for Chi‑square test.
Discussion
To the best of our knowledge, this is the first study assessing endometrial proliferative and secretory transformation after vaginally administering 1 mg E2 and 10 mg DG to POF patients. Changes in hormone levels and endometrial states were not endogenous, as the patients’ ovaries were inactive. Apart from hormone replacement therapy which can ameliorate physical disorders such as hot flashes, excessive sweating, and osteoporosis, alternative strategies including stem cell therapy and ovarian tissue cryopreservation may exert beneficial effects to restore ovarian function in POF patients.18
Previous research revealed that serum E2 levels are significantly higher following vaginal treatment,6 compared to oral treatment, and that there is a significant difference in the decrease of serum LH and FSH concentrations in postmenopausal women receiving estrogen therapy,10 which is in line with our results. In the current study, we administered femoston (E2 and DG) which are commonly administered in FET. Higher levels of estrogen inhibit the pituitary gland to secrete LH and FSH, which helps establish close normal gonadotropic hormone conditions. One of the POF patients of the vaginal treatment group had been diagnosed with POF five years previously, and FSH and LH concentrations were approximately 150 mIU/mL to 190 mIU/mL; however, on day 21 of the current study, the patient’s FSH and LH concentrations were 14.96 mIU/mL and 6.84 mIU/mL, respectively. After bleeding and vaginal administration of E2 and DG, the patient developed an 18-mm follicle at 248 pg/mL E2 and pregnancy was successfully established. This may be due to the decrease in FSH and LH concentrations during the luteal phase when the follicle began to develop; however, this may also be an incidental result.
Previous studies on postmenopausal women found serum E2 concentrations after very low dosages of E2 administrated vaginally, which were stable at eight and sixteen weeks.19 We found that these concentrations remained stable at 14 and 21 days, which may have considerable implications for embryo transfer. The vagina is an ideal site for drug delivery because of anatomic, histologic, and physiologic reasons,20 which may help achieve high physiological levels of serum E2. We measured SHBG, a glycoprotein produced in the liver, which can bind to and transport sex hormones and directly regulate the bioavailable fraction of steroid hormones and their access to target cells, thus preventing some of the clinical effects.21,22 No significant differences in SHBG concentrations between groups were observed, suggesting that potential adverse hepatic effects resulting from high serum E2 concentrations are negligible; however, vaginal E2 and DG administration improves endometrial proliferative and secretory transformation which not only affects endometrial thickness but also its microenvironment. Our study revealed that pinopodes were sufficiently developed on P7 after vaginal treatment. Occurrence of pinopodes confirmed the efficacy of vaginal DG, which previously has never been observed. A study claims that patients with on-time pinopodes development showed higher pregnancy rates.23 During the long 21-day treatment with E2 and DG, pinopodes were absent in nine out of twenty patients, thus in these patients, pinopodes formation was potentially delayed or did not occur at all. Previous studies found that fully developed pinopodes were detected early on day P6 or late on day P10;17 therefore, possible explanations for this phenomenon are that 10 mg DG is insufficient or that the timing of endometrial biopsies was not suitable. Further research would be required to elucidate these aspects.
To examine the effects of the two treatments on the endometrium, we used IHC to assess ER and PR expression, which participate in synchronized interactions between the endometrium and the embryo; these processes are also affected by steroid hormones. We found that ER and PR expression was higher on day 14 and was decreased on day 21, corresponding to the mid-secretory phase during a normal menstrual cycle. ER staining was stronger in the vaginal treatment group, both on day 14 and day 21. A previous study found that ER was positively correlated with the plasma concentration of E2 during the proliferative phase which may explain the observed result.24 Furthermore, PR immunostaining was stronger in oral treatment group, which was, however, not significant. This may be due to an insufficient DG dosage.
FET is an effective means of achieving pregnancy in patients undergoing IVF. Administering vaginal E2 pill treatments can promote endometrial thickening and thus help achieve acceptable pregnancy rates.3 This may be even more important for patients with a thin endometrium as vaginal E2 supplementation seems to be more effective than oral supplementation.25 However, a subsequent follow-up showed that patients of the vaginal treatment group may bleed more than those of the oral treatment group which should be because of the thicker endometrium. One POF patient of this study would bleed after administration of 1 mg E2 vaginally but not after receiving 2 mg E2 orally.
Insufficient progesterone intake could lead to deficient endometrial transformation. Further studies are required to examine the effects of vaginal administration of higher dosages such as 2–4 mg E2 and 20–40 mg DG which are frequently prescribed to FET patients with a thin endometrium or recurrent implantation failure. Since the embryo transfer was not performed at the end of this hormonal treatment cycle, these findings can be partly referred in FET and randomized controlled trails are required.
This study assessed the proliferative and secretory transformation of endometrium via the vaginal and oral route of estradiol and DG in patients with premature ovarian failure by not only serum hormone measurements and ultrasound examination of the uterus but also the histological changes including the conventional histology, IHC of ER and PR, and pinopodes development.
Conclusion
After E2 and DG endometrial priming in POF patients, exogenous vaginal hormonal supplementation is more effective than oral steroid therapy, as was evident from stronger effects on endometrial transformation. Vaginal administration of low-dose E2 and DG increased endometrial thickness and uterine volume and exerted high bioactivity, as histology revealed the improved proliferative and secretory transformation of the endometrium.
Funding Statement
This work was supported by the Science Research Foundation Project of Qilu Hospital of Shandong University (2015QLMS40), Jinan Science and Technology Plan Project (201805024) and Medical Health Science and Technology Development Program of Shandong Province (2016WS0137).
Data Sharing Statement
We would like to share all individual de-identified participant data related to this study in a spreadsheet format. The data will be accessible upon request to the corresponding author and will be available for at least 5 years after publication.
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Le QV, Abhari S, Abuzeid OM, et al. Modified natural cycle for embryo transfer using frozen-thawed blastocysts: a satisfactory option. Eur J Obstet Gynecol Reprod Biol. 2017;213:58–63. doi: 10.1016/j.ejogrb.2017.04.010 [DOI] [PubMed] [Google Scholar]
- 2.Tourgeman DE, Slater CC, Stanczyk FZ, Paulson RJ. Endocrine and clinical effects of micronized estradiol administered vaginally or orally. Fertil Steril. 2001;75(1):200–202. doi: 10.1016/S0015-0282(00)01640-X [DOI] [PubMed] [Google Scholar]
- 3.Liao X, Li Z, Dong X, Zhang H. Comparison between oral and vaginal estrogen usage in inadequate endometrial patients for frozen-thawed blastocysts transfer. Int J Clin Exp Pathol. 2014;7(10):6992–6997. [PMC free article] [PubMed] [Google Scholar]
- 4.Gilman AG. Goodman and Gilman’s the Pharmacological Basis of Therapeutics. 1990. [Google Scholar]
- 5.Benziger DP, Edelson J. Absorption from the vagina. Drug Metab Rev. 1983;14(2):137–168. doi: 10.3109/03602538308991387 [DOI] [PubMed] [Google Scholar]
- 6.Tourgeman DE, Gentzchein E, Stanczyk FZ, Paulson RJ. Serum and tissue hormone levels of vaginally and orally administered estradiol. Am J Obstet Gynecol. 1999;180(6):1480–1483. doi: 10.1016/S0002-9378(99)70042-6 [DOI] [PubMed] [Google Scholar]
- 7.Bennink HJ, Boerrigter PJ. Use of dydrogesterone as a progestogen for oral contraception. Steroids. 2003;68(10–13):927–929. doi: 10.1016/j.steroids.2003.07.006 [DOI] [PubMed] [Google Scholar]
- 8.Mitwally MF, Diamond MP, Abuzeid M. Vaginal micronized progesterone versus intramuscular progesterone for luteal support in women undergoing in vitro fertilization–embryo transfer. Fertil Steril. 2010;93(2):554–569. doi: 10.1016/j.fertnstert.2009.02.047 [DOI] [PubMed] [Google Scholar]
- 9.Tavaniotou A, Smitz J, Bourgain C, Devroey P. Comparison between different routes of progesterone administration as luteal phase support in infertility treatments. Hum Reprod Update. 2000;6(2):139–148. doi: 10.1093/humupd/6.2.139 [DOI] [PubMed] [Google Scholar]
- 10.Fatemi HM, Bourgain C, Donoso P, et al. Effect of oral administration of dydrogestrone versus vaginal administration of natural micronized progesterone on the secretory transformation of endometrium and luteal endocrine profile in patients with premature ovarian failure: a proof of concept. Human Reprod. 2007;22(5):1260–1263. doi: 10.1093/humrep/del520 [DOI] [PubMed] [Google Scholar]
- 11.Ziegler DD, Fanchin R. Progesterone and progestins: applications in gynecology. Steroids. 2000;65(10):671–679. doi: 10.1016/S0039-128X(00)00123-9 [DOI] [PubMed] [Google Scholar]
- 12.Goldenberg RL, Grodin JM, Rodbard D, Ross GT. Gonadotropins in women with amenorrhea. Am J Obstet Gynecol. 1973;116(7):1003–1012. doi: 10.1016/S0002-9378(16)33850-9 [DOI] [PubMed] [Google Scholar]
- 13.Rebar RW, Erickson GF, Yen SSC. Idiopathic premature ovarian failure: clinical and endocrine characteristics. Fertil Steril. 1982;37(1):35–41. doi: 10.1016/S0015-0282(16)45973-X [DOI] [PubMed] [Google Scholar]
- 14.Chien LW, Au H-K, Chen PL, Xiao J, Tzeng CR. Assessment of uterine receptivity by the endometrial-subendometrial blood flow distribution pattern in women undergoing in vitro fertilization-embryo transfer. Fertil Steril. 2002;78(2):245–251. doi: 10.1016/S0015-0282(02)03223-5 [DOI] [PubMed] [Google Scholar]
- 15.Mohamed Amer MI, Omar OH, El Sherbiny Hamed M, Dahroug EG. Subendometrial blood flow changes by 3-dimensional power Doppler ultrasound after hysteroscopic lysis of severe intrauterine adhesions: preliminary study. J Minim Invasive Gynecol. 2015;22(3):495–500. doi: 10.1016/j.jmig.2014.12.165 [DOI] [PubMed] [Google Scholar]
- 16.Yu X, Gao C, Dai C, Yang F, Deng X. Endometrial injury increases expression of hypoxia-inducible factor and angiogenesis in the endometrium of women with recurrent implantation failure. Reprod Biomed Online. 2019;38(5):761–767. doi: 10.1016/j.rbmo.2018.12.027 [DOI] [PubMed] [Google Scholar]
- 17.Nikas G, Drakakis P, Loutradis D, et al. Uterine pinopodes as markers of the ‘nidation window’ in cycling women receiving exogenous oestradiol and progesterone. Human Reprod. 1995;10(5):1208–1213. doi: 10.1093/oxfordjournals.humrep.a136120 [DOI] [PubMed] [Google Scholar]
- 18.Sheshpari S, Shahnazi M, Mobarak H, et al. Ovarian function and reproductive outcome after ovarian tissue transplantation: a systematic review. J Transl Med. 2019;17(1):396–410. doi: 10.1186/s12967-019-02149-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Illston JD, Wheeler TL, Parker CR, Conner MG, Burgio KL, Goode PS, Richter HE. Low-dose 17-β-estradiol cream for vaginal atrophy in a cohort without prolapse: serum levels and vaginal response including tissue biomarkers associated with tissue remodeling. Maturitas. 2015;81(4):475–479. doi: 10.1016/j.maturitas.2015.05.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Alexander NJ, Baker E, Kaptein M, Karck U, Miller L, Zampaglione E. Why consider vaginal drug administration? Fertil Steril. 2004;82(1):1–12. doi: 10.1016/j.fertnstert.2004.01.025 [DOI] [PubMed] [Google Scholar]
- 21.Hammond GL. Potential functions of plasma steroid-binding proteins. Trends Endocrinol Metab. 1995;6(9–10):298–304. doi: 10.1016/1043-2760(95)00162-X [DOI] [PubMed] [Google Scholar]
- 22.Westphal U. Steroid-Protein Interactions II. Vol. 27. Springer: Berlin, Heidelberg; 1986. [Google Scholar]
- 23.Sudoma I, Goncharova Y, Zukin V. Optimization of cryocycles by using pinopode detection in patients with multiple implantation failure: preliminary report. Reprod Biomed Online. 2011;22(6):590–596. doi: 10.1016/j.rbmo.2011.02.004 [DOI] [PubMed] [Google Scholar]
- 24.Kanki S. Cyclic changes in steroid hormone concentration and steroid hormone receptor in the human endometrium. Nihon Sanka Fujinka Gakkai Zasshi. 1982;34(12):2177–2184. [PubMed] [Google Scholar]
- 25.Liu SM, Zhou YZ, Wang HB, et al. Factors associated with effectiveness of treatment and reproductive outcomes in patients with thin endometrium undergoing estrogen treatment. Chin Med J. 2015;128(23):3173–3177. doi: 10.4103/0366-6999.170258 [DOI] [PMC free article] [PubMed] [Google Scholar]