Abstract
Background:
In the treatment of anterior cruciate ligament (ACL) injuries, there is little evidence of when and why a decision for ACL reconstruction (ACLR) or nonoperative treatment (non-ACLR) is made.
Purpose:
To (1) describe the key characteristics of ACL injury treatment decisions and (2) compare patient-reported knee instability, function, and preinjury activity level between patients with non-ACLR and ACLR treatment decisions.
Study Design:
Cohort study; Level of evidence, 2.
Methods:
A total of 216 patients with acute ACL injury were evaluated during the first year after injury. The treatment decision was non-ACLR in 73 patients and ACLR in 143. Reasons guiding treatment decision were obtained from medical charts and questionnaires to patients and orthopaedic surgeons. Patient-reported instability and function were obtained via questionnaires and compared between patients with non-ACLR and ACLR treatment decisions. The ACLR treatment group was classified retrospectively by decision phase: acute phase (decision made between injury day and 31 days after injury), subacute phase (decision made between 32 days and up to 5 months after injury), and late phase (decision made 5-12 months after injury). Data were evaluated using descriptive statistics, and group comparisons were made using parametric or nonparametric tests as appropriate.
Results:
The main reasons for a non-ACLR treatment decision were no knee instability and no problems with knee function. The main reasons for an ACLR treatment decision were high activity demands and knee instability. Patients in the non-ACLR group were significantly older (P = .031) and had a lower preinjury activity level than did those in the acute-phase (P < .01) and subacute-phase (P = .006) ACLR decision groups. There were no differences in patient-reported instability and function between treatment decision groups at baseline, 4 weeks after injury, or 3 months after injury.
Conclusion:
Activity demands, not patient-reported knee instability, may be the most important factor in the decision-making process for treatment after ACL injury. We suggest a decision-making algorithm for patients with ACL injuries and no high activity demands; waiting for >3 months can help distinguish those who need surgical intervention from those who can undergo nonoperative management.
Registration:
NCT02931084 (ClinicalTrials.gov identifier).
Keywords: ACL injury, ACL reconstruction, treatment decision
Anterior cruciate ligament (ACL) injuries can be treated nonoperatively or operatively. In both treatments, rehabilitation is considered important. ACL injury treatment guidelines have recommended that surgery be considered when a patient experiences knee instability and/or has high activity demands.4,25,26,29 When activity demands are low or moderate, the first-line treatment should be a period of rehabilitation aimed at maximizing knee function.4,25,26
Rehabilitation aims to improve knee function, which is beneficial for surgical outcome if an ACL reconstruction (ACLR) is performed later.2,32 An initial period of rehabilitation also allows time for the patient to evaluate whether the knee is unstable in activities of daily living and physical activity, which might not be obvious in the acute phase after injury.17,27 An early ACLR might be beneficial in cases where associated injuries are present (ie, a severe meniscal injury that requires immediate surgery)16 and for active patients who want to return to high knee-demand activities.17
Some studies have suggested that early ACLR might prevent additional meniscal and cartilage injuries that could occur with giving-way episodes.6,14 However, the evidence base is weak, and the implications of ACLR are unclear for patients without subjective instability.7 An ACLR may not be necessary for patients who experience a stable knee and sufficient knee function in chosen activities.15,28
Patients with an ACL injury should be involved in decision making for injury management.16,28 When patients actively participate in health care decision making, outcomes can improve.19,33 A study reported that orthopaedic surgeons and physical therapists unanimously believe that patients’ wishes are important and that giving-way symptoms, high activity level, and young age are factors that guide recommendations for ACLR.16 However, it is unknown how these factors influence treatment decisions or if the treatment decision corresponds to patients’ perceived knee symptoms and function. This information may facilitate effective shared decision making between the clinician and the patient and guide evidence-based treatment decisions.
The aim of the present study was 2-fold: first, to describe the key characteristics of treatment decision making for an ACL injury—nonoperative (non-ACLR) versus operative intervention (ACLR)—including when the decision was made and why; second, to compare patient-reported knee instability, knee function, and preinjury activity levels between the treatment groups after injury (at baseline, 4 weeks, and 3 months). The hypothesis was that patients who made an ACLR treatment decision later would report worse function and more knee instability at 3 months after injury than would patients with a non-ACLR treatment decision.
Methods
This study is part of a prospective cohort study (NAtural COrollolary and recovery after acute anterior cruciate [X] ligament injury [NACOX study]) designed to describe the natural corollary and recovery after acute ACL injury.22 Ethical approval was granted, and the study was registered on ClinicalTrials.gov (NCT02931084). All patients provided informed consent to participate.
Participants
Between June 2016 and October 2018, patients were recruited from 6 orthopaedic clinics in cities of various size in Sweden (urban and suburban environments). Inclusion criteria for the NACOX study were as follows: ACL injury verified using magnetic resonance imaging (MRI) and sustained no more than 6 weeks before inclusion and age between 15 and 40 years at the time of the ACL injury. Patients were excluded if they had previous ACL surgery to the same knee, had fractures that required separate treatment, were unable to understand written and spoken Swedish language, or had cognitive impairments or other illnesses or injuries that impaired function (eg, fibromyalgia, rheumatic diseases, and other diagnoses associated with chronic pain). Participants completed electronically administered questionnaires.22
For the analyses in this article, patients were included if they had made (1) a decision for non-ACLR treatment that persisted at 12 months after the ACL injury or (2) a decision for ACLR within 12 months after injury. Participation in this study did not alter the usual course of treatment and treatment decision, which means that patients may have had initial rehabilitation and then a follow-up with the orthopaedic surgeon to decide on operative or nonoperative treatment. Patients aiming to return to cutting or pivoting sports may have had to make an earlier decision.1 To facilitate our analyses in this article, patients who had made an ACLR treatment decision were classified retrospectively into 3 groups based on time from injury to decision:
Acute phase: when the decision was made between injury day and 31 days after injury
Subacute phase: when the decision was made between 32 days and up to 5 months after injury
Late phase: when the decision was made from 5 to 12 months after injury
The decision-making intervals, used for analysis only, were based on recommendations for patients who did not aim to return to cutting or pivoting sports but should complete adequate rehabilitation before making a decision about treatment.1 A decision made in the acute phase was unlikely to have been preceded by a rehabilitation phase and follow-up evaluation, while a decision made in the subacute phase could have been preceded by sufficient rehabilitation.
Sources for Information About Treatment Chosen, Reasons, and Timing
Information about the chosen treatment and the reasons and timing for the treatment decision was derived from 3 sources: medical charts, questionnaires to orthopaedic surgeons, and questionnaires to patients.
Medical Chart Review
All medical charts were reviewed by the first author (H.T.G., physical therapist experienced in knee rehabilitation). Data were extracted for (1) the treatment decision that was made, (2) the main reasons why it was made, and (3) when it was made.
Questionnaire Responses From Orthopaedic Surgeons
When a patient had an appointment with the orthopaedic surgeon and a treatment decision was made, the orthopaedic surgeon answered a question about which treatment was delivered and described the reason for the decision in free text. Questionnaires were administered in print at the time of the appointment or were electronically sent to the orthopaedic surgeon by email, as preferred by the clinic or the surgeon.
Questionnaire Responses From Patients
Patient-reported data about treatment and reasons for the decision were collected via electronically administered questionnaires. When a non-ACLR treatment decision was made, patients continued to receive electronic questionnaires with questions about treatment at 3, 6, and 12 months after injury to ensure that the decision had not changed (ie, from non-ACLR treatment to ACLR). Treatment decisions that had not changed 12 months after injury were analyzed.
Categorizing Reasons for Treatment Decision
Information from the medical chart and orthopaedic surgeon and patient questionnaires was used to identify the most prominent reason for making the treatment decision. The reasons for each patient were categorized according to clinical practice guidelines.25,26,29
Categories for non-ACLR treatment included
Absence of patient-perceived knee instability/giving way
Low activity demands
Sufficient knee function
Other reasons
Categories for ACLR treatment included
Patient-perceived knee instability/giving way
High activity demands
Patient-perceived knee instability/giving way and high activity demands
Other reasons
Timing of Final Treatment Decision
The decision date was when the patient had an appointment with an orthopaedic surgeon and a decision for treatment was made. In cases where patients reported that a decision for non-ACLR treatment was made and no orthopaedic surgeon appointment had occurred, the date when the patient first indicated that the treatment decision was non-ACLR was used. If the patient (1) had not replied to the questionnaire and (2) there was no other information about the decision, the medical chart was reviewed for information about treatment. In cases where information from the medical chart indicated that the patient had not had ACLR treatment, the date 12 months after injury was used in the analysis.
Patient-Reported Data
Patient-reported outcome data were collected at baseline (the time that patients were included in the study) and then 4 weeks and 3 months after injury. The following measures were used.
The Tegner Activity Scale24 was used to collect information about preinjury activity, activity level, and working situation, according to the definitions by Fältström et al.10 The score is from 0 to 10, where 0 equals “sick-leave or disability due to knee problems” and 10 equals “competitive sports at national or international level; soccer, football, rugby.”
Two questions assessed knee instability: “How stable is your knee in everyday situations?” asked at baseline and 4 weeks and 3 months after injury and “How stable is your knee when you do rehabilitation training, recreational activities or sports activities?” asked at 3 months after injury. Both questions had a rating scale of 1 to 10, where 1 was “totally unstable” and 10 was “totally stable.” These explicit questions about instability are not found in other knee-related questionnaires and were therefore added to complement the patient-reported knee function data collected via the International Knee Documentation Committee Subjective Knee Form (IKDC-SKF). Patients answered the IKDC-SKF at 4 weeks and 3 months after injury. The IKDC-SKF is an 18-item knee-specific questionnaire, covering symptoms, function, and activity level.20
For patients who had ACLR during the follow-up period, data were analyzed from the 4-week and 3-month follow-ups if the patient had not yet had ACLR.
Statistical Analysis
All statistical analyses were performed using SPSS Statistics for Windows (Version 25.0; IBM Corp). Data were compared between patients with a decision to have non-ACLR treatment and to have ACLR at acute, subacute, and late phases. Comparisons were made for the following independent variables: age; sex; preinjury Tegner score; instability in everyday living (at baseline, 4 weeks, 3 months); instability in rehabilitation training, recreational activities, or sports activities (at 3 months); and IKDC-SKF (at 4 weeks, 3 months). A chi-square test was used for sex comparisons between groups. Kruskal-Wallis and Mann-Whitney U tests were used for the ordinal variables Tegner score and instability ratings. Independent-samples t tests and 1-way analyses of variance with a post hoc Tukey test were used for the continuous variables of age and IKDC-SKF scores. A P value <.05 was considered significant. The data had a normal distribution as assessed via interpretation of plot statistics, interpretation of mean and SD, and the Kolmogorov-Smirnov test.
Results
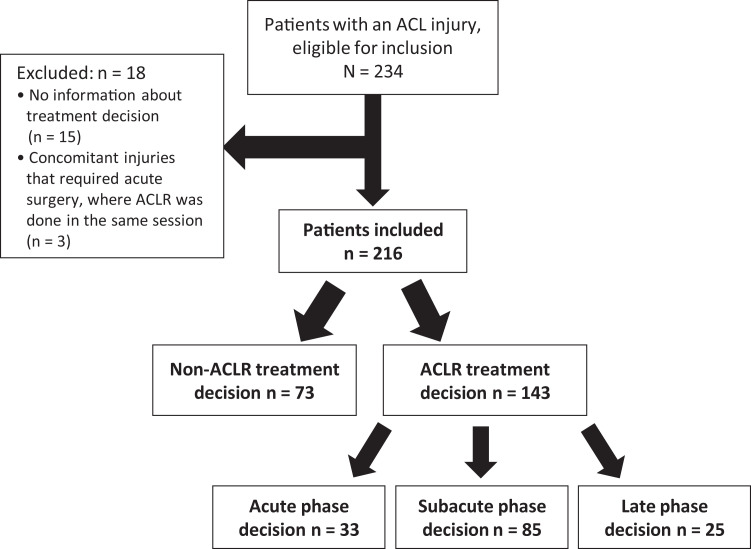
There were 234 patients eligible for inclusion for this study. Eighteen patients were excluded owing to inadequate information (n = 15) or concomitant injuries that led to acute surgery (n = 3). This left 216 patients with a mean ± SD age of 25 ± 7.2 years (Figure 1, Table 1). Preinjury Tegner score, instability ratings, and IKDC-SKF scores are reported in Table 2.
Figure 1.
Flowchart of patient inclusion, proportion, and timing of treatment chosen. ACL, anterior cruciate ligament; ACLR, anterior cruciate ligament reconstruction.
Table 1.
Demographic Data and Time From Injury to Decision and ACLR by Groupa
| ACLR by Decision Phase | ||||||
|---|---|---|---|---|---|---|
| Overall (N = 216) | Non-ACLR (n = 73) | All (n = 143) | Acute (n = 33) | Subacute (n = 85) | Late (n = 25) | |
| Age at injury, y | 25 ± 7.2 | 28 ± 7b | 25 ± 7.2 | 24 ± 7b | 23 ± 6b | 25 ± 8 |
| Male:female (male) | 101:118 (46) | 39:34 (54) | 59:84 (41) | 11:22 (33) | 36:49 (42) | 12:13 (48) |
| Injury to, d | ||||||
| Decision | 118 ± 91 | 162 ± 99 | 94 ± 76 | 19 ± 10 | 84 ± 39 | 226 ± 54 |
| ACLR | 154 ± 91 | 79 ± 51 | 144 ± 65 | 290 ± 63 | ||
aValues are presented as mean ± SD or No. (%). ACLR, anterior cruciate ligament reconstruction.
bPatients in the non-ACLR treatment group were significantly older than were patients in the acute-phase (P = .031) and subacute-phase (P < .001) ACLR decision groups.
Table 2.
Patient-Reported Preinjury Activity Participation and Knee Instability and Functiona
| ACLR by Decision Phase | ||||||
|---|---|---|---|---|---|---|
| Overall (N = 216) |
Non-ACLR (n = 73) |
All (n = 143) | Acute (n = 33)b | Subacute (n = 85) | Late (n = 25) | |
| Preinjury TAS | 8 (5) | 7 (6)c | 8 (5) | 8 (5)c | 8 (4)c | 6 (7) |
| Instabilityd in ADL | ||||||
| Baseline | 5 (3) | 5 (3) | 4 (3) | 4 (1) | 5 (3) | 5 (4) |
| 4 wk | 6 (3) | 5 (3) | 6 (3) | 4 (2) | 6 (2) | 5 (4) |
| 3 mo | 7 (2) | 7 (2) | 7 (2) | — | 7 (2) | 7 (4) |
| Instabilityd in rehabilitation, recreation, and activity at 3 mo | 6 (3) | 6 (2) | 6 (3) | — | 6 (2) | 5 (4) |
| IKDC-SKF | ||||||
| 4 wk | 45.0 ± 11.5 (201) | 44.8 ± 12.3 (70) | 45.2 ± 11.1 (129) | 46.4 ± 10.2 (27) | 45.5 ± 11.4 (77) | 43.1 ± 11.2 (25) |
| 3 mo | 53.8 ± 12.8 (159) | 56.5 ± 12.7 (66) | 52.8 ± 12.6 (90) | — | 52.4 ± 11.2 (60) | 53.2 ± 14.4 (21) |
aValues are presented as median (interquartile range) or mean ± SD (No.). ACLR, anterior cruciate ligament reconstruction; ADL, activities of daily living; IKDC-SKF, International Knee Documentation Committee Subjective Knee Form; TAS, Tegner activity score. Dashes refer to no data collected, since the acute group had undergone their ACLR at that time.
bPatients in the acute-phase decision group did not respond to questions about instability and IKDC-SKF at 3 months after injury.
cThe non-ACLR decision group had a significantly lower preinjury TAS than did the acute-phase (P < .01) and subacute-phase (P < .02) ACLR decision groups.
dKnee instability scored from 1 (totally unstable) to 10 (totally stable).
Reasons for Treatment Decision
To check the validity of the data, we compared the reasons for the treatment decision among the medical charts (reports for 196 treatment decisions), orthopaedic surgeons’ responses to questionnaires (144 responses), and patients’ responses to questionnaires (150 responses). Each patient had decisions from at least 2 of the 3 possible sources. There were no conflicts.
Non-ACLR Treatment
The main reason for deciding for non-ACLR treatment was “no instability/no giving way” (45%) (Table 3). For 20 (27%) patients, the decision for non-ACLR treatment was based on “other reasons”:
The patient had not completed sufficient rehabilitation to evaluate surgical indications (n = 4).
The patient did not want to have ACLR (n = 4).
The patient had not attended a follow-up appointment to assess indications for ACLR (n = 5).
The medical chart stated that the patient could return for a follow-up appointment if he or she wanted to have ACLR (n = 2).
Follow-up MRI, arthroscopy, or clinical assessment showed no indication for ACLR (n = 3).
Medical reasons (surgery was contraindicated for medical reasons; n = 2)
Table 3.
Free Text Responses From Patients and Orthopaedic Surgeons for Why the Treatment Decision Was Madea
| ACLR Decision Phase | ||||
|---|---|---|---|---|
| Non-ACLR Treatment (n = 73) | Acute (n = 33) | Subacute (n = 85) | Late (n = 25) | |
| No knee instability | 33 (45) | |||
| Knee instability/giving way | 1 (3) | 22 (26) | 13 (52) | |
| Activity demands | ||||
| Low | 4 (5) | |||
| High | 21 (64) | 25 (29) | 4 (16) | |
| Sufficient knee function | 16 (22) | |||
| Knee instability/giving way and high activity demands | 11 (33) | 36 (42) | 5 (20) | |
| Other reason | ||||
| Non-ACLR treatment | 20 (27) | |||
| ACLR | 2 (2) | 3 (12) | ||
aThe responses were categorized and are reported based on clinical treatment guidelines. Data are reported as No. (%). ACLR, anterior cruciate ligament reconstruction
For 9 patients, a decision to undergo non-ACLR treatment was changed a decision to undergo ACLR. Of the 9 patients, 5 did not want to undergo ACLR initially, but the decision was changed because of repeated giving way or perceived instability. Three patients wanted to undergo ACLR initially; however, the orthopaedic surgeon advised against it, and the decision changed when the patient sought an opinion from another orthopaedic surgeon. One patient decided for non-ACLR treatment owing to sufficient knee function but subsequently sustained a meniscal injury and decided to have ACLR at the time the menisci were repaired.
ACLR Treatment
When a decision to undergo ACLR was made in the acute phase, “high activity demands” (64%) was the main reason. In the subacute phase, “instability/giving way and high activity demands” (55%) was the main reason for the decision to undergo ACLR. In the late phase, “instability/giving way” (52%) was the main reason for deciding to have ACLR (Table 3).
For 5 patients who underwent ACLR, the treatment decision was based on the patient’s desire for an ACLR. Why the patient asked for ACLR was not reported.
For 5 patients, the initial treatment decision was ACLR, which changed to non-ACLR treatment: 2 patients reported that the decision changed because they could participate in their sports (handball, floorball) without knee instability, and 3 patients were assessed via follow-up arthroscopy (n = 2) or MRI (n = 1), which revealed that ACLR was no longer indicated.
Group Comparisons
Patients in the non-ACLR decision group were older and had a lower preinjury activity level than did patients in the acute-phase ACLR decision group (P = .031 and P = .01 and the subacute phase (P < .001 and P < .02, respectively) (Tables 1 and 2). There were no differences in age or preinjury activity level between the non-ACLR group and the late-phase ACLR decision group. There were no differences in patient-reported knee instability or IKDC-SKF at baseline, 4 weeks, or 3 months after injury.
Discussion
During the first year after ACL injury, we identified that absence of knee instability was the most prominent reason for deciding to undergo non-ACLR treatment, as stated in 45% of the cases. However, patient-reported instability during the first 3 months after injury was similar between the patients in the non-ACLR group (median, 7) and those in the ACLR groups (median, 7) who had not had the surgery yet. Therefore, for the patients with a subacute- or late-phase decision, there may have been a discrepancy between the reasons stated for the treatment decision and how patients rated their condition early after an ACL injury. In the clinic, this may suggest that within the first 3 months after injury, the decision to undergo ACLR is, to a large extent, based on patient-reported instability, as guidelines and recommendations have stated.4,23,24
The majority of patients (66%) had an ACLR treatment, and most decisions to undergo ACLR (59%) were made in the subacute phase. The main reason for an ACLR treatment decision differed depending on when the decision was made. For patients where a decision for ACLR was made in the acute phase, the reason was mainly based on the patient’s desire to return to highly demanding activity, which supports previous research.17 For patients who decided to undergo ACLR treatment in the late phase, the decision was more influenced by perceived knee instability. When the decision to undergo ACLR was made early, it seems that it was based on concerns about future function. In contrast, later decisions for ACLR seemed to be guided by current knee function, which supports previous research.30
Patients in the non-ACLR group reported a greater diversity of reasons for choice of treatment than did patients in the ACLR group. Nearly one-third of the patients with a non-ACLR treatment decision reported other factors that influenced the treatment decision. Some patients did not attend their appointment with the orthopaedic surgeon. It is possible that patients and their physical therapists may have reached a shared decision regarding non-ACLR treatment and patients may not have felt the need to consult with an orthopaedic surgeon before reaching that decision.27
The present results reflect treatment guideline recommendations for ACLR in the presence of high activity demands and/or knee instability.25,26 Decisions for ACLR in the acute phase were principally based on high activity demands; decisions for ACLR in the late phase were principally based on knee instability. The present study showed that of 73 patients who made an initial decision to undergo non-ACLR treatment, only 9 changed to a decision to have ACLR within the first year after injury. Among them, 5 experienced knee instability despite adequate rehabilitation, and 1 sustained a meniscal injury, which indicates that the chosen treatment was successful during the first year after injury for the majority of the patients. However, the present study did not report new injuries >12 month after injury, which is a limitation.
In this study, we described the characteristics for treatment decisions made in clinical practice. Participation in this prospective study did not influence the treatment decision, and we believe that the decision was based on clinical reasoning and patient involvement. A potential bias could be the orthopaedic surgeons’ influence on the treatment decision. A recommendation from health care personnel for or against a specific treatment decision could have affected the patient’s wishes and expectations. When the patient is provided with adequate and nuanced information about the condition and possible treatments, the shared decision-making process is enhanced.8 However, meetings in the orthopaedic clinic do not always follow a shared decision-making model, with lack of time as a great barrier.5
We found that older patients with lower activity level had a non-ACLR treatment decision. Patients with non-ACLR treatment can achieve a sufficient activity level and be satisfied with their knee function.15,18 Younger patients with high activity demands had early ACLR treatment decisions. After ACLR, approximately 90% achieve normal or near normal knee function3; however, knee function may not be fully restored, and functional limitations and deteriorated knee-related quality of life are still present 5 years after ACLR.23 Returning to demanding activity entails a risk for new injuries and knee-related problems irrespective of the treatment chosen.9,13 Studies with long-term follow-up have also suggested that knee-related quality of life and risk for symptomatic knee osteoarthritis do not differ between ACLR and non-ACLR treatment.11,12,21,31 This emphasizes the importance of making the right decision for the right patient to minimize the risk of subsequent injuries and to avoid unnecessary surgery. Treatment decisions after ACL injury seem to be made with consideration of existing guidelines,4,26,29 and follow-ups with patients from the present study will show if the decisions were appropriate regarding satisfaction with knee function, activity level, and risk for new injuries for each patient.
Limitations
This study had limitations. Patient-reported outcomes were collected at predefined time points (baseline, 4 weeks, and 3 months after injury) and not measured at the same time as the treatment decision was made. Therefore, patient-reported data did not in every case reflect patient-perceived knee instability and function at the time when the treatment decision was made. However, for the ACLR and non-ACLR decision groups, the repeated rating of instability and IKDC-SKF scores (reported before the ACLR procedure) improved over time, suggesting that both groups experienced similar instability and function and positive progress for the first 3 months after ACL injury. The term instability can be interpreted by the patient in different ways, ranging from knee buckling to true giving way. In the present study, patient-perceived instability or lack of instability was reported as the reason for either treatment decision.
Some patients did not attend the orthopaedic clinic for follow-up, which might suggest a non-ACLR treatment decision as “default.” Without consistent follow-up of patients with non-ACLR treatment, it is difficult to know if the choice of non-ACLR treatment was an active choice or simply a result of not consulting the orthopaedic surgeon.
Crossover from non-ACLR treatment to ACLR can occur >12 months after injury.15,18 Therefore, it is possible that the final treatment for all patients in the non-ACLR treatment group might not have been captured. A follow-up at 24 to 36 months with patient-reported outcomes is planned.
Conclusion
Activity demands, not patient-reported knee instability, may be the most important factor in the decision making for treatment after ACL injury. There were no differences in patient-reported knee instability and function at baseline, at 4 weeks after injury, and at 3 months after injury. We suggest a decision algorithm for patients with ACL injuries and no high activity demands; waiting for >3 months can help distinguish those who need surgical intervention from those who can be treated nonoperatively.
Acknowledgment
The authors thank all participating patients, orthopaedic surgeons, and clinics of the NACOX cohort study.
Footnotes
Final revision submitted February 2, 2021; accepted February 17, 2021.
One or more of the authors has declared the following potential conflict of interest or source of funding: This study is a part of the NACOX cohort, which is supported by the Swedish Medical Research Council, the Swedish Research Council for Sport Science, the Medical Research Council of Southeast Sweden, and ALF Grants Region Östergötland. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval for this study was obtained from the ethical review authority of Linköping (2016/44/31, 2018/123-32).
References
- 1. Ahldén M, Kvist J, Samuelsson K, Eriksson KO, Karlsson J. Individualiserad terapi viktigt vid främre korsbandsskada. Läkartidningen. 2014;111:CXWS. [PubMed] [Google Scholar]
- 2. Alshewaier S, Yeowell G, Fatoye F. The effectiveness of pre-operative exercise physiotherapy rehabilitation on the outcomes of treatment following anterior cruciate ligament injury: a systematic review. Clin Rehabil. 2017;31(1):34–44. [DOI] [PubMed] [Google Scholar]
- 3. Ardern CL, Webster KE, Taylor NF, Feller JA. Return to sport following anterior cruciate ligament reconstruction surgery: a systematic review and meta-analysis of the state of play. Br J Sports Med. 2011;45(7):596–606. [DOI] [PubMed] [Google Scholar]
- 4. Beaufils P, Hulet C, Dhenain M, Nizard R, Nourissat G, Pujol N. Clinical practice guidelines for the management of meniscal lesions and isolated lesions of the anterior cruciate ligament of the knee in adults. Orthop Traumatol Surg Res. 2009;95(6):437–442. [DOI] [PubMed] [Google Scholar]
- 5. Braddock C, III, Hudak PL, Feldman JJ, Bereknyei S, Frankel RM, Levinson W. “Surgery is certainly one good option”: quality and time-efficiency of informed decision-making in surgery. J Bone Joint Surg Am. 2008;90(9):1830–1838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Church S, Keating JF. Reconstruction of the anterior cruciate ligament: timing of surgery and the incidence of meniscal tears and degenerative change. J Bone Joint Surg Br. 2005;87(12):1639–1642. [DOI] [PubMed] [Google Scholar]
- 7. Ekås GR, Ardern CL, Grindem H, Engebretsen L. Evidence too weak to guide surgical treatment decisions for anterior cruciate ligament injury: a systematic review of the risk of new meniscal tears after anterior cruciate ligament injury. Br J Sports Med. 2020;54(9):520–527. [DOI] [PubMed] [Google Scholar]
- 8. Epstein RM, Alper BS, Quill TE. Communicating evidence for participatory decision making. JAMA. 2004;291(19):2359–2366. [DOI] [PubMed] [Google Scholar]
- 9. Fältström A, Hägglund M, Kvist J. Functional performance among active female soccer players after unilateral primary anterior cruciate ligament reconstruction compared with knee-healthy controls. Am J Sports Med. 2017;45(2):377–385. [DOI] [PubMed] [Google Scholar]
- 10. Fältström A, Hägglund M, Kvist J. Patient-reported knee function, quality of life, and activity level after bilateral anterior cruciate ligament injuries. Am J Sports Med. 2013;41(12):2805–2813. [DOI] [PubMed] [Google Scholar]
- 11. Filbay SR, Ackerman IN, Russell TG, Macri EM, Crossley KM. Health-related quality of life after anterior cruciate ligament reconstruction: a systematic review. Am J Sports Med. 2014;42(5):1247–1255. [DOI] [PubMed] [Google Scholar]
- 12. Filbay SR, Culvenor AG, Ackerman IN, Russell TG, Crossley KM. Quality of life in anterior cruciate ligament–deficient individuals: a systematic review and meta-analysis. Br J Sports Med. 2015;49(16):1033–1041. [DOI] [PubMed] [Google Scholar]
- 13. Filbay SR, Roos EM, Frobell RB, Roemer F, Ranstam J, Lohmander LS. Delaying ACL reconstruction and treating with exercise therapy alone may alter prognostic factors for 5-year outcome: an exploratory analysis of the KANON trial. Br J Sports Med. 2017;51(22):1622–1629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Foster A, Butcher C, Turner PG. Changes in arthroscopic findings in the anterior cruciate ligament deficient knee prior to reconstructive surgery. Knee. 2005;12(1):33–35. [DOI] [PubMed] [Google Scholar]
- 15. Frobell RB, Roos HP, Roos EM, Roemer FW, Ranstam J, Lohmander LS. Treatment for acute anterior cruciate ligament tear: five year outcome of randomised trial. Br J Sports Med. 2015;49(10):700. [DOI] [PubMed] [Google Scholar]
- 16. Grevnerts HT, Fältstrom A, Sonesson S, Gauffin H, Carlfjord S, Kvist J. Activity demands and instability are the most important factors for recommending to treat ACL injuries with reconstruction. Knee Surg Sports Traumatol Arthrosc. 2018;26(8):2401–2409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Grindem H, Eitzen I, Engebretsen L, Snyder-Mackler L, Risberg MA. Nonsurgical or surgical treatment of ACL injuries: knee function, sports participation, and knee reinjury: the Delaware-Oslo ACL Cohort Study. J Bone Joint Surg Am. 2014;96(15):1233–1241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Grindem H, Wellsandt E, Failla M, Snyder-Mackler L, Risberg MA. Anterior cruciate ligament injury—who succeeds without reconstructive surgery? The Delaware-Oslo ACL Cohort Study. Orthop J Sports Med. 2018;6(5):2325967118774255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Holland WC, Hunold KM, Mangipudi SA, Rittenberg AM, Yosipovitch N, Platts-Mills TF. A prospective evaluation of shared decision-making regarding analgesics selection for older emergency department patients with acute musculoskeletal pain. Acad Emerg Med. 2016;23(3):306–314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Irrgang JJ, Anderson AF, Boland AL, et al. Development and validation of the International Knee Documentation Committee Subjective Knee Form. Am J Sports Med. 2001;29(5):600–613. [DOI] [PubMed] [Google Scholar]
- 21. Kvist J, Filbay S, Andersson C, Ardern CL, Gauffin H. Radiographic and symptomatic knee osteoarthritis 32 to 37 years after acute anterior cruciate ligament rupture. Am J Sports Med. 2020;48(10):2387–2394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Kvist J, Gauffin H, Tigerstrand Grevnerts H, et al. Natural corollaries and recovery after acute ACL injury: the NACOX cohort study protocol. BMJ Open. 2018;8(6):e020543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Kvist J, Kartus J, Karlsson J, Forssblad M. Results from the Swedish national anterior cruciate ligament register. Arthroscopy. 2014;30(7):803–810. [DOI] [PubMed] [Google Scholar]
- 24. Lysholm J, Gillquist J. Evaluation of knee ligament surgery results with special emphasis on use of a scoring scale. Am J Sports Med. 1982;10(3):150–154. [DOI] [PubMed] [Google Scholar]
- 25. Marx RG, Jones EC, Angel M, Wickiewicz TL, Warren RF. Beliefs and attitudes of members of the American Academy of Orthopaedic Surgeons regarding the treatment of anterior cruciate ligament injury. Arthroscopy. 2003;19(7):762–770. [DOI] [PubMed] [Google Scholar]
- 26. Meuffels DE, Poldervaart MT, Diercks RL, et al. Guideline on anterior cruciate ligament injury. Acta Orthop. 2012;83(4):379–386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Österberg A, Kvist J, Dahlgren MA. Ways of experiencing participation and factors affecting the activity level after nonreconstructed anterior cruciate ligament injury: a qualitative study. J Orthop Sports Phys Ther. 2013;43(3):172–183. [DOI] [PubMed] [Google Scholar]
- 28. Sackett DL, Rosenberg WM, Gray JA, Haynes RB, Richardson WS. Evidence based medicine: what it is and what it isn’t. BMJ. 1996;312(7023):71–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Shea KG, Carey JL, Richmond J, et al. The American Academy of Orthopaedic Surgeons evidence-based guideline on management of anterior cruciate ligament injuries. J Bone Joint Surg Am. 2015;97(8):672–674. [DOI] [PubMed] [Google Scholar]
- 30. Swirtun LR, Eriksson K, Renström P. Who chooses anterior cruciate ligament reconstruction and why? A 2-year prospective study. Scand J Med Sci Sports. 2006;16(6):441–446. [DOI] [PubMed] [Google Scholar]
- 31. Tsoukas D, Fotopoulos V, Basdekis G, Makridis KG. No difference in osteoarthritis after surgical and non-surgical treatment of ACL-injured knees after 10 years. Knee Surg Sports Traumatol Arthrosc. 2016;24(9):2953–2959. [DOI] [PubMed] [Google Scholar]
- 32. van Melick N, van Cingel RE, Brooijmans F, et al. Evidence-based clinical practice update: practice guidelines for anterior cruciate ligament rehabilitation based on a systematic review and multidisciplinary consensus. Br J Sports Med. 2016;50(24):1506–1515. [DOI] [PubMed] [Google Scholar]
- 33. Washington K, Shacklady C. Patients’ experience of shared decision making using an online patient decision aid for osteoarthritis of the knee—a service evaluation. Musculoskeletal Care. 2015;13(2):116–126. [DOI] [PubMed] [Google Scholar]