Abstract
Background
Cataracts is the major global causes of blindness and a vision-affecting disease of the eye. Cataract surgery is a curative and cost-effective intervention. The number of people who undergo cataract surgery has increased rapidly. Hence, this study was aimed to determine predictors and the time of recovery of cataract patients after cataract surgery by using Simi parametric models of survival analysis.
Methods
A retrospective cohort study was conducted from January/01/2015 and January/30/2019. STATA version14.0 statistical software was used for analysis. The Kaplan-Meier survival method and log-rank test curves were applied. Weibull regression was used and adjusted hazard ratio 95% CI with a value of p less than 0.05 was used to identify a significant association.
Results
Two hundred twenty three cataract patients were recovered from cataract, 72.6% (95% CI 69.8%–75.9%). The overall median survival time was 23 weeks (IQR = 16 to 35) with (95% CI, 21%–25%). aged between 16 and 30year (AHR = 1.20 CI; 1.07–2.36), age 31 to 45 (AHR = 1.24 CI; 1.08–1.54), urban dwellers (AHR = 1.59; 95% CI, 1.18–2.14), medium visual acuity (AHR = 4.14 CI; 2.57–6.67), high visual acuity (AHR = 5.23 CI; 3.06–8.93), Secondary cataract (AHR = 2.59 CI; 1.01–3.02), traumatic cataract (AHR = 1.75 CI; 1.01–3.02), extra capsular cataract extraction surgery (AHR = 1.43 CI; 1.07–1.94),and diabetes mellitus (AHR = 0.75, CI; 0.41–0.96) were notably associated with time to recovery.
Conclusion
Time to recovery in the study area was slightly higher as compared with the global cut of time. Cataract patients with comorbidity of DM had lower recovery time.
Keywords: Cataract, Surgery, Recovery time, Survival, Ethiopia
Highlights
-
•
A 72.6% cataract patients were recovered and 27.4% of were censored from cataract.
-
•
The overall median survival time was 23 weeks and the mean recovery time of the patients was 23.24 weeks.
-
•
A significant difference seen in the recovery rate among cataract patients with/out diabetes mellitus.
-
•
Time to recovery in the study area was slightly higher.
1. Background
In low-income countries, cataract account about half of blindness and has a major impact on physical, psychological, and socio-economic development of country, individuals and societies [1,2]. Visual impairment is more prevalent in low and middle income countries (LMICs) about 80%–90% of world's visually impaired people are reported [3,4]. The global causes of blindness due to eye diseases excluding refractive errors were onchocerciasis (1%), trachoma (4%), congenital (4%), diabetic retinopathy (5%), corneal opacities (5%), age-related Macular degeneration (9%), glaucoma (12%), cataracts (47%), and others (13%) [5]. According to a 2006 National Survey report in Ethiopia, the prevalence of blindness was 1.6% of which, 50% of the blindness was due to cataract [6]. In a survey conducted in Central Ethiopia, we found the prevalence of blindness (<3/60 Snellen acuity) and visual impairment (6/24 to 3/60 Snellen acuity) among those 40 years of age and older to be 7.9% and 12.1%, respectively [7].
Cataracts is the major global causes of blindness and a vision-affecting disease of the eye which resulting from damage to the retina, age-related macular degeneration [8]. Despite this, it is the opacity of the natural human lens, which may be resulted from congenital, developmental and acquired causes. Cataract affects all age groups even though it is highly prevalent in people's age greater 50 years and it is the most preventable condition if timely intervention is applied [9,10].
Numerous studies reported that the factors for delaying from timely treatment are low economic.
Status, lack of transportation, wrong perception, residual vision and poor knowledge [[11], [12], [13]]. However, in recent years, the visual rehabilitation is made through sight-restoring surgery. The number of people who undergo cataract surgery has increased rapidly and it becomes the most frequently performed cost-effective surgical procedure throughout the world [14,15]. The outcome of cataract surgery for an individual or for a defined population is therefore as important as measuring the quantity of surgical operations performed [16]. The outcome of cataract surgery can be measured through postoperative level of visual acuity, ability to function, quality of life, and economic rehabilitation [17]. Since the patient's visual satisfaction, vision related quality of life, ability to function in daily activities and their overall productivity mainly depend on the visual outcome, the World Health Organization (WHO) recommends that poor (best corrected visual acuity [BCVA] <6/60) or borderline (BCVA <6/18) visual outcomes after cataract surgery should not be>10%–20% [3].
Cataract surgery is a curative and cost-effective intervention. As result blindness programs are tasked with providing good quality of surgery and sustainable services to meet present and future needs [18]. This requires the reasonable distribution of resources such as human, infrastructure, equipment, and materials. Multiple factors affecting output of existing cataract surgery services, many of which are provider related, like, the availability of surgeons, support staff. Health facilities, consumables equipment [19]. Previously, some studies were conducted in developing countries that reported regarding the burden and knowledge of cataract, and outcome of cataract surgery [8,10,17,19].Nevertheless, the time of recovery and determinants of recovery after cataract surgery not yet been elaborated among eye cataract patients. Hence, this retrospective follow up study was preliminarily attempt to identify determinants and the survival time of recovery of cataract patients by using Simi parametric models of survival analysis.
2. Methods and materials
2.1. Study design and setting
A retrospective follow-up study was conducted from January/01/2015 and January/30/2019 in comprehensive tertiary eye care center. This eye care center provides all-inclusive clinical and community eye care health services for the region and serves as a major referral center for more than 14 million people and which provides different specialty eye care services and training of eye care professionals such as Optometrists, Ophthalmologists, and ophthalmic nurses [8,20].
2.2. Source and study population
All cataract patients treated with eye cataract surgery in the study area were the source population, and the study population of this study was cataract patients treated between January 2015 and January 2019. All cataract patients treated with different types of cataract surgery were included in the study. However, patients with incomplete medical records were excluded, unfortunately no medical chart was excluded by incompleteness.
2.3. Sample size and sampling procedure
The sample size required for this study was determined using the single population proportion formula [21] and calculated using Epi Info software version7.1 (Centres for Disease Control and Prevention, USA). The derived power calculated sample size was n = 307 with an assumption of 95% confidence level, 5% margin of error, and proportion of estimated eye cataract patients (50%) and the sample were taken from a relatively small population (N = 1500), the required sample size were obtained by the following calculation.
| n = NZ2P (1-P)/d2 (N-1) +Z2P | (1-P) |
Where.
n = sample size
N = size of the target population = N= (the estimated number of eye cataract patients from Gondar University hospital eye care center registry)
Z = statistic for 95% level of confidence equal to 1.96
P = proportion estimated eye cataract patients 50%
d = margin of error = 5%
Therefore,N = 1500, Z = 1.96, d = 0.05, P = 0.5, q = 1-P = 0.5
n = 1500*(1.96)2 *0.5(1–0.5)/(0.05)2 * [1500-1] + (1.96)2 *0.5(1–0.5), n = 307
The study participants were recruited by using simple random sampling method. As the study was conducted through a review of records, no consent was asked from the study subjects. The confidentiality and privacy of the patient records were ensured by avoiding names and identification numbers from the extraction form and codes were used.
2.4. Data collection tools and procedures
A structured data extraction checklist and questionnaire was developed and used to extract information from patient medical registered chart. A two-day intensive practical training was given for data collectors on the objectives of the study and the procedure, how to review registration medical logbook and the patient's medical record chart, and to maintain the confidentiality of the data. Ophthalmic nurse professionals working at a cataract unit extracted the required data from patient medical charts under supervision. This study was reported in accordance with the declaration of Helsinki and registered at www.researchregistry.com with Research Registry UIN: research registry 6424. This study is reported according to the STROCSS guidelines [22].
2.5. Outcome measures
Time to recovery from cataract with visual acuity.
2.6. Data processing and analysis
Data were checked for completeness and entered into Epi-Info version 7.1 and then exported to STATA version14.0 statistical software for coding, recoding, storing and further analysis. The data were checked for inconsistencies, coding error, completeness, accuracy, clarity and missing values. Summary measures such as counts, percentages, medians, means and SD were calculated. The Kaplan-Meier survival method and log-rank test curves were applied to estimate the probability of recovery at a given time and to compare the survival curve, respectively. Cox proportional hazards assumption was checked using the Schoenfeld residuals test. Model selection was done using Akaike Information Criteria (AIC) and Bayesian Information Criteria. The parametrical survival analysis, Weibull regression, was used to identify predictors of time to recovery. Model goodness of fit was checked using Cox Snell residual test. Adjusted HRs (AHRs) with their respective 95% CIs was estimated and a value of p less than 0.05 was used to declare the presence of a significant association.
Initially, bivariable analysis was conducted and independent variables that were found statistically significant were included in multivariable analysis. When clear subgroups seemed present in the data, significance testing using Cox Snell residual test and interaction and multicollinearity analysis were done to check the cofounder variable effect.
3. Results
3.1. Baseline characteristics of the study participants
A total of 307 study participants with cataract medical chart were reviewed. Among the total participants 191 (62.2%) were males. One-quarter 79 (25.7%) of the study participants were above the age of 60 years old. Most of the study participants, 159 (51.8%), were urban dwellers. Nearly one in three, 107 (34.9%) participants were reported age related cataract. More than 170 (55.4%) of the cataract patient had gotten small incision cataract extraction (SICE) surgery and regarding the comorbidity, 117 (38.1%) of the cataract patients had diabetic mellitus (Table 1).
Table 1.
Baseline characteristics of study participants with cataract (n = 307).
| Variables | Category | Frequency | Percent (%) |
|---|---|---|---|
| Sex | Male | 191 | 62.2 |
| Female | 116 | 37.8 | |
| Age in years | 1–15 | 44 | 14.3 |
| 16–30 | 57 | 18.6 | |
| 31–45 | 62 | 20.2 | |
| 46–60 | 65 | 21.2 | |
| >60 | 79 | 25.7 | |
| Residence | Rural | 148 | 48.2 |
| Urban | 159 | 51.8 | |
| Smoking habit | No | 239 | 77.9 |
| Yes | 68 | 22.1 | |
| Drinking alcohol habit | Never | 75 | 24.4 |
| Past alcoholic | 130 | 42.4 | |
| Current alcoholic | 102 | 33.2 | |
| Diabetic Mellitus | No | 190 | 61.9 |
| Yes | 117 | 38.1 | |
| Level of Visual acuity | Low | 101 | 32.4 |
| Medium | 133 | 43.3 | |
| High | 73 | 23.8 | |
| Types of cataract | Age related | 107 | 34.9 |
| Traumatic | 115 | 37.4 | |
| Secondary | 43 | 14.0 | |
| Congenital | 42 | 13.7 | |
| Types of cataract surgery | SICE + PC IOL | 170 | 55.4 |
| ECCE + PC IOL | 137 | 44.6 |
SICE: Small incision cataract extraction; PC IOL: Post cataract intra ocular lenses; ECCE: Extract capsular cataract extraction.
3.2. Time to recovery of patients with cataract
A total of 223 cataract patients were recovered from cataract, make it a recovery rate of 72.6% with 95% CI 69.8%–75.9%) and 27.4% of them were censored. The recovery rate of men cataract patients were 73.3% whereas the recovery rate of women were 71.6%. The recovery rate for age related cataract was 61.7% while the recovery rate of cataract treated with extra capsular cataract extraction surgery was high (81.7%) (Table 2).
Table 2.
Predictors of time to recovery among cataract patients (n = 307).
| Variables | Recovery |
Crude HR (95%CI) | Adjusted HR (95%CI) | |
|---|---|---|---|---|
| Event (n %) | Censored (n %) | |||
| Sex | ||||
| Male | 140(73.3%) | 51(26.7%) | 1.02 (0.765–1.348) | 1.02 (0.76–1.35) |
| Female | 83(71.5%) | 33(28.5%) | 1 | 1 |
| Age in years | ||||
| 1–15 | 36 (81.8%) | 8(18.2%) | 1 | 1 |
| 16–30 | 51 (89.5%) | 6 (10.5%) | 1.12 (0.730–1 .362) | 1.20 (1.07–2.36)* |
| 31–45 | 50(80.6%) | 12(19.4%) | 1.24 (1 .08 -1 .53) | 1.24 (1.08–1.54)* |
| 46–60 | 50(76.9%) | 15(23.1%) | 1.35 (1.08–1 .81) | 1.35 (0.98–1.89) |
| >60 | 36(45.6%) | 43(54.4%) | 1.45 (1.005–2 .562) | 1.4 (1.0–2.56) |
| Residence | ||||
| Rural | 89(60.1%) | 59(39.9%) | 1 | 1 |
| Urban | 134(84.3%) | 25(15.7%) | 0.68 (0.17–1.13) | 1.59 (1.18–2.14)* |
| Smoking habit | ||||
| No | 179(74.9%) | 60(25.1%) | 1 | 1 |
| Yes | 44(64.7%) | 24(35.3%) | 0.80 (0.55–1.17) | 0.80 (0.55–1.17) |
| Drinking alcohol habit | ||||
| Never | 64(85.3%) | 11(14.7%) | 1 | 1 |
| Past alcoholic | 96(73.85%) | 34(26.2%) | 1.12 (0.71 1.76) | 1.12 (0.71–1.78) |
| Current alcoholic | 63(61.8%) | 39(38.2%) | 1.53 (1.09–1.96) | 0.87 (0.47–1.63) |
| Diabetic Mellitus | ||||
| No | 158(83.2%) | 32(16.8%) | 1 | 1 |
| Yes | 65(55.6%) | 52(44.4%) | 0.75(0.04–0.84) | 0.75 (0.41–0.96)* |
| Level of Visual acuity | ||||
| Low | 32(31.68%) | 69(68.3%) | 1 | 1 |
| Medium | 122(91.7%) | 11(8.3%) | 0.72 (0.25–2.59) | 4.14(2.57–6.67)* |
| High | 69(94.5%) | 4(5.5%) | 0.29 (0.12–2.09 | 5.23(3.06–8.93)* |
| Types of cataract | ||||
| Age related | 66(61.7%) | 41(38.3%) | 1 | 1 |
| Traumatic | 100(87.0%) | 15(13.0%) | 0.65 0 (0.09–2.17) | 1.75 (1.01–3.02)* |
| Secondary | 23(53.5%) | 20(46.5%) | 0.71 (0.15–2.97) | 2.59 (1.46–4.60)* |
| Congenital | 34(81.0%) | 8(19.0%) | 0.55 (0.04 1.13) | 2.64 (0.86–8.11) |
| Types of cataract surgery | ||||
| SICE + PC IOL | 111(65.3%) | 59(34.7%) | 1 | 1 |
| ECCE + PC IOL | 112(81.7%) | 25(18.3%) | 0.79 (0.13–1.87) | 1.43(1.07–1.94)* |
Note: * variables significant with p-value ≤0.05; 1 = reference category; CHR = crude hazard ratio; AHR = adjusted hazard ratio; CI = confidence interval.
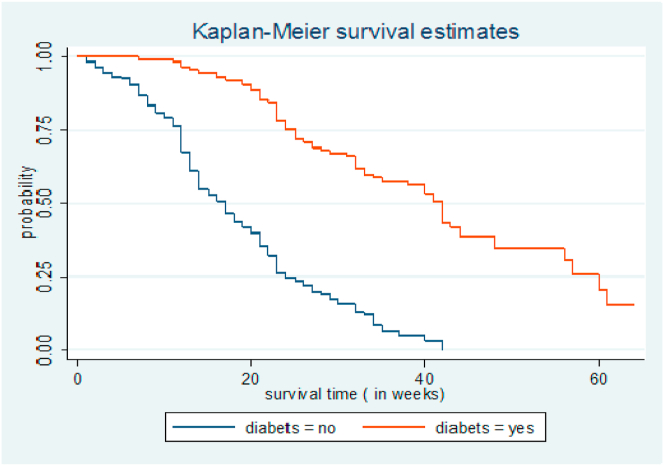
The overall median survival time was 23 weeks (IQR = 16 to 35) with (95% CI, 21%–25%). The average mean recovery time of the patients was 23.24 with (95% CI, 21.72%–24.76%). There was a significant difference in the time of recovery between cataract patients with/out DM, where cataract patients without DM comorbidity were recovered faster (Fig. 1). A significant difference seen in the recovery rate among the two groups by the log-rank test χ2 = 19.46 and p = 0.0001.
Fig. 1.
Kaplan-Meier survival estimate for time to recovery among cataract patients treated with cataract surgery, sub grouped by DM status (n = 307).
3.3. Factors affecting time of recovery
The overall Schoenfeld residual test of the full model has met the proportional hazards assumption (χ2 = 18.5 and p = 0.086). In the bivariable Weibull regression analysis sex, age, residence, smoking and alcoholic habit, Diabetic mellitus, visual acuity, type of cataract and surgery were used to estimate their crude HR. In multiple co-variate analysis, all the above variables used with forward stepwise variable selection method to select the predictor's variables in cox proportional hazard model. In multiple co-variate analysis age, resident, DM, visual acuity, type of cataract and surgery were estimated as independent predictors of time to recovery with a value of p < 0.05. Table 2 shows the result of multi co-variate analysis.
The recovery time of cataract patients those aged between 16 to 30 and 31–45 years had 20% and 24% faster recovery as compared with aged less than 166 years (AHR = 1.20 CI; 1.07–2.36) and (AHR = 1.24 CI; 1.08–1.54) respectively. Cataract patients who live in urban had 59% faster recovery as compared with rural dwellers (AHR = 1.59; 95% CI, 1.18–2.14). Patients with had medium and high level of visual acuity had higher recovery as compared with their lower visual acuity counterpart (AHR = 4.14 CI; 2.57–6.67) and (AHR = 5.23 CI; 3.06–8.93) respectively. Secondary cataract patients had 59% ((AHR = 2.59 CI; 1.01–3.02) and traumatic cataract had 75% (AHR = 1.75 CI; 1.01–3.02) faster recovery time as compared to age related cataract. Cataract patient who are treated with extra capsular cataract extraction surgery had 43% of recovery rate (AHR = 1.43 CI; 1.07–1.94). Whereas patients with DM had a 25% lower pace of recovery when compared with those without DM (AHR = 0.75, CI; 0.41–0.96).
4. Discussion
This study was conducted to determine the survival time to recovery and its predictors from eye cataract patients. The overall median time to recovery was 23 weeks and the mean time of recovery was 23.24 weeks. Age of the patients, residence, DM, initial level of visual acuity, types of cataract and surgery were independent predictors of time to recovery.
The median recovery time of cataract surgery in this study was 23 weeks. This finding was supported by another study [23,24]. This shows the recovery after cataract surgery is now easier and patients no longer required inpatient hospital care after the cataract surgery. It concluded that the recovery time of cataract surgery is short; as result soreness and discomfort will disappear within a couple of weeks. However some studies reported that full recovery of cataract after surgery could take from four to sixteen weeks [[25], [26], [27]]. This could be due to the nature, the size of cataract and physiological difference. Another possible explanation might be the difference in type of surgical management, follow up time, and health facility service.
Adult cataract patients aged from 16 to 45 years had faster recovery as compared with children and older individual. This finding is supported in India [28]. The possible reason in this study could be due to an older age individual have a chance of coexisting ocular pathology and have associated medical co-morbidity.
Cataract patients who live in urban had 59% faster recovery as compared with rural dwellers. This finding reinforced by other studies with cataract patient lived in rural hindered from accessing sight restoring services in the area and urban dwellers had availability of eye care service and get appropriate utilization services timely [29,30]. Secondary cataract and traumatic cataract had faster recovery time as compared to age related cataract. This finding is supported by Indian study [31], which reported that good visual outcome after managing traumatic cataract with cataract surgery. Satisfactory visual acuity following cataract surgery was associated with eyes having open globe injuries and managed using a primary posterior capsulotomy and vistrectomy. The possible reason might be age-related cataract associated with coexisting ocular pathology causing loss of vision and age causes degeneration of lenses.
Cataract patient who are treated with extra capsular cataract extraction surgery had 43% of faster recovery rate as compared with Small incision cataract extraction surgery. This finding in line with the study done in Ghana [32],Nepal [33] and another randomised trial study done in London, UK on extra capsular cataract extraction surgery and small incision surgery with phacoemulsification showed that significantly less surgical complication and had higher proportional visual acuity [34]. As results, cataract patients treated with ECCE had the potential to reduce postoperative astigmatism and hasten visual rehabilitation of the patients.
Cataract patients with DM had a 25% lower pace of recovery when compared with those without DM. The finding of this study supported by the study done in Finland [35]. Diabetes increase the risk the retinal complication of the eye and the incidence of pseudophakic cystoid macular oedema after a routine cataract surgery is higher among diabetic patients compared to those without diabetes [36,37]. This could be the level of macular oedema after cataract surgery and pseudophakic cystoid macular oedema correlate with the diabetic retinopathy.
5. The strength and limitation of the study
This study has used a relatively large data set and parametric model which results in a better estimate of the magnitude of recovery and the predictors affecting it. Considering the benefits of future research, there are certainly few limitations to be mentioned. Being a retrospective study we were unable to find some important variables that should be considered to identify predictors. Hence, the findings should be interpreted with caution.
6. Conclusion
This retrospective cohort study assessed the time to recovery from cataract sing parametric model and has put forward a precise estimate of its predictors. Time to recovery in the study area was slightly higher as compared with the global cut of time. According to this study, middle age, urban resident, secondary cataract and patients treated with extra capsular extraction surgery had faster recovery rate. On contrary, cataract patients with comorbidity of DM had lower recovery time. Special emphasis should be given to prevent and treat comorbidities besides the cataract surgery in order to improve recovery time.
Provenance and peer review
Not commissioned, externally peer-reviewed.
Research registration unique identification number (UIN)
Research registry UIN: 6424.
Ethical approval
Ethical clearance was secured from the ethical review committee of the College of Natural and Computational sciences, University of Gondar, Ethiopia with reference number of: CNCS/10/662/7/2020. The names of the subjects were not extracted to insure privacy of patients and confidentiality was maintained throughout the data collection and analysis process. To collect the data, permission was obtained from medical board committee of University of Gondar referral Hospital and department of ophthalmologist of university of Gondar tertiary eye care and training center.
Author contribution
Beyene AM developed the proposal, organized data collection, analyzed the data, prepared and revised the manuscript. AE, Getnet MG, and AE revised the proposal, involved in data collection, data analysis, and revised the manuscript. AE and Getnet MG wrote the manuscript. All authors approved the final manuscript for publication.
Declaration of competing interest
All authors declare no conflict of interest.
Consent
We are not used Personal identifiers in the manuscript and during data collection processes. So consent for publication not applicable.
Registration of research studies
Research registry UIN: 6424.
Guarantor
Moges Gashaw Getnet, Asmare Mihret Beyene, Aragaw Esheti, Yohannes Tadesse.
Acknowledgments
The authors would like to thank you the data collectors and supervisors for their commitment.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.amsu.2021.102275.
Contributor Information
Asmare Mihret Beyene, Email: asmaremihret67@gmail.com.
Yohannes Tadesse, Email: yohannes023@gmail.com.
Moges Gashaw Getnet, Email: moges.gashaw@uog.edu.et.
List of Abbreviations/acronym
- AHR
Adjusted Hazard Ratio
- BCVA
Best Corrected Visual Acuity
- CI
Confidence Interval
- CHR
Cruds Odds Ratio
- DM
Diabetes Mellitus
- ECCE
Extra capsular Cataract Extraction
- SD
Standard Deviation
- SICE
Small Incision Cataract Extraction
- WHO
World Health Organization
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- 1.Salomão S.R., Mitsuhiro M.R., Belfort R., Jr. Visual impairment and blindness: an overview of prevalence and causes in Brazil. An. Acad. Bras. Cienc. 2009;81(3):539–549. doi: 10.1590/s0001-37652009000300017. [DOI] [PubMed] [Google Scholar]
- 2.Kuper H., Polack S., Eusebio C., Mathenge W., Wadud Z., Foster A. A case-control study to assess the relationship between poverty and visual impairment from cataract in Kenya, the Philippines, and Bangladesh. PLoS Med. 2008;5(12) doi: 10.1371/journal.pmed.0050244. e244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.World Health Organization Media centre Vision impairment and blindness. World Health Organization. 2017;2017(20) [Internet] [Google Scholar]
- 4.Oduntan A. Prevalence and causes of low vision and blindness worldwide. African Vision and Eye Health. 2005;64(2):44–57. [Google Scholar]
- 5.Stevens G.A., White R.A., Flaxman S.R., Price H., Jonas J.B., Keeffe J. Global prevalence of vision impairment and blindness: magnitude and temporal trends, 1990–2010. Ophthalmology. 2013;120(12):2377–2384. doi: 10.1016/j.ophtha.2013.05.025. [DOI] [PubMed] [Google Scholar]
- 6.Berhane Y., Worku A., Bejiga A., Adamu L., Alemayehu W., Bedri A. National survey on blindness, low vision and trachoma in Ethiopia: methods and study clusters profile. Ethiop. J. Health Dev. 2007;21(3):185–203. [Google Scholar]
- 7.Berhane Y., Worku A., Bejiga A., Adamu L., Alemayehu W., Bedri A. Prevalence and causes of blindness and low vision in Ethiopia. Ethiop. J. Health Dev. 2007;21(3):204–210. [Google Scholar]
- 8.Alimaw Y.A., Hussen M.S., Tefera T.K., Yibekal B.T. Knowledge about cataract and associated factors among adults in Gondar town, northwest Ethiopia. PloS One. 2019;14(4) doi: 10.1371/journal.pone.0215809. e0215809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Murthy G., Gupta S.K., John N., Vashist P. Current status of cataract blindness and Vision 2020: the right to sight initiative in India. Indian J. Ophthalmol. 2008;56(6):489. doi: 10.4103/0301-4738.42774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bhagwan J., Rastogi I., Malik J., Dhull C. Knowledge, attitude and practices regarding cataract surgery among senile cataract cases in Haryana. Indian J. Community Med. 2006;31(2):66–68. [Google Scholar]
- 11.Rao G.N., Khanna R., Payal A. The global burden of cataract. Curr. Opin. Ophthalmol. 2011;22(1):4–9. doi: 10.1097/ICU.0b013e3283414fc8. [DOI] [PubMed] [Google Scholar]
- 12.Ormsby G.M., Arnold A.-L., Busija L., Mörchen M., Keeffe J.E. The impact of knowledge and attitudes on access to eye-care services in Cambodia. The Asia-Pacific Journal of Ophthalmology. 2012;1(6):331–335. doi: 10.1097/APO.0b013e31826d9e06. [DOI] [PubMed] [Google Scholar]
- 13.Magliyah M.S., Nageeb M.R., Abdulmannan D.M., Badr H.M., Hemmeish M.M., Alotaibi W.T. Assessment of knowledge regarding cataract among Saudi adult population in Makkah city, Saudi Arabia. Int. J. Med. Sci. Publ. Health. 2015;4(5):595–600. [Google Scholar]
- 14.Habtamu E., Eshete Z., Burton M.J. Cataract surgery in Southern Ethiopia: distribution, rates and determinants of service provision. BMC Health Serv. Res. 2013;13(1):1–12. doi: 10.1186/1472-6963-13-480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kuper H., Polack S., Mathenge W., Eusebio C., Wadud Z., Rashid M. Does cataract surgery alleviate poverty? Evidence from a multi-centre intervention study conducted in Kenya, the Philippines and Bangladesh. PloS One. 2010;5(11) doi: 10.1371/journal.pone.0015431. e15431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Baltussen R., Sylla M., Mariotti S.P. Cost-effectiveness analysis of cataract surgery: a global and regional analysis. Bull. World Health Organ. 2004;82:338–345. [PMC free article] [PubMed] [Google Scholar]
- 17.Habtamu E., Eshete Z., Burton M.J. Cataract surgery in Southern Ethiopia: distribution, rates and determinants of service provision. BMC Health Serv. Res. 2013;13(1):480. doi: 10.1186/1472-6963-13-480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Johnson G.J., Minassian D.C., Weale R.A., West S.K. Arnold; 2003. The Epidemiology of Eye Disease. [Google Scholar]
- 19.Courtright P., Ndegwa L., Msosa J., Banzi J. Use of our existing eye care human resources: assessment of the productivity of cataract surgeons trained in eastern Africa. Arch. Ophthalmol. 2007;125(5):684–687. doi: 10.1001/archopht.125.5.684. [DOI] [PubMed] [Google Scholar]
- 20.Gashaw M., Janakiraman B., Minyihun A., Jember G., Sany K. Self-reported fall and associated factors among adult people with visual impairment in Gondar, Ethiopia: a cross-sectional study. BMC Publ. Health. 2020;20:1–10. doi: 10.1186/s12889-020-08628-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kasiulevičius V., Šapoka V., Filipavičiūtė R. Sample size calculation in epidemiological studies. Gerontol. 2006;7(4):225–231. [Google Scholar]
- 22.Agha R., Abdall-Razak A., Crossley E., Dowlut N., Iosifidis C., Mathew G. STROCSS 2019 Guideline: strengthening the reporting of cohort studies in surgery. Int. J. Surg. 2019;72:156–165. doi: 10.1016/j.ijsu.2019.11.002. [DOI] [PubMed] [Google Scholar]
- 23.M Taghai G . 2008. Comparison of Recovery Time and Complications in General Anesthesia with Remifentanyl and Propofol and Topical Anesthesia with Conscious Sedation in Non-complicated Cataract Phaco Surgery. [Google Scholar]
- 24.Porela‐Tiihonen S., Kokki H., Kaarniranta K., Kokki M. Recovery after cataract surgery. Acta Ophthalmol. 2016;94:1–34. doi: 10.1111/aos.13055. [DOI] [PubMed] [Google Scholar]
- 25.Li E., Margo C.E., Greenberg P.B. Cataract surgery outcomes in the very elderly. J. Cataract Refract. Surg. 2018;44(9):1144–1149. doi: 10.1016/j.jcrs.2018.05.025. [DOI] [PubMed] [Google Scholar]
- 26.Alió J., Rodríguez-Prats J.L., Galal A., Ramzy M. Outcomes of microincision cataract surgery versus coaxial phacoemulsification. Ophthalmology. 2005;112(11):1997–2003. doi: 10.1016/j.ophtha.2005.06.024. [DOI] [PubMed] [Google Scholar]
- 27.Shah M.A., Shah S.M., Shah S.B., Patel U.A. Effect of interval between time of injury and timing of intervention on final visual outcome in cases of traumatic cataract. Eur. J. Ophthalmol. 2011;21(6):760–765. doi: 10.5301/EJO.2011.6482. [DOI] [PubMed] [Google Scholar]
- 28.Hankinson S. WB Saunders; Philadelphia: 1994. The Epidemiology of Age-Related Cataract. Principles and Practice of Ophthalmology; pp. 1255–1266. [Google Scholar]
- 29.Rabiu M.M. Cataract blindness and barriers to uptake of cataract surgery in a rural community of northern Nigeria. Br. J. Ophthalmol. 2001;85(7):776–780. doi: 10.1136/bjo.85.7.776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Snellingen T., Shrestha B., Gharti M., Shrestha J., Upadhyay M., Pokhrel R. Socioeconomic barriers to cataract surgery in Nepal: the South Asian cataract management study. Br. J. Ophthalmol. 1998;82(12):1424–1428. doi: 10.1136/bjo.82.12.1424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Shah M., Shah S., Shah S., Prasad V., Parikh A. Visual recovery and predictors of visual prognosis after managing traumatic cataracts in 555 patients. Indian J. Ophthalmol. 2011;59(3):217. doi: 10.4103/0301-4738.81043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Guzek J.P., Ching A. Small-incision manual extracapsular cataract surgery in Ghana, West Africa. J. Cataract Refract. Surg. 2003;29(1):57–64. doi: 10.1016/s0886-3350(02)01440-2. [DOI] [PubMed] [Google Scholar]
- 33.Ruit S., Tabin G., Chang D., Bajracharya L., Kline D.C., Richheimer W. A prospective randomized clinical trial of phacoemulsification vs manual sutureless small-incision extracapsular cataract surgery in Nepal. Am. J. Ophthalmol. 2007;143(1):32–38. doi: 10.1016/j.ajo.2006.07.023. e2. [DOI] [PubMed] [Google Scholar]
- 34.Minassian D., Rosen P., Dart J., Reidy A., Desai P., Sidhu M. Extracapsular cataract extraction compared with small incision surgery by phacoemulsification: a randomised trial. Br. J. Ophthalmol. 2001;85(7):822–829. doi: 10.1136/bjo.85.7.822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Danni R., Taipale C., Ilveskoski L., Tuuminen R. Diabetes alone does not impair recovery from uneventful cataract surgery. Am. J. Ophthalmol. 2019;198:37–44. doi: 10.1016/j.ajo.2018.09.030. [DOI] [PubMed] [Google Scholar]
- 36.Schmier J.K., Halpern M.T., Covert D.W., Matthews G.P. Evaluation of costs for cystoid macular edema among patients after cataract surgery. Retina. 2007;27(5):621–628. doi: 10.1097/01.iae.0000249577.92800.c0. [DOI] [PubMed] [Google Scholar]
- 37.Chu C.J., Johnston R.L., Buscombe C., Sallam A.B., Mohamed Q., Yang Y.C. Risk factors and incidence of macular edema after cataract surgery: a database study of 81984 eyes. Ophthalmology. 2016;123(2):316–323. doi: 10.1016/j.ophtha.2015.10.001. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.