On March 11, 2020, the World Health Organization declared the spread of a novel coronavirus to be a pandemic. Subsequently, and only 272 d afterward, the Pfizer vaccine started to be applied in the United Kingdom. Never before had a vaccine been developed in such a short time. Currently, four COVID-19 vaccines are approved for full use, and another eight are in early or limited use (1). However, the supply of vaccines is still inadequate to meet current needs. In such a scenario, prioritization strategies are required, ideally guided by ethical values (2). In many countries, health care professionals were initially prioritized, followed by different groups (depending on the country) such as individuals with comorbidities associated with a higher risk of COVID-19 mortality, elderly people living in crowded settings, K-12 teachers and school staff, people in homeless shelters, people in prisons, and critical workers in high-risk setting (3). Some countries also include an age criteria for prioritization. This raises questions regarding ages that should be prioritized to save the most lives and to maximize years of life saved. Intuitively, one could imagine that vaccinating the elderly first saves the most lives, because they have a higher risk of dying from COVID-19. However, that would translate into fewer years of life saved because life expectancy at older ages is smaller. However, Goldstein et al. (4) provide mathematical proof that prioritizing those at highest risk of dying from COVID-19 would accomplish both goals.
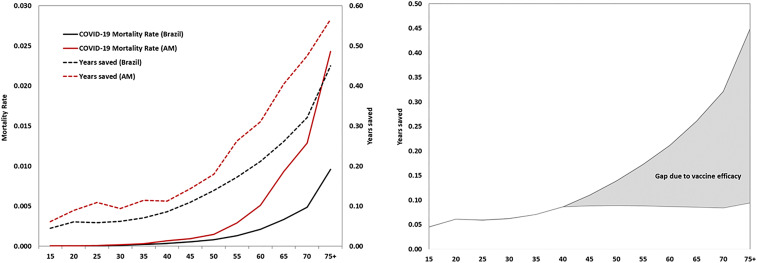
We offer a few reflections. First, the pattern of the age-specific COVID-19 mortality rate is similar to the pattern of overall mortality in a population. There are lower rates at younger ages and increasing rates after midadult ages. Therefore, the sheer volume of lives saved among the elderly, despite lower life expectancy, adds to a large number of years of life saved, in contrast to a very small number of potential lives to be saved at younger ages (given very low mortality). Goldstein et al. (4) show results for the United States, Germany, and South Korea. Here, we use the same approach to obtain estimates for Brazil and for Amazonas state within it (Fig. 1A). This was one of the states most heavily hit by COVID-19 in Brazil (5, 6). Our results corroborate Goldstein et al. (4): Targeting those aged 75 or more would save five times more lives than would be saved by prioritizing those aged 40 to 44 y.
Fig. 1.
Age-specific mortality rates and years saved considering (A) a hypothetical vaccination (protective efficacy of 90%) against COVID-19 in Brazil and in Amazonas state, and (B) an alternative scenario of vaccination against COVID-19 in Brazil with progressive declining efficacy starting at 45 y of age.
Second, the authors assume that vaccine efficacy does not vary by age. A modeling approach that examined vaccine prioritization strategies found that targeting those aged 60 and older would reduce the most deaths and years of life lost, but when vaccine efficacy declined from 59 or 69 y onward, prioritizing all adults or those aged 20 to 49 y would achieve a larger reduction, albeit by a small margin (7). In Fig. 1B, we use the prior example for Brazil but assume an alternative and hypothetical vaccine efficacy that varies by age (starting at age group 45 to 49, efficacy is about 80% of the previous age group). The years saved drops considerably (gray region in Fig. 1B), but prioritizing the elderly would still maximize lives and years of life saved.
Third, external factors may threaten the expected beneficial outcomes of prioritizing the elderly in COVID-19 vaccination campaigns, despite the demographic potential of maximizing lives and years of life saved. One factor is the demographic profile of individuals who refuse to be vaccinated. A recent survey done in the United States found age to be associated with a lower willingness to receive a COVID-19 vaccination (8). Another factor is compliance with prioritization strategies. In Brazil, the Congress recently approved a proposal to impose penalties to those that find ways to get a vaccine disrespecting the prioritization. The proposal now awaits approval from the senate. The extent to which such regulation prevents violations is debatable.
Footnotes
The authors declare no competing interest.
See companion article, “Vaccinating the oldest against COVID-19 saves both the most lives and most years of life,” 10.1073/pnas.2026322118.
References
- 1.Zimmer C., Corum J., Wee S.-L., Coronavirus vaccine tracker. NYTimes. https://www.nytimes.com/interactive/2020/science/coronavirus-vaccine-tracker.html. Accessed 24 February 2021.
- 2.Persad G., Peek M. E., Emanuel E. J., Fairly prioritizing groups for access to COVID-19 vaccines. JAMA 324, 1601–1602 (2020). [DOI] [PubMed] [Google Scholar]
- 3.National Academies of Sciences, Engineering, and Medicine , Framework for Equitable Allocation of COVID-19 Vaccine, Gayle H., Foege W., Brown L., Kahn B., Eds. (The National Academies Press, Washington, DC, 2020). [PubMed] [Google Scholar]
- 4.Goldstein J. R., Cassidy T., Wachter K. W., Vaccinating the oldest against COVID-19 saves both the most lives and most years of life. Proc. Natl. Acad. Sci. U.S.A. 118, e2026322118 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Buss L. F., et al., Three-quarters attack rate of SARS-CoV-2 in the Brazilian Amazon during a largely unmitigated epidemic. Science 371, 288–292 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sabino E. C., et al., Resurgence of COVID-19 in Manaus, Brazil, despite high seroprevalence. Lancet 397, 452–455 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bubar K. M., et al., Model-informed COVID-19 vaccine prioritization strategies by age and serostatus. Science 371, 916–921 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kreps S., et al., Factors associated with US adults’ likelihood of accepting COVID-19 vaccination. JAMA Netw. Open 3, e2025594 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]